Abstract
Purpose of the Study: To estimate the prevalence of culture change practice in U.S. nursing homes (NHs) and examine how state Medicaid policies may be associated with this prevalence. Design and Methods: In 2009/2010, we conducted a survey of a stratified proportionate random sample of NH directors of nursing (DONs) and administrators (NHAs) at 4,149U.S. NHs; contact was achieved with 3,695. Cooperation rates were 62.6% for NHAs and 61.5% for DONs. Questions focused on NH (physical) environment, resident-centered care, and staff empowerment domains. Domain scores were created and validated, in part, using qualitative interviews from 64 NHAs. Other NH covariate data were from Medicare/Medicaid surveys (Online Survey, Certification and Reporting), aggregated resident assessments (Minimum Data Set), and Medicare claims. Medicaid policies studied were a state’s average NH reimbursement rate and pay-for-performance (P4P) reimbursement (including and not including culture change performance measures). Multivariate generalized ordered logit regressions were used. Results: Eighty-five percent of DONs reported some culture change implementation. Controlling for NH attributes, a $10 higher Medicaid rate was associated with higher NH environment scores. Compared with NHs in non-P4P states, NHs in states with P4P including culture change performance measures had twice the likelihood of superior culture change scores across all domains, and NHs in other P4P states had superior physical environment and staff empowerment scores. Qualitative interviews supported the validity of survey results. Implications: Changes in Medicaid reimbursement policies may be a promising strategy for increasing culture change practice implementation. Future research examining NH culture change practice implementation pre-post P4P policy changes is recommended.
Key Words: Nursing homes, Culture change, Medicaid policy, Pay-for-performance
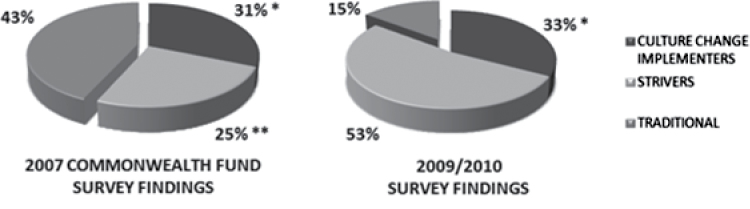
For over two decades, a movement to transform nursing homes (NHs) into person-centered homes has been occurring in the United States (Koren, 2010). This “culture change movement” aims to deinstitutionalize NH environments and individualize care for NH residents, and advocates for a less hierarchical structure that better values workers. Key principles of culture change include resident-directed care and activities; close relationships between residents, family members, staff, and community; empowerment of staff; management that enables collaborative and decentralized decision making; a systematic process for continuous quality improvement; and living environments that are designed to be homelike rather than institutional (Colorado Foundation for Medical Care, 2006). By 2007, a Commonwealth Fund survey found 31% of NH directors of nursing (DONs) nationally reported culture change “completely” or “for the most part” described their facilities; however, 43% reported little or no culture change implementation and no leadership commitment to adoption (Doty, Koren, & Sturla, 2008).
Although there are comprehensive NH culture change models such as the “Eden Alternative” (Thomas, Weiner, & Ronch, 2003) and the “Green House” model (Rabig, Thomas, Kane, Cutler, & McAlilly, 2006), NHs often do not implement a comprehensive model per se but instead select culture change practices based on their unique characteristics and needs (Chapin, 2006). Also, more complex culture change practices (such as creating self-managed work teams) are implemented in NHs with longer versus shorter durations of culture change implementation (Sterns, Miller, & Allen, 2010). Therefore, the practices exemplifying NH culture change efforts vary across facilities.
Although more and more rigorous research is needed (Rahman & Schnelle, 2008; Weiner, Freiman, & Brown, 2007; Zimmerman, 2003), studies have supported the benefits of NH culture change models and practices. For example, the Green House model of culture change has been shown to be associated with higher levels of quality of resident care and life (Kane, Lum, Cutler, Degenholtz, & Yu, 2007) and greater family satisfaction (Lum, Kane, Cutler, & Yu, 2008). Increased staff empowerment has also been supported as being beneficial (Loe & Moore, 2012), and research has shown staff practices aligned with culture change are positively associated with staff outcomes (Anderson, Corazzini, & McDaniel, 2004; Bishop, Squillace, Meagher, Anderson, & Wiener, 2009). Although existing research has not been sufficiently rigorous to support a “best practice” recommendation (Rahman & Schnelle, 2008), enthusiasm and support for NH culture change adoption has accelerated, probably, in part, given its strong face validity.
Since the 2007 national survey, numerous efforts by the Pioneer Network, the Advancing Excellence in America’s Nursing Homes Campaign (2012; supported by the American Health Care Association, Leading Age, and numerous other prominent organizations), state culture change coalitions, and the Centers for Medicare and Medicaid Services (CMS) have continued to support and promote culture change adoption. Notably, in 2009, CMS issued new interpretive guidelines (for use during Medicare/Medicaid inspections) calling for more homelike environments in NHs and confirming that regulations emanating from the Omnibus Budget Reconciliation Act of 1987 support the transformation to resident-centered care (Center for Medicare & Medicaid Services, 2009). Also, CMS’s “Eighth Scope of Work” promoted culture change by requiring state quality improvement organizations to work with NHs on projects that aimed to improve an organization’s culture (Koren, 2010). In addition to these efforts, because state variation in culture change adoption has been observed (Koren, 2010; Sterns et al., 2010), of interest was the role states and their Medicaid reimbursement policies may have played in promoting adoption/implementation.
