Summary
Background
Historically, health facilities in sub-Saharan Africa have mainly managed acute, infectious diseases. Few data exist for the preparedness of African health facilities to handle the growing epidemic of chronic, non-communicable diseases (NCDs). We assessed the burden of NCDs in health facilities in northwestern Tanzania and investigated the strengths of the health system and areas for improvement with regard to primary care management of selected NCDs.
Methods
Between November, 2012, and May, 2013, we undertook a cross-sectional survey of a representative sample of 24 public and not-for-profit health facilities in urban and rural Tanzania (four hospitals, eight health centres, and 12 dispensaries). We did structured interviews of facility managers, inspected resources, and administered self-completed questionnaires to 335 health-care workers. We focused on hypertension, diabetes, and HIV (for comparison). Our key study outcomes related to service provision, availability of guidelines and supplies, management and training systems, and preparedness of human resources.
Findings
Of adult outpatient visits to hospitals, 58% were for chronic diseases compared with 20% at health centres, and 13% at dispensaries. In many facilities, guidelines, diagnostic equipment, and first-line drug therapy for the primary care of NCDs were inadequate, and management, training, and reporting systems were weak. Services for HIV accounted for most chronic disease visits and seemed stronger than did services for NCDs. Ten (42%) facilities had guidelines for HIV whereas three (13%) facilities did for NCDs. 261 (78%) health workers showed fair knowledge of HIV, whereas 198 (59%) did for hypertension and 187 (56%) did for diabetes. Generally, health systems were weaker in lower-level facilities. Front-line health-care workers (such as non-medical-doctor clinicians and nurses) did not have knowledge and experience of NCDs. For example, only 74 (49%) of 150 nurses had at least fair knowledge of diabetes care compared with 85 (57%) of 150 for hyptertension and 119 (79%) of 150 for HIV, and only 31 (21%) of 150 had seen more than five patients with diabetes in the past 3 months compared with 50 (33%) of 150 for hypertension and 111 (74%) of 150 for HIV.
Interpretation
Most outpatient services for NCDs in Tanzania are provided at hospitals, despite present policies stating that health centres and dispensaries should provide such services. We identified crucial weaknesses (and strengths) in health systems that should be considered to improve primary care for NCDs in Africa and identified ways that HIV programmes could serve as a model and structural platform for these improvements.
Funding
UK Medical Research Council.
Introduction
Historically, health facilities in sub-Saharan Africa have focused on the acute management of infectious diseases such as malaria, diarrhoea, and respiratory infections.1 The scale of the HIV epidemic, and increasing availability of antiretroviral therapy, have resulted in intensive efforts to strengthen primary care health systems for HIV, which have transformed HIV from a life-threatening illness to a chronic non-fatal disease.2 In the past decade, an epidemic of chronic non-communicable diseases (NCDs) has also been recognised in sub-Saharan Africa.3, 4, 5 Although the primary care management of NCDs is similar to HIV management in many regards,2, 6 and primary care interventions for NCDs have proven to be highly cost effective,7 primary care health systems for NCDs reportedly remain weak in sub-Saharan Africa.1, 8
Data to quantify the burden of NCDs in health facilities in sub-Saharan Africa and the preparedness of these facilities for coping with the rising epidemic of NCDs are insufficient, making it difficult to plan appropriate responses and to assess the quality and effect of services provided.3, 8, 9 The result is a vicious cycle in which the absence of necessary data, the absence of evidence-based policies, and an inadequate response at primary care level reinforce each other, thus perpetuating a problem that will become worse with time unless the situation is actively addressed. Research is urgently needed to guide policies to improve primary care of patients with NCDs, while making effective use of few resources.3, 9, 10
We assessed the burden of NCDs in a representative sample of public and not-for-profit health facilities in northwestern Tanzania and investigated the strengths of the health system and areas for improvement with regard to primary care management of these diseases. We studied a broad range of chronic diseases with focus on hypertension, diabetes, and HIV (for comparison). We sought to determine and compare: the burden of NCDs and referral patterns; the availability of basic supplies and guidelines; the strength of management and training systems; and the preparedness of human resources. We hypothesised that low level health facilities would be the least prepared for care of NCDs, that achievable targets for the improvement of primary care for NCDs could be identified, and that care services for HIV might provide examples for how to improve and opportunities to achieve this improvement.
Methods
Study setting
Between November, 2012, and May, 2013, we did a cross-sectional survey of health facilities in northwestern Tanzania, in Mwanza city, Geita and Kahama towns, and in selected rural areas in Geita and Kahama districts. Mwanza, on the southern shores of Lake Victoria, is a regional administrative and commercial centre, which had a population of 706 453 in 2012.11 Geita and Kahama both have populations of roughly 200 000,11 with a major industry of gold mining. Areas located outside the towns of Geita and Kahama are typical of rural areas in Tanzania where people engage mainly in subsistence farming and fishing. This study is a self-standing part of an ongoing research programme aiming to investigate and improve health services for chronic diseases in Tanzania and Uganda.
In 2009, Tanzania established an NCD section within the Ministry of Health (MoH) and developed the National NCD Strategic Plan 2009–13 (Mghamba J, Tanzanian Ministry of Health, personal communication). This document acknowledged that more data would be necessary to assess the progress of preparedness for care of NCDs in health facilities in Tanzania. This study was done in close collaboration with the MoH to collect data needed to further develop and inform policy.
