Abstract
Purpose: This study is one of the first to examine the physical and mental health of transgender older adults and to identify modifiable factors that account for health risks in this underserved population. Design and Methods: Utilizing data from a cross-sectional survey of lesbian, gay, bisexual, and transgender older adults aged 50 and older (N = 2,560), we assessed direct and indirect effects of gender identity on 4 health outcomes (physical health, disability, depressive symptomatology, and perceived stress) based on a resilience conceptual framework. Results: Transgender older adults were at significantly higher risk of poor physical health, disability, depressive symptomatology, and perceived stress compared with nontransgender participants. We found significant indirect effects of gender identity on the health outcomes via fear of accessing health services, lack of physical activity, internalized stigma, victimization, and lack of social support; other mediators included obesity for physical health and disability, identity concealment for perceived stress, and community belonging for depressive symptomatology and perceived stress. Further analyses revealed that risk factors (victimization and stigma) explained the highest proportion of the total effect of gender identity on health outcomes. Implications: The study identifies important modifiable factors (stigma, victimization, health-related behaviors, and social support) associated with health among transgender older adults. Reducing stigma and victimization and including gender identity in nondiscrimination and hate crime statutes are important steps to reduce health risks. Attention to bolstering individual and community-level social support must be considered when developing tailored interventions to address transgender older adults’ distinct health and aging needs.
Key Words: Gender identity, LGBT, Minority health, Resilience
The Institute of Medicine (2011) recently identified transgender adults as an understudied population in critical need of health research. Although few population estimates exist, recent data suggest that 0.3%–0.5% of the adult population identify as transgender (Gates, 2011). Based on prior studies, Witten and Eyler (2012) estimate that the transgender population aged 65 and older number at least 700,000. Because more than 130 million Americans are projected to be aged 50 and older by 2050 (U.S. Census Bureau, 2012), the number of transgender older adults is expected to steadily increase.
The term “transgender” is used inclusively to describe individuals who have “gender identities, expressions, or behaviors not traditionally associated with their birth sex” (Mayer et al., 2008, p. 990). Although gender is assigned at birth according to visible sex characteristics, gender identity is an individual’s psychological sense of self as male or female; gender expression is how a person expresses gender and how others perceive gender through clothing, grooming, speech, body language, social interactions, and other behaviors (FORGE, 2007). Although gender is most often dichotomized along a single dimension (Clarkson-Freeman, 2004), gender identity and expression are multidimensional constructs (Alegria, 2011; Grant et al., 2011; Persson, 2009).
Transgender adults are diverse in terms of their gender identities, gender expressions, sexual orientations, and sociodemographic characteristics. Generally subsumed under the broad umbrella of lesbian, gay, bisexual, and transgender (LGBT), there has been an inadequate analysis of how transgender adults differ from nontransgender lesbian, gay, and bisexual (LGB) adults or how transgender older adults differ from younger and middle-aged transgender adults. Some existing descriptive studies have explored the sociodemographic characteristics, health care access, health-related behaviors, rates of victimization, and levels of social support experienced by transgender adults of all ages, with limited attention to how such factors are associated with specific health outcomes.
Transgender adults earn less household income (Conron, Scott, Stowell, & Landers, 2012; Rosser, Oakes, Bockting, & Miner, 2007) and are more likely to be unemployed (Conron et al., 2012) than nontransgender adults. Findings regarding educational levels are mixed. Some findings suggest that transgender adults are more educated than the general population (Grant et al., 2011; Rosser et al., 2007). Others find that they do not differ significantly in their levels of education (Conron et al., 2012).
Although relatively little is known about the physical health of transgender adults (Witten & Eyler, 2012), much of the research that does exist focuses on primary and secondary effects of hormone use (Berreth, 2003; Cook-Daniels, 1997). Research has found that transgender adults are at elevated risk of depression (Clements-Nolle, Marx, Guzman, & Katz, 2001) and attempted suicide although the risk of suicide decreases with age (Grant et al., 2011). Health behaviors that likely affect transgender health include higher rates of smoking (Conron et al., 2012; Grant et al., 2011), but little is known about other key health-related behaviors, such as excessive drinking, lack of physical activities, and obesity, which are known to heighten the risk of multiple diseases and poor health (Chipperfield, 2008; Ford, Moriarty, Zack, Mokdad, & Chapman, 2001; Sacco, Bucholz, & Spitznagel, 2009). Although lower rates of obesity (Conron et al., 2012) have been documented, the data are limited to young and middle-aged adults.
The larger social context may increase the risk of health problems as transgender adults experience a relatively high degree of violence and abuse and often are victims of hate crimes (Grant et al., 2011; Witten & Eyler, 2012); these often go unreported due to the fear that transgender victims will be mistreated by law enforcement officers (Xavier & Simmons, 2000). Transgender adults also risk discrimination, harassment, and victimization in health care settings (Grant et al., 2011). More than a quarter of transgender adults have experienced discrimination by a physician or have been denied enrollment in a health insurance due to their gender identity (Bradford, Reisner, Honnold, & Xavier, 2012). Other studies found that they are less likely than the general population to have health insurance (One Colorado Education Fund, 2011), and for those with insurance, many transgender-related medical needs are not covered (American Medical Association, 2008).
Research examining the social resources available to transgender adults is relatively mixed. Some studies have found that transgender adults have limited social support (Fredriksen-Goldsen et al., 2011; SAGE & National Center for Transgender Equality, 2012; Witten, 2003) and do not feel supported by the LGB community (Factor & Rothblum, 2008; Fredriksen-Goldsen et al., 2011). Despite the adversities that transgender adults face, a few studies have found that they have relatively large and diverse social networks (Lombardi, 1999), and they participate in spiritual and religious activities at levels comparable to their biological siblings (Factor & Rothblum, 2007).
To date, there is limited information on social determinants that predict transgender older adult physical and mental health, which limits the ability to identify modifiable risk factors that can be incorporated into intervention efforts to improve health in this community. Based on a resilience conceptual framework (Yates & Masten, 2004), in this article, we examine the interplay between key health indicators and risk and protective factors and identify modifiable factors that affect the physical and mental health of transgender older adults. We assess the effects of gender identity on physical and mental health outcomes and explore the mediating role of key health indicators, and risk and protective factors.