Medicaid is an important payer of NH care, with Medicaid residents representing 65% of all bed days (Werner, Tamara Konetzka, & Liang, 2010). Previous research has shown Medicaid reimbursement policy and rates influence NH care and management decisions. Differing policies and rates have been associated with differing NH hospitalization rates (Intrator et al., 2007). Also, changes in state Medicaid reimbursement policies and rates have resulted in changes in NH hospice use (Miller, Gozalo, Lima, & Mor, 2011), staffing levels (Feng, Grabowski, Intrator, Zinn, & Mor, 2008), resident acuity (Werner et al., 2010), and outcomes (Mor et al., 2011). Considering this, NHs in states with higher Medicaid NH payment rates and with pay-for-performance (P4P) programs that incentivize higher quality and culture change practice implementation (i.e., practices aligned with resident-centered care, staff empowerment, and home environments; Arling, Job, & Cooke, 2009; Werner et al., 2010) may have implemented more culture change practices. In non-NH settings, P4P programs have been associated with some (modest) quality improvements (Petersen, Woodard, Urech, Daw, & Sookanan, 2006), and in a NH study, Medicaid P4P program was associated with improved access and outcomes (Norton, 1992).
This study uses a mixed methods approach to understand the implementation of culture change practices in U.S. NHs. The overall goals were to estimate the prevalence of culture change practices in U.S. NHs and to identify the NH attributes and Medicaid reimbursement policy associated with varying levels of practice implementation. Additionally, through interviews, we sought to expand our understanding of the facilitators and barriers to implementation as well as to validate survey findings and enhance their interpretation (Shield, Miller, Looze, Tyler, & Lepore, 2013).
Theoretical Framework and Conceptual Model
Motivating this mixed methods research is Roger’s Diffusion of Innovation (DOI) theory (Rogers, 2003). DOI theory, while focusing on the individual, has been used to understand adoption of innovation by health care organizations (Rahimi, Timpka, Vimarlund, Uppugunduri, & Svensson, 2009) and NHs (Kovach, Morgan, Noonan, & Brondino, 2008). Knowledge from DOI theory teaches that positive (initial) perceptions of an innovation account for 49%–87% of the variance in its rate of adoption (Rogers, 2003). A momentum in adoption occurs as adoption starts to catch on, due, in part, to the interaction between early adopters and the next wave of adopters (the early majority); the early adopters and early majority account for 50% of potential adopters (Berwick, 2003; Rogers, 2003). Based on the 2007 Commonwealth survey (Doty et al., 2008), culture change adoption momentum had occurred by 2007 because 57% of surveyed NHs were committed to or had at least partially implemented culture change. According to DOI theory, therefore, nonadopting NHs in 2007 would subsequently be considered either “later majority adopters” or “laggards.” The later majority adopters are more skeptical, have a lower tolerance for uncertainty, and lower economic resources, whereas laggards are suspicious, traditional, more isolated, and have precarious economic situations (Rogers, 2003).
Some organizations will be more likely to be innovators (the first to attempt an innovation) or early adopters, whereas others will be more likely to be in the early majority, late majority, or to be laggards. Regardless, all organizations will need to be persuaded that adoption is in their best interests and appropriate for addressing their agenda/problem(s). For NHs, this persuasion (from peers/leadership, researchers, consumers, regulators, and others) can remove the uncertainty accompanying an innovation by providing reassurance that desired outcomes such as higher quality of resident care and quality of life and improved satisfaction of staff and families are feasible, and that the innovation would not have unexpected consequences and/or be costly or incompatible with regulatory oversight. Considering the CMS support for NH culture change (which provides persuasive motivation to NHs) and the numerous efforts to promote and support its use, we expected our survey (reflecting practice primarily in late 2009 and 2010) would show greater culture change implementation than was observed in 2007 (Doty et al., 2008). Also, because we believed the presence of Medicaid P4P programs would provide persuasive motivation for NHs to adopt culture change, we hypothesized that NHs in states with Medicaid P4P programs would have a greater prevalence of culture change practice implementation compared with those in non-P4P states. Additionally, compatible with DOI theory, we hypothesized that this difference would be even greater when P4P programs include culture change performance measures because concerns about incompatibility with regulatory oversight would be minimized; such incompatibility has been cited as an adoption barrier (Miller et al., 2011). Furthermore, based on previous research showing higher Medicaid rates are associated with higher quality processes and outcomes (Feng et al., 2008; Intrator et al., 2007; Miller et al., 2011; Mor et al., 2011), we hypothesized that NHs in states with higher Medicaid rates would have greater implementation of culture change practices.
Methods
NH Survey Instruments
This research is part of a larger program project comprised of four studies dependent upon NH DON and NHA survey data. Therefore, a preliminary study goal was to identify a parsimonious set of survey items. To accomplish this, we focused on identifying previously used survey items with good measurement properties and construct validity. To this end, we interviewed experts who had conducted NH culture change surveys (Bott et al., 2009; Doty et al., 2008; Mueller, 2007). Through the information shared by these experts, as well as a comprehensive review of NH culture change literature (Colorado Foundation for Medical Care, 2006), we identified the key domains to be measured and survey items for testing; most items chosen had validity support (Bott et al., 2009; Mueller, 2007). The three domains chosen for study were (a) a NH’s (physical) environment, (b) staff empowerment, and (c) resident choice and decision making (i.e., resident-centered care). Also, as done in two previous surveys (Bott et al., 2009; Doty et al., 2008), we included a single question to capture the DON’s perception of the extent of their NH’s implementation of culture change/resident-centered care (see Discussion section).
To reduce measurement error and increase data validity, cognitive-based interviews of the draft survey items were conducted with NHAs and DONs. In all cases, interviews were structured, and focused probing techniques were used; a “thinking out loud” approach was applied (Jobe & Mingay, 1989). Three rounds of cognitive-based interviews occurred, with the final two following survey revisions. Further details of this testing are described elsewhere (Tyler et al., 2011). Revised survey instruments and administration techniques were pilot tested and revised as needed (Clark et al., 2011).
