Abstract
Objective
The aims of the study were to determine the rates of multiple gestation, the stillbirth, perinatal, and neonatal mortality rates, and to determine health care characteristics associated with outcomes of these pregnancies in low- and mid-income countries.
Design/Methods
All pregnant women residing in defined geographic clusters located in 7 sites in 6 countries, Kenya, Zambia, Argentina, Guatemala, Pakistan, India (Belgaum and Nagpur) were enrolled and followed to 42 days postpartum, with staff collecting pregnancy characteristics and maternal and perinatal outcomes.
Results
A total of 69,706 women were enrolled. Multiple gestations accounted for 0.9% of all births (twins 0.9%, triplets 0.01%). Kenya and Pakistan had the highest rates of multiple gestation deliveries with 14.6/1000 and 10.7/1000 live births respectively. The mothers with a multiple gestation were more likely to deliver in a health care facility compared to singleton pregnancy mothers (70% and 66% respectively, p<0.001), to be attended by skilled health personnel (71% and 67%, p<0.001) and to be delivered by Cesarean section (18% vs. 9%, p<0.001). Multiple gestation fetuses had a relative risk (RR) for stillbirth of 2.65 (2.06, 3.41) and for perinatal mortality rate (PMR) a RR of 3.98 (3.40, 4.65) relative to singletons (both p<0.0001). Neither delivery in a health facility nor the Cesarean section rate was associated with decreased PMR. Among multiple gestation deliveries, physician attended delivery relative to delivery by other health providers was associated with a decreased risk of perinatal mortality.
Conclusions
Multiple gestations contribute disproportionately to PMR in low resource countries. Physician delivery may be associated with improved outcomes; however, neither delivery in a health facility nor the Cesarean section rate is associated with improved PMR. These results suggest that merely encouraging women to deliver in health facilities will not be sufficient to decrease these risks associated with multiple gestation.
INTRODUCTION
Multiple gestation, defined as the carriage of more than one fetus in a single pregnancy, is a leading risk factor for poor pregnancy outcome. (1-6) The incidence of multiple pregnancies has been on the rise in the developed countries with twins accounting for more than 4% of all births.(1, 2),(7) The incidence of multiple gestation is lower in developing countries, generally 2-3% of all births. However, the risk of neonatal death is significantly higher. Several studies have suggested that the risk of perinatal death may be ten-fold for multiple births compared to singleton, with increased risk for maternal morbidity and mortality as well.(3, 5)
Even with optimal care, including both prenatal and perinatal care, the risk of maternal as well as neonatal morbidity and mortality for multiple gestations is increased compared to singleton births. In many developing countries, antenatal clinic attendance is poor(6), skilled birth attendants are often unavailable, and nearly half of all births occur in the home or otherwise outside of health facilities(8). Compared to women carrying a singleton, women with a multiple pregnancy are at increased risk for conditions including preeclampsia, anemia, gestational diabetes, premature rupture of membranes and post-partum hemorrhage. Many of these are risk factors that require Cesarean section to improve outcomes. (9) Cesarian section is indicated for more than half of twin pregnancies and is almost always required for higher order gestations.(10) Even in developed countries, the risk of death for twins and higher multiples is significantly greater than singletons. (5) Nevertheless, significant disparities in maternal and perinatal outcomes associated with multiple births exist between developed and developing countries, with risk of adverse outcome several fold higher in developing compared to developed countries.(11) (12)
The increasing rates of ovarian stimulation and assisted reproductive techniques are associated with increased rates of multiple births, especially in developed countries. Less is known about the many and complex factors that contribute to a woman conceiving multiple fetuses; however, in developing countries, risk factors such as advanced maternal age may contribute to likelihood of multiple conception.(8, 10-12)
Despite its importance as a risk for adverse pregnancy outcomes, few studies have evaluated the prevalence and outcome of multiple gestation pregnancies in the rural, community setting of developing countries. We sought to describe multiple gestation pregnancies in rural settings of resource poor countries in Asia and Africa as well as a middle income country in South America. Our specific objectives were to determine the incidence of multiple births, describe relevant health demographic profiles of mothers with multiple pregnancies, describe the neonatal outcomes of these pregnancies and compare them to those of singleton pregnancies among the participating countries.