The resilience conceptual framework has four primary components: (a) key health indicators, including access to health services and health-related behaviors; (b) risk factors related to marginalization, including internalized stigma, victimization, and identity concealment; (c) protective factors, including social support, social network size, participation in religious and spiritual activities, and community belonging; and (d) health outcomes, including general health, disability, depressive symptomatology, and stress. Our research questions explore whether and how transgender older adults differ from nontransgender LGB older adults on key health indicators, risk and protective factors, and health outcomes, controlling for background characteristics (age, income, gender, and race/ethnicity). In addition, we investigate the extent to which these factors account for the relationship between gender identity and physical and mental health outcomes.
The specific research questions to be tested in this study are as follows:
To what extent do transgender older adults experience higher rates of adverse key health indicators and risk factors and lower rates of protective factors, compared with nontransgender LGB older adults, after controlling for covariates, including age, income, gender, and race/ethnicity?
Do transgender older adults experience elevated rates of poor general health, disability, depressive symptomatology, and stress than do nontransgender LGB older adults, after controlling for covariates?
What are the risk and protective factors and key health indicators that mediate the relationship between gender identity and health outcomes, after controlling for covariates?
A better understanding of the key health indicators and risk and protective factors influencing transgender health has important implications for developing and testing interventions to improve the health of this underserved population.
Methods
Sample
Utilizing a cross-sectional survey design, the Caring and Aging with Pride research project was conducted through collaboration with 11 community-based agencies across the United States serving LGBT older adults, to better understand the risk and protective factors affecting the health of these older adults (Fredriksen-Goldsen et al., 2011). Each participating agency distributed surveys via their agency contact lists to adults aged 50 and older. Data were gathered over a 6-month period, from June 2010 to November 2010. Surveys with an invitation letter were distributed; two reminder letters were sent as follow-ups in subsequent 2-week periods. The total N for the survey was 2,560, which represents the largest sample to date of LGBT older adults. Sixty-three percent (n = 2,201) of the printed surveys were returned that met the eligibility criteria (self-identified as LGBT and aged 50 or older). For agencies that used only electronic mailing lists, a similar internet web–based survey was used following the same survey distribution protocol; 359 electronic surveys were returned that met the eligibility criteria. In the total sample of LGBT older adults, 7%, or 174 persons, self-identified as transgender. Transgender identity was assessed with an affirmative response to any one of the two questions: (a) Are you transgender? and (b) How old were you when you first considered yourself transgender? The second question was used to identify and include participants (n = 13) because some noted that although they were a different sex than ascribed at birth, they had completed the transition process and no longer considered themselves transgender. All study procedures were reviewed and approved by the University of Washington Institutional Review Board.
Measures
Detailed information about measures is given in Table 1. In this study, we utilized standardized measures whenever possible. Health outcomes were physical health, disability, depressive symptomatology, and perceived stress; key health indicators included financial barriers to health care, fear of accessing health services, smoking, lack of physical activities, and obesity; risk factors included lifetime internalized stigma, victimization, and sexual minority concealment; and protective factors included social support, social network size, positive feelings of LGBT community belonging, and religious and spiritual activities.
Table 1.
Description of Measures
| Variables | Descriptions |
|---|---|
| Health outcomes | |
| Physical health | Measured using four items from the SF-8 Health Survey (Ware, Kosinski, Dewey, & Gandek, 2001). Participants were asked to rate their health over the previous 4-week period on physical functioning, role limitation due to physical problems, bodily pain, and general health. The summary score range was 0–100, with higher scores indicating better perceived physical health (Cronbach’s α = 0.89) |
| Disability | Measured by asking whether they (1) were limited in any way, in any activities because of physical, mental, or emotional problems and (2) had any health problem that requires the use of special equipment, such as a cane, a wheelchair, a special bed, or a special telephone (Centers for Disease Control and Prevention [CDC], 2012). Those who answered affirmatively to either of the two items were categorized as having a disability, as defined in Healthy People 2010 (U.S. Department of Health and Human Services, 2000) |
| Depressive symptomatology | Assessed via the 10-item short form of the Center for Epidemiological Studies Depression Scale (Radloff, 1977), which has been validated for older adults (Andresen, Malmgren, Carter, & Patrick, 1994). The range of the summed score was 0–30, with higher scores indicating higher levels of depressive symptomatology (Cronbach’s α = 0.87) |
| Perceived stress | Measured using the four-item Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983), which assesses the degree to which participants appraise life situations as being stressful during the past month. The summary score ranged from 0 to 4, with higher scores indicating greater levels of perceived stress (Cronbach’s α = 0.78) |
| Health indicators | |
| Financial barriers to health care | Assessed by asking participants whether they needed to see a physician in the past year but could not because of cost (CDC, 2012) |
| Fear of accessing health service | Assessed by asking participants whether they feared accessing health services outside the lesbian, gay, bisexual, or transgender community |
| Smoking | Defined as having ever smoked 100 or more cigarettes and currently smoking every day or some days (CDC, 2012) |
| Lack of physical activities | Defined as not being engaged, on a weekly basis, in at least moderate activities that cause some increase in breathing or heart rate (CDC, 2011) |
| Obesity | Measured by self-reported weight and height. Body mass index of 30kg/m2 or higher was categorized as obese (CDC, 2010) |
| Risk factors | |
| Internalized stigma | Measured using a modified Homosexual Stigma Scale (Liu, Feng, Rhodes, & Liu, 2009). Participants were asked to rate their agreement (1 = strongly disagree to 4 = strongly agree) with five statements such as, “If someone offered me the chance to be completely heterosexual or not transgender, I would accept the chance; I feel that being lesbian, gay, bisexual, or transgender is a personal shortcoming for me” (Cronbach’s α = .78). The summary score ranged from 1 to 4, with higher scores indicating higher levels of internalized stigma |
