Abstract
The practice of outpatient breast cancer surgery has been controversial in the United States. This study aimed to update time trends and geographic variation in outpatient breast cancer surgery among elderly Medicare fee-for-service women in the United States. Using the 1993–2002 linked Surveillance, Epidemiology and End Results (SEER)–Medicare claims data and the Area Resource Files, we identified 2 study samples, including the women whose breast cancers were the first-ever-diagnosed cancer at age 65 years or older from 9 regions continuously covered by the SEER registries since 1993. The first sample included the women receiving unilateral mastectomy for stage 0–IV cancer; the second included the women receiving the breast-conserving surgery with lymph node dissection (BCS/LND) for stage 0–II cancer. The proportions of patients receiving outpatient surgery increased from 3.2% to 19.4% for mastectomy and from 48.9% to 77.8% for BCS/LND from 1993 to 2002. We observed substantial geographic variation in the average proportion of the patients receiving outpatient surgery in the studied areas across the 10-year period, ranging from 3.9% in Connecticut to 27.2% in Utah for mastectomy and from 54.7% in Hawaii to 78.1% in Seattle, Washington, for BCS/LND. As the popularity of outpatient breast cancer surgery continues to grow, more evidence-based analyses related to quality and outcomes of outpatient breast cancer surgery among various populations are needed in order to facilitate the public debates about state and federal mandated health benefit legislations.
Keywords: Outpatient surgical procedures, breast neoplasm, quality of care, mandated health benefit laws
The use of outpatient (so-called “drive-through”) breast cancer surgery increased rapidly in the United States (U. S.) during the 1990s [1]–[3]. Among all women enrolled in either managed care or fee-for-service (FFS) plans in 5 states, the proportion of patients receiving outpatient mastectomy grew from 1%–2% in 1993 to 8% –22% in 19961[1]. Warren et al.[3] reported that the proportion of patients receiving outpatient mastectomy among elderly Medicare FFS women in the U.S. increased from virtually 0% to 11% during 1986–1995. However, the practice of outpatient breast cancer surgery has been controversial.
Opponents of outpatient breast cancer surgery, alleging increasing managed care influence in the U.S. for this shift in the delivery setting, have expressed concerns that by pressuring patients to undergo outpatient surgery, managed care plans may take away the patient's right of choice, with potentially detrimental implications for the quality and outcomes of health care[4],[5]. Proponents, on the other hand, counter that the choice of outpatient mastectomy may offer a surgery delivery setting better reflecting the preferences of patients and their physicians and may not adversely affect health outcomes of outpatient breast cancer surgery[6]. Almost no evidence has shown differences in quality or outcomes of health care between the patients receiving outpatient breast cancer surgery and those receiving inpatient one. However, one recent study found a negative association of outpatient mastectomy with the use of breast reconstruction[7], suggesting that the patients receiving outpatient mastectomy may not receive adequate post-mastectomy care.
The increasing popularity of outpatient breast cancer surgery began to attract widespread public attention in the U.S. in 1997, including warnings against “drive-through” mastectomy in the 1997 U.S. Presidential State of Union Address and the introduction of the Breast Cancer Patient Protection Act of 1997, a U. S. federal bill that mandated inpatient coverage for breast cancer surgery while providing patients and physicians with choices of deliver setting of surgery[8],[9]. Since then, more than 20 states in the U.S. have passed laws mandating inpatient coverage for breast cancer surgery[10], and the Breast Cancer Patient Protection Act (a U.S. federal bill) has been subsequently reintroduced 5 times, including the latest one in 2007[11].
This study aimed to update the time trends and geographic variation in outpatient breast cancer surgery in the U. S., reported in a previous study from 1986 to 1995[3]. Using the 1993–2002 linked Surveillance, Epidemiology and End Results (SEER)–Medicare claims data, we analyzed information from elderly women enrolled in Medicare FFS plans, who were newly diagnosed with breast cancer and underwent mastectomy or breast-conserving surgery with lymph node dissection (BCS/LND). The two outpatient breast cancer surgeries have been targeted by most state mandated-benefit laws and are currently under the consideration of the federal legislation[10],[11]. In the end, we briefly discussed some policy implications in the context of mandated-benefit laws because there have been heated ongoing debates over the merits of such mandated-benefit legislations.