Survey Sample
The surveys developed were administered to a stratified, proportionate random sample of DONs and NHAs at 4,149U.S. NHs; contact was achieved at 3,695 of these facilities. Surveys were completed online, by mail, or by phone between August 2009 and April 2011 (only 2.9% completed in 2011). Cooperation rates (i.e., proportion of responses when contact with a NHA or DON was achieved) were 62.6% for NHAs (n = 2,215) and 61.55% for DONs (n = 2,164). Survey weights were developed to adjust for the stratified sample design; therefore, generalizations at the national level can be made. Abbreviated surveys containing a subset of questions were offered to respondents who would not have otherwise completed the survey. A small number of these short surveys were completed by DONs (122; 5.6% of 2,165) and NHAs (55; 2.5% of 2,219). Analyses found no significant differences between respondents who answered abbreviated versus full surveys, suggesting no bias exists. However, the 122 short DON surveys lacked data needed to derive the resident-centered domain score, and the 55 short NHA surveys lacked data to derive the NH environment score. Starting Ns, therefore, were 2,164 for NH environment, 2,043 for resident-centered care, and 2,219 for staff empowerment; Ns for multivariate analyses were 2,020, 1,907, and 2,072, respectively (see Table 1).
Table 1.
Final Samples Numbers—Regression Models
| Exclusions due to missing data | Nursing home environment | Resident-centered care | Staff empowerment |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Total respondents to surveys which included domain items of interest | 2,164 (100%) | 2,043 (100%) | 2,219 (100%) |
| Missing > 2 survey items needed for domain score | 69 (3.1%) | 48 (2.2%) | 70 (3.2%) |
| Missing survey NHA and/or DON tenure/turnover items | 33 (1.5%) | 40 (2.0%) | 32 (1.4%) |
| Missing OSCAR/county data | 42 (1.9%) | 48 (2.3%) | 45 (2.0%) |
| Final model (N) | 2,020 | 1,907 | 2,072 |
Notes: DON = director of nursing; NHA = nursing home administrator; OSCAR = Online Survey, Certification and Reporting.
Variables of Interest and Other Data Sources
Culture Change Practices.
As done in previous surveys (Bott et al., 2009; Doty et al., 2008), DONs were asked a single question about their NH’s implementation of culture change. First, they were provided with the following definition: “Culture change or resident-centered care is an effort to make a NH less like an institution and more like a home. Core values include: choice for residents, improving quality of care, staff empowerment, and creating a homelike setting.” Then, they were asked to choose one of the following response categories: (a) there is no discussion around culture change; (b) culture change is under discussion, but we have not changed the way we take care of residents; (c) culture change has partially changed the way we care for residents in some or all areas of the organization; (d) culture change has completely changed the way we care for residents in some areas of the organization; (e) culture change has completely changed the way we care for residents in all areas of the organization; or (f) other (please specify). Investigators reviewed and agreed upon the coding of the “Other” responses (n = 40) into one of the above categories. Similar to Doty and colleagues (2008), we considered those NHs with no discussion, or discussion only, as “Traditional” NHs, those who reported culture change has partially changed the NH as “Strivers,” those who reported complete change in some areas as “Partial Adopters,” and those who reported complete change in all areas as “Complete Adopters.”
The NH environment domain included eight items, which measured facilities’ efforts at making the NH’s environment more homelike through practices such as having any residents living in self-contained (including kitchen and dining facilities) small households and/or neighborhoods, having private rooms, and having open dining policies and other homelike characteristics. The resident-centered care domain included four questions assessing residents’ involvement in determining their schedules, activities, and care. The staff empowerment domain included seven items assessing staff participation in management and decision making as well as questions about staff recognition. Survey items, response categories, and the allocation of item point values are presented in Supplementary Appendices A and B. A copy of the culture change survey is available upon request.
For each domain, item values were summed to create NH physical environment, resident-centered care, and staff empowerment domain scores with total possible scores of 22, 8, and 21, respectively. In cases where one or two (scaled) items in a domain score were missing, the modal responses for the other items in the score were imputed. Imputations were performed for a very small proportion of scores (28 environment scores, 66 staff scores, and 24 resident scores).
State Policies and Covariates.
A 2011 survey administered to state Medicaid officials by our institution provided data on a state’s average Medicaid NH reimbursement rate in 2009. Data on states having Medicaid NH P4P reimbursement programs in 2009 and P4P programs including culture change measures were obtained from a study by Werner and colleagues (2010). However, we only included states with a NH per diem add on, thus excluded Vermont as it provided a bonus to qualifying NHs. This decision was consistent with our institution’s survey response from Vermont. In 2009, seven states (Colorado, Georgia, Iowa, Kansas, Ohio, Oklahoma, and Utah) had Medicaid NH P4P programs, and three states included culture change measures in their programs (Colorado, Oklahoma, and Utah). These culture change measures targeted the homelike quality of the environment, employee satisfaction, and/or resident choice and autonomy (Werner et al., 2010).
NH survey data were merged with variables derived from Minimum Data Set (MDS), Medicare claims, and Online Survey, Certification and Reporting (OSCAR) data. NH OSCAR data closest in time to the date of a NH’s survey response were used. Resident aggregated data were from the 2009 MDS, and the 2009 MDS merged with Medicare claims. Supplementary Appendix C lists the covariates included in the multivariate models and describes their coding and the data source(s) from which they were derived.
Analytic Strategy.
Proportions and means were used to describe NHs’ involvement in culture change. We used generalized ordered logit regression models to estimate the independent associations between Medicaid policies and higher domain scores. NH domain scores were categorized into approximate quartiles for regression analyses. For all analyses, we applied probability weights to adjust for the stratified sampling design. Statistical analyses were conducted using Stata, version 11 (“Stata: Data Analysis and Statistical Software,” 2011).
Interviews of NH Administrators
Semistructured interviews of NHAs were completed. A total of 64 NHAs at NHs that had participated in the quantitative survey were interviewed. The sampling frame for these qualitative interviews was designed to include NHs in states where higher adoption of culture change practices had previously been reported (Doty et al., 2008) and included at least two states from each of the four major U.S. geographic regions.