| Lifetime victimization | Assessed with a modified version of the 16-item Lifetime Victimization Scale (D’Augelli & Grossman, 2001) and the Lifetime Discrimination Scale (Inter-University Consortium for Political and Social Research, 2010). Participants were asked how often in their lives they had experienced different types of victimization (including physical, verbal or sexual threat or assault, threat of being outed, property damage, being hassled by police, being ignored by police when assistance was needed, job-related discrimination, being denied or receiving inferior health care, and being prevented from living in a chosen neighborhood), because of their actual or perceived sexual orientation and/or gender identity. A four-point Likert rating scale was used, with summed score ranging from 0 to 46 (Cronbach’s α = .86) |
| Sexual/minority identity concealment | Measured through a modified version of the Outness Inventory scale (Mohr & Fassinger, 2000) that asks whether particular family members (i.e., mother, father, brothers, sisters, and children) or best friends “definitely do not know” participants’ gender or sexual identity |
| Protective factors | |
| Social support | The four-item abbreviated Social Support Instrument (Sherbourne & Stewart, 1991) was adapted to measure the degree of instrumental and emotional support received (Cronbach’s α = .85). The summary score ranged from 1 to 4, with higher scores indicating greater social support |
| Social network size | Assessed by asking participants how many people (e.g., friends, family members, colleagues, and neighbors) they have interacted within a typical month. We recoded the total size by quartiles with one indicating the lowest 25% (small) and four indicating the highest 25% (large) |
| Religious and spiritual activities | Measured how often during the past 30 days participants had attended spiritual or religious services or activities. The frequency ranged from 0 to 30 |
| Community belonging | Positive feeling of community belonging was measured by asking to what extent participants agreed with the following statement, “I feel good about belonging to the LGBT community” and “I’m glad I belong to the lesbian, gay, bisexual, or transgender community.” The summary score ranged from 1 (strongly disagree) to 4 (strongly agree) |
| Background characteristics | Included age (years), gender (current gender; men vs. women), race/ethnicity (non-Hispanic white vs. other), household income (≤200% of federal poverty level [FPL] vs. >200% FPL), education (high school or less vs. some college or more), relationship status (married/ partnered vs. other), having children, living arrangement (living alone vs. living with other), service in the military, current LGBT aging services use, and having a will and/or power of attorney for health care |
Statistical Analysis
Analyses were performed using STATA/IC for Windows (Version 11.2). Welch approximate t tests, due to unequal sample sizes among gender identity samples, and Pearson’s chi-squared test or Fisher exact test were used to examine the associations of gender identity with background characteristics (Table 2). Distributions of primary study variables including health care access, health-related behaviors, risk and protective factors, and health outcomes were examined by gender identity. Logistic or linear regression analyses controlling for key background characteristics including age, income, gender, and race/ethnicity were applied to test the gender identity effects on the primary variables (Table 3). Next, prior to testing the mediation roles of health care access, health-related behaviors, risk factors, and protective factors in the relationship between gender identity and health outcomes, we also examined the associations between mediators and dependent variables (health outcomes) as suggested by Baron and Kenny (1986) (Table 4). We applied linear regression or logistic regression analyses, as appropriate, to examine whether mediators were significantly associated with dependent variables, after controlling for key background characteristics.
Table 2.
Background Characteristics by Gender Identity
| Total (N = 2,546) | Transgender (n = 174) | Nontransgender (n = 2,372) | Gender identity difference | |
|---|---|---|---|---|
| Age, mean (±SD) | 66.47 (±9.08) | 60.97 (±7.96) | 66.87 (±9.03) | t = 9.35*** |
| Gender, men | 1,592 (62.78) | 61 (36.97) | 1,531 (64.57) | χ2 = 50.30*** |
| Race/ethnicity | ||||
| Non-Hispanic white | 2,187 (86.48) | 136 (79.07) | 2,051 (87.02) | χ2 = 34.28*** |
| African American | 89 (3.52) | 8 (4.65) | 81 (3.44) | |
| Hispanic | 112 (4.43) | 6 (3.49) | 106 (4.50) | |
| Asian/Pacific Islander | 41 (1.62) | 3 (1.74) | 38 (1.61) | |
| Native American | 48 (1.90) | 12 (6.98) | 36 (1.53) | |
| Multiracial | 18 (0.71) | 4 (2.33) | 14 (0.59) | |
| Other | 34 (1.34) | 3 (1.74) | 31 (1.32) | |
| Household income, ≤200% federal poverty level | 734 (30.72) | 78 (47.56) | 656 (29.48) | χ2 = 23.45*** |
| Education, ≤high school | 201 (7.96) | 20 (11.63) | 181 (7.70) | χ2 = 3.38 |
| Married/partnered | 1,121 (44.27) | 74 (42.53) | 1,047 (44.40) | χ2 = 0.23 |
| Children | 622 (24.58) | 103 (59.20) | 519 (22.02) | χ2 = 120.82*** |
| Living alone | 1,394 (55.16) | 76 (44.19) | 1,318 (55.97) | χ2 = 8.99** |
| Veterans | 642 (25.56) | 70 (40.94) | 572 (24.43) | χ2 = 22.81*** |
| Service use | 709 (28.46) | 26 (15.20) | 683 (29.44) | χ2 = 15.85*** |
| Legal planning | ||||
| Power of attorney for health care | 1,580 (63.58) | 61 (36.53) | 1,519 (65.53) | χ2 = 56.59*** |
| Will | 1,738 (69.80) | 84 (49.41) | 1,654 (71.29) | χ2 = 35.98*** |
Notes: Chi-squared or Fisher exact tests or Welch approximate t tests were conducted to examine differences by gender identity; numbers with percentages in parentheses for categorical variables and means with standard deviations in parentheses for continuous variables are reported.
**p < .01. ***p < .001.
Table 3.
Associations Between Gender Identity and Key Health Indicators, Risk and Protective Factors, and Health Outcomes
| Total | Transgender | Nontransgender | Gender identity effect | |
|---|---|---|---|---|
| Health care access | ||||
| Financial barrier to health service, % | 7.46 | 21.84 | 6.41 | OR = 1.80* |
| Fear of accessing health services, % | 14.87 | 39.53 | 13.01 | OR = 3.96*** |
| Health-related behaviors | ||||
| Current smoking, % | 9.16 | 14.97 | 8.74 | OR = 1.25 |
| Lack of physical activity, % | 15.13 | 22.67 | 14.58 | OR = 2.00** |
| Obesity, % | 25.59 | 39.52 | 24.59 | OR = 1.56* |
| Risk factors | ||||
| Internalized stigma, M (±SD) | 1.47 (±0.57) | 1.78 (±0.65) | 1.45 (±0.55) | b = .42*** |
| Victimization, M (±SD) | 6.51 (±7.33) | 10.99 (±10.05) | 6.19 (±6.98) | b = 3.60*** |
| Identity concealment, % | 17.42 | 31.98 | 16.34 | OR = 4.00*** |
| Protective factors | ||||
| Social support, M (±SD) | 3.09 (±.79) | 2.88 (±.82) | 3.11 (±.79) | b = −.24*** |
| Social network size, M (±SD) | 2.51 (±1.11) | 2.86 (±1.09) | 2.48 (±1.11) | b = .40*** |
| Religious and spiritual activities, M (±SD) | 2.03 (±4.65) | 3.02 (±6.29) | 1.96 (±4.49) | b = .71 |
| Community belonging, M (±SD) | 3.42 (±.76) | 3.30 (±.87) | 3.42 (±.75) | b = −.22** |
| Health outcomes | ||||
| Physical health, M (±SD) | 69.68 (±22.41) | 62.07 (±23.40) | 70.24 (±22.24) | b = −5.54*** |
| Disability, % | 46.81 | 61.76 | 45.73 | OR = 1.55* |
| Depressive symptomatology, M (±SD) | 7.41 (±6.36) | 10.34 (±7.29) | 7.20 (±6.23) | b = 2.19*** |
| Perceived stress, M (±SD) | 1.25 (±.81) | 1.56 (±.88) | 1.22 (±.79) | b = .22** |
Notes: OR = odds ratio; logistic or linear regression analyses were applied to examine the gender identity effect on key health indicators, risk and protective factors, and health outcomes, controlling for age, income, gender, and race/ethnicity.
