Abstract
Background
The treatment of extensively drug-resistant tuberculosis (XDR TB) presents a major challenge. Second-line antimycobacterial drugs are less effective, more toxic, and more costly than first-line agents, and XDR TB strains are, by definition, resistant to the most potent second-line options: the injectable agents and fluoroquinolones. We conducted a meta-analysis to assess XDR TB treatment outcomes and to identify therapeutic approaches associated with favorable responses.
Methods
We searched PubMed and EMBASE databases to identify studies conducted through May 2009 that report XDR TB treatment outcomes.
Results
The search yielded 13 observational studies covering 560 patients, of whom 43.7% (95% confidence interval, 32.8%–54.5%) experienced favorable outcomes, defined as either cure or treatment completion, and 20.8% (95% confidence interval, 14.2%–27.3%) died. Random effects meta-analysis and meta-regression showed that studies in which a higher proportion of patients received a later-generation fluoroquinolone reported a higher proportion of favorable treatment outcomes (P = .012).
Conclusions
This meta-analysis provides the first empirical evidence that the use of later-generation fluoroquinolones for the treatment of XDR TB significantly improves treatment outcomes, even though drug-susceptibility testing demonstrates resistance to a representative fluoroquinolone. These results suggest that the addition of later-generation fluoroquinolones to XDR TB regimens may improve treatment outcomes and should be systematically evaluated in well-designed clinical studies.
Extensively drug-resistant (XDR) tuberculosis (TB) refers to infection with Mycobacterium tuberculosis strains that are resistant to the 2 mainstays of first-line TB therapy, isoniazid and rifampin, as well as to 2 of the most effective second-line therapies: a fluoroquinolone and at least 1 of the second-line injectable agents (amikacin, capreomycin, or kanamycin) [1]. Since 2006 when it was first described, XDR TB has been shown to be widespread, with documented cases in 6 continents and 55 countries [2]. Although the worldwide burden of XDR TB has been difficult to assess, high prevalences have been reported in countries of the former Soviet Union: 24% of multidrug-resistant (MDR) TB cases in Estonia and 15% of MDR TB cases in Donetsk Oblast in the Ukraine are reported to be also XDR [3]. Nearly 500,000 new MDR TB cases are diagnosed yearly, of which 10% are estimated to be XDR [3, 4].
Treatment outcomes have been significantly worse for patients with XDR TB than for patients with TB that is either drug-susceptible or MDR, defined as resistance to isoniazid and rifampin [5–7]. In the first recognized outbreak of XDR TB, Gandhi et al [8] reported that 53 patients in KwaZulu-Natal, South Africa, who were coinfected with XDR TB and human immunodeficiency virus (HIV) survived for a median of only 16 days, with a mortality of 98%. Although some subsequent studies have reported better outcomes [9], therapeutic options for XDR TB are extremely limited because second-line drugs are less effective, more toxic, and more costly than are first-line therapies, and XDR TB strains are, by definition, resistant to the more potent of the second-line options. Although several new drugs are being evaluated for the treatment of XDR TB, none are currently available.
In the absence of systematic evaluations of the existing regimens, current XDR TB treatment guidelines rely on expert opinion. Available data come from small, observational cohort studies, some of which were recently reviewed by Sotgiu et al [10], who reported that XDR TB can be successfully treated in up to 65% of patients, with better outcomes for those not coinfected with HIV. Treatment duration was found to be longer and outcomes generally poorer for patients with XDR TB, compared with patients with other types of MDR TB. This study did not pool the data to report a summary outcome statistic or assess the impact of specific strategies on outcomes. Here, we use data from existing studies, supplemented by information on treatment approaches and study design obtained from the authors, to evaluate the benefit of existing treatment strategies and to identify those that improve outcomes.
METHODS
We conducted this meta-analysis according to the guidelines set forth by the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group for reporting systematic reviews of observational studies [11].