The semistructured interview format ensured that the same basic questions were asked of each NHA, but it also allowed for the NHAs to tell their individual stories (Bernard, 2011; Curry, Shield, & Wetle, 2006). NHAs were first asked to describe any practices or changes they had implemented to improve quality of care or quality of life for their facility’s residents and/or staff, as well as any changes made to the physical environment. Follow-up questions were asked to gather information about the motivations behind these changes; the process of implementing these changes, including the facilitators and barriers to making these changes; the responses of residents, staff, and families to these changes; and other outcomes perceived to be associated with changes made. Immediately after interview completion, and based on the interview content, the interviewer rated each facility on a scale from 1 to 5 (1 = not at all; 5 = very much) representing the NH’s level of involvement in each domain of culture change (resident-centered care, staff empowerment, and NH environment).
Standard qualitative methods for analysis were used and are described in depth elsewhere (Shield et al., 2013). In this article, findings from the qualitative interviews are triangulated with results from the quantitative survey to validate survey findings and to aid in their interpretation (Denzin, 1978; Mark & Shotland, 1987; Rossman & Wilson, 1985). More detailed information on the identified themes can be found elsewhere (Shield et al., 2013).
Results
NH Involvement in Culture Change
Eighty-five percent of the DON respondents reported at least partial involvement in NH culture change, whereas 15% reported their facilities to be “traditional” facilities—where culture change is not or is only under discussion (see Figure 1). As shown, the 2007 Commonwealth culture change survey found these levels of involvement in 2007 to be 57% and 43%, respectively. Not shown in Figure 1 is that only 13% of DONs in 2009/2010 reported culture change had “completely changed the way they care for residents” in all areas of the NH; this compares with 5% in 2007.
Figure 1.
Culture change implementation reported by nursing home directors of nursing: 2007 and 2009/2010. *Implementers in 2007 survey included facilities where culture change completely or for the most part describes the facility. For 2009/2010 survey, implementers included 12% that reported culture change “completely changed the way they care for residents” in all areas of the organization and 19% that reported culture change “completely changed the way they care for residents” in some areas of the organization. 2009/2010 percentages are rounded. The 2007 pie chart is from Doty et al. (2008). **Strivers also included nursing homes with no implementation but with leadership reported to be extremely or very committed to implementation.
Reliability and Validity of Culture Change Practice Measures
Table 2 describes the culture change domain scores and reports the Chronbach’s alphas.
Table 2.
Culture Change Domain Scores and Reliability
| Domain | Number of items | Total possible score | Mean score (SD) | Range of scores | Internal consistency reliability | |
|---|---|---|---|---|---|---|
| Cronbach’s alpha | Item-total correlation (range) | |||||
| Nursing home environment (n = 2,095) | 8 | 22 | 6.45 (3.94) | 0–22 | .61 | 0.22–0.44 |
| Resident-centered care (n = 1,995) | 4 | 8 | 5.20 (1.81) | 0–8 | .49 | 0.23–0.37 |
| Staff empowerment (n = 2,149) | 7 | 21 | 10.45 (3.19) | 2–21 | .62 | 0.23–0.45 |
Reliability coefficients for NH environment and staff empowerment were acceptable considering the small number of items within each domain (α = .61 and α = .62, respectively). For the resident-centered domain, the alpha was .48, which is likely reflective of the fact that this domain included only four survey items. Despite the lower alpha, the domain was retained given its strong face validity (and previous validity findings for the questions asked; Bott et al., 2009; Mueller, 2007).
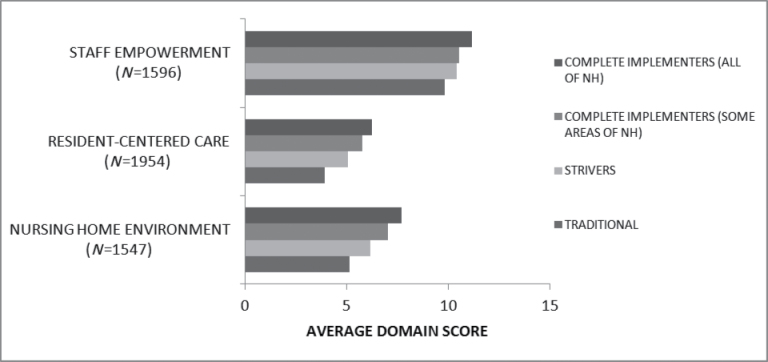
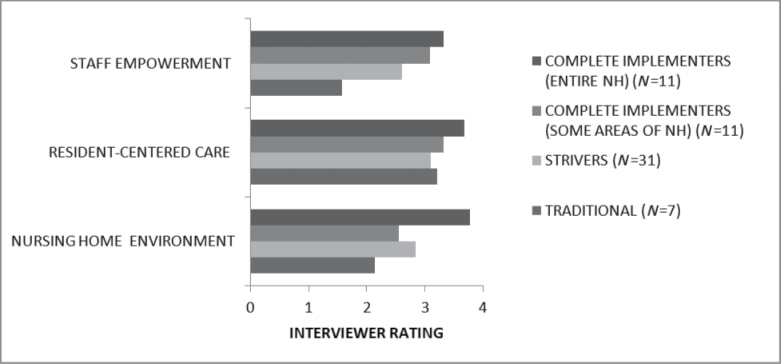
For NHs with both a NHA and DON survey respondent (and a nonmissing response to the single DON implementation question), Figure 2 shows culture change domain scores are consistently higher when DONs reported greater culture change implementation, supporting the internal consistency of survey responses. Also, survey validity is supported by comparing the DON’s response to this question and the qualitative interview rating scores (as assigned by the interviewer; Figure 3). For all domains, interviewers assigned the highest interview scores to facilities with the most culture change involvement. The least interview/survey discrimination was observed for the resident-centered care domain and this may relate to the low number of questions in that domain (Figure 3).
Figure 2.
Average culture change domain scores by director of nursing’s response to culture change implementation question.
Figure 3.
Average qualitative interviewer rating (0–5) of culture change domain implementation by director of nursing response to culture change implementation question.
