Abstract
Study Objectives:
To survey Advanced Practice Registered Nurse (APRN) and Physician Assistant (PA) utilization, roles and educational background within the field of sleep medicine.
Methods:
Electronic surveys distributed to American Academy of Sleep Medicine (AASM) member centers and APRNs and PAs working within sleep centers and clinics.
Results:
Approximately 40% of responding AASM sleep centers reported utilizing APRNs or PAs in predominantly clinical roles. Of the APRNs and PAs surveyed, 95% reported responsibilities in sleep disordered breathing and more than 50% in insomnia and movement disorders. Most APRNs and PAs were prepared at the graduate level (89%), with sleep-specific education primarily through “on the job” training (86%). All APRNs surveyed were Nurse Practitioners (NPs), with approximately double the number of NPs compared to PAs.
Conclusions:
APRNs and PAs were reported in sleep centers at proportions similar to national estimates of NPs and PAs in physicians' offices. They report predominantly clinical roles, involving common sleep disorders. Given current predictions that the outpatient healthcare structure will change and the number of APRNs and PAs will increase, understanding the role and utilization of these professionals is necessary to plan for the future care of patients with sleep disorders. Surveyed APRNs and PAs reported a significant deficiency in formal and standardized sleep-specific education. Efforts to provide formal and standardized educational opportunities for APRNs and PAs that focus on their clinical roles within sleep centers could help fill a current educational gap.
Citation:
Colvin L, Cartwright Ann, Collop N, Freedman N, McLeod D, Weaver TE, Rogers AE. Advanced practice registered nurses and physician assistants in sleep centers and clinics: a survey of current roles and educational background. J Clin Sleep Med 2014;10(5):581-587.
Keywords: advanced practice registered nurse, physician assistant, nurse practitioner, sleep disorders, sleep center, role, utilization, scope of practice, sleep
Nurse practitioners (NPs), and Physician Assistants (PAs) have been providing care since the 1960s.1,2 There are approximately 200,000 NPs and PAs currently practicing in the United States; approximately 56% are NPs and 44% are PAs.3 NPs are the largest group of Advanced Practice Registered Nurses (APRNs) comprising 58% of APRNs.4 By 2025, estimates indicate that the numbers of PAs and NPs will increase by 74% and 94% respectively.5,6 Just under half (49%) of all physicians' offices, and 41% of medical specialty practices, employ at least one NP, PA or certified nurse midwife(CNM).7 There are approximately one tenth the number of CNMs compared to NPs.4 The number of PAs and NPs is expected to increase overall with the increased demands associated with the implementation of the Affordable Care Act.8
There are no published data regarding APRNs and PAs within sleep centers. To date, knowledge of their numbers, utilization, and roles, as well as their educational background pertaining to sleep medicine, have been limited to anecdotal accounts.
APRN and PA Overview
From the patient perspective, the roles of the APRN and PA within a sleep center can be quite similar; their educational programs prepare them to provide clinical assessment, diagnosis, and treatment of patients. However, the scope of practice of the NP versus PA in the clinical setting may be affected by differences in educational backgrounds, state licensure, physician oversight, prescriptive authority, and reimbursement issues.
The term, APRN, refers to nurses with specialized training for providing direct care to individuals at an advanced level.9 APRNs are categorized into 4 groups, the clinical nurse specialist (CNS), certified registered nurse anesthetist (CRNA), certified nurse midwife (CNM), and nurse practitioner (NP). NPs are the most common sub-group of APRNs.4 Although the terms, NP and APRN, often are used interchangeably, this use is incorrect; all NPs are APRNs, but not all APRNs are NPs. There is some historical overlap, however variations exist between CNSs and NPs, particularly related to education and training in pharmacology, diagnosis, and treatment. Because of these differences, NPs generally have prescriptive authority while CNSs do not. Specialties for NPs often are determined by population (eg: adults) or work environment (eg: acute care).10 Examples of specialties that may be seen within sleep practices include Acute Care NP (ACNP), Adult NP (ANP), Family Practice NP (FNP), Pediatric NP (PNP), and Psychiatric/Mental Health NP (PMHNP).10 National efforts are underway to standardize APRN educational requirements, professional titles, areas of clinical practice, and state regulation.9
NP programs generally focus on a specific population (eg: pediatrics or adults), with the exception of training for FNPs which covers the lifespan. The NP clinical setting is determined by the area of specialty and may either focus on one setting (eg: outpatient) or multiple settings. PA educational programs include various clinical environments in both inpatient and outpatient settings for all age ranges.