Search and selection strategy
Using the search strategy described in Table 1, we identified studies that reported the outcomes of XDR TB treatment. We searched the PubMed database from 1965 to May 2009 and the EMBASE database from 1974 to May 2009, using combinations of the keywords “tuberculosis,” “extensively drug-resistant,” “extremely drug-resistant,” and “XDR TB.” We also hand-searched bibliographies of retrieved articles for additional references. We restricted our analysis to human studies and placed no restrictions on language. We included peer-reviewed reports of observational studies from which the proportion of patients who experienced favorable outcomes could be clearly calculated. We defined favorable outcomes, in accordance with World Health Organization recommendations, as patients who meet criteria either for cure (treatment completion plus at least 5 consecutive negative cultures during the last year of treatment) or for treatment completion (treatment completion but <5 cultures performed in the last year of treatment) [12]. We included only those studies that (1) confirmed that patients had XDR TB by drug-susceptibility testing of M. tuberculosis cultures; (2) followed treatment protocols that included the following second-line drugs: amikacin, kanamycin, capreomycin, streptomycin, fluoroquinolones, ethionamide, protionamide, cycloserine, terizidone, and p-aminosalicylic acid; and (3) explicitly reported treatment outcomes. In addition, studies were excluded if >50% of patients were still receiving treatment at the time of manuscript preparation and no additional information on their outcomes was available by personal correspondence with the authors or if the study reported <3 cases of XDR TB. If multiple published reports from the same cohort were available, we included only the one with the most detailed information on treatment protocol and outcomes. Because in a few cases we were unable to determine whether the same patients were included in different publications, we conducted a sensitivity analysis to assess the possible bias introduced by the inclusion of the smaller studies that may have included duplicated patients.
Table 1.
Search Strategy to Identify Observational Studies of Extensively Drug-Resistant Tuberculosis (XDR TB) Treatment Outcomes
| PubMed database |
Medical Subject Headings (MeSH) terms
|
Text terms
|
| EMBASE |
Emtree tool
|
Text terms
|
Data extraction
Data were extracted independently by 2 investigators (K.R.J. and D.B.T.), and differences were resolved by discussion with a third investigator (M.B.M.). We extracted the following data: first author, publication year, country in which the study was conducted, study period, number of patients with XDR TB, mean number of drugs to which patients’ isolates were resistant, mean age in years, percentage of female patients, percentage of patients with HIV infection, mean number of drugs in the XDR TB treatment regimen, mean number of “likely active drugs” in the XDR TB treatment regimen, percentage of patients who received later-generation fluoroquinolones (levofloxacin, moxifloxacin, or sparfloxacin), percentage of patients who received linezolid, percentage of patients who underwent surgery, and treatment outcomes. The term “likely active drugs” is defined as the following: (1) drugs to which the TB strains have been tested and have been found to be susceptible or (2) drugs to which the patient has not been previously exposed or had been exposed for <1 month and for which susceptibility testing had not been done. Additional details on treatment protocol or outcomes were obtained via personal correspondence with one of the authors (K.R.J.).
Data analysis
We summarized the proportion of patients who experienced favorable outcomes and the proportion of deaths across the studies using a random effects model, which assigns weights according to the methods described by Der-Simonian and Laird [13]. We used the 95% score interval method to calculate the 95% confidence interval (CI) for proportions close to 0 or 1 [14]. We assessed the heterogeneity of outcomes within and between each group of studies, using the Cochrane Q test for heterogeneity and the I2 statistic described by Higgins et al [15, 16]. Because 2 studies may have included some patients who had been described in previously published reports, we performed sensitivity analyses, removing the original studies to determine whether this duplication could have a significant effect on the summary statistics.
To determine whether the outcomes varied significantly by specific treatment approaches, we performed univariate meta-regression, in which we evaluated the impact of study characteristics on the proportion of favorable outcomes, weighting the studies by the inverse of the sum of within- and between-study variance. We evaluated the distribution of outcomes using the Shapiro-Wilk test and found the outcomes to be normally distributed, allowing the outcomes in proportions to be assessed using meta-regression. We assessed the following variables for each study: (1) HIV prevalence among patients with XDR TB receiving treatment; (2) mean age; (3) proportion of patients who were female; (4) mean number of drugs in treatment regimens; (5) mean number of “likely active drugs” in a treatment regimen; (6) percentage of patients who received a later-generation fluoroquinolone; (7) percentage of patients who received linezolid; (8) percentage of patients who underwent surgery. We tested the significance of these coefficients by Student’s t test and reported the P value for significance of trend. We performed a multivariate meta-regression using the 2 statistically significant covariates in univariate meta-regression: age and fluoroquinolone use. To further study the impact of later-generation fluoroquinolone use, we did a subgroup analysis examining the differences in favorable treatment outcomes in studies in which at least 50% of patients received a later-generation fluoroquinolone, compared with studies in which <50% of patients received a later-generation fluoroquinolone. Statistical procedures were performed using STATA version 10 [17].
