Abstract
Complex sleep apnea syndrome (CompSAS) is characterized by predominant obstructive sleep disordered breathing with evolution of central disordered breathing following exposure to nasal continuous positive airway pressure (CPAP) therapy in obstructive sleep apnea (OSA) patients. We report a case of CompSAS associated with use of a nasal expiratory positive airway (nEPAP, Provent) device. We therefore recommend obtaining objective sleep data to confirm treatment effectiveness of the nEPAP device for OSA prior to long-term prescription. Further research is warranted to understand the underlying pathophysiological mechanisms and risk factors associated with CompSAS.
Citation:
Chopra A, Das P, Ramar K, Staats B, St Louis EK. Complex sleep apnea associated with use of nasal expiratory positive airway (nEPAP) device. J Clin Sleep Med 2014;10(5):577-579.
Keywords: nasal expiratory positive airway, complex sleep apnea syndrome, obstructive sleep apnea
Complex sleep apnea syndrome (CompSAS) refers to emergence of central apnea events (CAI > 5) upon treatment with CPAP in patients with OSA.1 The etiopathology of CompSAS is controversial and the underlying mechanisms potentially include abnormalities of both upper airway resistance and central nervous system ventilatory control.2 CompSAS patients typically have fragmented sleep with elevated arousal indices and repetitive desaturations that could pose health risk, thereby requiring prompt recognition and treatment with modalities such as adaptive servo-ventilation (ASV) therapy.3 To our knowledge, we report the first case of CompSAS associated with Provent (Ventus Medical, Belmont, CA, USA), a nasal expiratory positive airway (nEPAP) device, which is a treatment alternative for a subset of OSA patients.4
REPORT OF CASE
A 72-year-old Caucasian man with a past history significant for mitral valve prolapse and left nasal septal deviation presented for sleep evaluation due to supine snoring without witnessed apneas, snort or gasp arousals. He denied excessive daytime sleepiness and his Epworth Sleepiness Scale (ESS) score was 3. The remainder of the sleep history was essentially negative.
His medications included warfarin and paracetamol. He had a remote 10 pack-year history of smoking and reported rare alcohol use. Physical exam was significant for BMI of 24 kg/m2, neck circumference of 37 cm, Friedman stage III tongue palate position, and left nasal septal deviation. Electrocardiogram showed sinus bradycardia, and echocardiogram revealed normal left ventricular size and function with an ejection fraction of 57%, mild right ventricular enlargement with normal systolic function, trivial tricuspid valve regurgitation, and bileaflet mitral valve prolapse with mild regurgitation.
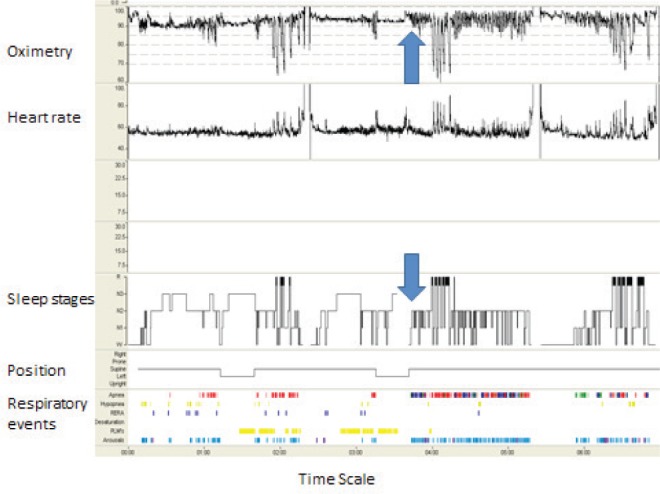
The patient underwent split-night polysomnography (PSG) and chose to use Provent due to his strong aversion to CPAP use. The diagnostic part of the split-night PSG revealed supine-dependent obstructive apneic events (Figure 1) suggestive of moderately severe OSA with an apnea-hypopnea index (AHI) of 18/h (Table 1). With Provent use during second half of the night, the patient developed CompSAS response with frequent mixed (17/h) and central (11/h) apneic events (Figure 2), with an overall AHI of 48/h (Table 1). Figure 3 represents the hypnogram for the study with initiation of Provent at 1:30:08 AM.