In the Tanzanian health-care system, the bulk of care provision occurs through the public sector. Private, not-for-profit facilities are often designated by the MoH to serve the functions of public facilities and therefore receive both the benefits of training and supervision from the MoH and the responsibility to follow national guidelines. The present Tanzanian policy for health-care funding involves both government subsidisation and cost-sharing fees. Adult outpatients usually pay a user fee equivalent to roughly US$1·5 for a clinic visit and medications, plus additional small fees for laboratory tests when required. When drugs are out of stock at the health facility, patients are usually asked to purchase the drugs from a private pharmacy. Unlike for NCDs, HIV visits and drugs are provided free of charge because of strong funding from both national and international sources.
This study was approved by the ethics committees of the Tanzanian National Institute for Medical Research and the London School of Hygiene and Tropical Medicine. The study was jointly conducted with the MoH and regional/district health-care management teams. Health-care workers' data were collected without any identifying information after written informed consent.
Health facility and health-care worker selection
24 public or private not-for-profit health facilities in the study areas were selected, including four hospitals (two referral and two district hospitals), eight health centres (two urban and six rural), and 12 dispensaries (six urban and six rural). In Mwanza, both the zonal referral hospital (Bugando Medical Center) and the regional referral hospital (Sekou Toure Hospital) were purposefully included, and two urban health centres and four urban dispensaries were randomly selected. In Geita and Kahama, the two district hospitals were purposefully included, and one urban dispensary was randomly chosen from each town. In each of the rural areas of Geita and Kahama districts, three rural health centres were randomly chosen and, for each randomly selected health centre, the nearest dispensary, preferably within 5 km, was also included (with random selection if more than one).
Health-care workers providing outpatient care to adults with chronic diseases were eligible for enrolment. Lists of such workers were provided by the facility heads, and included medical doctors, non-medical-doctor clinicians (either assistant medical officers or clinical officers), nurses, and clinical assistants.
Data collection
The study was done by a team of clinical fieldworkers (medical doctors, clinical officers, and nurses) under the direction of a senior epidemiologist. We collected data for epilepsy, heart failure, chronic obstructive pulmonary disease (COPD), and asthma (appendix), but focused on HIV, hypertension, and diabetes. Hypertension and diabetes were chosen because the burden of these diseases is believed to be high and increasing in sub-Saharan Africa,12, 13, 14 and they provide a useful entry point for the control of other NCDs.15 Data for HIV were collected for comparison because of recent strengthening efforts for primary care of HIV, but also because HIV and NCDs pose similar challenges to health systems as both require life-long monitoring and drug provision.
Data were collected with three instruments. First, service statistics were collected. Outpatient register books at each of the health facilities were reviewed to establish service provision for adults (≥18 years) retrospectively from July, 2012, to September, 2012, including the number of adults seen per month with each chronic disease, the number of visits made by these patients, and the total number of adult outpatient visits. These standard register books record all visits to the outpatient department and are completed by the senior clinicians of each facility. The data collection period corresponds to the dry season. Second, we interviewed the heads of health facilities and relevant outpatient departments to assess facility readiness to provide chronic disease services by use of an adapted version of the WHO Service Availability and Readiness Assessment (SARA) questionnaire,16 a comprehensive approach to systematically assess and monitor health services, which has been adopted by the Tanzanian MoH. We examined general characteristics of health facilities; service availability; referral patterns; drug supply; reporting systems, monitoring, and supervision; staffing; equipment; and laboratory services; with direct observation of supplies and reports. Finally, health-care workers completed an anonymous, ten-page self-reported questionnaire developed to assess experience, training, supervision, comfort level with case management, and availability of drugs and equipment related to HIV, hypertension, and diabetes. We tested basic knowledge with case scenarios (appendix). This questionnaire was piloted with five Tanzanian medical doctors who all scored 30 of 30 and reported that the questions were reasonable and well worded. Questions were stated in both English and Kiswahili, and the Kiswahili version was verified by an independent translator.
Statistical analysis
We identified ten key study outcomes (table 1): one for present service provision, three for availability of guidelines and supplies, three for management and training systems, and three for preparedness of human resources. We also assessed the staffing levels at each facility. We summarised our results with frequencies and percentages, and compared outcomes by facility level with Fisher's exact test for 2×c tables.17 When comparing health-care worker responses by facility level or cadre, we took account of the clustering of health-care workers within facilities with robust standard errors. To compare results of hypertension and diabetes versus HIV, we used sign tests to account for matched responses within health facility or health-care worker. All analyses were done with Stata (version 12).
Table 1.