Data and Methods
Data sources
Two datasets were used for this study. The first was the 1993–2002 linked SEER-Medicare claims data. (The SEER program is a cancer registry covering approximately 20%–25% of the U.S. populations.) The other was the Area Resource Files providing county-level proxy variables characterizing the demand for and supply of health care resources during 1993–2002. (For a detailed discussion of the linked SEER-Medicare claims data, see the work by Warren et al.[12] Cooper et al.[13], and Du et al.[14])
The SEER-Medicare claims data provided a unique opportunity to identify surgical treatments for diagnosed breast cancer cases and corresponding surgery delivery settings. Two main components of the linked data were relevant to this study. The first component includes information on patient demographics, cancer diagnoses, cancer stage at diagnosis (e.g., stage defined by the American Joint Committee on Cancer), treatment within 4 months of diagnosis (e.g., type of surgery, receipt of lymph node dissection), and monthly indictors for Medicare managed care enrollment status. The second component includes Medicare inpatient, outpatient, and physician supplier claims data.
The patient sample included the women newly diagnosed with breast cancer at age 65 years or older from the SEER registries. Five entire states and 4 large metropolitan areas (or partial states), continuously covered by SEER registries since 1993, were eligible for this study. The 5 entire states are Connecticut, Hawaii, Iowa, New Mexico, and Utah, and the 4 large metropolitan areas are Atlanta, Georgia; San Francisco, San Jose, and Los Angeles, California; Detroit, Michigan; and Seattle, Washington. We further restricted the sample to the women whose breast cancers were the first-ever-diagnosed cancer, who received unilateral mastectomy (that is, total/simple or modified radical mastectomy) for stage 0–IV cancer or BCS/LND (that is, segmental mastectomy, lumpectomy, quadrantectomy, tylectomy, wedge resection, excisional biopsy, partial mastectomy) for stage 0–II cancer, who were not enrolled in Medicare managed care plans, who had both Medicare Part A and Part B benefits at diagnosis.
The delivery setting for each corresponding mastectomy or BCS/LND was of key interest, determined from Medicare inpatient, outpatient, and physician supplier claims data[13],[14]. It was coded as 1 if a surgery was delivered in a hospital outpatient setting or 0 if a surgery was delivered in an inpatient setting. Primary and secondary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes and Current Procedural Terminology, Fourth Edition (CPT-4) codes in the claims data used to identify mastectomy and BCS/LND were based on the work by Nattinger et al.[15]. (See the detailed algorithm by Bian et al.[7] used to determine the surgery delivery setting.)
Statistical analysis
We summarized the time trends and geographic variation in outpatient delivery by either type of breast cancer surgery, and analyzed these time trends and geographic variation in outpatient delivery, using multivariable logistic regression models controlling for patient-level characteristics (that is, race/ethnicity, age, marital status, comorbidities[16],[17], and cancer stage at diagnosis) and county-level demand and supply variables for health care resources at the SEER registry location (that is, per capita income in $10 000, county population, the number of short-term acute hospital beds per 1000 county population, and the number of specialty surgeons per 1000 county population[18]). A set of dummy indicators for years and states in which the SEER registries were located was used in the regression models for time and geographic comparisons. In addition, we controlled for the Metropolitan Statistical Area status of the SEER registries. Standard errors were adjusted for Huber standard errors correction[19].