*p < .05. **p < .01. ***p < .001.
Table 4.
Associations of Health Care Access, Health-Related Behaviors, and Risk Factors and Protective Factors With Health Outcomes: The Results of Adjusted Linear Regression and Logistic Regression Analyses
| Physical health | Disability | Depressive symptomatology | Perceived stress | |
|---|---|---|---|---|
| b | OR | B | B | |
| Health care access | ||||
| Financial barriers | −11.45*** | 2.39*** | 4.46*** | 0.56*** |
| Fear of access | −3.82** | 1.64*** | 2.32*** | 0.34*** |
| Health-related behaviors | ||||
| Lack of physical activity | −12.60*** | 2.38*** | 3.05*** | 0.38*** |
| Obesity | −12.00*** | 2.38*** | 1.20*** | 0.10** |
| Risk factors | ||||
| Internalized stigma | −3.62*** | 1.37*** | 2.20*** | 0.28*** |
| Victimization | −0.60*** | 1.04*** | 0.16*** | 0.02*** |
| Identity concealment | 0.93 | 1.10 | 0.99** | 0.14** |
| Protective factors | ||||
| Social support | 3.81*** | 0.71*** | −2.96*** | −0.35*** |
| Community belonging | 1.97** | 0.87* | −1.29*** | −0.16*** |
Note: OR = odds ratio; the analyses controlled for age, income, gender, and race/ethnicity.
*p < .05. **p < .01. ***p < .001.
Finally, we calculated the direct and indirect effects of gender identity (transgender and nontransgender) on health outcomes (physical health, disability, depressive symptomatology, and perceived stress) through (a) health care access, (b) health-related behaviors, (c) risk factors, and (d) protective factors (Table 5). This provided direct effects of gender identity on health outcomes with and without mediators, as well as indirect effects of gender identity on health outcomes via each mediator, by calculating the product of path coefficients from gender identity to the mediator and from the mediator to the health outcome. Figure 1 demonstrates graphically one of the mediation models we tested. Bootstrapping with 500 replications was used to conduct significance tests of direct and indirect effects (Preacher & Hayes, 2008). The proportion of the total effect that is mediated (the indirect effect divided by the total effect) was also calculated to assess what proportion of the total effect of gender identity on a health outcome is due to its indirect effect through each of the mediator components (MacKinnon, Warsi, & Dwyer, 1995).
Table 5.
Mediation Models Examining the Effect of Gender Identity on Health Outcomes by Health Care Access, Health-Related Behaviors, Risk Factors, and Protective Factors
| Dependent variables | ||||
|---|---|---|---|---|
| Physical health | Disability | Depressive symptomatology | Perceived stress | |
| Path coefficient | Path coefficient | Path coefficient | Path coefficient | |
| Health care access as mediators | ||||
| Direct effect | −0.041 | 0.036 | 0.041 | 0.028 |
| Indirect effect: financial barriers | −0.010 | 0.009 | 0.012 | 0.012 |
| Indirect effect: fear of access | −0.008* | 0.015** | 0.019*** | 0.023*** |
| Proportion of total effect mediated | 0.300 | 0.394 | 0.434 | 0.557 |
| Health-related behaviors as mediators | ||||
| Direct effect | −0.030 | 0.037 | 0.055* | 0.050* |
| Indirect effect: lack of physical activity | −0.017** | 0.014** | 0.017** | 0.016** |
| Indirect effect: obesity | −0.013* | 0.012* | 0.004 | 0.002 |
| Proportion of total effect mediated | 0.507 | 0.417 | 0.278 | 0.274 |
| Risk factors as mediators | ||||
| Direct effect | −0.021 | 0.017 | 0.008 | 0.004 |
| Indirect effect: internalized stigma | −0.015** | 0.017** | 0.034*** | 0.035*** |
| Indirect effect: victimization | −0.023*** | 0.022*** | 0.023*** | 0.017*** |
| Indirect effect: identity concealment | 0.003 | 0.005 | 0.008 | 0.009* |
| Proportion of total effect mediated | 0.631 | 0.724 | 0.888 | 0.943 |
| Protective factors as mediators | ||||
| Direct effect | −0.047* | 0.047 | 0.040 | 0.033 |
| Indirect effect: social support | −0.008** | 0.010** | 0.026** | 0.024** |
| Indirect effect: community belonging | −0.002 | 0.002 | 0.006* | 0.006* |
| Proportion of total effect mediated | 0.180 | 0.202 | 0.446 | 0.474 |
Note: The regression analyses controlled for age, income, gender, and race/ethnicity.
*p < .05. **p < .01. ***p < .001.
Figure 1.
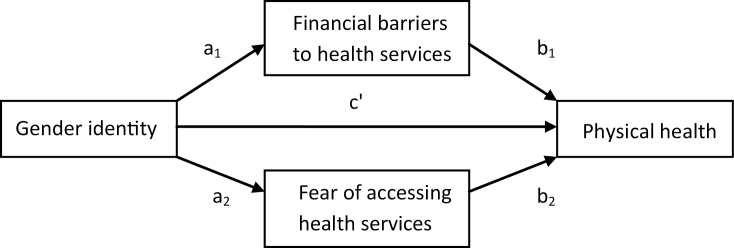
The mediation model where gender identity is associated with physical health through limited health care access. c′ indicates the direct effect in the model with mediators. The indirect path coefficients via financial barriers to health services and fear of accessing health services are a1 × b1 and a2 × b2, respectively. The proportion of the total effect mediated is computed with dividing the total indirect effect [(a1 × b1) + (a2 × b2)] by the total effect [c′ + (a1 × b1) + (a2 × b2)].