METHODS
The Global Network for Women and Children’s Health Research Maternal Newborn Health registry study is a prospective multicenter study conducted in Kenya, Zambia Pakistan, Guatemala, Argentina and India (8). The registry includes 106 geographically defined study clusters across the sites. The birth registry methods and initial data have been described in detail elsewhere (8). Briefly, in all study clusters, registry administrators who are study staff enroll pregnant mothers as early as 20 weeks of gestation and follow them through delivery and to 42 days postpartum. Maternal and neonatal outcomes are recorded.
For this study, mothers enrolled from January 2010 to December 2010 were included in the final analyses. Adjusted relative risks (RRs) and 95% confidence intervals (CIs) from generalized estimating equation (GEE) extensions of logistic regression models adjusting for cluster were reported for twin fetal and neonatal outcomes by gender. Multivariate logistic, proportional odds regression models and mixed regression models with GEE adjusting for cluster were used to determine differences in pregnancy and infant outcomes between multiple and single gestation pregnancies. Adjusted RRs and 95% CIs from GEE extensions of a logistic regression model adjusting for clustering of multiples were reported for perinatal mortality as a function of site and the average cluster rates of physician deliveries, hospital deliveries and c-section deliveries. Data were analyzed using SAS software version 9.2 (Cary, NC).
Ethical considerations
Institutional review board approval was obtained from all involved institutions, including local ethics review boards in each of the countries. Consent was obtained from all participants. Subject identification numbers were used to ensure confidentiality. Subject information and records were kept confidentially.
RESULTS
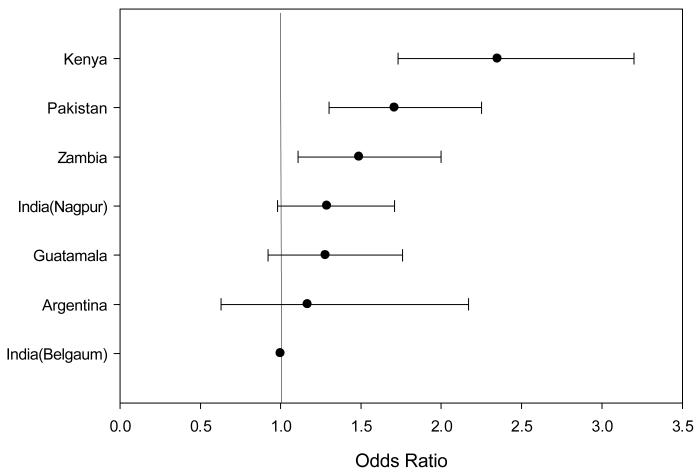
The total number of pregnant women enrolled was 69,706 (Table 1). The Belgaum (India) site had the highest number of deliveries, while Argentina had the lowest. Multiple births accounted for approximately 1% of all of the pregnancies, with twins contributing 0.9% and triplets 0.01%. Kenya and Pakistan had the highest rates of multiple gestation deliveries with rates of 14.6/1000 and 10.7/1000 live births respectively. The incidence of multiple gestation pregnancy varied by site (Figure 1). Kenyan multiple gestation rates were almost twice that of Argentina. Kenya also reported the highest rate of triplets (0.3/1000 live births). Zambia, Belgaum, and Pakistan also reported triplets during this study period.
Table 1. Rates of multiple gestation pregnancies by study site.
| Total | Argentina | Guatemala | Kenya | Zambia | India Belgaum |
India Nagpur |
Pakistan | |
|---|---|---|---|---|---|---|---|---|
| Pregnant Women (N) |
69,706 | 2,840 | 5,979 | 8,953 | 7,093 | 20,547 | 10,006 | 14,288 |
| Multiple Gestation pregnancies N (Rate/1000) |
637 (9.1) | 21 (7.4) | 48 (8.0) | 131 (14.6) | 65 (9.2) | 134 (6.5) | 85 (8.5) | 153 (10.7) |
| Twin pregnancies N (Rate/1000) |
630 (9.0) | 21 (7.4) | 48 (8.0) | 128 (14.3) | 64 (9.0) | 133 (6.5) | 85 (8.5) | 151 (10.6) |
| Triplet pregnancies N (Rate/1000) |
7 (0.1) | 0 (0.0) | 0 (0.0) | 3 (0.3) | 1 (0.1) | 1 (0.0) | 0 (0.0) | 2 (0.1) |
Figure 1.