Educational programs for APRNs are typically a blend of nursing and medical models, while PA programs are based exclusively on a medical model. The undergraduate education for APRNs prepares them for licensure as a registered nurse while the undergraduate education for PAs is typically in a health-related field. In general, NPs and PAs can perform health histories and physical examinations, order and interpret appropriate testing for further assessment and develop a treatment plan for patients with common health problems. Basic tests, such as laboratory testing, can be interpreted by a PA or NP. In certain clinical settings, other testing such as electrocardiography or x-rays may also may be reviewed or interpreted by a NP or PA. Additionally, any testing, which includes a physician review and interpretation, may be utilized in their assessments (eg: sleep studies). APRNs and PAs can prescribe therapeutics including pharmacologic agents and durable medical equipment. The extent of APRN and PA formal education in pharmacology and prescribing can affect state legislation regarding the degree of prescriptive authority. Within the sleep specialty, controlled-substance prescribing is a commonly encountered prescriptive limitation resulting from either state- or federal-level regulation relating to the scheduled classification of the medication.11
Any drug that utilizes a central pharmacy (eg: sodium oxybate) must adhere to prescribing and dispensing rules for the state in which the central pharmacy is located, affecting prescribing by a provider when practicing in other states if the rules differ.
APRN organizations and the American Association of Colleges of Nursing have recommended that the doctoral degree (either a Doctorate in Philosophy [PhD] or Doctorate of Nursing Practice [DNP]) be the minimum level of education required for certification by 2015.9,12 The PhD provides preparation with a focus on research while the DNP provides a clinically focused doctoral degree, focusing on evidence-based advanced nursing practice. PA programs have a target date of 2020 to award a master's degree as the minimum level of education to maintain national program accreditation.13 The American Academy of Nurse Practitioners (AANP) estimates that 98% of their members surveyed have a graduate degree and 14.6% have a doctoral degree (AANP personal communication).14 The American Academy of Physician Assistants estimates that 72% of clinically practicing PAs have a master's degree, 5% have a doctoral degree or a graduate certificate, and 20% have a bachelor's degree.15
Many factors besides educational background influence the scope of practice for APRNs and PAs.9,16 State “licensure” is probably the most obvious determinant with wide variation; some states choose to narrowly define scope of practice, while others approach it broadly. In some states, the authorization to practice does not come through licensure, but rather through other regulatory processes referred to as recognition, registration, or certification.9,16 In general, PA oversight is through the state medical board17 while APRN oversight is by the board of nursing.9 State oversight may include medication prescribing, restricted geographic location, and physician supervision or collaboration with APRN and PA practice.9,16 Additionally, state educational requirements ultimately determine what the minimum degree is for practice recognition within a state. APRN practice models can vary from independent practices to physician-collaborative practices while PA practices require physician supervision. State and federal regulatory agencies also can influence APRN and PA practices through their policies on controlled-substances prescribing, ordering therapeutic devices such as durable medical equipment and reimbursement of services.11,18,19 Employer or healthcare facilities further can influence the APRN or PA scopes of practice through internal policies.
As part of the licensure process, each state board determines the minimum standard for formal educational preparation and whether or not national certification is required to practice within the state. For APRNs, the majority of states require graduate- level education and/or national certification to practice20,21 while a small number of states require master's-level education as a minimum requirement for practice as a PA.22
Both APRNs and PAs have national organizations that determine standards for competency and educational preparation.13,23 PAs have one examination,24 whereas, NPs take specialty-specific certification examinations.10 Both disciplines require maintenance of a clinical practice and the completion of continuing education and professional-development activities for recertification. PAs and APRNs are allowed to use physician-level credits to meet their continuing education requirements; although, APRNs may need a portion of their credits to be earned from approved nursing organizations at an advanced practice level.10,25
There are a growing number of post-graduation PA-residency training programs, primarily in emergency medicine and surgery, and PAs can take optional specialty certification exams offered by the National Commission on Certification of Physician Assistants.25 In addition, both APRNs and PAs may be eligible for subspecialty certifications that reflect advanced levels of preparation (eg: advanced diabetes management certification)26 or more general levels of preparation (eg: asthma educator)27 administered by multidisciplinary professional organizations.
No formal training or certification in sleep medicine currently exists for APRNs or PAs. As the push towards formal education and greater specialty training increases, having specialty certifications in sleep for APRNs and PAs may become desirable; anecdotal reports suggest that some state boards are requesting additional proof of knowledge (continuing education) and competency in cases in which APRNs and PAs hold positions that exceed the education and training obtained during their initial formal education (eg: a family nurse practitioner working in a sleep center).
Finally, the terminology used to refer to these professional groups can be confusing to other disciplines. For example, there are a number of terms used to identify APRNs and PAs as one group. The Drug Enforcement Agency (DEA) uses the term mid-level provider (MLP), The Centers for Medicare and Medicaid (CMS) uses the term non-physician practitioner (NPP), but there is no term that has been defined and supported by both APRN and PA professional organizations. Although the term Advanced Practice Nurse (APN) has been used by some healthcare professionals to refer to an APRN, Advance Practice Registered Nurse is the term endorsed by the APRN consensus statement9 and the recent Institute of Medicine report.28
METHODS
Formation of the Task Force
In 2011, the AASM created an inter-professional Task Force composed of sleep physicians, advanced practice nurses and physician assistants practicing in the field of sleep to explore utilization, role definition and scope of practice of APRNs and PAs practicing at sleep centers, describe APRN and PA education and determine educational needs with regards to sleep medicine.