Results
Descriptive statistics
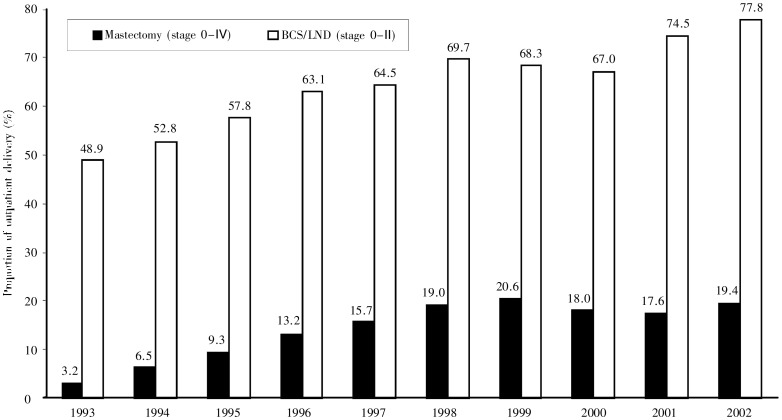
In the 9 regions, 27 261 patients with breast cancer received mastectomy, and 3680 (13.5%) of them received outpatient mastectomy. In the same regions, 17 180 received BCS/LND, and 11 330 (65.9%) of them received outpatient BCS/LND. Figure 1 illustrates the time trends of utilization of outpatient breast cancer surgery. The proportion of outpatient delivery of mastectomy increased from 3.2% in 1993 to 20.6% in 1999, declined to 17.6% in 2001, and increased again to 19.4% in 2002. Similarly, the proportion of outpatient delivery of BCS/LND increased from 48.9% in 1993 to 69.7% in 1998, declined to 67.0% in 2000, and rose to 77.8% in 2002. The proportions of outpatient delivery between 1993 and 2002 were increased by 506% (from 3.2% to 19.4% ) for mastectomy and by 59% (from 48.9% to 77.8%) for BCS/LND.
Figure 1. Time trends of outpatient delivery of breast cancer surgery among Medicare fee-for-service women. Each black bar represents the proportion of outpatient delivery of mastectomy for stage 0–II cancer in each year. Each white bar represents the proportion of outpatient delivery breast-conserving surgery with lymph node dissection (BCS/LND) for stage 0–II cancer in each year.
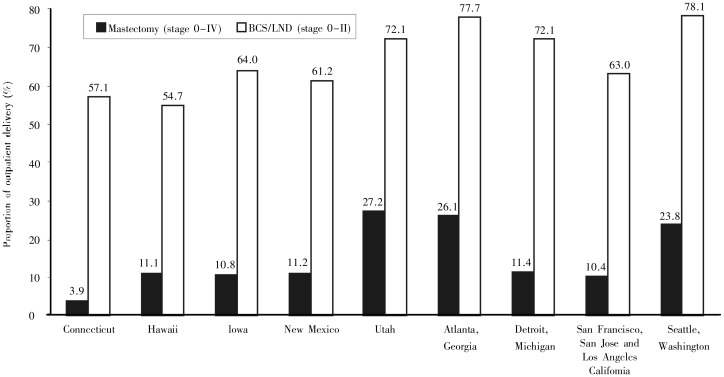
There was substantial geographic variation in the proportion of outpatient breast cancer surgery (Figure 2). Among the 5 states covered by the SEER registries across the 10-year study period, Utah had the highest average annual proportions of both outpatient mastectomy (27.2%) and outpatient BCS/LND (72.1%), whereas Connecticut had the lowest average annual proportion of outpatient mastectomy (3.9%) and Hawaii had the lowest average annual proportion of outpatient BCS/LND (54.7%). Among the 4 large metropolitan areas, the average annual proportion of outpatient mastectomy was the highest at 26.1% in Atlanta, and the proportion of outpatient BCS/LND was the highest at 78.1% in Seattle. The 3 big cities in California had the lowest average annual proportions of both outpatient mastectomy (10.4%) and outpatient BCS/LND (63.0%).