Characterization of Facilities in Domain Models
Table 3 presents descriptive statistics of the NHs in each domain model. Although the Ns of each model differ, the observed differences are small. Eighty-two percent of the NHs were in states with no NH P4P Medicaid reimbursement program, and 3%–4% in states with P4P reimbursement systems including culture change performance measures. The average Medicaid per diem rate was $160.
Table 3.
State Medicaid Policies and Nursing Homes and County Characteristics—Facilities in Domain Regression Modelsa
| Nursing home environment (n = 2,020) | Resident-centered care (n = 1,907) | Staff empowerment (n = 2,072) | ||||
|---|---|---|---|---|---|---|
| %/mean | SE | %/mean | SE | %/mean | SE | |
| Medicaid reimbursement policy/payment | ||||||
| Pay-for-performance reimbursement | ||||||
| None | 81.8% | 81.6% | 81.8% | |||
| Without culture change measures | 14.9% | 14.5% | 15.0% | |||
| With culture change measures | 3.2% | 3.8% | 3.3% | |||
| Average Medicaid daily rate (mean, SE) | 159.94 | 0.66 | 159.26 | 0.67 | 159.99 | 0.65 |
| Nursing home and county characteristics | ||||||
| Resident days on Medicare SNF care | 20.0% | 19.5% | 20.0% | |||
| Residents with Medicaid | 61.0% | 61.2% | 61.0% | |||
| Non-Hispanic Black | 10.4% | 10.1% | 10.4% | |||
| For-profit | 70.3% | 69.8% | 70.5% | |||
| Facility is part of chain | 55.7% | 53.9% | 55.7% | |||
| Facility has special care unit | 20.0% | 20.1% | 20.0% | |||
| Small facility (<50 beds) | 9.5% | 9.8% | 9.5% | |||
| Occupancy rate | 84.8% | 84.5% | 84.7% | |||
| Facility in rural county | 31.8% | 32.8% | 32.0% | |||
| County level Herfindahl index (mean, SE) | 0.21 | 0.01 | 0.21 | 0.01 | 0.21 | 0.01 |
| Administrator tenure (years; mean, SE) | 5.52 | 0.15 | 5.55 | 0.15 | ||
| Number of directors of nursing in past 2 years | ||||||
| 3 or more | 14.5% | 14.7% | ||||
| 2 | 27.6% | 27.6% | ||||
| 1 | 57.9% | 57.8% | ||||
| Director of nursing tenure (years; mean, SE) | 4.47 | 0.12 | ||||
Note: SNF = skilled nursing facility.
aWeighted analyses to adjust for the sampling design.
Multivariate Results
Controlling for NH attributes and compared with NHs in states with no NH P4P reimbursement, NHs in states with P4P reimbursement without inclusion of culture change measures had significantly higher odds of having NH environment domain scores in the top two quartiles (vs bottom two quartiles) or in the top quartile (vs other quartiles; Table 4). They also had significantly greater odds of having staff empowerment scores in the top three quartiles (vs the bottom quartile) or in the top quartile (vs the lower three quartiles). There were no significant differences between quartile comparisons when considering P4P reimbursement (not including culture change measures) and the resident-centered care domain. NHs in states with NH P4P systems that included culture change measures (compared with NHs in states with no P4P) had significantly greater odds of having higher scores across all domains, and when considering almost all quartile comparisons (Table 4). For example, NHs in these states (compared with those in states without P4P) had approximately double the odds of having NH environment and resident-centered care domain scores in the upper three quartiles versus the lowest quartile (adjusted odds ratio [AOR]: 2.1; confidence interval [CI]: 1.09, 3.86 and AOR: 1.9; 95% CI: 1.09, 3.25, respectively); they had over double the odds of having staff empowerment scores in the two highest versus two lowest quartiles (AOR: 2.4; CI: 1.39, 3.96). For each $10 in higher Medicaid NH per diem reimbursement within a state, NHs had significantly greater odds (AOR: 1.12; 95% CI: 1.0, 1.24) of having NH environment domain scores in the top three quartiles (vs the bottom quartile; Table 4).
Table 4.
Multivariate Ordered Logic Regression Resultsa
| Factors | Nursing home environment quartiles (n = 2,020) | Resident-centered care quartiles (n = 1,907) | Staff empowerment quartiles (n = 2,072) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2, 3, 4 vs 1 | 3, 4 vs 1, 2 | 4 vs 1, 2, 3 | 2, 3, 4 vs 1 | 3, 4 vs 1, 2 | 4 vs 1, 2, 3 | 2, 3, 4 vs 1 | 3, 4 vs 1, 2 | 4 vs 1, 2, 3 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Nursing home Medicaid reimbursement policy/payment | |||||||||
| No pay-for-performance | REF | REF | REF | REF | REF | REF | REF | REF | REF |
| Pay-for-performance (without culture change measures) | 1.26 (0.95, 1.67) | 1.57 (1.19, 2.06) | 1.50 (1.10, 2.05) | 0.89 (0.67, 1.18) | 1.01 (0.77, 1.32) | 0.93 (0.67, 1.3) | 1.61 (1.18, 2.19) | 1.13 (0.87, 1.47) | 1.35 (1.01, 1.79) |
| Pay-for-performance (with culture change measures) | 2.04 (1.08, 3.85) | 2.54 (1.49, 4.33) | 2.27 (1.27, 4.04) | 1.88 (1.09, 3.25) | 1.98 (1.2, 3.25) | 1.61 (0.94, 2.78) | 1.76 (0.94, 3.3) | 2.35 (1.39, 3.96) | 1.81 (1.06, 3.09) |
| Average state Medicaid payment (per $10 increments) | 1.11 (1.00, 1.24) | 1.20 (1.08, 1.33) | 1.08 (0.96, 1.21) | 1.03 (0.92, 1.14) | 1.04 (0.94, 1.16) | 1.11 (0.99, 1.25) | 0.97 (0.87, 1.08) | 0.89 (0.8, 0.98) | 0.84 (0.75, 0.94) |
Notes: Models also controlled for % resident days on Medicare SNF, % residents with Medicaid, % residents non-Hispanic Black, for-profit status, chain status, presence of any special care unit, size of facility (<50 beds), occupancy rate, location of facility in a rural county, county level Herfindahl index, administrator tenure, and DON tenure and turnover. DON = director of nursing; OR = odds ratio; SNF = skilled nursing facility.
aWeighted analyses to adjust for the sampling design.