Survey of AASM Member Centers (Survey 1)
The Task Force electronically surveyed three groups: AASM member centers, the APRNs and PAs associated with these centers, and the APRNs and PAs who attended a dedicated educational course. The first survey (Survey 1) developed by the AASM APRN/PA Task Force queried AASM member centers about their practices. It asked 14 questions that included basic respondent contact information, sleep center structure, utilization of APRNs or PAs and very basic information on roles, and why the center representatives did or did not utilize an APRN or PA. Additionally, these centers formed the sample for initial contact with the second survey (Survey 2, Part 1). Privacy regarding provider-specific information was protected by not requesting direct contact information for the APRN or PA within their centers from the center representatives. After approval by the AASM Board of Directors, this questionnaire was distributed electronically to 1,950 AASM accredited sleep disorders centers, utilizing the email addresses provided in their AASM membership applications. There were 271 respondents (14%) to this initial electronic survey. Those representatives completing the survey included a variety of roles such as physicians, technical managers, and office managers, as well as APRNs or PAs (n = 15).
Survey of APRNs and PAs in AASM Member Sleep Centers (Survey 2, Part 1)
To obtain more information directly from APRNs and PAs about their sleep practices, a second survey was developed and approved by the AASM Board of Directors. This more detailed survey included questions about their roles, clinical focuses, educational levels, and educational opportunities in sleep medicine.
The instructions specifically asked that APRNs and PAs complete the survey describing their own roles within their sleep centers.
An invitation to participate in the second survey was sent electronically to the 245 AASM member center representatives who agreed to subsequent contact by the Task Force during the summer of 2012. These individuals were asked to forward the invitation to complete the electronic survey to the APRNs and PAs within their sleep centers. Thirty-one responses were received with one incomplete questionnaire (97% incomplete) and one duplicate questionnaire, leaving 29 responses for analysis (12%). For the duplicate respondent, the first set of responses received was analyzed.
Survey of APRNs and PAs in Clinical Practice (Survey 2, Part 2)
After reviewing the survey responses to the second survey, the Task Force sought to obtain information from more APRNs and PAs in an effort to have broader representation of national trends, especially since only 20 states were represented in initial response to Survey 2. During the fall of 2012, the AASM hosted an educational workshop designed for PAs and NPs at their national office in Darien, Illinois. Primarily marketed by the AASM through brochures and emails to members, the workshop was also promoted through word of mouth and internet searches, according to participant feedback. Course participants were asked to complete the same electronic questionnaire distributed to APRNs and PAs previously (Survey 2, Part 1), their responses becoming the second part of the data collected (Survey 2, Part 2). Even though the group who received invitations to participate was much smaller than Part 1, the response rate was significantly higher, more than doubling the responses to Survey 2. There were 44 responses to the survey, which accounted for 62% of the total number of attendees, but included 4 duplicate respondents from Part 1. Although the course was advertised specifically to PAs and NPs, other healthcare professionals attended (e.g., dentists, and physicians). Questionnaires completed by other professions despite instructions that the survey was intended for APRNs and PAs, were removed from the analysis (4 were removed). Excluding duplicates and non-APRN/non-PA respondents, 36 responses were included in the analysis (61% of the total number of APRNs and PAs in attendance).
Of the participants in Survey 2 Part 2 (n = 36), 52% chose sleep as their primary clinical interest, while the other participants chose interests from a list provided which reflected physician specialties commonly found within sleep practices; these included pulmonary, neurology, internal medicine, psychiatry, otolaryngology, pediatrics, and family practice. These data were not collected for Survey 2, part 1. Although all participants in Survey 1 and Part 1 of Survey 2 had an affiliation with an AASM member center, not all participants in Part 2 of Survey 2 were affiliated with an AASM member center.
Almost all respondents provided their name (on a voluntary basis) and other requested demographic information. When these demographics were not provided, there were sufficient responses regarding state, credentials, and institutions to allow the Task Force members to identify and exclude duplicate responses. For duplicate responses, the first set of responses submitted was utilized for analysis. When asked about clinical responsibilities, four APRNs and one PA did not provide a response and were excluded, leaving 60 for this portion of the analysis.
RESULTS
Survey of AASM Member Centers (Survey 1)
Table 1 provides an overview of responses from 271 sleep center representatives. Centers averaged 6.4 ± 4.5 beds, with five centers reporting more than 20 beds. The majority of the practices were hospital-based or nonhospital-based physician-owned practices. Practices employed on average 3.4 ± 3.3 physicians.
Table 1.