Figure 2. Geographic variation in outpatient delivery of breast cancer surgery among Medicare fee-for-service women during 1993–2002. Each black bar represents the proportion of outpatient delivery of mastectomy for stage 0–II cancer in each area during 1993–2002. Each white bar represents the proportion of outpatient delivery of BCS/LND for stage 0–II cancer in each area during 1993–2002.
Table 1 shows the time trends in the proportion of outpatient surgery by region over the 10-year study period. Similar to the patterns observed above, the proportion of either outpatient mastectomy or outpatient BCS/LND in most states or large metropolitan areas increased rapidly since 1993, reached a plateau in 1998, and rose again after 2001. Among the 5 states, the proportions of outpatient delivery were the highest at 38.7% in Utah in 1999 for mastectomy and at 78.6% in Connecticut in 2002 for BCS/LND. Among the 4 large metropolitan areas, the proportions were the highest at 40.8% in Seattle in 1999 for mastectomy and at 90.3% in Atlanta in 2002 for BCS/LND. (Additional mean descriptive statistics of the two samples are shown in the middle panel of Table 2.)
Table 1. Geographic variation in proportion of outpatient delivery of breast cancer surgery from 1993 to 2002.
| Area | Surgery | Proportion of outpatient delivery in each year (%) |
|||||||||
| 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | ||
| Connecticut | |||||||||||
| Mastectomy | 0.5 | 1.7 | 2.7 | 4.3 | 4.7 | 2.7 | 5.1 | 9.1 | 9.5 | 3.3 | |
| BCS/LND | 42.3 | 49.3 | 47.1 | 52.0 | 53.2 | 55.8 | 58.6 | 54.2 | 65.6 | 78.6 | |
| Hawaii | |||||||||||
| Mastectomy | 0.0 | 0.0 | 1.5 | 1.5 | 14.6 | 10.1 | 16.5 | 21.9 | 22.7 | 21.7 | |
| BCS/LND | 40.7 | 47.5 | 51.7 | 45.9 | 50.0 | 57.1 | 40.0 | 62.0 | 65.7 | 66.7 | |
| Iowa | |||||||||||
| Mastectomy | 1.3 | 4.8 | 5.4 | 9.5 | 17.3 | 16.5 | 19.9 | 12.1 | 11.8 | 13.3 | |
| BCS/LND | 50.0 | 51.2 | 59.0 | 62.7 | 61.7 | 70.6 | 68.3 | 58.8 | 72.6 | 68.9 | |
| New Mexico | |||||||||||
| Mastectomy | 3.0 | 3.9 | 9.2 | 14.6 | 4.0 | 11.1 | 16.0 | 13.3 | 12.5 | 26.2 | |
| BCS/LND | 44.2 | 44.7 | 48.5 | 60.9 | 45.5 | 59.2 | 62.5 | 71.1 | 78.4 | 70.6 | |
| Utah | |||||||||||
| Mastectomy | 14.0 | 19.3 | 22.5 | 29.7 | 24.3 | 30.9 | 38.7 | 32.4 | 25.1 | 36.5 | |
| BCS/LND | 60.7 | 69.5 | 73.8 | 71.2 | 81.7 | 65.5 | 73.1 | 76.5 | 73.3 | 71.6 | |
| Atlanta, Georgia | |||||||||||
| Mastectomy | 6.9 | 16.0 | 23.2 | 26.6 | 28.9 | 36.8 | 36.7 | 34.3 | 33.6 | 28.8 | |
| BCS/LND | 52.1 | 61.8 | 65.3 | 72.4 | 78.1 | 81.6 | 78.9 | 85.2 | 88.0 | 90.3 | |
| Detroit, Michigan | |||||||||||
| Mastectomy | 1.6 | 2.7 | 7.3 | 13.0 | 12.6 | 15.8 | 16.0 | 17.7 | 15.4 | 18.4 | |
| BCS/LND | 45.9 | 43.7 | 53.0 | 60.5 | 68.8 | 73.8 | 73.6 | 75.6 | 83.3 | 84.4 | |
| San Francisco, San Jose and Los Angeles, California | |||||||||||
| Mastectomy | 1.8 | 5.0 | 8.2 | 9.8 | 12.1 | 17.7 | 13.1 | 14.7 | 13.6 | 16.5 | |
| BCS/LND | 46.0 | 51.3 | 56.5 | 62.4 | 60.7 | 68.0 | 65.6 | 63.8 | 71.6 | 73.9 | |
| Seattle, Washington | |||||||||||
| Mastectomy | 7.9 | 12.6 | 16.8 | 21.4 | 28.4 | 37.0 | 40.8 | 24.6 | 31.5 | 29.3 | |
| BCS/LND | 66.7 | 67.9 | 74.9 | 79.4 | 81.4 | 82.1 | 79.5 | 74.9 | 78.2 | 86.1 | |
All data are from 1993–2002 linked Surveillance, Epidemiology and End Results (SEER) Medicare. BCS/LND, breast conserving surgery with lymph node dissection.