Study outcome derivations
| Instrument for data collection | Derivation | |
|---|---|---|
| Service provision | ||
| Number and proportion of outpatient visits related to each chronic disease | Service statistics | Averaged from July, 2012, to September, 2012, and types of facilities |
| Availability of guidelines and basic supplies | ||
| Availability of guidelines | SARA questionnaire | Guidelines observed in the outpatient clinic or respective specialist clinic for HIV, hypertension, or diabetes |
| Availability of basic diagnostic equipment | SARA questionnaire | HIV: screening and confirmatory rapid tests available and valid (not expired). Hypertension: digital blood pressure apparatus or manual blood pressure apparatus and stethoscope observed and functioning in outpatient department or hypertension clinic. Diabetes: glucometer observed and functioning in outpatient department or diabetes clinic, or available and often or always functioning in laboratory (with test strips never or only occasionally out of stock) |
| Availability of first-line drug therapy | SARA questionnaire | HIV: at least one first-line regimen available and valid (TDF+3TC or TDF+FTC or AZT+3TC or d4T+3TC and NVP or EFV). Hypertension: at least one thiazide diuretic (hydrochlorothiazide or bendrofluazide) available and valid. Diabetes: metformin available and valid |
| Management and training systems | ||
| Training | SARA questionnaire | Any outpatient staff member having received training in the diagnosis and management of HIV, hypertension, or diabetes within the past 2 years |
| Supervision | SARA questionnaire | Having received a monitoring or supervisory visit from a high level of the health service within past 3 months for HIV, hypertension, or diabetes (asked of non-communicable diseases combined and assumed to apply equally to hypertension and diabetes) |
| Reporting | SARA questionnaire | Able to show a monthly report for HIV, hypertension, or diabetes for some time in the past year |
| Preparedness of human resources | ||
| At least fair knowledge | Self-completed questionnaire | Assessed via case scenario questionnaires for HIV, hypertension, and diabetes, and defined as scoring at least 7/10 |
| Experienced | Self-completed questionnaire | Having seen more than five patients with each of HIV, hypertension, or diabetes in past 3 months |
| Comfortable | Self-completed questionnaire | Reporting “very comfortable” when asked whether feel comfortable with HIV, hypertension, or diabetes and know how to manage |
SARA=Service Availability and Readiness Assessment. TDF=tenofovir. FTC=emtricitabine. 3TC=lamivudine. AZT=zidovudine. d4T=stavudine. NVP=nevirapine. EFV=efavirenz.
Role of the funding source
The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report, or the decision to submit for publication. RP and SK had access to all the data and final responsibility for the decision to submit for publication.
Results
All 24 selected health facilities agreed to participate and were enrolled in the study. Of these, 18 were owned by the Tanzanian Government, five were not-for-profit faith-based facilities, and one was a joint venture (appendix p 1).
In these 24 health facilities, we identified 335 eligible health-care workers, of whom all consented and completed the questionnaire. 34 were medical doctors, 68 were non-medical-doctor clinicians, 150 were nurses, and 83 were clinical assistants (appendix p 1).
The mean number of outpatient visits related to chronic diseases per month per facility was 1411 for hospitals, 44 for health centres, and 22 for dispensaries (figure, table 2). Of outpatient visits to hospitals, 58% of visits were due to chronic diseases versus 20% in health centres and 13% in dispensaries (table 2). Of all visits, 28% were related to HIV, compared with 4% for hypertension, 5% for diabetes, 5% for epilepsy, 2% for heart failure, and 2% for COPD or asthma (table 2).
Figure.
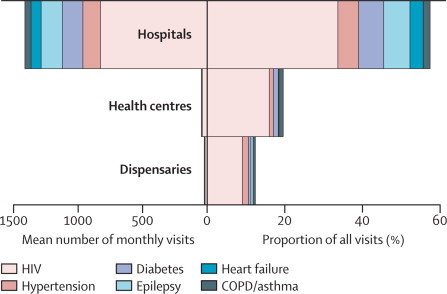
Burden of chronic diseases at 24 health facilities in northwest Tanzania
Mean number of chronic disease visits per month per facility is displayed to the left of the midline and the proportion of all outpatient visits due to chronic diseases is on the right. Data were collected from the adult outpatient departments of these 24 health facilities. COPD=chronic obstructive pulmonary disease.
Table 2.
Service provision for chronic diseases in adults seen at the outpatient departments of 24 health facilities in northwest Tanzania
| Hospitals (N=4) | Health centres (N=8) | Dispensaries (N=12) | Overall (N=24) | ||
|---|---|---|---|---|---|
| All visits/month/facility | 2447 | 223 | 157 | 561 | |
| Visits related to chronic diseases | 1411 (57·6%) | 44 (19·8%) | 22 (12·7%) | 271 (46·3%) | |
| HIV | |||||
| Patients/month | 829 | 36 | 14 | 157 | |
| Visits/month | 829 (33·9%) | 36 (16·2%) | 14 (9·0%) | 157 (28·1%) | |
| Hypertension | |||||
| Patients/month | 131 | 3 | 2 | 24 | |
| Visits/month | 131 (5·3%) | 3 (1·5%) | 3 (1·7%) | 24 (4·3%) | |
| Diabetes | |||||
| Patients/month | 162 | 1 | 1 | 28 | |
| Visits/month | 162 (6·6%) | 1 (0·3%) | 1 (0·8%) | 28 (5·0%) | |
| Epilepsy | |||||
| Patients/month | 161 | 1 | <1 | 28 | |
| Visits/month | 161 (6·6%) | 1 (0·5%) | <1 (0·5%) | 29 (4·9%) | |
| Heart failure | |||||
| Patients/month | 81 | <1 | <1 | 13 | |
| Visits/month | 81 (3·3%) | <1 (0·1%) | <1 (<0·1%) | 13 (2·4%) | |
| COPD or asthma | |||||
| Patients/month | 48 | 3 | 1 | 9 | |
| Visits/month | 48 (1·9%) | 3 (1·1%) | 1 (0·7%) | 9 (1·7%) | |
Results are mean number of patients and visits per month per facility, and proportion of visits as percentage of all visits. COPD=chronic obstructive pulmonary disease.