Discussion
Reported NH involvement in culture change has increased substantially in a short period of time. In the 2007 Commonwealth Fund survey, only 56% of surveyed DONs in U.S. NHs reported any culture change implementation or leadership commitment to implementation (Doty et al., 2008); by late 2009/2010, 85% of DONs reported at least partial culture change implementation in some or all areas of the organization. However, in 2009/2010, only 13% reported culture change had completely changed the way the NH cared for residents in all areas of the NH; this compares with 5% in 2007. This research found state Medicaid NH reimbursement rates and P4P policies to be associated with the presence of culture change practices in NHs. NHs in states with P4P reimbursement systems that included culture change measures had higher culture change practice scores across all domains studied, and NHs in states with P4P reimbursement systems without culture change measures had higher NH environment and staff empowerment domain scores. Additionally, NHs in states with higher Medicaid reimbursement rates had higher NH environment domain scores. Although we cannot attribute cause and effect in this cross-sectional study, findings suggest Medicaid reimbursement generosity and P4P payment models may be one avenue for promoting the implementation of culture change in U.S. NHs.
Although there has been much growth in culture change practice implementation, it must be emphasized that the vast majority of NHs (72%) have only partially implemented these practices. A better understanding of what must occur and what factors are associated with NHs transitioning from partial to complete implementation is needed, and longitudinal research is required to gain this understanding. Also, study is needed on how the “laggard” NHs—the 15% of U.S. NHs where culture change is not or is only under discussion—can be persuaded and assisted in adopting culture change practices. One promising approach for helping low-achieving NHs to improve performance was initiated through the Advancing Excellence’s Local Areas Networks of Excellence and involved assistance by a “SWAT” team of consultants/colleagues (Brady & Frank, 2011). Similar efforts are likely needed.
As speculated, there was much growth in reported culture change implementation by DONs between 2007 and 2009/2010. In accordance with DOI theory (Rogers, 2003), many events and initiatives may have provided the peer and leadership persuasion needed to promote the decision to adopt and the resources to facilitate implementation; also, CMS’s demonstrated support of NH culture change may have allayed fears of “unexpected consequences.” Also, the influence of the Advancing Excellence Campaign may have facilitated implementation because it has provided resources, leadership, and guidance to NHs to assist them in improving clinical outcomes, enhancing quality of resident life, and achieving a happier, stronger, and more stable workforce since October 2006. In fact, by 2009, over half of U.S. NHs had participated in at least one of the nine Advancing Excellence goals (Advancing Excellence in America’s Nursing Homes Campaign, 2012). In addition to Advancing Excellence, 24 states by 2009 had functioning culture change coalitions that provided resources, workshops, and/or training to assist NHs in their effort to adopt culture change practices (Pioneer Network in Culture Change, 2009).
Interviews confirmed the importance of the above initiatives/efforts. For example, Medicare/Medicaid survey oversight was identified as being one motivator of the culture change adoption decision (Shield et al., 2013). Specifically, administrators discussed how they were experiencing or expecting more state oversight in relation to the creation of more homelike environments and resident-centered care.
The observed association between Medicaid NH P4P and the implementation of culture change practices was as we hypothesized. Of particular interest is the finding of greater effect sizes and the statistically significant association between resident-centered care practices and P4P when Medicaid programs included targeted culture change performance measures. In agreement with DOI theory (Rogers, 2003), it may be that when culture change is specifically targeted in P4P programs, NHs (in additional to responding to financial incentives) may also have more certainty that practice implementation is compatible with regulatory oversight.
The P4P findings are in agreement with a randomized controlled trial that showed Medicaid resident payment system incentives targeted to admissions, outcomes, and discharges resulted in significantly better Medicaid beneficiary access and outcomes and in significantly higher proportions of discharges made to appropriate (lower) care settings (Norton, 1992). As in Norton’s study, the targeting of culture change measures by Medicaid P4P programs in three states (Colorado, Oklahoma, and Utah) may have resulted in targeted culture change implementation; however, this cannot be confirmed in this cross-sectional study. The three states with targeted culture change measures included differing measures and weighting of measures. In interviews, administrators did not specifically mention P4P reimbursement systems in relation to culture change practice adoption. However, some of the reported “oversight” may have been related to P4P programs; in fact, in at least one P4P state with culture change measures (Colorado), on-site examinations to determine compliance were planned (Werner et al., 2010). To examine cause and effect, future research using pre-post designs and examining changes in the presence of Medicaid NH P4P programs as well as changes in the presence and weighting of culture change performance measures within these programs is warranted.
Higher average Medicaid NH per diem rates were associated with higher NH environment practice scores, but although the generosity of Medicaid rates has previously been found to be have been associated with NH care practices such as hospitalization rates (Intrator et al., 2007) and improvements in patient outcomes (Mor et al., 2011), we did not find this to be the case for resident-centered care and staff empowerment culture change practices. Administrator interviews provide insight into this finding because administrators noted few costs associated with implementation of many culture change practices, but did identify the costs associated with physical plant changes as a culture change barrier (Shield et al., 2013).
Limitations
This study has limitations that deserve comment. First, our measurement of the implementation of culture change practices focused on only three of the six domains suggested by the Colorado report (Colorado Foundation for Medical Care, 2006), and within each we included only between four and eight items, meaning our assessment of culture change practice implementation was not complete. Nonetheless, the scales used had good measurement properties, and items used had construct validity (Bott et al., 2009; Doty et al., 2008; Mueller, 2007). Also, we surveyed only DONs and NHAs and did qualitative interviews only of NHAs. Although responses may have differed between the two NH leaders, by asking different questions of the two respondents, we covered more information and fielded a large national study. Because we found good correspondence between the quantitative and qualitative data, regardless of information source, we feel comfortable with the validity of the data. Additionally, we did not assess in this cross-sectional study whether adopting culture change causes improvements in quality.