Table 2. Summary of mean descriptive statistics and estimates of multivariate Logistic regression model of the outpatient delivery of breast cancer surgery from 1993 to 2002.
| Variate | Mean descriptive statistics |
Adjusted odds ratioa |
||||
| Mastectomy |
BCS/LND |
Mastectomy (n=27 261) | BCS/LNC (n=17 180) | |||
| Inpatient (n=23 581) | Outpatient (n=3 680) | Inpatient (n=5 850) | Outpatient (n=11 330) | |||
| Non-whites | 0.14 | 0.13 | 0.13 | 0.12 | 0.98 | 1.00 |
| Age ≥ 75 years (vs. age < 75 years) | 0.52 | 0.49 | 0.39 | 0.37 | 0.89c | 0.87c |
| Married | 0.42 | 0.46 | 0.50 | 0.53 | 1.08 | 1.06 |
| Charlson index ≥ 1 (vs. Charlson index = 0) | 0.25 | 0.14 | 0.21 | 0.08 | 0.50c | 0.32c |
| Cancer stage III or IV (vs. cancer stage 0, I, or II) | 0.11 | 0.08 | n/a | n/a | 0.64c | n/a |
| Total mastectomy (vs. modified radical mastectomy) | 0.08 | 0.19 | n/a | n/a | 2.04c | n/a |
| Per capita income in $10 000 | 2.51 | 2.69 | 2.70 | 2.83 | 1.03 | 1.12c |
| County population in 100 000 people | 18.95 | 15.09 | 22.95 | 23.60 | 0.99b | 1.00c |
| Number of specialty surgeons per 1000 people | 0.51 | 0.55 | 0.59 | 0.57 | 1.50c | 0.62c |
| Number of short-term acute hospital beds per 1000 people | 2.97 | 2.70 | 2.79 | 2.67 | 0.93c | 1.07c |
| Metropolitan Statistics Area | 0.79 | 0.86 | 0.87 | 0.89 | 1.91c | 1.35c |
| Connecticut (reference) | 0.11 | 0.03 | 0.17 | 0.12 | 1.00 | 1.00 |
| Hawaii | 0.03 | 0.02 | 0.04 | 0.02 | 3.87c | 0.91 |
| Iowa | 0.20 | 0.15 | 0.11 | 0.10 | 6.36c | 1.32c |
| New Mexico | 0.05 | 0.04 | 0.04 | 0.03 | 4.93c | 1.31b |
| Utah | 0.05 | 0.13 | 0.04 | 0.05 | 13.01c | 2.24c |
| Atlanta, Georgia | 0.05 | 0.12 | 0.04 | 0.07 | 10.09c | 2.62c |
| Detroit, Michigan | 0.16 | 0.13 | 0.14 | 0.16 | 3.86c | 1.53c |
| San Francisco, San Jose and Los Angeles, California | 0.26 | 0.19 | 0.34 | 0.30 | 3.64c | 1.00 |
| Seattle, Washington | 0.10 | 0.19 | 0.08 | 0.14 | 9.62c | 2.80c |
All data are from 1993–2002 linked SEER Medicare and Area Resource Files. Estimates of year dummies, jointly statistically significant at 1%, are not reported here. aThe dependent variable was surgery delivery setting: 1 if outpatient or 0 if inpatient. bP < 0.05; cP < 0.01.