Results
Background Characteristics
Table 2 presents the background characteristics of the transgender older adult participants compared with nontransgender LGB older adults in the study. Compared with the nontransgender older adults, the transgender older adults were less likely to be non-Hispanic white and more likely to be younger and have lower household incomes. Transgender older adults were more likely to have children, less likely to live alone, and more likely to have served in the military compared with the nontransgender older participants; the rates of being married or partnered were similar between the two groups.
Gender Identity and Key Health Indicators and Outcomes
As given in Table 3, the associations of gender identity with key health indicators and risk and protective factors were examined after controlling for age, income, gender, and race/ethnicity. In terms of health care access, 22% of transgender older adult participants indicated having experienced financial barriers to health services, and 40% reported that they feared accessing health services outside the LGBT community. These proportions were significantly higher than those for nontransgender LGB older adult participants. In terms of health-related behaviors, the rates of obesity (40%) and lack of physical activity (23%) among transgender older adults were significantly higher than those for nontransgender LGB older adults although no significant difference on smoking was observed.
Transgender older adult participants reported higher rates of lifetime victimization and internalized stigma and were more likely to conceal their gender identity than nontransgender LGB older adult participants. On average, transgender older adults reported 11 incidents of lifetime discrimination and victimization, compared with an average of 6 for nontransgender LGB older adult participants. Additional analyses revealed that the most common types of discrimination and victimization experienced by transgender older adult participants were verbal insults (76%), being threatened with physical violence (54%), not being hired for job (46%), being denied or provided inferior health care (40%), being denied a promotion (39%), and being hassled by the police (37%). We also observed some important differences in protective factors for transgender older adults: they reported lower levels of social support and community belonging than nontransgender LGB older adults although their social network sizes were larger. We observed no significant difference in the levels of participation in spiritual and religious activities by gender identity.
Table 3 demonstrates that gender identity was significantly associated with health outcomes after controlling for key demographic characteristics. Transgender older adults reported significantly poorer physical health and a higher likelihood of having a disability than nontransgender participants. In addition, the levels of clinically significant depressive symptomatology and perceived stress for transgender older adult participants were significantly higher than those for nontransgender LGB older adult participants.
Key Health Indicators and Health Outcomes
As a preliminary step for mediation analyses, we tested whether the key health indicators and risk and protective factors were associated with health outcomes, controlling for age, income, gender, and race/ethnicity. Smoking, spiritual, and religious activities and social network size were not included in the further analyses because they were not associated with poor health outcomes. Table 4 demonstrates that financial barriers to health services, fear of accessing health services, obesity, lack of physical activity, and higher degrees of internalized stigma and victimization were significantly associated with poorer physical health, higher likelihood of disability, and higher degrees of depressive symptomatology and perceived stress. Concealment of gender identity was also significantly associated with higher degrees of depressive symptomatology and perceived stress. Social support and positive feelings of LGBT community belonging were significantly associated with better physical health, lower likelihood of disability, and lower levels of depressive symptomatology and perceived stress.
Factors That Explain the Adverse Health of Transgender Older Adults
First, as given in Table 5, we tested four sets of mediation models, with health care access (financial barriers to health services and fear of accessing health services) mediating the relationship between gender identity and each of the health outcomes, controlling for age, income, gender, and race/ethnicity. In the mediation models, the direct effects of gender identity on all of the health outcomes were not significant. The proportions of total effects of gender identity on health outcomes mediated through health care access were 30% for physical health, 39% for disability, 43% for depressive symptomatology, and 56% for perceived stress. According to the results of significance tests of indirect effects, fear of accessing health services was a significant mediator in the relationship between gender identity and the four health outcomes, but financial barrier to health services was not.
Second, in the models where health-related behaviors (lack of physical activities and obesity) mediate the relationship between gender identity and health outcomes, the direct effects of gender identity on physical health and disability were not significant. The direct effects on depressive symptomatology and perceived stress remained significant, but both the levels of significance and the sizes of path coefficients were reduced. Nearly 51% of the total effect of gender identity on physical health, 42% on disability, 28% on depressive symptomatology, and 27% on perceived stress were due to indirect effects through health-related behaviors. The indirect effects of gender identity on physical health and disability through lack of physical activity and obesity were statistically significant. The indirect effects of gender identity on depressive symptomatology and perceived stress through lack of physical activity were statistically significant, but the indirect effects through obesity were not.
The next set of analyses tested the mediating role of risk factors as listed in Table 5 in the relationships between gender identity and health outcomes. In the mediation models, the direct effects of gender identity on health outcomes were not significant. The proportions of total effects of gender identity that were mediated through risk factors were substantial; they accounted for 63% of physical health, 72% of disability, 89% of depressive symptomatology, and 94% of perceived stress. The indirect effects of gender identity on all the health outcomes through internalized stigma and victimization were statistically significant. The indirect effect on perceived stress through concealment of sexual minority identity was also statistically significant.
Finally, we tested whether the protective factors listed in Table 5 mediate the associations of gender identity and health outcomes. In the mediation models, the direct effect of gender identity on physical health was significant, but both the levels of significance and the sizes of path coefficients were reduced. The direct effects of gender identity on disability, depressive symptomatology, and perceived stress were not significant. Although only 18% of total effect on physical health and 20% on disability were due to indirect effects through protective factors, the proportions of total effect mediated for depressive symptomatology and perceived stress were 45% and 47%, respectively. The indirect effects of gender identity through social support on all the health outcomes were statistically significant. Although the indirect effects of gender identity through positive feeling of community belonging on physical health and disability were not significant, the respective indirect effects on depressive symptomatology and perceived stress were statistically significant.
Discussion
Transgender older adults have been largely invisible in existing aging and health research (Institute of Medicine, 2011; Persson, 2009). Although most previous studies combine LGBT older adults into a single group, this study demonstrates the importance of identifying the distinct health concerns and strengths of transgender older adults. In this study, we found that the transgender older adult participants had significantly poorer health in terms of physical health, disability, depressive symptomatology, and perceived stress than the nontransgender LGB older adult participants, controlling for key background characteristics. These findings suggest that the patterns of adverse health identified among transgender adults in early and middle adulthood (Conron et al., 2012; Grant et al., 2011) persist into later life.
