Abstract
In 2005, a program named “Early Detection and Early Treatment of Esophageal and Cardiac Cancer” (EDETEC) was initiated in China. A total of 8279 residents aged 40–69 years old were recruited into the EDETEC program in Linzhou of Henan Province between 2005 and 2008. Howerer, the cost-benefit of the EDETEC program is not very clear yet. We conducted herein a cost-benefit analysis of screening for esophageal and cardiac cancer. The assessed costs of the EDETEC program included screening costs for each subject, as well as direct and indirect treatment costs for esophageal and cardiac severe dysplasia and cancer detected by screening. The assessed benefits of this program included the saved treatment costs, both direct and indirect, on esophageal and cardiac cancer, as well as the value of prolonged life due to screening, as determined by the human capital approach. The results showed the screening cost of finding esophageal and cardiac severe dysplasia or cancer ranged from ¥2707 to ¥4512, and the total cost on screening and treatment was ¥13 115–¥14 920. The cost benefit was ¥58 944–¥155 110 (the saved treatment cost, ¥17 730, plus the value of prolonged life, ¥41 214–¥137 380). The ratio of benefit-to-cost (BCR) was 3.95–11.83. Our results suggest that EDETEC has a high benefit-to-cost ratio in China and could be instituted into high risk areas of China.
Keywords: Esophageal cancer, gastric cardiac cancer, screening, cost-benefit
Linzhou of Henan Province is a high-risk area of esophageal and cardiac cancer in China[1],[2]. In 2003, the incidence rate of esophageal cancer was as high as 73.2/105 [3], and its mortality rate was 59.6/105 [4], which was much higher than the mean mortality rate in China (15.04/105 [5]) between 2004 and 2005.
Esophageal cancer is usually fatal, with a very poor 5-year survival rate of 16% in the United States and only 10% in Europe[6],[7]. In China, the survival rate is less than 10% when diagnosed at an advanced stage but over 85% when detected at an early stage [8]–[10]. The main reason for the low survival rate is that most cases are asymptomatic and go undetected until they are at an advanced stage and no longer amenable to surgical resection. Clinical therapy for the advanced-stage esophageal cancer is very expensive and often causes a heavy disease burden for residents in rural high risk areas.
Previous studies have shown that the survival rates could be increased by early detection and early treatment of esophageal and cardiac cancer (EDETEC) [8],[11]–[13]; however, there are few published data evaluating the cost-benefit of the EDETEC, which is necessary to provide a scientific basis for continuing and extending the program.
The EDETEC program, funded by Chinese Central Financial Transfer Payment Program, has been conducted in Linzhou of Henan Province since 2005. We collected the screening and treatment costs of 8279 participants in EDETEC program in Linzhou between 2005 and 2008 to evaluate the cost-benefit of the EDETEC program, providing basic information for further generalization.
Materials and Methods
In our study, eligible population aged 40–69 years were screened by endoscopy with mucosal iodine staining in combination with index biopsies, and then diagnosed by pathology detection. For severe dysplasia/carcinoma in situ (SC/CIS) or intramucosal carcinomas (IC) found during screening, endoscopic mucosal resection (EMR) and/or argon plasma coagulation (APC) treatments were used as local therapies. For submucosal carcinoma (SC) and invasive carcinoma (IVC), therapies included esophagectomy, radiotherapy, and other conventional treatments.
The costs of EDETEC included screening and treatment costs. The benefits of screening comprised of two parts: the saved treatment costs from decreased incidence of esophageal and cardiac cancer at an advanced stage, as well as the value of prolonged expected life years resulting from EDETEC.
Costs of screening
The EDETEC program was conducted in Feicheng of Shandong Province, Linzhou of Henan Province, and Ci County of Hebei Province starting in 2005, with funding from the Chinese Central Financial Transfer Payment Program. The eligible population aged 40–69 years were screened by endoscopy with mucosal iodine staining in combination with index biopsies, and then diagnosed by pathology detection. Screening costs included the costs of the drugs, staff, supplies, equipment and facilities, and so on. The screening costs per capita were Ұ129.14 in Linzhou, Ұ133.62 in Ci County, and Ұ122.78 in Feicheng. Full details of each component are given in Table 1.