Regression estimates
In the multivariable regression analyses of the associations of patient- and county-level characteristics with surgery delivery setting (shown in the right panel of Table 2), patients with more comorbidities, older age, or a higher stage of cancer at diagnosis were more likely to receive an inpatient surgery; and non-white patients were more likely than white patients to receive an inpatient surgery (all P < 0.01). However, county-level variables (such as population and per capita income) did not differ by surgery delivery setting for either surgery. The results from the multivariable models were consistent with those from the descriptive analysis.
Discussion
Our study found that from 1993 to 2002, the proportion of outpatient breast cancer surgery increased by more than 506% from 3.2% to 19.4% for mastectomy and by 59% from 48.9% to 77.8% for BCS/LND among the women enrolled in the Medicare FFS plans in the 9 regions studied. The proportion of outpatient surgery did not increase consistently for each year of the study period; it was decreased during 1999–2001. We also observed substantial geographic variation in the proportion of outpatient surgery over time. For example, the proportions of outpatient mastectomy were the highest at 27% in Utah and the lowest at 4% in Connecticut, varying by approximately 7-fold difference between the two states. The time trend of the proportion of outpatient mastectomy for Medicare elderly FFS patients in this update is very similar to the time trend reported in an earlier study during 1993–1995, an overlapping period of the two studies. Warren et al.[3] reported that the proportions were 4.7% in 1993, 7.3% in 1994, and 10.8% in 1995. The corresponding proportions in our study were 3.2%, 6.5%, and 9.3%, respectively.
There are some limitations to this study. First, outpatient mastectomy has been alleged to result from managed care influence on health care cost containment. Thus, it may be important to analyze populations who were directly affected by the managed care influence (e.g., patients enrolled in managed care plans). However, we were unable to study outpatient breast cancer surgery received by the Medicare managed care patients because these patients' claims data are not available. Second, this study did not examine some important factors associated with outpatient breast cancer surgery. For example, Warren et al.[3], using only Medicare claims data, suggested that outpatient mastectomy may be more likely to be performed in non-teaching or for-profit hospitals. Missing data on hospital characteristics in the linked SEER-Medicare claims data limited our ability to analyze the associations of those important organizational factors with the proportion of outpatient breast cancer surgery. Third, quality and outcomes of outpatient breast cancer surgery were not studied here. Lack of scientific evidence on quality and outcomes has hampered the public debates about the practice of outpatient breast cancer surgery.
Nonetheless, the updated time trends and geographic variation in outpatient breast cancer surgery highlighted some important policy implications related to the ongoing debates about mandated inpatient coverage for breast cancer surgery at both the state and the federal levels.
The reversed increasing trends in outpatient breast cancer surgery in 2000 and 2001 from those in the previous period may merit special policy attention. One possible explanation for the changes in trend may be increased public awareness of outpatient breast cancer surgery after mass media coverage for this practice, beginning in 1997[8],[10]. Another is that the widespread passages of state laws mandating inpatient coverage for breast cancer surgery between 1997 and 1999 may have, at least temporally, curbed outpatient use of the two types of breast cancer surgery shortly after the adoption of the state legislations[20]. Thus, a central policy question is whether there is a need for a federal mandate of inpatient coverage for breast cancer surgery, similar to the federal Newborns' and Mothers' Health Protection Act of 1996.