Survey 1 Responses from 271 AASM Member Centers
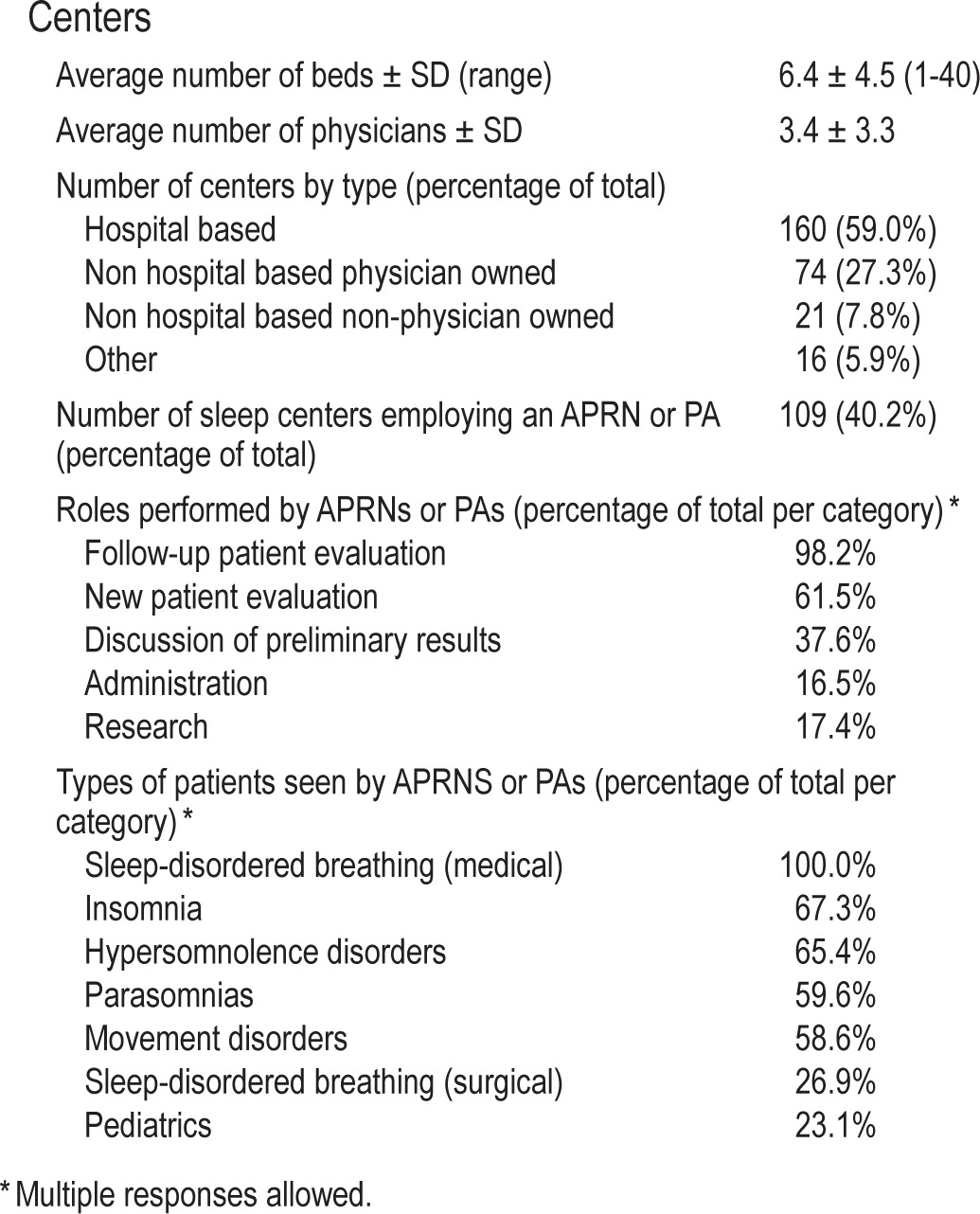
Slightly less than half of these AASM member centers (40%) employed an APRN or PA. Among the 109 centers reporting the employment of an APRN or PA, a majority reported the APRNs or PAs had clinical responsibilities providing new and follow-up evaluation, while less than half reported research or administrative responsibilities.
When the AASM member center representatives were asked if they were interested in hiring an APRN or PA, 29% of the respondents indicated there was an interest in hiring an APRN or PA, while 35% reported there was not an interest in hiring an APRN or PA, and the remaining 36% did not answer the question. Respondents were asked to comment on considerations for hiring an APRN or PA. Those comments can be broadly categorized as: (1) reimbursement issues, (2) costs associated with salaries, (3) difficulties associated with finding APRNs and PAs with training in sleep medicine, and (4) concerns about patient and/or physician acceptance of APRNs and PAs.
Survey of APRNs and PAs in Sleep Centers and in Clinical Practice (Survey 2, Parts 1 and 2)
Table 2 provides an overview of the 65 respondents to Survey 2, Parts 1 and 2. As expected, a high percentage of APRN and PA respondents to both parts of Survey 2 were prepared at the master's level or doctoral level (89%). Only one respondent reported receiving specialty training in sleep during their graduate program; whether this specialty training was clinical experience or coursework was not ascertained. Most of the respondents (86%) indicated that they received the majority of their training “on-the-job” from a physician.