Table 1. Estimates of the screening cost per capita among Linzhou, Ci County and Feicheng.
| Item | Linzhou | Ci County | Feicheng |
| Endoscopy with mucosal Iodine staining combined with Index biopsy | |||
| Drugs | 20.20 | 20.30 | 20.35 |
| Supplies | 11.29 | 11.02 | 10.50 |
| Equipment and facilities | 53.69 | 46.89 | 35.98 |
| Staff | 10.68 | 17.45 | 18.95 |
| Other | 1.75 | 1.23 | 0.66 |
| Total | 97.61 | 96.89 | 86.44 |
| Histology and pathology detection | |||
| Supplies | 9.53 | 12.79 | 10.97 |
| Equipment and facilities | 10.94 | 7.18 | 9.26 |
| Staff | 9.74 | 16.15 | 15.86 |
| Other | 1.32 | 0.61 | 0.25 |
| Total | 31.53 | 36.73 | 36.34 |
| Total cost per capita | 129.14 | 133.62 | 122.78 |
Values are presented as cost, with a unit of RMB.
This analysis does not include the transportation costs (the screening location was within walking distance of the residential area), the costs of participants' time lost to screening (at most 2–3 h), the costs of adverse effects of screening (none was observed in our study), or administrative costs of the program. Because the total costs would be greater when considering the aforementioned excluded costs, the costs per capita were defined as ¥120, ¥130, ¥140, ¥150, and ¥200, for this study.
According to the proportion of SD/CIS and cancer in the screening group, the costs of finding each SD/CIS or cancer by screening could be calculated by formula (1):
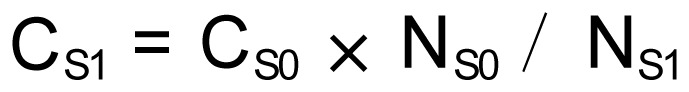 |
(1) |
In formula (1), CS1 denotes the mean screening cost of each SD/CIS or cancer detected; CS0 denotes screening cost of each participant in the screening group; NS0 denotes the number of participants in the screening group; and NS1 denotes the number of SD/CIS and cancer detected in the screening group.
Thus, the costs of EDETEC per capita could be estimated by formula (2):
 |
(2) |
In formula (2), C0 denotes the cost per capita of EDETEC; C1 denotes screening and treatment cost per capita of SD/CIS and cancer; NS1 denotes the numbers of SD/CIS and cancer in the screening group; and NS0 denotes the numbers of participants in the screening group.
Costs of treatment
Treatment costs included direct and indirect costs. Direct costs referred to medical costs, including drugs, disposable supplies, equipment and facilities, and staff, and non-medical costs, including transportation, accommodation, nutrition, etc. Indirect costs included the cost of time lost for both the patients and caregivers (their missed work days due to the disease), and it was calculated using the human capital approach (3):
 |
(3) |
In formula (3), CI denotes indirect costs (¥); D denotes the days for missed work; and G denotes annual Gross Domestic Production (GDP) per capita in Linzhou (¥).
In 2006, the annual GDP per capita of Linzhou was ¥13 738 based on data from the Statistics Bureau of Henan Province. We collected 161 cases of SD/CIS and cancer in Linzhou Cancer Hospital in 2008 and categorized them into two groups according to whether they were diagnosed by screening or not. We then calculated the treatment cost for each group. The treatment cost per capita of SD/CIS and cancer was ¥10 408 in the screening group and ¥21 058 in the non-screening group (Table 2).
Table 2. Treatment cost per capita in screening and non-screening groups.
| Treatment cost (¥) | Cost of initial treatment |
Cost of follow-up treatment |
Total cost |
|||
| Screening group | Non-screening group | Screening group | Non-screening group | Screening group | Non-screening group | |
| Direct cost | 5 845 | 10 127 | 601 | 1 380 | 6 446 | 11 507 |
| Medical cost | 5 179 | 8 420 | 544 | 1 244 | 5 723 | 9 664 |
| Non-medical cost | 666 | 1 707 | 57 | 136 | 723 | 1 843 |
| Indirect cost | 2 226 | 2 703 | 1 736 | 6 848 | 3 962 | 9 551 |
| Total | 8 071 | 12 830 | 2 337 | 8 228 | 10 408 | 21 058 |
Taking into account that only a certain proportion of SD/CIS would develop into symptomatic esophageal and cardiac cancer, a coefficient (A) should be set for further calculation. According to the literature and experts' opinions, the transition probability from SD/CIS to advanced cancer within 10 years ranges from 73.9% to 81.66%[14],[15], and the transition probability within 3.5 years ranges from 65.2% to 68.8%[16],[17]. Therefore, we defined A as 75%, which represented the transition probability from SD/CIS to advanced cancer over a lifetime. Intramucosal carcinoma (IC) or submucosal carcinoma (SC) would take a relatively short time to progress to invasive carcinoma (IVC), so we assumed that all the IC or SC would progress to IVC in 10 years. Therefore, if no screening program was conducted, the costs of treatment for SD/CIS and cancer (CT1) can be estimated as formula (4):
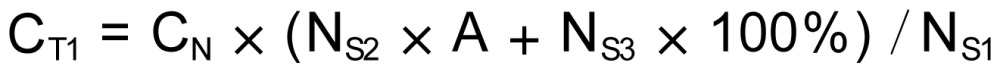 |
(4) |
In formula (4), CN denotes the mean treatment costs of each SD/CIS and cancer in the non-screening group (¥21 058); NS1 denotes the numbers of SD/CIS and cancer in the screening group; NS2 denotes the numbers of SD/CIS in the screening group; and NS3 denotes the numbers of IC and above in the screening group.