One argument for federal mandates is that they cover populations enrolled in the federal insurance programs (e.g., the Medicare and Medicaid) and employer-sponsored plans, which are largely exempted from state insurance regulation because of the federal Employee Retirement Income Security Act (ERISA). Similar to a previous report by Warren et al.[3], our study showed that the practice of outpatient breast cancer surgery, allegedly resulting from rising managed care influence, has spilled over to the care of elderly patients enrolled in the Medicare FFS plans. If outpatient breast cancer surgery does inflict harmful consequences on patients, as the opponents have suggested, mere state mandated-benefit laws, currently available in more than 20 states[10], may not adequately protect elderly patients enrolled in the Medicare FFS plans. In this regard, a federal mandate, such as the Breast Cancer Patient Protection Act of 2007[11], may be needed to extend the benefits covered in state mandates to ERISA-exempted populations residing in these states.
A second argument for federal mandates is that they extend benefits to populations residing in states without such state mandates. Our study showed that the passages of state mandated-benefit laws were seemingly unrelated to the prevalence of outpatient breast cancer surgery. For example, among the regions studied here, Connecticut had the lowest proportion of outpatient mastectomy at 2.3% during the 4 years before the passage of the law related to inpatient coverage for breast cancer surgery in 1997[10]. Utah, which has not yet passed a law[10], on the other hand, had the highest at 21.4% during the same 4-year period. More than 20 states have passed mandates of inpatient coverage for breast cancer surgery since 1997. Unless the trend of passing such state mandated-benefit laws continues, a federal mandate may be warranted.
There are, however, several arguments against the need for such a federal mandate. First, no definitive evidence exists that an outpatient breast cancer surgery results in worse quality and/or outcomes than does an inpatient surgery. It can be questioned whether a federal mandate should be passed to support a delivery setting which has not been shown to be superior to the alternative. Second, the effectiveness of such state mandated-benefit laws has not been fully understood. Two recent studies suggest that state “drive-through” delivery and breast cancer surgery laws may indirectly affect care received by populations enrolled in the plans not subject to state regulation[20],[21]. Furthermore, Dow et al.[20] found that the federal Newborns' and Mothers' Health Protection Act of 1996 (taking effect in 1998 after all states had passed outpatient delivery laws) had little effect on some ERISA-exempted populations.
There has been scant evidence on quality and outcomes of outpatient breast cancer surgery. More evidence is needed to better understand whether outpatient delivery of breast cancer surgery affects quality and outcomes of care. Lack of evidence on quality and outcomes for inpatient versus outpatient breast cancer surgery, in general, has been clouded the debates over mandated-benefit laws in the past[22],[23]. To better facilitate the public debates about state and federal mandated-benefit legislations, more evidence-based analyses of quality and outcomes of and careful monitoring of the trends in outpatient breast cancer surgery among various populations are needed in the future research.
Acknowledgments
This study used the linked SEER-Medicare database, produced and made available as a joint effort by the Applied Research Program, National Cancer Institute; the Office of Research, Development and Information, Centers for Medicare & Medicaid Services; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries. The SEER-Medicare analyses reported herein are the sole responsibility of the authors.
References
- 1.Case C, Johantgen M, Steiner C. Outpatient mastectomy: clinical, payer, and geographic influences [J] Health Serv Res. 2001;36(5):869–884. [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrante J, Gonzalez E, Pal N, et al. The use and outcomes of outpatient mastectomy in Florida [J] Am J Surg. 2000;179(4):253–259. doi: 10.1016/s0002-9610(00)00336-6. [DOI] [PubMed] [Google Scholar]
- 3.Warren JL, Riley GF, Potosky AL, et al. Trends and outcomes of outpatient mastectomy in elderly women [J] J Natl Cancer Inst. 1998;90(11):833–840. doi: 10.1093/jnci/90.11.833. [DOI] [PubMed] [Google Scholar]
- 4.Sinks LF, Zarfos KA. Notes from Connecticut: a surgeon's travail [J] Med Pediatr Oncol. 1998;31(2):105. doi: 10.1002/(sici)1096-911x(199808)31:2<105::aid-mpo11>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 5.Kroll SS. Drive-through mastectomy and breast reconstruction [J] Ann Surg Oncol. 2000;7(6):399–401. doi: 10.1007/s10434-000-0399-9. [DOI] [PubMed] [Google Scholar]
- 6.National Breast Cancer Coalition “Drive-through mastectomy: NBCC does not support the Breast Cancer Patient Protection Act”. Available at http://www.natlbcc.org/bin/index.asp?strid=722&depid=9 [Access July 18 2010].