Although all hospitals reported providing services for HIV, hypertension, and diabetes, two of eight health centres and ten of 12 dispensaries reported that they routinely referred patients with HIV (p=0·003), compared with three health centres and ten dispensaries for hypertension (p=0·005), and six health centres and 11 dispensaries (p=0·005) for diabetes (appendix p 2). Very few health centres and dispensaries reported receiving referrals back (seven of 11 for HIV, two of 16 for hypertension, and two of 16 for diabetes).
Guidelines for HIV management were observed at all four hospitals compared with five health centres and one dispensary (table 3). Guidelines for hypertension and diabetes were observed in only three health facilities (all faith-based dispensaries; appendix p 6).
Table 3.
Availability of guidelines and basic supplies, and strength of management, training, and reporting systems to ensure quality primary care for HIV, hypertension, and diabetes at 24 health facilities in northwest Tanzania, by health facility level
| Hospitals (N=4) | Health centres (N=8) | Dispensaries (N=12) | p value | Total | p value vs HIV | |
|---|---|---|---|---|---|---|
| Guidelines | ||||||
| HIV | 4 (100%) | 5 (63%) | 1 (8%) | 0·001 | 10 (42%) | .. |
| Hypertension | 0 | 0 | 3 (25%) | 0·25 | 3 (13%) | 0·07 |
| Diabetes | 0 | 0 | 3 (25%) | 0·25 | 3 (13%) | 0·07 |
| Diagnostic equipment | ||||||
| HIV | 4 (100%) | 2 (25%) | 4 (33%) | 0·05 | 10 (42%) | .. |
| Hypertension | 3 (75%) | 5 (63%) | 9 (75%) | 0·84 | 17 (71%) | 0·09 |
| Diabetes | 3 (75%) | 3 (38%) | 2 (17%) | 0·10 | 8 (33%) | 0·69 |
| First-line therapy | ||||||
| HIV | 4 (100%) | 6 (75%) | 1 (8%) | 0·0005 | 11 (46%) | .. |
| Hypertension | 3 (75%) | 2 (25%) | 3 (25%) | 0·16 | 8 (33%) | 0·51 |
| Diabetes | 4 (100%) | 1 (13%) | 3 (25%) | 0·007 | 8 (33%) | 0·51 |
| Training | ||||||
| HIV | 1 (25%) | 2 (25%) | 4 (33%) | 1·00 | 7 (29%) | .. |
| Hypertension | 1 (25%) | 0 (0%) | 0 (0%) | 0·17 | 1 (4%) | 0·03 |
| Diabetes | 1 (25%) | 0 (0%) | 0 (0%) | 0·17 | 1 (4%) | 0·03 |
| Supervision | ||||||
| HIV | 4 (100%) | 6 (75%) | 3 (25%) | 0·009 | 13 (54%) | .. |
| Hypertension | 0 | 3 (38%) | 2 (17%) | 0·42 | 5 (21%) | 0·04 |
| Diabetes | 0 | 3 (38%) | 2 (17%) | 0·42 | 5 (21%) | 0·04 |
| Reporting | ||||||
| HIV | 4 (100%) | 6 (75%) | 1 (8%) | 0·0005 | 11 (46%) | .. |
| Hypertension | 0 | 0 | 0 | .. | 0 | 0·001 |
| Diabetes | 3 (75%) | 0 | 0 | 0·002 | 3 (13%) | 0·008 |
Data are n (%) unless otherwise indicated. See table 1 for outcome definitions.
Basic diagnostic equipment for HIV and diabetes was observed more frequently in hospitals than in health centres and dispensaries (table 3). Basic diagnostic equipment for hypertension was consistently present in 63–75% of health facilities (table 3), but even hospital outpatient departments sometimes did not have essential instruments such as sphygmomanometers. Overall, basic diagnostic equipment for hypertension was observed in 17 health facilities compared with ten facilities for HIV and eight facilities for diabetes.
Other equipment for the management of chronic diseases was also scarce (appendix pp 7–8). For example, six of 20 health centres and dispensaries did not have functioning weight scales and 14 did not have height measurement devices. Only three (all health centres) reported having CD4 cell counters for the management of HIV.
First-line drugs for HIV, hypertension, and diabetes were frequently lacking. For HIV, first-line antiretroviral drugs were available in all four hospitals and six of eight health centres, but only one of 12 dispensary. Of note, all facilities designated to provide HIV care had antiretroviral drugs available. For hypertension, thiazide diuretics were identified in three hospitals, but only two health centres and three dispensaries (table 3). For diabetes, metformin was available in all hospitals, but only one health centre and three dispensaries (table 3).
Drug stock-outs were commonly reported by all health facilities (appendix p 3). 23 facilities reported having stock-outs at least occasionally; one hospital, three health centres, and three dispensaries reported having stock-outs often or always.