The benefits from prolonged life gained by early detection and treatment
The human capital approach was used to calculate the value of prolonged lifetime by formula (5):
 |
(5) |
In formula (5), B denotes benefit (¥); Y denotes prolonged years of life expectancy; and G denotes annual Gross Domestic Production (GDP) per capita in Linzhou (¥13 738).
The mean age of patients found by screening was 56 years old, and the mean age of patients in the non-screening group (seeking medical treatment by themselves) was 62 years old. Moreover, the mean life expectancy of the population of Linzhou in 2006 was 70.65 years. Accordingly, the life expectancy of the over 40-year-old group should be longer than 70.65 years.
Early studies have shown that 5-year survival rates could reach 90% or above by EDETEC, and survival time of patients with early stage (SD/CIS, IC, SC) cancer after esophagectomy was almost the same as that of healthy individuals, with a 5-year survival rate of 97.4%–100%[12],[18] and a 20-year survival rate as high as 50.9%[19].
For the non-screening group who sought medical treatment by themselves, the mortality rate of esophageal and cardiac cancer was 58% in the first year and reached 70% by the second year according to the 19 000-case cancer registry data of Yanting County. On the basis of the statistics above, if the life expectancy of patients was 70 or 71 years in the screening group (of which the mean age was 56 years old), then the remaining lifetime is 14 to 15 years. Additionally, the mean life expectancy of advanced esophageal and cardiac cancer in the non-screening group was about 2 years. Deducting 6 years for leading time bias, the mean expected additional life expectancy of the screening group was 6 to 7 years longer than that of the non-screening group. Therefore, for this study, the prolonged life was defined as 3 to 10 years considering the individual diversity of patients.
Results
Costs of early detection and treatment
In the EDETEC program, 8279 participants were screened among the eligible population aged 40–69 in Linzhou between 2005 and 2008. The number of cases of each stage of esophageal and cardiac cancer was as follows: 232 cases of SD/CIS; 76 cases of IC; 32 cases of SC; and 27 cases of IVC. Overall, 367 cases were diagnosed with esophageal and cardiac SD/CIS and cancer (251 cases of esophageal diseases and 116 of cardiac diseases).
On the basis of formula (1), the mean screening cost could be estimated in the range of ¥120 to ¥200, and the screening cost of finding a patient with SD/CIS and cancer was estimated. Then the costs of screening and treatment of patients with SD/CIS and cancer were estimated as shown in Table 3.
Table 3. Estimates of the screening and treatment costs per capita.
| Screening cost (¥) | Screening cost for per SD/CIS a and cancer (¥) | Screening and treatment costs b for per SD/CIS and cancer (¥) |
| 120 | 2 707(5 069) c | 13 115(15 477) |
| 130 | 2 933(5 491) | 13 341(15 899) |
| 140 | 3 158(5 914) | 13 566(16 322) |
| 150 | 3 384(6 336) | 13 792(16 744) |
| 200 | 4 512(8 448) | 14 920(18 856) |
a SD, severe dysplasia; CIS, carcinoma in situ; bTreatment cost per capita of SD/CIS and cancer of the screening group was ¥10 408; c Numbers in the parentheses only represent esophageal diseases.
Thus, the total cost per capita of SD/CIS and cancer was between ¥13 115 and ¥14 920 in the EDETEC program. On the basis of the statistics above, the cost of EDETEC per capita could be estimated by formula (2) and ranged from ¥581 to ¥661.
Calculations were as follows:
C0 min = 13 115 × 367/8279 = ¥581;
C0 max = 14 920 × 367/8279 = ¥661.