- 7.Bian J, Krontiras H, Allison JJ. Outpatient mastectomy and breast reconstructive surgery [J] Ann Surg Oncol. 2008;15(4):1032–1039. doi: 10.1245/s10434-007-9762-4. [DOI] [PubMed] [Google Scholar]
- 8.Clinton WJ. State of the Union 1997 - February 4, 1997. Available at http://odur.let.rug.nl/∼usa/P/bc42/speeches/sud97wjc.htm [Accessed July 18, 2010].
- 9.The Breast Cancer Patient Protection Act of 1997, S.B. 249, 105th Cong., 1st Sess., Jan. 30, 1997
- 10.State Legislative Data Program Available at http://www.scld-nci.net/ [Accessed June 26, 2010].
- 11.The Breast Cancer Patient Protection Act of 2007, H.R. 758, 110th Cong., 1st Sess., Jan. 31, 2007
- 12.Warren JL, Klabunde CN, Schrag D, et al. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population [J] Med Care. 2002;40(8 Suppl):IV-3–IV-18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 13.Cooper GS, Viring B, Klabunde CN, et al. Use of SEER-Medicare data for measuring cancer surgery [J] Med Care. 2002;40(8 Suppl):IV-43–IV-43. doi: 10.1097/00005650-200208001-00006. [DOI] [PubMed] [Google Scholar]
- 14.Du X, Freeman JL, Warren JL, et al. Accuracy and completeness of Medicare claims Data for surgical treatment of breast cancer [J] Med Care. 2000;38(7):719–727. doi: 10.1097/00005650-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Nattinger AB, Laud PW, Bajorunaite R, et al. An algorithm for the use of Medicare claims data to identify women with incident breast cancer [J] Health Serv Res. 2004;39(6 Pt 1):1733–1749. doi: 10.1111/j.1475-6773.2004.00315.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation [J] J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases [J] J Clin Epidemiol. 1992;45(5):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 18.Bian J, Morrisey MA. HMO penetration, hospital competition, and growth of ambulatory surgery center [J] Health Care Financ Rev. 2006;27(4):111–122. [PMC free article] [PubMed] [Google Scholar]
- 19.White H. A heteroskedasticity-consistent covariate matrix estimator and a direct test for heteroskedasticity [J] Econometrica. 1980;48(4):817–838. [Google Scholar]
- 20.Bian J, Lipscomb J, Mello MM. Spillover effects of state mandated benefit laws: the case of outpatient breast cancer surgery [J] Inquiry. 2009–2010;46(4):433–447. doi: 10.5034/inquiryjrnl_46.4.433. [DOI] [PubMed] [Google Scholar]
- 21.Dow WH, Harris DM, Liu Z. Differential effectiveness in patient protection laws: what are the causes? An exmaple from the drive-through delivery laws [J] J Health Polit Policy Law. 2006;31(6):1107–1127. doi: 10.1215/03616878-2006-021. [DOI] [PubMed] [Google Scholar]
- 22.Kassirer JP. Practicing medicine without a license—the new instructions by Congress [J] N Engl J Med. 1997;336(24):1747. doi: 10.1056/NEJM199706123362409. [DOI] [PubMed] [Google Scholar]
- 23.Schauffler HH. Politics trumps science: rethinking state-mandated benefits [J] Am J Prev Med. 2002;19(2):136–137. doi: 10.1016/s0749-3797(00)00190-2. [DOI] [PubMed] [Google Scholar]