Figure 1. Presence of obstructive apneas apneic events during the diagnostic PSG (5-min window).
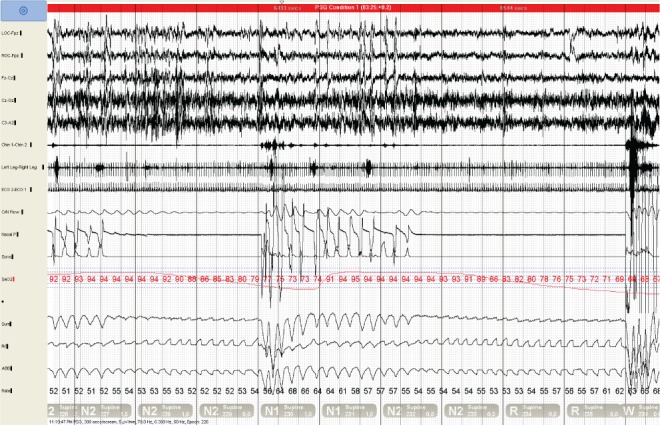
Table 1.
Polysomnography data.
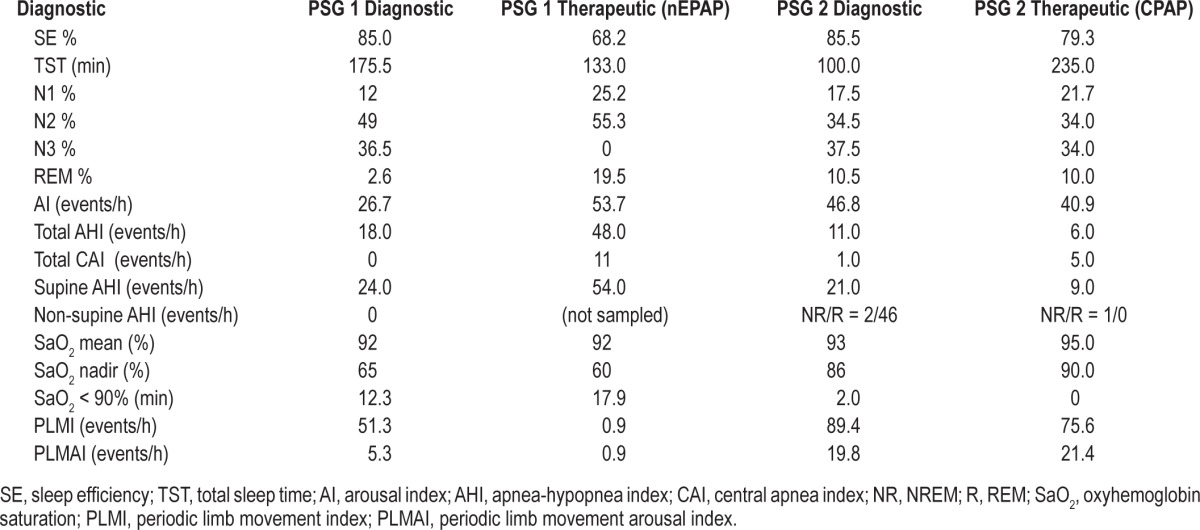
Figure 2. Development of complex sleep apnea with Provent use (5-min window).
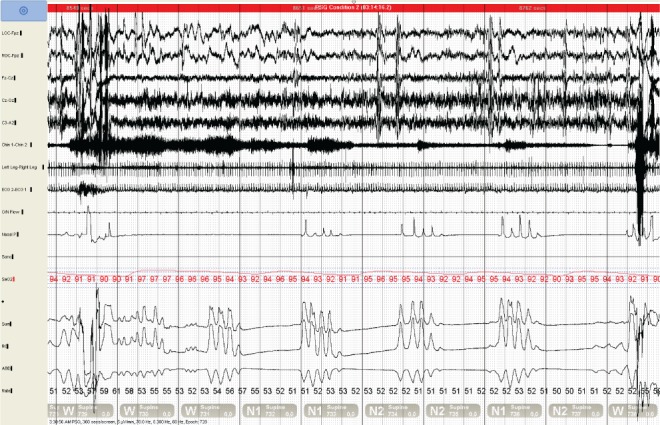
Figure 3. Hypnogram with initiation of Provent device (arrow).