Benefits of the early detection and treatment
The benefits of EDETEC equal the sum of the savings from treatment costs and the value of prolonged expected life years. In this paper, the savings from treatment costs was equivalent to the treatment expenses of SD/CIS and cancer in the non-screening group, ¥21 058 per capita.
As mentioned above, a coefficient A, which represented the transition rate of SD/CIS to advanced cancer, was determined to be 75%, and the transition rate from IC or SC to advanced cancer was 100%. In other words, if EDETEC was not implemented, 75% of SD/CIS and 100% of IC and SC would transition into advanced carcinoma. According to formula (4), in the non-screening group, the treatment cost of SD/CIS and cancer was ¥17 730 per capita. Calculations were as follows:
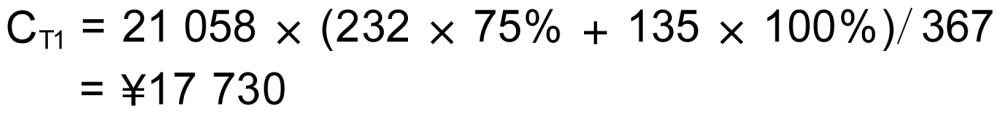 |
The value of CT1 was much greater than the screening and treatment costs of SD/CIS and cancer, which ranged from ¥13 115 to ¥14 920 per capita.
Assuming the prolonged life expectancy in the screening group was between 3 and 10 years per capita, the benefit calculated by formula (5) was ¥137 380. Calculations were as follows:
Bmin=13 738×3 = ¥41 214; Bmax=13 738×10 = ¥137 380
Therefore, the total benefits of early detection and early treatment could be estimated accordingly. More specifically, the benefits of each patient with SD/CIS and cancer discovered by the EDETEC program ranged from ¥58 944 to ¥155 110, and the benefits of each participant ranged from ¥2613 to ¥6876.
Cost-benefit analysis of screening
For the cost-benefit analysis, the per capita cost of screening was defined as ¥120, ¥150, or ¥200 for separate calculations, and the prolonged life expectancy was defined as 3 or 10 years. Thus, there were 6 ways for calculating the cost-benefit of SD/CIS and cancer. The outcomes of the cost-benefit analysis are shown in Table 4. BCRs of the EDETEC program ranged from 3.95 to 11.83, which showed that the EDETEC program had great benefits.
Table 4. Analysis of cost-benefit on EDETEC program.
| Scenarioa | Costs (¥) | Benefits (¥) | Benefit-cost ratio (BCR) |
| 1 | 13 115 | 58 944 | 4.49 |
| 2 | 13 115 | 155 110 | 11.83 |
| 3 | 13 792 | 58 944 | 4.27 |
| 4 | 13 792 | 155 110 | 11.25 |
| 5 | 14 920 | 58 944 | 3.95 |
| 6 | 14 920 | 155 110 | 10.37 |
a Numbers represent different combinations of screening cost and prolonged life expectancy: 1, screening cost per capita was ¥120, and prolonged life expectancy was 3 years; 2, screening cost per capita was ¥120, and prolonged life expectancy was 10 years; 3, screening cost per capita was ¥150, and prolonged life expectancy was 3 years; 4, screening cost per capita was ¥150, and prolonged life expectancy was 10 years; 5, screening cost per capita was ¥200, and prolonged life expectancy was 3 years; 6, screening cost per capita was ¥200, and prolonged life expectancy was 10 years.
Discussion
Linzhou of Henan Province is a high-risk area for esophageal cancer in China and is also an important site of the EDETEC program funded by the Chinese Central Financial Transfer Payment Program. By estimating the cost-benefit of the EDETEC program there, we could understand its effects in high-risk areas from a health economics perspective and use this knowledge to provide theoretical support for further generalization of the program. Our study directly compared inputs and outputs of the EDETEC program by converting them into money, which is easily understood and also makes it possible to obtain detailed and exact data for comparisons between different areas and programs.
One previous study in China, in which the costs of “esophageal traditional therapy” and “early detection and treatment for esophageal cancer” were evaluated, showed a BCR of 4, a number almost completely less than the range of BCRs found in our study (3.95–11.83)[20]. Furthermore, indirect costs were not considered in the “esophageal traditional therapy” of the previous study. In our study, both direct and indirect costs of treatment were included, which complements the disadvantages of the former study. Different levels of screening costs (from ¥120 to ¥200 per capita) were calculated, taking the economic levels of different sites into consideration. The natural progress of esophageal cancer was also considered, with the transition rate (A) from SD/CIS to IVC defined as 75%. Two different periods (3 or 10 years) were chosen when calculating prolonged life expectancy, considering the individual diversity of patients. All the indicators above were obtained from related literature and research as well as experts' opinions, which ensure the reliability of our results.