Training, supervision, and reporting systems were significantly weaker for hypertension and diabetes than for HIV (table 3). Overall, seven facilities reported training of some staff for HIV in the past 2 years compared with only one (a hospital) for hypertension and diabetes (table 3). 13 facilities reported receiving a monitoring and supervision visit for HIV in the past 3 months compared with five for hypertension or diabetes (table 3). 11 facilities could show at least one monthly report for HIV care from the past year compared with none for hypertension and three (all hospitals) for diabetes (table 3).
Outreach activities for health promotion were done by 18 facilities, and seven reported disease-screening outreach (appendix p 3). Six facilities had done HIV outreach activities, but only one reported such activities for hypertension or diabetes. Health facilities doing outreach activities commonly reported the following challenges: absence of transport (17), insufficient funds (16), insufficient staff or time (15), staff insufficiently trained (12), absence of drugs (11), and absence of equipment (10).
Basic essential knowledge related to HIV was generally better than that for hypertension or diabetes (table 4). For HIV, 261 (78%) of 335 health-care workers showed at least fair knowledge compared with 198 (59%) for hypertension and 187 (56%) for diabetes (table 4). Knowledge was similar across health facility levels for HIV, hypertension, and diabetes (table 4). As expected, medical doctors showed greater knowledge than did non-medical-doctor clinicians, nurses, and assistants (table 5).
Table 4.
Present level of preparedness of human resources to ensure quality primary care for HIV, hypertension, and diabetes at 24 health facilities in northwest Tanzania, among 335 health-care workers by health facility level
| Hospitals (N=176) | Health centres (N=92) | Dispensaries (N=67) | p value | Total | p value vs HIV | |
|---|---|---|---|---|---|---|
| At least fair knowledge | ||||||
| HIV | 134 (76%) | 74 (80%) | 53 (79%) | 0·67 | 261 (78%) | .. |
| Hypertension | 108 (61%) | 57 (62%) | 33 (49%) | 0·52 | 198 (59%) | <0·0001 |
| Diabetes | 109 (62%) | 42 (46%) | 36 (54%) | 0·24 | 187 (56%) | <0·0001 |
| Experienced | ||||||
| HIV | 140 (80%) | 67 (73%) | 30 (45%) | 0·01 | 237 (71%) | .. |
| Hypertension | 101 (57%) | 19 (21%) | 14 (21%)* | 0·001 | 134 (40%) | <0·0001 |
| Diabetes | 96 (55%) | 6 (7%) | 7 (10%) | <0·0001 | 109 (33%) | <0·0001 |
| Comfortable | ||||||
| HIV | 26 (15%) | 13 (14%) | 13 (19%) | 0·78 | 52 (16%) | .. |
| Hypertension | 17 (10%) | 8 (9%) | 9 (13%) | 0·84 | 34 (10%) | 0·01 |
| Diabetes | 14 (8%) | 10 (11%) | 8 (12%) | 0·78 | 32 (10%) | 0·003 |
Data are n (%) unless otherwise indicated. See table 1 for outcome definitions.
Result missing for one respondant.
Table 5.
Present level of preparedness of human resources to ensure quality primary care for HIV, hypertension, and diabetes at 24 health facilities in northwest Tanzania, among 335 health-care workers by health-care worker cadre
| Medical doctors(N=34) | Non-medical clinicians(N=68) | Nurses(N=150) | Assistants(N=83) | p value | |
|---|---|---|---|---|---|
| At least fair knowledge | |||||
| HIV | 33 (97%) | 60 (88%) | 119 (79%) | 49 (59%) | 0·0007 |
| Hypertension | 33 (97%) | 58 (85%) | 85 (57%) | 22 (27%) | <0·0001 |
| Diabetes | 34 (100%) | 55 (81%) | 74 (49%) | 24 (29%) | 0·02 |
| Experienced | |||||
| HIV | 32 (94%) | 45 (66%) | 111 (74%) | 49 (59%) | 0·002 |
| Hypertension | 31 (91%) | 33 (49%) | 50 (33%) | 20 (24%)* | <0·0001 |
| Diabetes | 31 (91%) | 24 (35%) | 31 (21%) | 23 (28%) | <0·0001 |
| Comfortable | |||||
| HIV | 10 (29%) | 10 (15%) | 21 (14%) | 11 (13%) | 0·09 |
| Hypertension | 10 (29%) | 11 (16%) | 8 (5%) | 5 (6%) | 0·002 |
| Diabetes | 11 (32%) | 8 (12%) | 6 (4%) | 7 (8%) | 0·0005 |
Data are n (%) unless otherwise indicated. See table 1 for outcome definitions.
Result missing for one assistant.
Experience related to the management of chronic diseases was significantly less at low health facility levels (table 4). For example, 55% of health-care workers at hospitals reported seeing more than five patients with diabetes in the past 3 months versus 7% at health centres and 10% at dispensaries (table 4). Of all health-care workers, experience related to HIV was greater than that related to hypertension and diabetes (table 4); 237 (71%) reported seeing more than five patients with HIV in the past 3 months versus 134 (40%) for hypertension and 109 (33%) for diabetes.