Table 2.
Survey 2 APRN and PA Demographics.
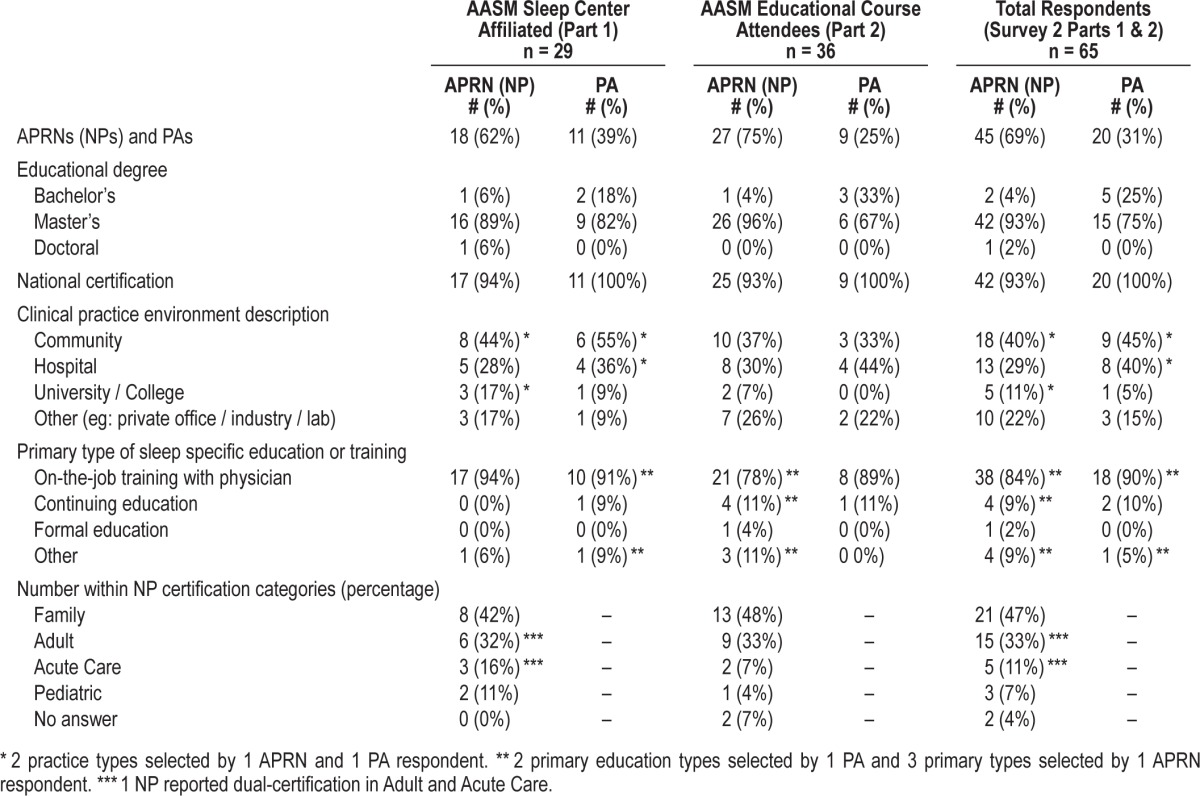
All of the APRNs reported NP certification, with the majority being certified as Family Nurse Practitioners (47%) or Adult Nurse Practitioners (33%). Smaller numbers reported being certified as Acute Care Nurse Practitioners (11%) or Pediatric Nurse Practitioners (7%). APRNs responding to Survey 2 represented 26 states, while the PAs responding to Survey 2 lived in 13 states.
Almost three-fourths (74%) of APRNs and PAs responding to the two surveys reported working at community- or hospital-based centers. Almost all (91%) of the APRNs and PAs reported spending at least 75% of their time in a clinical role with 82% reporting at least 90% in a clinical role; only 3% reported less than 50% of time in a clinical role. Proportions were similar between the 2 groups responding to Survey 2. When questioned about nonclinical roles, respondents selected research, administrative and community outreach via educational activities from the provided list.