Our study showed that the costs of EDETEC for each patient with SD/CIS and cancer were between ¥13 155 and ¥14 920, and the saved treatment cost from reduced incidence was ¥17 730 per capita. These benefits were in addition to prolong life expectancy, which increased productivity values. Therefore, the EDETEC program is cost-efficient with a high benefit-to-cost ratio.
Compared to health economics evaluations of other diseases, we found that conducting screening for a specific disease resulted in higher benefit-to-cost ratios in high risk areas than in other areas. As a result, the screening in China, where the incidence rate of esophageal carcinoma is very high[21], should gain a high profit. Wang et al.[22],[23] demonstrated that in high risk areas for gastric cancer (incidence rates of 38.74/105), treatment costs could be significantly decreased by screening for Helicobacter pylori and treating precancerous lesions or early stages cancer. Moreover, screening in high risk areas will likely result in early detection and, therefore, a lower treatment cost or overall cost, which correlates to high economic efficiency. In 2003, the incidence rate of esophageal cancer in Linzhou was 73.2/105, much higher than that in other areas; thus, screening for esophageal cancer will be more economic and efficient in this area. Compared with screening costs of Wang's gastric cancer program and our program, the cost of finding one esophageal and cardiac SD/CIS or cancer was ¥2707, while the cost of finding one gastric cancer patient was ¥6623. As a result, screening in areas at high risk for esophageal cancer could result in fewer costs and more profits. In addition, the treatment cost of esophageal and cardiac SD/CIS and cancer in the non-screening group was ¥21 058 per capita, whereas costs ranged from ¥11 700 to ¥12 900 for gastric cancer. Therefore, early detection and early treatment of esophageal and cardiac cancer could cost less money, alleviate more disease burden, and provide more benefits than screening for gastric cancer. However, local situations (such as the incidence, financial condition, and so on) should be taken into account before extrapolating the results into other areas.
Some limitations of this study should be considered. To simplify the calculations, our estimates did not consider the growth of medical expenditures and the discount rate. According to a general analysis of health economics, the saved treatment costs for the next few years should be discounted from the current price. However, due to the growth of medical expenditures, the mean treatment costs for the next few years will be more than what they are currently. In this way, if the growth rate of medical expenditure is almost the same as the inflation rate, the increase will be counteracted by the discount rate. However, if the growth rate of medical expenditures is lower than the discount rate, our study may over-evaluate the benefits of screening. A similar situation exists when calculating the gained benefit from prolonged life expectancy. Regardless, due to the high benefit-to-cost ratios of the EDETEC program, even the discount would not significantly influence our conclusion.
In summary, by comparing the costs invested and health outputs of the EDETEC program in Linzhou, we conclude that the EDETEC program spent less, gained high profits, and decreased patients' medical expenditures and disease burdens. We recommend that the EDETEC program be extended to other high risk areas of China.
Acknowledgments
This work was supported by Key Projects in the National Science & Technology Pillar Program (No. 2006BAI02 A15).