Odds ratio for a multiple gestation pregnancy by site, relative to India-Belgaum
Table 2 summarizes the characteristics of the mothers, location and mode of delivery, presence of birth attendant, and maternal outcomes, compared for by study site. The mean maternal age was higher among mothers with multiple pregnancies compared to mothers with singleton pregnancies (26±5 years vs. 24±5 years respectively). Similarly mothers with multiple pregnancies had a higher median parity (p<0.001). The multiple pregnancy mothers were more likely to have delivered in a health care facility as compared to singleton pregnancy mothers (70.3% vs. 66.2% respectively, p<0.001) and more likely to be attended by skilled health personnel (70.8% vs. 66.6%, p<0.001). Likewise, they were more likely to be delivered by caesarian section (18.1% vs. 9.5%, p<0.001).
Table 2. Maternal demographic by gestational status.
| Multiple Gestation | Single Gestation | P-value* | |
|---|---|---|---|
| N | 637 | 68,987 | |
| Maternal Age, N | 636 | 68,793 | <.0001 |
| Mean ± SD | 26.1 ± 5.4 | 24.5 ± 5.1 | |
| Parity, N | 637 | 68,816 | <.0001 |
| Median (P25, P75) | 2.0 (0.0, 3.0) | 1.0 (0.0, 3.0) | |
| Delivery Location, N (%) | 636 | 68,921 | <.0001 |
| Hospital | 335 (52.7) | 28,114 (40.8) | |
| Clinic | 112 (17.6) | 17,502 (25.4) | |
| Home/Other | 189 (29.7) | 23,305 (33.8) | |
| Delivery Attendant, N (%) | 637 | 68,977 | <.0001 |
| Physician | 304 (47.7) | 24,288 (35.2) | |
| Nurse/Nurse Midwife/HW | 147 (23.1) | 21,659 (31.4) | |
| TBA | 148 (23.2) | 19,313 (28.0) | |
| Family | 38 (6.0) | 3,717 (5.4) | |
| Delivery Mode, N (%) | 637 | 68,972 | <.0001 |
| Vaginal/Vaginal Assisted | 522 (81.9) | 62,429 (90.5) | |
| C-Section | 115 (18.1) | 6,543 (9.5) | |
| Maternal Outcome at 6 Weeks, N (%) | 598 | 67,005 | 0.2 |
| Died | 3 (0.5) | 93 (0.1) | |
| Alive | 595 (99.5) | 66,912 (99.9) | |
| Mother hospitalized after last visit, N (%) | 630 | 67,901 | 0.1 |
| Yes | 5 (0.8) | 174 (0.3) | |
| No | 625 (99.2) | 67,727 (99.7) |
Adjusted for site
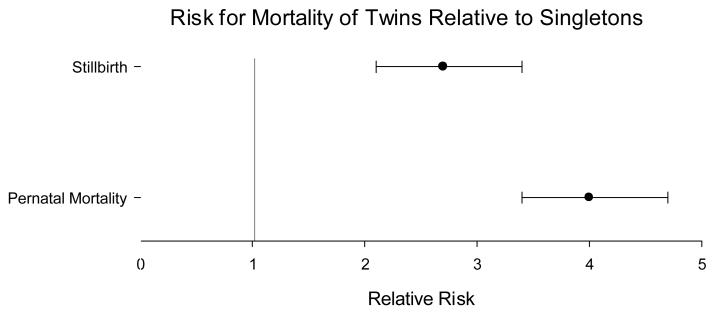
Tables 3A and 3B provide the fetal and infant outcomes by singleton vs. multiple gestation status. Compared to singletons, multiple gestation infants were at significantly higher risk of stillbirth (RR 3.2, 95% CI 2.4, 4.2) and of death before perinatal visit (RR 7.7, 95% CI 6.2, 9.6) (Table 3A). The mean gestational age, determined by LMP or best obstetrical estimate(8), for those with multiple pregnancies was 35.8 weeks compared to those with singleton of 38.7 weeks.The relative risk (95% CI) for stillbirth was 2.7 (2.1, 3.4) and for PMR was 4.0 (3.4, 4.7) compared to singletons, both p<0.0001 (Figure 2).Of the twin infants, 287 (47%) were male and 326 (53%) were female. 235 (38%) of the twins were gender discordant, while 378 (62%) were gender concordant. Males were at higher risk for all measures of mortality except stillbirth (Table 3B).