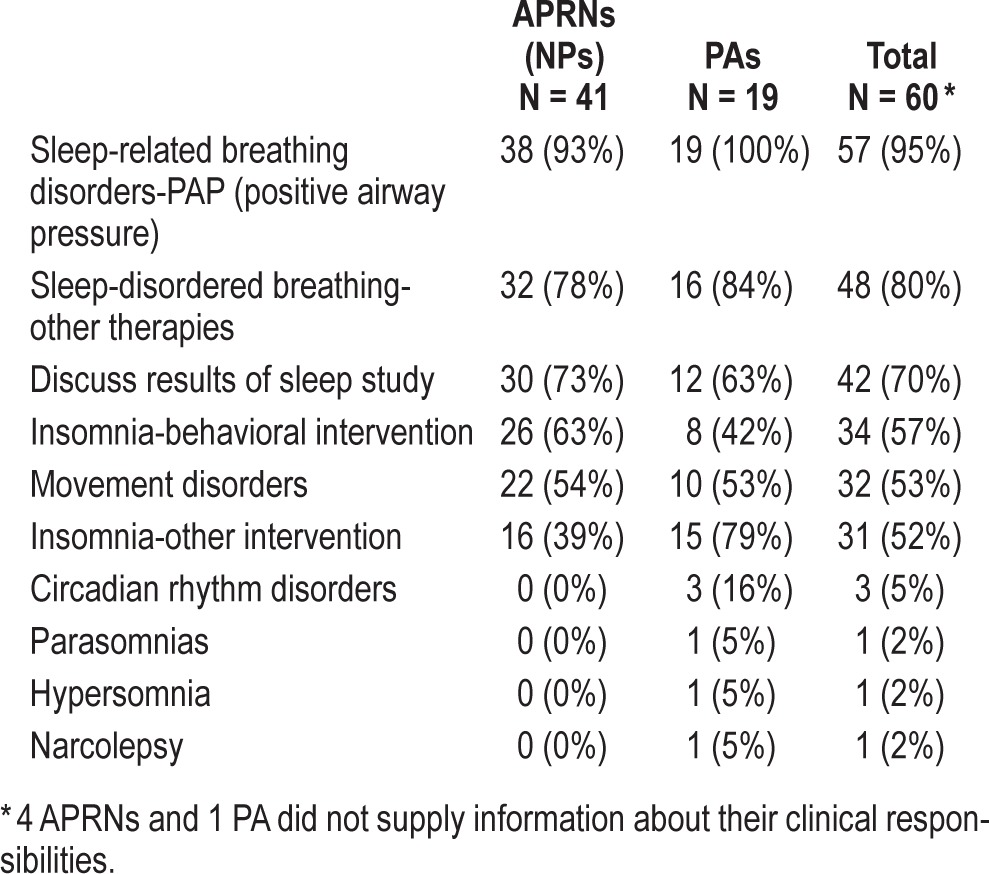
As shown in Table 3, a majority of APRNs and PAs reported regularly managing patients with sleep-related breathing disorders, insomnia, and/or movement disorders, as well as discussing sleep-study results with patients. A small number indicated routinely performing services for parasomnias, narcolepsy and/or hypersomnia, and circadian rhythm disorders. Based on the survey format, we were unable to ascertain if the small numbers reflected the overall lower numbers of these disorders in sleep-center patient populations or reflected a focus on other disorders by APRNs and PAs. APRNs and PAs were queried on their clinical services provided for insomnia using both behavioral and “other” interventions. PAs were more likely to report using interventions that were not behavioral interventions for insomnia than APRNs (X2 [1, N = 60] = 6.765, p = 0.0046). There were no other differences in clinical services reported by APRNs and PAs. The majority of APRNs and PAs (67%) reported that they could bill under their own National Prescriber Identity (NPI) number for more than half of their insurers, while approximately a quarter (26%) reported they did not know if they could bill under their own NPI, and four (6%) did not answer the question.
Table 3.
Clinical Services Routinely Provided by APRNs and PAs in Sleep Centers or Clinics
DISCUSSION
As new models are being considered by AASM for the delivery of care for patients with sleep disorders, understanding the contributions and the roles APRNs and PAs can play as members of the sleep team is essential. These needs were highlighted in a recent editorial by AASM President, Dr. Badr,29 regarding future models of care and the changes affecting the practice of sleep medicine, which include out-of-center sleep testing, a sharpening focus on chronic disease management, and the potential reduction in sleep-boarded physicians. His discussion included the importance of understanding the potential roles of NPs and PAs and their educational needs as we think about the future of sleep medicine.
Based on our survey data, APRNs (specifically NPs) and PAs are involved in the clinical practice of sleep medicine throughout the United States with NPs outnumbering PAs, similar to national published generic and specialty data.3 Within the AASM membership, APRNs also appear to be more prevalent than PAs based on the 2012 data, demonstrating a distribution of 76% APRNs and 24% PAs (AASM personnel communication).
NPs and PAs responding to this survey reported spending the majority of their time in sleep-related clinical activities, which appears to be higher than a recently published report of survey data of AASM physician members.30 Similar to the AASM physicians who were surveyed, APRNs and PAs reported devoting only limited time to research, educational, and administrative activities. Although these results may reflect the survey methods that were based largely on AASM accreditation or affiliation, the findings are still intriguing. APRNs and PAs provide many patient-care services, including initial and follow-up visits and explaining the results of sleep studies. They manage a range of sleep disorders, devoting most of their time to more commonly found sleep disorders, such as sleep-disordered breathing, insomnia, and movement disorders.