Conclusions
In summary, within a short period of time, there has been a substantial increase in reported implementation of culture change practices in U.S. NHs. This increase, in part, may be due to key national initiatives and to CMS’s demonstrated support of NH culture change. Also, given this study’s strong observed associations between greater implementation of culture change practices when NHs reside in Medicaid NH P4P states (vs non-P4P states), these P4P programs may have contributed to increased implementation. Given the recent increases in state Medicaid NH P4P programs and in Medicaid P4P programs incorporating culture change performance measures, research examining the effect of these Medicaid policy changes on subsequent NH culture change adoption is recommended. Also recommended is longitudinal research examining factors associated with changes in culture change practice implementation and the effect of such changes on quality outcomes.
Supplementary Material
Supplementary material can be found at: http://gerontologist.oxfordjournals.org.
Funding
This research was made possible by a grant from the Retirement Research Foundation (2008-086) and from the Shaping Long Term Care in America Project funded by the National Institute on Aging (P01AG027296). During this study, Drs. Lepore and Sterns were funded through the Agency for Healthcare Research and Quality (AHRQ) National Research Service Awards (NRSA) Post doctoral fellowship training grant (5T32HS000011).
Supplementary Material
References
- Advancing Excellence in America’s Nursing Homes Campaign (2012). For nursing homes Retrieved from http://www.nhqualitycampaign.org/star_index.aspx?controls=nursing_homes
- Anderson R. A., Corazzini K. N., McDaniel R. R., Jr (2004). Complexity science and the dynamics of climate and communication: Reducing nursing home turnover. The Gerontologist, 44, 378–388. 10.1093/geront/44.3.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arling G., Job C., Cooke V. (2009). Medicaid nursing home pay for performance: Where do we stand? The Gerontologist, 49, 587–595. 10.1093/geront/gnp044 [DOI] [PubMed] [Google Scholar]
- Bernard H. R. (2011). Research methods in anthropology: Qualitative and quantitative approaches (5th ed.). Lanham, MD: AltaMira Press; [Google Scholar]
- Berwick D. M. (2003). Disseminating innovations in health care. Journal of the American Medical Association, 289, 1969–1975. 10.1001/jama.289.15.1969 [DOI] [PubMed] [Google Scholar]
- Bishop C. E., Squillace M. R., Meagher J., Anderson W. L., Wiener J. M. (2009). Nursing home work practices and nursing assistants’ job satisfaction. The Gerontologist, 49, 611–622. 10.1093/geront/gnp040 [DOI] [PubMed] [Google Scholar]
- Bott M., Dunton N., Gajewski B., Lee R., Boyle D., Bonnel W. … Rachlin R. (2009). Culture change and turnover in Kansas nursing homes. Topeka, KS: Kansas Department on Aging [Google Scholar]
- Brady C., Frank B. (2011). Enhancing LANEs capacity to improve outcomes in critical access nursing homes: Project review, lessons, and recommendations Retrieved from http://www.bandfconsultinginc.com/Site/Critical_Access_and_Special_Focus_Facilities.html
- Center for Medicare & Medicaid Services (2009). CMS Manual System Pub. 100-07 State Operations Provider Certification. Appendix PP/§483.15(b)/Self-Determination and Participation/Tag F242 Washington, DC: Department of Health and Human Services; Retrieved from http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R48SOMA.pdf [Google Scholar]
- Chapin M. (2006). Creating innovative places: Organizational and architectural case studies of the culture change movement in long-term care (Doctoral dissertation, University of Wisconsin-Milwaukee; ). Retrieved from http://www.meldrenachapin.com/mchapin_dissertation_abstract.pdf [Google Scholar]
- Clark M., Rogers M., Foster A., Dvorchak F., Saadeh F., Weaver J., Mor V. (2011). A randomized trial of the impact of survey design characteristics on response rates among nursing home providers. Evaluation & The Health Professions, 34, 464–486. 10.1177/0163278710397791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colorado Foundation for Medical Care (2006). Measuring culture change: Literature review (Report No. PM-411-114 CO 2006). Retrieved from http://www.cfmc.org/files/nh/MCC%20Lit%20Review.pdf [Google Scholar]
- Curry L., Shield R., Wetle T. (2006). Improving aging and public health research: Qualitative and mixed methods. Washington, DC: American Public Health Association; [Google Scholar]
- Denzin N. K. (1978). The research act: An introduction to sociological methods (2nd ed.). New York: McGraw-Hill; [Google Scholar]
- Doty M. M., Koren M. J., Sturla E. L.(2008). http://www.commonwealthfund.org/Publications/Fund-Reports/2008/May/Culture-Change-in-Nursing-Homes--How-Far-Have-We-Come--Findings-From-The-Commonwealth-Fund-2007-Nati.aspx. http://www.commonwealthfund.org/Publications/Fund-Reports/2008/May/Culture-Change-in-Nursing-Homes--How-Far-Have-We-Come--Findings-From-The-Commonwealth-Fund-2007-Nati.aspx Culture change in nursing homes: How far have we come? Findings from the Commonweath Fund 2007 National Survey of Nursing Homes. Retrieved from.