The findings reveal significant but modifiable mediators that explain heightened risks in physical and mental health for transgender older adults. Of these, risk factors (especially internalized stigma and victimization) are notably strong mediators in the relationship between gender identity and all the health outcomes. Internalized stigma in other minority populations has been found to be associated with increased risk of poor health, morbidity, and mortality (Ahmed, Mohammed, & Williams, 2007). Transgender older adults are a highly marginalized population in our society, which can exacerbate the impact of stigma. Link and Phelan (2006) posit that being stigmatized is, in itself, a source of chronic stress that negatively affects both physical and mental health. We know from the HIV literature that experiences of, and fear of, stigma are associated with decreased access to care and treatment (Nyblade, Stangl, Weiss, & Ashburn, 2009). Considering that 40% of the transgender older adults in this study feared accessing health services, both discrimination from health care providers and internalized stigma can exacerbate chronic stress and act as further impediments to accessing needed health care. Stigma reduction strategies for health care professionals and improved education about gender identity and aging are essential to reduce stigma and discrimination in health care settings for transgender older adults.
Many transgender older adults in this study are at risk of victimization, including verbal insult, threatened physical assault, harassment by police and others, and employment discrimination. The transgender older adult participants experienced a higher prevalence of lifetime victimization compared with their nontransgender counterparts. A comprehensive meta-analytic review provides strong evidence that when individuals perceive that they are being discriminated against, both their physical and mental health suffer (Pascoe & Smart Richman, 2009). Individuals who experience victimization are at increased risk for developing subsequent serious psychiatric disorders, including depression (Cramer, McNiel, Holley, Shumway, & Boccellari, 2012).
Interestingly, the transgender older adult participants in the study were significantly more likely than nontransgender participants to have served in the military. Both the heightened likelihood of victimization and potential combat exposure place the transgender older adults at elevated risk of trauma-related conditions, such as post-traumatic stress disorder. Yet, transgender older adult veterans remain largely invisible and their contributions to this country are overlooked. The Department of Veterans Affairs and Veterans Health Administration (2011) recently issued a directive declaring that “eligible” transgender veterans have the same rights to health and medical care as nontransgender veterans. Unfortunately, even with the repeal of “Don’t Ask, Don’t Tell,” transgender Americans still cannot serve openly in the military as gender identity disorder constitutes a designation that categorically bars entrance into or mandates separation from the military (Servicemembers Legal Defense Network & National Center for Transgender Equality, 2010).
Although the mediating effects of identity concealment were not as strong as internalized stigma and victimization, it still contributed to explaining the effect of gender identity on perceived stress, with concealment significantly related to higher levels of stress. Hypervigilance due to the risk of exposure and the fear of rejection by important others can result from concealing a stigmatized identity (Meyer, 2003). Still, transgender adults who have revealed their gender identities to their families report improvement in these relationships over time, with strong family relationships related to more positive health outcomes (Grant et al., 2011). Thus, creating environments whereby transgender older adults do not possess stigmatized identities and do not feel the need to conceal their gender identity is critically important.
In terms of health care access, transgender older adults’ fear of accessing services was a significant mediator across the physical and mental health outcomes in this study. Transgender older adults are hesitant to seek medical attention, due to both negative experiences with and fear of judgments by health care providers (Cahill, South, & Spade, 2000; Cook-Daniels, 1997; Witten & Eyler, 2012). To date, many health care providers are inadequately prepared to address the needs of transgender older adults, a growing and underserved population (Cook-Daniels, 1997; Witten & Eyler, 2012). It has been suggested that those who disclose their gender identity are more likely to experience discrimination in medical settings (Grant et al., 2011). Most providers lack knowledge concerning transgender health issues both in their training and in the lack of frequency in which they encounter openly transgender individuals (Fallas, Landers, Lawrence, & Sperber, 2000; Grant et al., 2011). As a result, transgender individuals incur great time and travel costs necessary to reach trained and affirming providers (One Colorado Education Fund, 2011). Transgender adults’ reluctance to access health care and to disclose their gender identity, combined with the failure of health care providers to deliver culturally competent care, are likely to create barriers to care and subsequently lead to diminished health (American Medical Student Association, 2012).
Transgender older adult participants were less likely to be engaged in regular physical activity than the nontransgender older adult participants. The lowered levels of physical activities were linked with poor physical and mental health among transgender older adults. Reduced physical activity levels may be related to higher disability rates (Tak, Kuiper, Chorus, & Hopman-Rock, 2013). In addition, adults who have a history of discrimination are less likely to engage in protective health-related behaviors such as physical activity (Pascoe & Smart Richman, 2009). In this study, obesity mediated the effect of gender identity on physical health and disability. Although Conron and colleagues (2012) found no differences in obesity by gender identity, obesity becomes a more pronounced concern as age increases among transgender adults, particularly because obesity is associated with low levels of physical activity and increases the risk of other negative health outcomes, such as diabetes, coronary heart disease, and osteoarthritis (CDC, 2010).
In the general older adult population, the prevalence of obesity increases with age (Han, Tajar & Lean, 2011) and is associated with comorbidities and mobility limitations that affect physical activity (Corona et al., 2013) and quality of life (Han et al., 2011). Han and colleagues (2011) suggest that weight loss management programs be tailored according to individual needs. Considering the distrust and fear of accessing health services by the transgender older adults in this study, more research is needed to develop and test interventions that promote health and access to care for this population.
It is important to recognize that the transgender older adults in this study evidence resources that may be tapped in intervention development to bolster health. Compared with the nontransgender older adults in the study, the transgender older adults were significantly more likely to have children, have larger social networks, and were significantly less likely to live alone. Previous research suggests that transgender adults have slightly larger social networks than the general population although they are less likely to comprise family members (Lombardi, 1999). Despite the availability of these potentially protective resources, they did not necessarily translate into more support for the transgender older adults. Lower levels of social support and community belonging among transgender older adults accounted for markedly poorer mental health compared with their nontransgender LGB counterparts. Social support can be a resilience factor against the deleterious effects of victimization and is associated with positive health outcomes among sexual minorities (Fredriksen-Goldsen et al., in press). It will be important to examine (a) how other characteristics of social networks, such as density, reciprocity, and homogeneity (El-Bassel, Chen, & Cooper, 1998), are reflected in the quality of social resources and (b) their interplay with the prejudice that transgender older adults experience in the larger society and in sexual minority communities (Weiss, 2004). As health-related interventions are developed, it will be critical to explore what is needed to ensure that the social resources evidenced by transgender older adults translate into greater levels of social and community support.
Although this study highlights important findings regarding the health and aging of transgender older adults, several limitations must be considered. Because the participants were recruited via mailing lists from agencies, service users are likely to be overrepresented among the study participants. In the general older adult population, service users are likely to have more aging and health needs than nonservice users. Yet, it remains unclear if transgender older adults connected to service agencies have greater or fewer needs compared with nonservice users.