Table 3A. Perinatal outcomes for multiple vs. singleton gestation.
| Multiple Gestation |
Single Gestation |
Relative Risk (95% CI)* |
P-Value | |
|---|---|---|---|---|
| Total Infants, N | 1,268 | 68,988 | ||
| Birth Outcome, N (%) | <.0001 | |||
| Stillbirth | 99 (7.8) | 2,008 (2.9) | 3.2 (2.4, 4.2) | |
| Born alive, died Before perinatal visit |
160 (12.6) | 1,338 (1.9) | 7.7 (6.2, 9.6) | |
| Alive at perinatal visit | 1,009 (79.6) | 65,640 (95.1) | 1.00 | |
| Gestational age†, N | ||||
| Mean ± SD | 35.8 ± 5.2 | 38.7 ± 4.4 | <.0001 |
Adjusted for site
determined by last menstrual period or best obstetric estimate if LMP unknown(8)
Table 3B. Twin Fetal and Neonatal Outcomes by Gender.
| Outcome | Gender | RR (95% CI)* | |
|---|---|---|---|
| Male | Female | ||
| Perinatal Mortality, N (%) | 140 (218.8) | 100 (165.6) | 1.32 (1.04, 1.67) |
| Stillbirths, N (%) | 51 (79.7) | 41 (67.9) | 1.17 (0.74, 1.86) |
| Early Neonatal Mortality, N (%) | 89 (152.4) | 59 (107.9) | 1.40 (1.06, 1.84) |
| Neonatal Mortality at 6 weeks, N (%) | 119(203.8) | 81 (148.1) | 1.37 (1.07, 1.75) |
Adjusted for site
Figure 2.
Odds ratio for mortality of twins relative to singletons*
* Odds ratios were estimated by GEE binomial models adjusting for multiple gestation and site.
Finally, we developed a model to evaluate the association of technical delivery characteristics with outcomes of multiple gestations. Delivery in a health facility was not associated with a statistically significant decreased risk of perinatal mortality (Table 4). On the other hand, physician attended delivery was associated with a slightly decreased perinatal mortality risk (Relative Risk 0.9 [CL 0.8, 1.0], p<0.05).
Table 4. Relative risk for technical delivery characteristics.
| Explanatory Variables | P-Value (Wald) | Relative Risk for a 10% increase |
|---|---|---|
| Study site | 0.07 | -- |
| % Physician deliveries | 0.04 | 0.9 (0.8, 1.0) |
| % Hospital deliveries | 0.7 | 1.0 (0.9, 1.1) |
| % C-Section deliveries | 0.4 | 1.1 (0.8, 1.6) |
DISCUSSION
Our study is among the first prospective, population-based studies to examine the rates of multiple birth and their outcomes in low-resource settings. We enrolled approximately 70,000 pregnant women, of which 1% had a multiple gestation. We found significantly higher risks of stillbirth, perinatal mortality and neonatal death among multiples.
Many complications occurring in multiple gestation pregnancies might be prevented with proper utilization of antenatal services, early diagnosis of multiple pregnancies, good maternal nutrition and utilization of health services for delivery(13). However, in low-income countries, many women especially in rural settings, do not attend antenatal clinic throughout pregnancy(6, 14, 15). In these geographic areas, there are also few ultrasound facilities that would facilitate early detection of multifetal pregnancies.
In this study, one-third of mothers delivered at home with the help of unskilled birth attendants. At the time of delivery (the intrapartum period) most of these pregnancies are diagnosed as multiple gestation. There is an increasing emphasis on discouraging home births, especially when delivery is accomplished by unskilled birth attendants(16, 17). The two Indian sites had much higher rates of hospital delivery and skilled attendants than did either of the two African sites. In spite of this, the perinatal and neonatal mortality rates for twins were higher in the Indian sites than in either Kenya or Zambia. These data suggest that merely moving deliveries from homes into facilities is unlikely to reduce perinatal mortality sufficiently to reach the MDG4 goal to reduce childhood mortality. Rather, increased attention, resources, and training may need to be focused on the obstetric and neonatal care provided within health facilities if we are to reach achieve these goals. This is clearly an hypothesis that needs further, well controlled study.
Multiple pregnancies are an important risk factor for neonatal mortality in low-income countries. Identification of multiple fetuses early in pregnancy to enhance planning for delivery and postnatal care may be important to reduce neonatal mortality.