Very few health-care workers reported feeling “very comfortable” in management of any disease, although medical doctors did show higher levels of comfort than did other cadres, particularly for hypertension and diabetes (table 5).
Assessment of staffing levels showed that the largest regional hospital had 83 medical doctors or non-medical-doctor clinicians available, and the remaining hospitals had 26–31 (appendix p 4). By comparison, the health centres had one to seven (median 2·5) and the dispensaries none to five (1·5) of such staff available. All hospitals had more than 100 nurses available compared with one to 18 (median 6·5) in health centres and one to six (2·0) dispensaries. Only two of 20 health centres or dispensaries met MoH recommended staffing levels.18
Discussion
In this representative sample of health facilities in northwestern Tanzania, most outpatient services for NCDs were provided in hospitals instead of health centres and dispensaries. In fact, most dispensaries and half of health centres reported not providing services for common NCDs such as hypertension and diabetes, despite being expected to do so according to present policy, and instead routinely referred these patients to hospitals. The low number of primary care visits for NCDs recorded in this study contrasts greatly with the high burden of NCDs described both in the community and among inpatients in Tanzania in three recent studies.19, 20, 21 In our survey of a representative sample of 1095 adults living in urban and rural areas surrounding the health facilities described in this study, the prevalence of hypertension was 22% and of diabetes was 1·6%, and the prevalences were similar in urban and rural areas (Kavishe B, Mwanza Intervention Trials Unit, personal communication).
We have described several challenges to primary care of NCDs in Tanzania. One obvious deficiency was that guidelines, basic supplies, and first-line drug regimens were absent at many health facilities, particularly at low-level facilities. For example, only 13% of facilities possessed guidelines for the management of hypertension and diabetes. Such guidelines are crucially important in facilities where most services are provided by non-medical-doctor clinicians, nurses, and assistants.2, 22, 23 Additionally, absence of diagnostic equipment and drugs for NCDs is a major reason for non-attendance,24 and a consistent supply of basic diagnostics and drugs is essential.25 Improvement in the quality of primary care for NCDs at the low-level health facilities will hopefully lead to a virtuous cycle of increased use of preventive services and fewer complications requiring care at high levels.26
Inconsistency of management systems for training, supervision, and reporting is another barrier to effective primary care for NCDs in Tanzania. Only one of the 24 health facilities surveyed reported any training in the past year for hypertension or diabetes. Training, supervision, and reporting were significantly better for HIV than for hypertension or diabetes, suggesting that systems developed for HIV in Tanzania could provide a model to strengthen these functions. For HIV, the rapid roll-out of complex antiretroviral therapy regimens to millions of people in sub-Saharan Africa in the past 10 years was made possible by: (1) strong leadership by Ministries of Health; (2) clear and practical national HIV guidelines; (3) consistent procurement and use of one or two regimens; (4) intensive training schedules focusing on non-medical-doctor clinicians and nurses; and (5) frequent supervision and monitoring.2 In particular, creation of reporting and monitoring systems that are similar to those for HIV will be crucial to improve surveillance of efforts to strengthen primary care for NCDs.2, 8 Compared with the complexities and expenses associated with primary care for HIV, the management of hypertension and diabetes are likely to pose a smaller and less costly challenge.
Human resources for primary care of NCDs must be developed. The number of health-care workers in health centres and dispensaries needs to be increased, at least to recommended staff levels.1, 3, 8 Because poor knowledge and experience of front-line health-care workers has been recognised as a major barrier to care for NCDs in sub-Saharan Africa,27, 28, 29 internship and externship training programmes are needed, particularly for non-medical-doctor clinicians and nurses. With proper training and supervision, non-medical-doctor clinicians or nurse-led clinics could provide effective primary care for NCDs in sub-Saharan Africa.22, 23, 30
We identified four key strengths of the health system that should be harnessed. First, the many knowledgeable and experienced health-care workers employed at hospitals could provide support and supervision for health-care workers at smaller facilities.1 Second, because most facilities provide some form of outreach services, community education and screening programmes for NCDs could build on these services, as successfully shown in Uganda.31 Third, the success of many health centres and dispensaries in provision of complex primary care for HIV proves that primary care for NCDs can be provided at these facilities, and provides the opportunity for integration of care for both HIV and NCDs, as has been done in Cambodia.32 Lastly, health-care workers at health facilities that are not at present providing services for NCDs consistently reported a desire to provide such care, with most suggesting that care for NCDs could be provided at their facilities if mechanisms for training, support, supervision, and consistent provision of basic supplies were in place.
This study has several limitations. First, although this study included a representative sample of health facilities from three regions including four districts in northwest Tanzania, the sample might not be representative of the entire country. However, a senior MoH official and coinvestigator of this study confirmed that our findings are consistent with the status of health services in other regions in Tanzania (Mghamba J, Tanzanian Ministry of Health, personal communication). Second, as a descriptive study, all p values should be regarded as exploratory rather than hypothesis testing, and moderate p values should be interpreted cautiously.