Although the sample is geographically and demographically diverse, it is a nonprobability sample, and the findings do not generalize to transgender older adults in general. In addition, because the agencies are primarily located in large urban areas, transgender older adults residing in rural areas are likely to be underrepresented among the study participants. It is important to note that typically, transgender adults connected to LGBT organizations are those who have taken action concerning their gender identity and have become activists (Lombardi, 1999). An unknown but likely large portion of transgender older adults blend into the mainstream society and no longer identify as transgender (Witten & Eyler, 2012). In the past transgender, older adults were typically urged by health care professionals to remain silent about a gender transition, and hence are likely difficult to identify for studies such as this. Although this cross-sectional analysis provides an important snapshot at one point in time of the health of an understudied population, it does not allow for the examination of health trends over time. Longitudinal studies are needed in order to better understand the health trajectories of transgender older adults over time.
Conclusions
This study represents one of the first to address transgender older adults’ physical and mental health and to identify modifiable risk factors that mediate their health. In order to develop effective interventions for this population, it will be important to address both the common health risks faced by older adults in general (such as lack of physical activity and social support) and the unique risk factors influencing transgender older adult health (including fear of accessing health services, internalized stigma, and victimization). As interventions and services are developed the identification of resources aimed at bolstering social support and a sense of community of belonging is also needed. Addressing the heterogeneity within diverse communities is necessary to reduce health disparities among older adults.
Funding
This research was funded, in part, by the National Institutes of Health and the National Institute on Aging (R01 AG026526).
References
- Ahmed A. T., Mohammed S. A., Williams D. R. (2007). Racial discrimination & health: Pathways & evidence. The Indian Journal of Medical Research, 126(4), 318–327 [PubMed] [Google Scholar]
- Alegria C. A. (2011). Transgender identity and health care: Implications for psychosocial and physical evaluation. Journal of the American Academy of Nurse Practitioners, 23(4), 175–182. 10.1111/j.1745-7599.2010.00595.x [DOI] [PubMed] [Google Scholar]
- American Medical Association. (2008). Removing financial barriers to care for transgender patients. House of Delegates (Vol. 122, p. 4). Washington, DC: Author; [Google Scholar]
- American Medical Student Association. (2012). Transgender health resources. Retrieved July 11, 2012, from http://www.amsa.org/AMSA/Homepage/About/Committees/GenderandSexuality/TransgenderHealthCare.aspx
- Andresen E. M., Malmgren J. A., Carter W. B., Patrick D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10(2), 77–84 [PubMed] [Google Scholar]
- Baron R. M., Kenny D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Berreth M. E. (2003). Nursing care of transgendered older adults. Implications from the literature. Journal of Gerontological Nursing, 29(7), 44–49 [DOI] [PubMed] [Google Scholar]
- Bradford J., Reisner S. L., Honnold J. A., Xavier J. (in press). Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. American Journal of Public Health. 10.2105/AJPH.2012.300796. Retrieved from http://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2012.300796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill S., South K., Spade J. (2000). Outing Age: Public policy issues affecting gay, lesbian, bisexual and transgender elders. Washington, DC: National Gay and Lesbian Task Force; [Google Scholar]
- Centers for Disease Control and Prevention. (2010). Overweight and obesity: Defining overweight and obesity. Retrieved March 12, 2011, from http://www.cdc.gov/obesity/defining.html
- Centers for Disease Control and Prevention. (2011). Physical activity for everyone: Older adults Retrieved October 26, 2011, from http://www.cdc.gov/physicalactivity/everyone/guidelines/olderadults.html
- Centers for Disease Control and Prevention. (2012). Behavioral risk factor surveillance system Retrieved February 24, 2012, from http://www.cdc.gov/brfss/
- Chipperfield J. G. (2008). Everyday physical activity as a predictor of late-life mortality. The Gerontologist, 48(3), 349–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkson-Freeman P. A. (2004). The defense of marriage act (DOMA): Its impact on those seeking same sex marriages. Journal of Homosexuality, 48(2), 1–19 [DOI] [PubMed] [Google Scholar]
- Clements-Nolle K., Marx R., Guzman R., Katz M. (2001). HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. American Journal of Public Health, 91(6), 915–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396 [PubMed] [Google Scholar]
- Conron K. J., Scott G., Stowell G. S., Landers S. J. (2012). Transgender health in Massachusetts: Results from a household probability sample of adults. American Journal of Public Health, 102(1), 118–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook-Daniels L. (1997). Lesbian, gay male, bisexual and transgendered elders: Elder abuse and neglect issues. Journal of Elder Abuse & Neglect, 9(2), 35–49 [Google Scholar]
- Corona L. P., Nunes D. P., Alexandre Tda. S., Ferreira Santos J. L., Oliveira Duarte Y. A., Lebrão M. L. (2013). Weight gain among elderly women as risk factor for disability: Health, well-being and aging study (SABE Study). Journal of Aging and Health, 25(1), 119–135. 10.1177/0898264312466261 [DOI] [PubMed] [Google Scholar]
- Cramer R. J., McNiel D. E., Holley S. R., Shumway M., Boccellari A. (2012). Mental health in violent crime victims: Does sexual orientation matter? Law and Human Behavior, 36(2), 87–95. 10.1037/h0093954 [DOI] [PubMed] [Google Scholar]
- D’Augelli A. R., Grossman A. H. (2001). Disclosure of sexual orientation, victimization, and mental health among lesbian, gay, and bisexual older adults. Journal of Interpersonal Violence, 16(10), 1008–1027 [Google Scholar]
- Department of Veterans Affairs, & Veterans Health Administration. (2011). Providing healthcare for transgender and intersex veterans Retrieved from http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2416
- El-Bassel N., Chen D.-R., Cooper D. (1998). Social support and social network profiles among women on methadone. Social Service Review, 72(3), 379–401 [Google Scholar]
- Factor R. J., Rothblum E. D. (2007). A study of transgender adults and their non-transgender siblings on demographic characteristics, social support, and experiences of violence. Journal of LGBT Health Research, 3(3), 11–30 [DOI] [PubMed] [Google Scholar]
- Factor R. J., Rothblum E. D. (2008). Exploring gender identity and community among three groups of transgender individuals in the United States: MTFs, FTMs, and genderqueers. Health Psychology Review, 17, 235–253 [Google Scholar]