References
- 1.Zhang SW, Chen WQ, Kong LZ, et al. An analysis of cancer incidence and mortality from 30 cancer registries in China, 1998–2002 [J] China Cancer. 2006;15(7):430–448. [in Chinese] [Google Scholar]
- 2.Cheng LP, Lian SY, Liu ZC, et al. An analysis of incidence and mortality with esophageal cancer from 1985 to 2002 [J] China Cancer. 2008;8(1):12–13. [in Chinese] [Google Scholar]
- 3.Zhang SW, Chen WQ, Kong LZ, et al. An annual report: cancer incidence in 35 cancer registries in China, 2003 [J] China Cancer. 2007;16(7):494–506. [in Chinese] [Google Scholar]
- 4.Chen WQ, Zhang SW, Kong LZ, et al. An annual report: cancer mortality in 35 cancer registries in China, 2003 [J] China Cancer. 2007;16(8):586–597. [in Chinese] [Google Scholar]
- 5.Yin L, Hu GC. The Leading ten malignant tumors in China from 2004 to 2005 [Z] Yearbook of health in the People's Republic of China. 2008 [in Chinese] [Google Scholar]
- 6.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006 [J] CA Cancer J Clin. 2006;56(2):106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 7.Sant M, Aareleid T, Berrino F, et al. EUROCARE-3: survival of cancer patients diagnosed 1990-94—results and commentary [J] Ann Oncol. 2003;14(5):v61–v118. doi: 10.1093/annonc/mdg754. [DOI] [PubMed] [Google Scholar]
- 8.Wang GQ, Jiao GG, Chang FB, et al. Long-term results of operation for 420 patients with early squamous cell esophageal carcinoma discovered by screening [J] Ann Thorac Surg. 2004;77(5):1740–1744. doi: 10.1016/j.athoracsur.2003.10.098. [DOI] [PubMed] [Google Scholar]
- 9.Shao LF, Chen MY. The Recent status of the surgical treatment of the esophageal carcinoma[J] Chin J Gastrointest Surg. 1998;1(2):70–71. [in Chinese] [Google Scholar]
- 10.Shao LF, Gao ZR, Xu JL, et al. The summary on surgical treatment for esophageal and cardiac carcinoma in 15707 cases [A] Proceedings of the 1st International Conference on Esophageal Cancer and the 7th Chinese Conference on Esophageal Cancer. 2005:40–46. [in Chinese] [Google Scholar]
- 11.Yoshida M, Hanashi T, Momma K, et al. Endoscopic mucosal resection for radical treatment of esophageal cancer [J] Gan to Kagku Ryoho. 1995;22(7):847–854. [PubMed] [Google Scholar]
- 12.Wang GQ. 30-year Experiences on early detection and treatment of esophageal cancer in high risk areas [J] Acta Academiae Medicinae Sinicae. 2001;23(1):69–72. [in Chinese] [PubMed] [Google Scholar]
- 13.Shao LF, Gao ZR, Li ZC, et al. Long-term consequences of surgical resection on early esophageal and gastric cardia carcinoma in 204 cases [J] Chin J Surg. 1993;31(3):131–133. [in Chinese] [PubMed] [Google Scholar]
- 14.Chen ZF, Wang GQ, Hou J, et al. Follow-up results of esophageal squamous severe dysplasia in 158 cases [J] Chin J Clin Oncol. 2004;31(6):306–308. [in Chinese] [Google Scholar]
- 15.Wang GQ, Abnet CC, Shen Q, et al. Histological precursors of esophageal squamous cell carcinoma: results from a 13 year prospective follow up study in a high risk population [J] Gut. 2005;54(2):187–192. doi: 10.1136/gut.2004.046631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dawsey SM, Lewin KJ, Wang GQ, et al. Squamous esophageal histology and subsequent risk of squamous cell carcinoma of the esophagus [J] Cancer. 1994;74(6):1686–1692. doi: 10.1002/1097-0142(19940915)74:6<1686::aid-cncr2820740608>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 17.Wang GQ, Qiao YL. Research on precancerous—key of esophageal carcinoma control [J] Cancer Res Clin. 2003;15(1):3–4. [in Chinese] [Google Scholar]
- 18.Wang GQ, Hao CQ, Wei WQ. Long-term survival rate of precancerous lesions and early esophageal cancers after endoscopic mucosal resection [J] Chin J Digest Endosc. 2008;25(11):584–586. [in Chinese] [Google Scholar]
- 19.Shen Q, Wang DY, Xing YY, et al. Esophageal balloon cytology in China: a 30-year review [J] Acta Cytol. 1998;42(Suppl):566. [Google Scholar]
- 20.Liu ZR, Wei WQ, Huang YQ. Economic evaluation of early detection and treatment of esophageal cancer [J] Chin J Cancer. 2006;25(2):200–203. [in Chinese] [PubMed] [Google Scholar]
- 21.Parkin DM, Bray F, Ferlay J, et al. Global Cancer Statistics, 2002 [J] CA Cancer J Clin. 2005;55(2):74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 22.Wang Q, Jin PH, Lin GW, et al. Cost-effectiveness of helicobacter pylori screening to prevent gastric cancer: markov decision analysis [J] Chin J Epidemiol. 2003;24(2):135–139. [in Chinese] [PubMed] [Google Scholar]
- 23.Wang Q, Jin PH, Lin GW, et al. Cost-effectiveness of population-based Helicobacter pylori screening to prevent gastric cancer [J] World Chin J Digestol. 2000;8(3):262–265. [in Chinese] [Google Scholar]