Our study has several strengths. It provides information about a variety of key components related to service quality. A standard WHO recommended and validated data collection instrument was used (the SARA questionnaire), and findings were triangulated with health services statistics and data obtained through a pretested health-worker questionnaire. The study not only focused on services for selected NCDs, but also on those for HIV infection, which allowed assessment of what types of improvement might be possible if similar attention is given to NCDs in the future. Importantly, the study was done on behalf of and in collaboration with policy makers and health programme managers, so its results can be expected to affect policy and practices of care services for NCDs.
In conclusion, clearly a multifaceted health system strengthening approach is needed to enable health facilities in Tanzania to provide high-quality primary care for the ever-increasing burden of NCDs (panel).3 These efforts should focus on three major targets: provision of clinical guidelines, basic diagnostic equipment, and first-line drug therapy for NCDs to all health centres and dispensaries; strengthening of management systems for NCDs to provide regular training, supervision, and reporting; and ensuring sufficient knowledge and experience related to NCDs among front-line health-care workers. For all these targets, primary-care systems for HIV could serve as both a model and foundation. The strengths of the primary care systems, such as highly experienced health-care workers stationed in hospitals, existing outreach programmes, and the desire of health workers to expand services, should be harnessed.
Panel. Research in context.
Systematic review
We searched PubMed and Medline for papers published in all languages between Jan 1, 1969, and Aug 13, 2013, with the terms “Africa south of the Sahara”, “primary health care”, and either “hypertension” or “diabetes mellitus”. We also searched the reference lists of identified articles for further relevant papers. Only 14 studies were identified from the past 15 years that provided quantitative data to describe either the burden of hypertension and diabetes at primary care facilities or the health system resources to manage these diseases in sub-Saharan Africa. No studies were identified that describe both the burden of these diseases and the preparedness of health systems at multiple levels of health facilities in sub-Saharan Africa. Most studies were done in either South Africa or Nigeria, and most were retrospective.
Interpretation
To the best of our knowledge this study is the first to systematically assess primary care for chronic diseases in sub-Saharan Africa in terms of both the present burden of chronic, non-communicable diseases (NCDs) and the preparedness of health facilities at multiple levels to manage an increasing burden of these diseases. Our results show that, in northwest Tanzania, most primary care for NCDs is occurring at hospitals in urban areas. Health systems strengthening, including consistent provision of guidelines and basic supplies, management and training systems, and preparedness of human resources, are urgently needed if health centres and dispensaries in sub-Saharan Africa are to provide high-quality primary care for the growing number of adults with NCDs in this region.
Acknowledgments
Acknowledgments
This study was funded by the UK Medical Research Council. We thank the district and regional medical officers, the heads of each health facility, and the health-care workers who took part in this study; and Kaushik Rumaiya for his insight into health systems for diabetes in Tanzania. FV and RH receive support from the MRC and Department for International Development (G0700837). LS is supported by a Wellcome Trust Senior Research Fellowship in Clinical Science grant number 098504/Z/12/Z. SK receives support from the MRC and Department for International Development (G0901756).
Contributors
HG, JM, LS, RH, and SK designed the study. BK, RP, and VR did the fieldwork. FV and RH did the analyses. HG and SK provided input to fieldwork and analysis. FV and RP wrote the first draft of the manuscript, and all authors approved the final version.
Declaration of interests
We declare that we have no competing interests.
Supplementary Material
References
- 1.Beaglehole R, Epping-Jordan J, Patel V. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372:940–949. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 2.Harries AD, Zachariah R, Jahn A, Schouten EJ, Kamoto K. Scaling up antiretroviral therapy in Malawi-implications for managing other chronic diseases in resource-limited countries. JAIDS. 2009;52:S14–S16. doi: 10.1097/QAI.0b013e3181bbc99e. [DOI] [PubMed] [Google Scholar]
- 3.Daar AS, Singer PA, Persad DL. Grand challenges in chronic non-communicable diseases. Nature. 2007;450:494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 4.Addo J, Smeeth L, Leon D. Hypertension in sub-saharan Africa: a systematic review. Hypertension. 2007;50:1012–1018. doi: 10.1161/HYPERTENSIONAHA.107.093336. [DOI] [PubMed] [Google Scholar]
- 5.Mbanya JCN, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 6.Levitt NS, Steyn K, Dave J, Bradshaw D. Chronic noncommunicable diseases and HIV-AIDS on a collision course: relevance for health care delivery, particularly in low-resource settings—insights from South Africa. S Afr Med J. 2011;94:1690–1696. doi: 10.3945/ajcn.111.019075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortegon M, Lim S, Chisholm D, Mendis S. Cost effectiveness of strategies to combat cardiovascular disease, diabetes, and tobacco use in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012;344:e607. doi: 10.1136/bmj.e607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali MK, Rabadán-Diehl C, Flanigan J, Blanchard C, Narayan KMV, Engelgau M. Systems and capacity to address noncommunicable diseases in low- and middle-income countries. Sci Transl Med. 2013;5:181cm4. doi: 10.1126/scitranslmed.3005121. [DOI] [PubMed] [Google Scholar]
- 9.Maher D, Sekajugo J, Harries AD, Grosskurth H. Research needs for an improved primary care response to chronic non-communicable diseases in Africa. Trop Med Int Heal. 2010;15:176–181. doi: 10.1111/j.1365-3156.2009.02438.x. [DOI] [PubMed] [Google Scholar]
- 10.Unwin N. Non-communicable disease and priorities for health policy in sub-Saharan Africa. Heal Policy Plan. 2001;16:351–352. doi: 10.1093/heapol/16.4.351. [DOI] [PubMed] [Google Scholar]
- 11.National Bureau of Statistics . Tanzania 2012 Population and Housing Census. National Bureau of Statistics; Dar es Salaam: 2013. http://www.nbs.go.tz/sensa/new.html (accessed Jan 6, 2014). [Google Scholar]
- 12.Dalal S, Beunza JJ, Volmink J. Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40:885–901. doi: 10.1093/ije/dyr050. [DOI] [PubMed] [Google Scholar]
- 13.Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast asian and african regions: need for effective strategies for prevention and control in primary health care settings. Int J Hypertens. 2013;2013:1–14. doi: 10.1155/2013/409083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Danaei G, Finucane MM, Lin JK. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 15.Mendis S, O'Brien E, Seedat YK, Yusuf S. Hypertension and diabetes: entry points for prevention and control of the global cardiovascular epidemic. Int J Hypertens. 2013;2013:1–3. doi: 10.1155/2013/878460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO Service Availability and Readiness Assessment (SARA) http://www.who.int/healthinfo/systems/sara_indicators_questionnaire/en/ (accessed Aug 30, 2013).