Acknowledgements
Support for this project came from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), part of the National Institutes of Health within the U.S. Department of Health and Human Services by grants U01 HD040477, U01 HD043464, U01 HD040657, U01 HD042372, U01 HD040607, U01 HD058322, U01 HD058326, and U01 HD040636.
References
- 1.Public Health Agency of Canada . Canadian Perinatal Health Report, 2008 Edition. Ottawa: 2008. [Google Scholar]
- 2.U.S. Census Bureau . Statistical Abstract of the United States. 2007. [Google Scholar]
- 3.Doyle P. The outcome of multiple pregnancy. Hum Reprod. 1996;11(Suppl 4):110–7. doi: 10.1093/humrep/11.suppl_4.110. discussion 8-20. [DOI] [PubMed] [Google Scholar]
- 4.Mathews TJ, Minino AM, Osterman MJ, Strobino DM, Guyer B. Annual summary of vital statistics: 2008. Pediatrics. 2011;127:146–57. doi: 10.1542/peds.2010-3175. [DOI] [PubMed] [Google Scholar]
- 5.Powers WF, Kiely JL. The risks confronting twins: a national perspective. Am J Obstet Gynecol. 1994;170:456–61. doi: 10.1016/s0002-9378(94)70211-x. [DOI] [PubMed] [Google Scholar]
- 6.van Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, Rosen DH, et al. Use of antenatal services and delivery care among women in rural western Kenya: a community based survey. Reprod Health. 2006;3:2. doi: 10.1186/1742-4755-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mathews TJ, Minino AM, Osterman MJK, Strobino DM, Guyer B. Annual Summary of Vital Statistics: 2008. Pediatrics. 2011;127:146–57. doi: 10.1542/peds.2010-3175. [DOI] [PubMed] [Google Scholar]
- 8.Belizan JM, McClure EM, Goudar SS, Pasha O, Esamai F, Patel A, et al. Neonatal Death in Low-to Middle-Income Countries: A Global Network Study. American journal of perinatology. 2012 doi: 10.1055/s-0032-1314885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kogan MD, Alexander GR, Kotelchuck M, MacDorman MF, Buekens P, Martin JA, et al. Trends in twin birth outcomes and prenatal care utilization in the United States, 1981-1997. JAMA: the journal of the American Medical Association. 2000;284:335–41. doi: 10.1001/jama.284.3.335. [DOI] [PubMed] [Google Scholar]
- 10.Suri K, Bhandari V, Lerer T, Rosenkrantz TS, Hussain N. Morbidity and mortality of preterm twins and higher-order multiple births. Journal of perinatology: official journal of the California Perinatal Association. 2001;21:293–9. doi: 10.1038/sj.jp.7200492. [DOI] [PubMed] [Google Scholar]
- 11.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2004 period linked birth/infant death data set. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2007;55:1–32. [PubMed] [Google Scholar]
- 12.Habib NA, Dalveit AK, Mlay J, Oneko O, Shao J, Bergsjo P, et al. Birthweight and perinatal mortality among singletons and twins in north-eastern Tanzania. Scandinavian journal of public health. 2008;36:761–8. doi: 10.1177/1403494808089559. [DOI] [PubMed] [Google Scholar]
- 13.Chamberlain G. ABC of antenatal care. Multiple pregnancy. BMJ. 1991;303:111–5. doi: 10.1136/bmj.303.6794.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ornella Lincetto SM-A, Patricia Gomez, Stephen Munjanja. Antenatal Care. In: Lawn J, Kerber K, editors. Opportunities for Africa’s Newborns: Practical data, policy and programmatic support for newborn care in Africa. WHO; Capetown: 2006. [Google Scholar]
- 15.Mwaniki PK, Kabiru EW, Mbugua GG. Utilisation of antenatal and maternity services by mothers seeking child welfare services in Mbeere District, Eastern Province, Kenya. East Afr Med J. 2002;79:184–7. doi: 10.4314/eamj.v79i4.8875. [DOI] [PubMed] [Google Scholar]
- 16.Stanton C. Steps towards achieving skilled attendance at birth. Bulletin of the World Health Organization. 2008;86:242–3. doi: 10.2471/BLT.08.052928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Skilled birth attendants. http://www.who.int/maternal_child_adolescent/topics/maternal/skilled_birth/en/index.html.