- Fallas G., Landers S., Lawrence S., Sperber J. (2000). Access to health care for transgendered persons in Greater Boston. Boston: JSI Research & Training Institute, Inc., GLBT Health Access Project; [Google Scholar]
- Ford E. S., Moriarty D. G., Zack M. M., Mokdad A. H., Chapman D. P. (2001). Self-reported body mass index and health-related quality of life: Findings from the Behavioral Risk Factor Surveillance System. Obesity Research, 9(1), 21–31 [DOI] [PubMed] [Google Scholar]
- FORGE. (2007). Fast facts about gender rights Retrieved from http://forge-forward.org/wp-content/docs/fast-facts-about-gender-rights_WI_2007.pdf
- Fredriksen-Goldsen K. I., Emlet C. A., Kim H.-J., Muraco A., Erosheva E. A., Goldsen J, et al. (in press). The physical and mental health of lesbian, gay male and bisexual (LGB) older adults: The role of key indicators and risk and protective factors. Gerontologist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I., Kim H.-J., Emlet C. A., Muraco A., Erosheva E. A., Hoy-Ellis C. P, et al. (2011). The aging and health report: Disparities and resilience among lesbian, gay, bisexual, and transgender older adults. Seattle, WA: Institute for Multigenerational Health; 10.1093/geront/gns123. Retrieved from http://gerontologist.oxfordjournals.org/content/early/2012/09/25/geront.gns123.full.pdf+html [Google Scholar]
- Gates G. J. (2011). How many people are lesbian, gay, bisexual, and transgender? Los Angeles: The Williams Institute; [Google Scholar]
- Grant J. M., Mottet L. A., Tanis J., Harrison J., Herman J. L., Keisling M. (2011). Injustice at every turn: A report of the National Transgender Discrimination Survey. Washington, DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; [Google Scholar]
- Han T. S., Tajar A., Lean M. E. (2011). Obesity and weight management in the elderly. British medical bulletin, 97, 169–196. 10.1093/bmb/ldr002 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press; [PubMed] [Google Scholar]
- Inter-University Consortium for Political and Social Research. (2010). National Survey of Midlife Development in the United States (MIDUS II), 2004–2006: Documentation of psychosocial constructs and composite variables in MIDUS II Project 1 Retrieved April 10, 2012, from http://www.icpsr.umich.edu/cgi-bin/file?comp=none&study=4652&ds=1&file_id=1047483
- Link B. G., Phelan J. C. (2006). Stigma and its public health implications. Lancet, 367(9509), 528–529 [DOI] [PubMed] [Google Scholar]
- Liu H., Feng T., Rhodes A. G., Liu H. (2009). Assessment of the Chinese version of HIV and homosexuality related stigma scales. Sexually Transmitted Infections, 85(1), 65–69 [DOI] [PubMed] [Google Scholar]
- Lombardi E. L. (1999). Integration within a transgender social network and its effect upon members’ social and political activity. Journal of Homosexuality, 37(1), 109–126 [DOI] [PubMed] [Google Scholar]
- Mackinnon D. P., Warsi G., Dwyer J. H. (1995). A simulation study of mediated effect measures. Multivariate Behavioral Research, 30(1), 41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer K. H., Bradford J. B., Makadon H. J., Stall R., Goldhammer H., Landers S. (2008). Sexual and gender minority health: What we know and what needs to be done. American Journal of Public Health, 98(6), 989–995. 10.2105/AJPH.2007.127811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr J., Fassinger R. (2000). Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development, 33(2), 66–90 [Google Scholar]
- Nyblade L., Stangl A., Weiss E., Ashburn K. (2009). Combating HIV stigma in health care settings: What works? Journal of the International AIDS Society, 12, 15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- One Colorado Education Fund. (2011). Invisible: The state of LGBT health in Colorado. Denver, CO: Author; [Google Scholar]
- Pascoe E. A., Smart Richman L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson D. I. (2009). Unique challenges of transgender aging: Implications from the literature. Journal of Gerontological Social Work, 52(6), 633–646 [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401 [Google Scholar]
- Rosser B. R. S., Oakes J. M., Bockting W. O., Miner M. (2007). Capturing the social demographics of hidden sexual minorities: An Internet study of the transgender population in the United States. Sexuality Research & Social Policy, 4(2), 50–64 [Google Scholar]
- Sacco P., Bucholz K. K., Spitznagel E. L. (2009). Alcohol use among older adults in the National Epidemiologic Survey on Alcohol and Related Conditions: A latent class analysis. Journal of Studies on Alcohol and Drugs, 70(6), 829–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAGE, & National Center for Transgender Equality. (2012). Improving the lives of transgender older adults: Recommendations for policy and practice. New York: Authors; [Google Scholar]
- Servicemembers Legal Defense Network, & National Center for Transgender Equality. (2010). Attention transgender service members: It is NOT safe to come out as transgender. Washington, DC: Authors; [Google Scholar]
- Sherbourne C. D., Stewart A. L. (1991). The MOS social support survey. Social Science & Medicine (1982), 32(6), 705–714 [DOI] [PubMed] [Google Scholar]
- Tak E., Kuiper R., Chorus A., Hopman-Rock M. (2013). Prevention of onset and progression of basic ADL disability by physical activity in community dwelling older adults: A meta-analysis. Ageing Research Reviews, 12(1), 329–338 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2012). The 2012 statistical abstract: Population. Estimates by age, sex, race/ethnicity: 9 – Resident population projections by sex and age Retrieved June 29, 2012, from http://www.census.gov/compendia/statab/cats/population/estimates_and_projections_by_age_sex_raceethnicity.html
- U.S. Department of Health and Human Services. (2000). Healthy people 2010. Washington, DC: Author; [Google Scholar]
- Ware J. E., Kosinski M., Dewey J. E., Gandek B. (2001). How to score and interpret single-item health status measures: A manual for users of the SF-8 Health Survey. Lincoln, RI: QualityMetric; [Google Scholar]
- Weiss J. T. (2004). GL vs. BT: The archaeology of biphobia and transphobia within the U.S. gay and lesbian community. Journal of Bisexuality, 3, 25–55 [Google Scholar]
- Witten T. M. (2003). Transgender aging: An emerging population and an emerging need. Review Sexologies, 12(4), 15–20 [Google Scholar]
- Witten T., Eyler A. E. (2012). Gay, lesbian, bisexual, and transgender aging: Challenges in research, practice, and policy. Baltimore: Johns Hopkins University Press; [Google Scholar]
- Xavier J., Simmons R. (2000). The executive summary of the Washington Transgender Needs Assessment Survey Retrieved September 27, 2012, from http://www.gender.org/vaults/wtnas.html
- Yates T. M., Masten A. S. (2004). Fostering the future: Resilience theory and the practice of positive psychology. In Linley P. A., Joseph S. (Eds.), Positive psychology in practice (pp. 521–539). Hoboken, NJ: Wiley; [Google Scholar]