- 17.Mehta CR, Patel NR. A network algorithm for performing Fisher's exact test in r_c contingency tables. J Am Stat Assoc. 1983;78:427–434. [Google Scholar]
- 18.Tanzanian Ministry of Health and Social Welfare . Guidelines Standards for Health Facilities. Tanzanian Ministry of Health and Social Welfare; Dar es Salaam: 1996. [Google Scholar]
- 19.Dewhurst MJ, Dewhurst F, Gray WK, Chaote P, Orega GP, Walker RW. The high prevalence of hypertension in rural-dwelling Tanzanian older adults and the disparity between detection, treatment and control: a rule of sixths? J Hum Hypertens. 2013;27:374–380. doi: 10.1038/jhh.2012.59. [DOI] [PubMed] [Google Scholar]
- 20.Hendriks ME, Wit FWNM, Roos MTL. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PLoS One. 2012;7:e32638. doi: 10.1371/journal.pone.0032638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peck R, Green E, Mtabaji J. Hypertension-related diseases as a common cause of hospital mortality in Tanzania: a 3-year prospective study. J Hypertens. 2013;31:1806–1811. doi: 10.1097/HJH.0b013e328362bad7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mamo Y, Seid E, Adams S, Gardiner A, Parry E. A primary healthcare approach to the management of chronic disease in Ethiopia: an example for other countries. Clin Med. 2007;7:228–231. doi: 10.7861/clinmedicine.7-3-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kengne AP, Awah PK, Fezeu LL, Sobngwi E, Mbanya J-C. Primary health care for hypertension by nurses in rural and urban sub-Saharan Africa. J Clin Hypertens. 2009;11:564–572. doi: 10.1111/j.1751-7176.2009.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thorogood M, Connor MD, Hundt GL, Tollman SM. Understanding and managing hypertension in an African sub-district: a multidisciplinary approach. Scand J Public Heal. 2007;69:52–59. doi: 10.1080/14034950701355411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO . Development of an updated Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. World Health Organization; Geneva: 2012. [Google Scholar]
- 26.Stringer JSA, Chisembele-taylor A, Chibwesha CJ. Protocol-driven primary care and community linkages to improve population health in rural Zambia: the Better Health Outcomes through Mentoring and Assessment (BHOMA) project. BMC Health Serv Res. 2013;13:S7. doi: 10.1186/1472-6963-13-S2-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mendis S, Abegunde D, Oladapo O, Celletti F, Nordet P. Barriers to management of cardiovascular risk in a low-resource setting using hypertension as an entry point. J Hypertens. 2004;22:59–64. doi: 10.1097/00004872-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Haque M, Emerson SH, Dennison CR, Navsa M, Levitt NS. Barriers to initiating insulin therapy in patients with type 2 diabetes mellitus in public-sector primary health care centres in Cape Town. S Afr Med J. 2005;95:798–802. [PubMed] [Google Scholar]
- 29.Sengwana MJ, Puoane T. Knowledge, beliefs and attitudes of community health workers about hypertension in the Cape Peninsula, South Africa. Curationis. 2004;27:65–71. doi: 10.4102/curationis.v27i1.958. [DOI] [PubMed] [Google Scholar]
- 30.Kengne AP, Fezeu L, Sobngwi E. Type 2 diabetes management in nurse-led primary healthcare settings in urban and rural Cameroon. Prim Care Diabetes. 2009;3:181–188. doi: 10.1016/j.pcd.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 31.Chamie G, Kwarisiima D, Clark TD. Leveraging rapid community-based HIV testing campaigns for non-communicable diseases in rural Uganda. PLoS One. 2012;7:e43400. doi: 10.1371/journal.pone.0043400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Janssens B, Van Damme W, Raleigh B. Offering integrated care for HIV/AIDS, diabetes and hypertension within chronic disease clinics in Cambodia. Bull World Health Organ. 2007;85:880–885. doi: 10.2471/BLT.06.036574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