- Feng Z., Grabowski D. C., Intrator O., Zinn J., Mor V. (2008). Medicaid payment rates, case-mix reimbursement, and nursing home staffing–1996-2004. Medical Care, 46, 33–40. 10.1097/MLR.0b013e3181484197 [DOI] [PubMed] [Google Scholar]
- Intrator O., Grabowski D. C., Zinn J., Schleinitz M., Feng Z., Miller S., Mor V. (2007). Hospitalization of nursing home residents: The effects of states’ Medicaid payment and bed-hold policies. Health Services Research, 42, 1651–1671. 10.1111/j.1475-6773.2006.00670.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobe J. B., Mingay D. J. (1989). Cognitive research improves questionnaires. American Journal of Public Health, 79, 1053–1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane R. A., Lum T. Y., Cutler L. J., Degenholtz H. B., Yu T. C. (2007). Resident outcomes in small-house nursing homes: A longitudinal evaluation of the initial Green House program. Journal of the American Geriatrics Society, 55, 832–839. 10.1111/j.1532-5415.2007.01169.x [DOI] [PubMed] [Google Scholar]
- Koren M. J. (2010). Person-centered care for nursing home residents: The culture-change movement. Health Affairs (Millwood), 29, 312–317. 10.1377/hlthaff.2009.0966 [DOI] [PubMed] [Google Scholar]
- Kovach C. R., Morgan S., Noonan P. E., Brondino M. (2008). Using principles of diffusion of innovation to improve nursing home care. Journal of Nursing Care Quality, 23, 132–139. 10.1097/01.NCQ.0000313762.79396.ec [DOI] [PubMed] [Google Scholar]
- Loe M., Moore C. D. (2012). From nursing home to Green House: Changing contexts of edlder care in the United States. Journal of Applied Gerontology, 31, 755–763. 10.1177/0733464811401022 [Google Scholar]
- Lum T. Y., Kane R. A., Cutler L. J., Yu T. C. (2008). Effects of Green House nursing homes on residents’ families. Health Care Financing Review, 30, 35–51 [PMC free article] [PubMed] [Google Scholar]
- Mark M. M., Shotland R. L. (1987). Alternative models for the use of multiple methods. New directions for program evaluation: Special Issue on Multiple Methods in Program Evaluation, 35, 95–100. 10.1002/ev.1461 [Google Scholar]
- Miller S. C., Gozalo P., Lima J. C., Mor V. (2011). The effect of Medicaid nursing home reimbursement policy on Medicare hospice use in nursing homes. Medical Care, 49, 797–802. 10.1097/Mlr.0b013e318223c0ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V., Gruneir A., Feng Z., Grabowski D. C., Intrator O., Zinn J. (2011). The effect of state policies on nursing home resident outcomes. Journal of the American Geriatrics Society, 59, 3–9. 10.1111/j.1532-5415.2010.03230.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller C. (2007). Nursing leadership and nursing home culture change. Paper presented at the Gerontological Society of America 60th Annual Scientific Meeting, San Francisco, CA [Google Scholar]
- Norton E. C. (1992). Incentive regulation of nursing homes. Journal of Health Economics, 11, 105–128 [DOI] [PubMed] [Google Scholar]
- Petersen L. A., Woodard L. D., Urech T., Daw C., Sookanan S. (2006). Does pay-for-performance improve the quality of health care? Annals of Internal Medicine, 145, 265–272 [DOI] [PubMed] [Google Scholar]
- Pioneer Network in Culture Change (2009). http://www.pioneernetwork.net/Data/Documents/2009StateCoalitionAccomplishments.pdf. http://www.pioneernetwork.net/Data/Documents/2009StateCoalitionAccomplishments.pdf 2009 state coalition accomplishments. Retrieved from .
- Rabig J., Thomas W., Kane R. A., Cutler L. J., McAlilly S. (2006). Radical redesign of nursing homes: Applying the Green House concept in Tupelo, Mississippi. The Gerontologist, 46, 533–539. 10.1093/geront/46.4.533 [DOI] [PubMed] [Google Scholar]
- Rahimi B., Timpka T., Vimarlund V., Uppugunduri S., Svensson M. (2009). Organization-wide adoption of computerized provider order entry systems: A study based on diffusion of innovations theory. BMC Medical Informatics and Decision Making, 9, 52. 10.1186/1472-6947-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A. N., Schnelle J. F. (2008). The nursing home culture-change movement: Recent past, present, and future directions for research. The Gerontologist, 48, 142–148. 10.1093/geront/48.2.142 [DOI] [PubMed] [Google Scholar]
- Rogers E. M. (2003). Diffusion of innovations (5th ed.). New York: Free Press; [Google Scholar]
- Rossman G. B., Wilson B. L. (1985). Numbers and words: Combining quantitative and qualitative methods in a single large-scale evaluation study. Evaluation Review, 9, 627–643. 10.1177/0193841X8500900505 [Google Scholar]
- Shield R. R., Miller S. C., Looze J., Tyler D. A., Lepore M. J. (2013). Why and how do nursing homes implement culture change practices? Insights from qualitative interviews in a mixed methods study. Manuscript submitted for publication [DOI] [PMC free article] [PubMed]
- Stata: Data Analysis and Statistical Software (Version 11) [Software] (2011). College Station, TX: StataCorp LP; Retrieved from http://www.stata.com [Google Scholar]
- Sterns S., Miller S. C., Allen S. (2010). The complexity of implementing culture change practices in nursing homes. Journal of the American Medical Directors Association, 11, 511–518. 10.1016/j.jamda.2009.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas W. (2003). Evolution of Eden. In Weiner A. S., Ronch J. L. (Eds.), Culture change in long-term care (pp. 141–158). New York: Hawthorn Press; [Google Scholar]
- Tyler D. A., Shield R. R., Rosenthal M., Miller S. C., Wetle T., Clark M. A. (2011). How valid are the responses to nursing home survey questions? Some issues and concerns. The Gerontologist, 51, 201–211. 10.1093/geront/gnq095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner J. M., Freiman M., Brown D. (2007). Strategies for improving the quality of long-term care. Paper presented at the National Commission for Quality Long-Term Care, Washington, DC [Google Scholar]
- Werner R. M., Tamara Konetzka R., Liang K. (2010). State adoption of nursing home pay-for-performance. Medical Care Research and Review, 67, 364–377. 10.1177/1077558709350885 [DOI] [PubMed] [Google Scholar]
- Zimmerman D. R. (2003). Improving nursing home quality of care through outcomes data: The MDS quality indicators. International Journal of Geriatric Psychiatry, 18, 250–257. 10.1002/ gps.820 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.