The challenge for the future is to combine our knowledge of APRN and PA disciplines with our new knowledge of APRN (specifically NP) and PA practices currently described within sleep centers. With the increase in APRNs and PAs in sleep practice, as with all professions engaged in the relatively new practice of sleep, educational preparation, specialty training, and competencies need to be determined with associated educational offerings, including academic preparation, provided to meet the future challenges of society.
Our survey highlights the lack of formal sleep education for most APRNs and PAs beyond “on-the-job” training with physicians, which in itself lacks standardization. Although this mentored clinical education provides practical experience in the diagnosis and treatment of sleep disorders, the mentor-ship may reduce clinic productivity initially during the training period. Additionally, physician mentors must focus their time and energy on providing basic didactic instruction in sleep and sleep disorders. Perhaps, this additional education could be delivered more efficiently with a national, standardized continuing education program or formal coursework. Modern technology allows “on-demand” education to be delivered via video, audio, and print formats. Based on both survey responses and informal communications with APRNs and PAs, formal sleep education for APRNs and PAs is lacking prior to employment or during their initial training in a sleep clinic.
Limitations
The first survey (Survey 1) had a number of limitations. First, because the survey was sent to AASM member centers, the results may not reflect the practices of APRNs and PAs in sleep centers that do not maintain AASM membership. Additionally, because the survey focused on APRNs and PAs, those healthcare professionals who actively employ or are interested in employing APRNs and PAs may have been more likely to respond. The survey did not ask the respondents to note their states in which they were located thus, regional variation in ARPN and PA utilization may have been under- or over-estimated. The response rate to Survey 1 was low and may have been explained, in part, by the role of the center representative who was designated to receive email communications from the AASM and by their interest or involvement in the topic. Only 15 (5%) of clinic respondents identified themselves as APRNs or PAs.
In the first portion of the second survey (Survey 2, Part 1), the same limitations described above could influence the response rate. Additionally, respondents were given a relatively short time to respond during the summer vacation period. Of the respondents to the first survey (Survey 1), 10% indicated they did not wish to be contacted again. The lack of direct or email contact with APRN and PA stakeholders probably reduced the number of APRNs and PAs who knew about and responded to Part 1 of Survey 2. The second portion of the second survey (Survey 2, Part 2) was administered via email around the time of an in-person course advertised to a target audience of PAs and NPs (an APRN subgroup). The course participants were told verbally about the survey during the course, and this in-person invitation to participate probably increased participation rates. Additionally, the attendees' decision to attend a dedicated course may also influence their likelihood to participate in the survey.
Despite these limitations, the three surveys provide valuable information about the current roles of APRNs and PAs in sleep medicine and highlight the current need for formal sleep educational opportunities for these groups of providers.
DISCLOSURE STATEMENT
This was not an industry supported study. The analysis was performed at Emory University, Atlanta, GA and Clayton Sleep Institute, St. Louis, MO. Dr. Collop receives royalties from Up to Date. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the American Academy of Sleep Medicine (AASM) and Jordana Money and Patrick Murray for assisting with survey preparation, distribution, and collection of data. We would also like to thank incoming Task Force members Kimberly Vana and Denise Lassaline for manuscript review assistance.
REFERENCES
- 1.Fairman JA. Historic and historical opportunities: nurse practitioners and the opportunities of health reform. In: Sullivan-Marx EM, McGivern DO, Fairman JA, Greenberg SA, editors. Nurse Pracitioners: The Evolution and Future of Advanced Practice. 5th ed. New York: Springer; 2010. pp. 3–14. [Google Scholar]
- 2.Vorvick LJ. Physican Assistant Profession: History of the Profession. 2011. [Accessed December 28, 2013]. http://www.nlm.nih.gov/medlineplus/ency/article/001935.htm.
- 3.Bureau of Labor Statistics, United States Department of Labor. Occupational Employment Statistics. 2012. [Accessed December 28, 2013]. http://www.bls.gov/oes/current/oes_stru.htm#29-0000.
- 4.Brassard A. Types of Advanced Practice Nurses. 2012. [Accessed December 28, 2013]. http://campaignforaction.org/photo/types-advanced-practice-registered-nurses.
- 5.Auerbach DI. Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Med Care. 2012;50:606–10. doi: 10.1097/MLR.0b013e318249d6e7. [DOI] [PubMed] [Google Scholar]
- 6.Hooker RS, Cawley JF, Everett CM. Predictive modeling the physician assistant supply: 2010-2025. Public Health Rep. 2011;126:708–16. doi: 10.1177/003335491112600513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park M, Cherry D, Decker SL. Nurse practitioners, certified nurse midwives, and physician assistants in physician offices. NCHS Data Brief. 2011. [Accessed December 28, 2013]. http://www.cdc.gov/nchs/data/databriefs/db69.pdf. [PubMed]
- 8.Cunningham R. Tapping the Potential of the Health Care Workforce: Scope-of-Practice and Payment Policies for Advanced Practice Nurses and Physician Assistants. National Health Policy Forum Background Paper No. 76. 2010. [Accessed December 28, 2013]. http://www.nhpf.org/library/background-papers/BP76_SOP_07-06-2010.pdf.