At this time, the patient declined further treatment and was lost to follow-up until he presented again one year later with persistent symptoms of snoring and disturbed sleep continuity. Subsequent split-night polysomnogram again demonstrated a CompSAS response during nasal CPAP titration with a central apnea index of 5/hour. The patient disliked CPAP and given the minimal disordered breathing in the lateral sleep position, it was recommended that he utilize positional therapy.
DISCUSSION
Provent, a nasal expiratory positive airway (nEPAP) device, is applied to each nostril with an adhesive to provide a seal. The nEPAP contains a mechanical valve with a very low inspiratory resistance but a high expiratory resistance that results in positive pressure application throughout exhalation, resulting in the upper airway being more resistant to collapse on subsequent inspiration.4 Additionally, the presence of mild hypercapnia secondary to hypoventilation induced by the expiratory resistance of the nEPAP, may result in an increased respiratory drive to stent open the upper airway.4
CompSAS associated with non-PAP therapies has been reported in patients with tracheostomy, maxillofacial surgery, nasal surgery to relieve obstruction and mandibular advancement devices for OSA treatment,5–9 although the occurrence of this phenomenon seems to be rare. Our patient developed CompSAS with use of both nEPAP and CPAP devices, more severe with the nEPAP device during the supine position, highlighting the importance of obtaining objective sleep data prior to long-term prescription of a nEPAP device for treatment of OSA. Further research is warranted to understand the underlying pathophysiological mechanisms and risk factors associated with CompSAS.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Gilmartin GS, Daly RW, Thomas RJ. Recognition and management of complex sleep-disordered breathing. Curr Opin Pul Med. 2005;11:485–93. doi: 10.1097/01.mcp.0000183061.98665.b0. [DOI] [PubMed] [Google Scholar]
- 2.Kuźniar TJ, Morgenthaler TI. Treatment of complex sleep apnea syndrome. Chest. 2012;142:1049–57. doi: 10.1378/chest.11-3223. [DOI] [PubMed] [Google Scholar]
- 3.Allam JS, Olson EJ, Gay PC, Morgenthaler TI. Efficacy of adaptive servoventilation in treatment of complex and central sleep apnea syndromes. Chest. 2007;132:1839–46. doi: 10.1378/chest.07-1715. [DOI] [PubMed] [Google Scholar]
- 4.Berry RB, Kryger MH, Massie CA. A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: a randomized controlled trial. Sleep. 2011;34:479–85. doi: 10.1093/sleep/34.4.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fletcher EC. Recurrence of sleep apnea syndrome following tracheostomy. A shift from obstructive to central apnea. Chest. 1989;96:205–9. doi: 10.1378/chest.96.1.205. [DOI] [PubMed] [Google Scholar]
- 6.Corcoran S, Mysliwiec V, Niven AS, Fallah D. Development of central sleep apnea after maxillofacial surgery for obstructive sleep apnea. J Clin Sleep Med. 2009;5:151–3. [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstein C, Kuźniar TJ. The emergence of central sleep apnea after surgical relief of nasal obstruction in obstructive sleep apnea. J Clin Sleep Med. 2012;8:321–2. doi: 10.5664/jcsm.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avidan AY, Guilleminault C, Robinson A. The development of central sleep apnea with an oral appliance. Sleep Med. 2006;7:187–91. doi: 10.1016/j.sleep.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Kuźniar T, Kovačević-Ristanović R, Freedom T. Complex sleep apnea unmasked by the use of a mandibular advancement device. Sleep Breath. 2011;15:249–52. doi: 10.1007/s11325-010-0459-8. [DOI] [PubMed] [Google Scholar]