- 9.APRN Consensus Work Group & the National Council of State Boards of Nursing APRN Advisory Committee. Consensus Model of APRN Regulation: Licensure, Accrediation, Certification & Education. 2008. [Accessed December 28, 2013]. http:///www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf.
- 10.American Nurse Credentialing Center. ANCC Certification Center. 2013. [Accessed December 28, 2013]. http://www.nursecredentialing.org/certification.
- 11.U.S. Drug Enforcement Agency. Mid-Level Providers Authorization by State. 2013. [Accessed December 28, 2013]. http://www.deadiversion.usdoj.gov/drugreg/practioners/
- 12.National Council of State Boards of Nursing I. NCSBN's APRN Campaign for Consensus: State Progress toward Uniformity. 2013. [Accessed December 28, 2013]. https://www.ncsbn.org/2567.htm.
- 13.Accreditation Review Commission on Education for the Physician Assistant. Accreditation Standards for the Physician Assistant Education. 2013. Sep, [Accessed December 28, 2013]. http://www.arc-pa.org/documents/Standards4theditionwithclarifyingchanges9.2013%20FNL.pdf.
- 14.American Academy of Nurse Practitioners. 2012 AANP Survey. 2012. [Accessed December 28, 2013]. http://www.aanp.org/images/documents/research/2012%20membership%20survey%20report.pdf.
- 15.American Academy of Physician Assistants. Alexandria, VA: 2013. AAPA 2012/2013 Census Report. [Google Scholar]
- 16.American Academy of Physician Assistants. Professional Issues. 2011. [Accessed December 28, 2013]. http://www.aapa.org/uploadedFiles/content/The_PA_Profession/Federal_and_State_Affairs/Resources_Items/PI_PAScopePractice_110811_Final.pdf.
- 17.American Academy of Physician Assistants. Physician Assistant State and Territorial Regulatory Authorities. [Accessed December 28, 2013]. http://www.aapa.org/the_pa_profession/federal_and_state_affairs/resources/item.aspx?id=759.
- 18.Centers for Medicare and Medicaid Services (CMS) Pub 100-08, tranmittal 468, CMS Manual System. 2013. [Accessed December 28, 2013]. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R468PI.pdf.
- 19.Department of Health and Human Services. Centers for Medicare and Medicaid Services. 2001. Dec 13, [Accessed December 28, 2013]. Medicare Carriers Manuel Part 3 – Claims Process. Transmittal 1734. http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1734B3.pdf.
- 20.National Council of State Boards of Nursing. APRN Maps-Certification Requirements. [Accessed December 28, 2013]. https://www.ncsbn.org/2567.htm.
- 21.National Council of State Boards of Nursing. APRN Maps-Education Requirements. [Accessed December 28, 2013]. https://www.ncsbn.org/2567.htm.
- 22.American Academy of Physician Assistants. Statutory and Regulatory Requirements for State Licensure. [Accessed December 28, 2013]. http://www/aapa.org/uploadedFiles/content/Your_PA_Career/Licensing_and_Certification/Resource_Items/Requirements%20for%20Licensure%20(Summary%20Chart)%202-13.pdf.
- 23.American Association of Colleges of Nursing. CCNE Accreditation. [Accessed December 28, 2013]. http://www.aacn.nche.edu/ccne-accreditation.
- 24.National Commission on Certification of Physican Assistants. Inital Certification. [Accessed December 28, 2013]. http://www.nccpa.net/Pance.
- 25.National Commission on Certification of Physican Assistants. Certificates of Added Qualifications. [Accessed December 28, 2013]. http://www.nccpa.net/SpecialtyCAQs.
- 26.American Association of Diabetes Educators. Board Certified Advanced Diabetes Management Certification. [Accessed December 28, 2013]. http://www.diabeteseducator.org/ProfessionalResources/Certification/BC-ADM/
- 27.National Asthma Educator Certification Board. Exam Information. [Accessed December 28, 2013]. http://www.naecb.com/exam_information.php.
- 28.Institute of Medicine (IOM) Washington D.C.: The National Academies Press; 2011. The Future of Nursing: Leading Change, Advancing Health. [PubMed] [Google Scholar]
- 29.Bahr MS. The future of sleep is here. J Clin Sleep Med. 2013;9:841–3. doi: 10.5664/jcsm.2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Redline S, Badr S, Chervin R. A snapshot of the practice of sleep medicine: a survey solicited by the American Academy of Sleep Medicine. J Clin Sleep Med. 2013;9:175–6. doi: 10.5664/jcsm.2422. [DOI] [PMC free article] [PubMed] [Google Scholar]