RESULTS
Of the 322 publications that we identified on XDR TB, 281 were excluded after abstract review because they were reviews or commentaries; did not report treatment outcome; focused on drug development, diagnostics, or vaccine development; were mathematical models or ethics articles; or studied animals (Figure 1). We performed a full text review for 41 articles, of which 13 met inclusion criteria [5, 9, 18–28]. Table 2 summarizes the characteristics of the 13 included studies. Four studies were conducted in South Korea, 4 in the United States, 2 in Germany, 1 in Estonia, 1 in Peru, and 1 in Russia. In total, these publications report 560 patients treated for XDR TB. All the studies were retrospective, observational, cohort studies of treatment outcomes for patients with XDR TB receiving second-line drug regimens. All 13 studies were reported in English and included cohorts who received treatment between 1984 and 2007.
Figure 1.
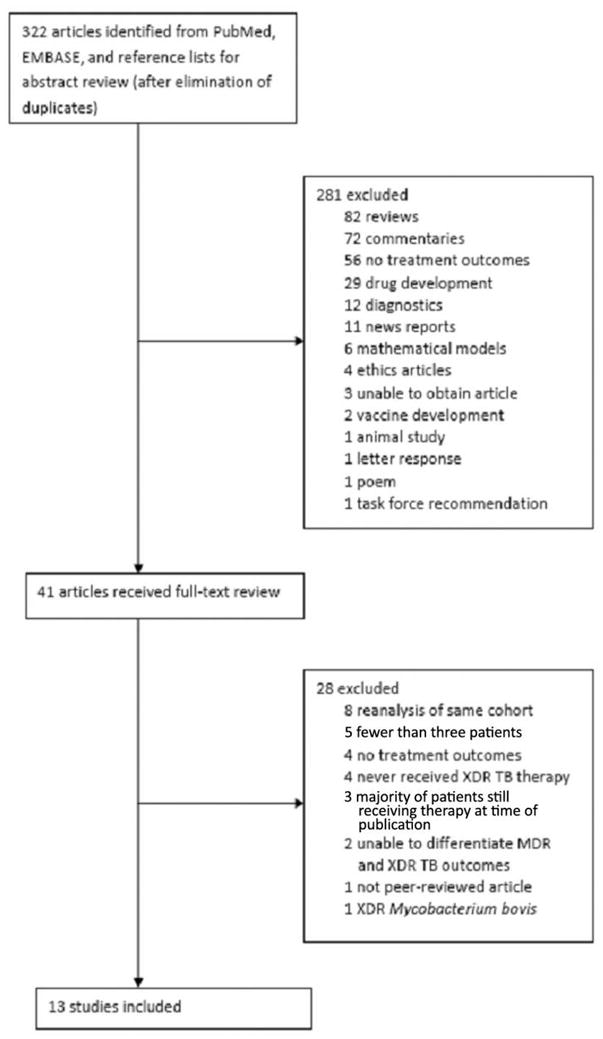
Flowchart depicting methods for article inclusion.
Table 2.
Characteristics of Patients, Treatment Regimens, and Cure Definitions in 13 Observational Studies of Extensively Drug-Resistant Tuberculosis (XDR TB) Treatment Outcomes
| Study authors | Study location | Study years | Sample size, no. of patients | HIV prevalence, % | Mean age, years | Female, % | Mean resistance, no. of drugs | Mean no. of drugs/no. activea | FQ,b % | Linezolid,c % | Surgery,d % | Definition of curee |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Banerjee et al [18] | US | 1993–2006 | 17 | 0 | 45 | … | … | … | … | … | … | Treatment completion |
| Blaas et al [19] | Germany | 1997–2006 | 4 | 0 | 42 | 0 | 10.5 | 7.3/4.5 | 75 | 50 | 50 | WHO |
| Chan et al [20] | US | 1984–1998 | 10 | 0 | 44.9 | 20 | 10.1 | 7.1/3.9 | 0 | 0 | 60 | 3 negative cultures and no clinical evidence of TB |
| Condos et al [21] | US | 2000–2007 | 6 | 16.7 | 30.5 | 100 | 9.8 | 7.2/4.8 | 83.3 | 100 | 50 | Treatment completion plus 1 negative culture |
| Eker et al [22] | Germany | 2004–2006 | 7 | 0 | 42.4 | 14.3 | 9.1 | 3.6/3.1 | 14.3 | 71.4 | 14.3 | WHO |
| Jeon et al [23] | South Korea | 2001–2005 | 158 | 0 | 42.1 | 27.8 | 6.9 | 5.3/1.9 | 16 | 5 | 10.1 | WHO |
| Keshavjee et al [9] | Russia | 2000–2004 | 29 | 0 | 33.9 | 17.2 | … | 5.6/… | 3.5 | 0 | 10.3 | WHO |
| Kim D et al [24] | South Korea | 2000–2006 | 75 | 0 | 47.8 | 29.3 | 7.8 | 5/2 | 8 | 0 | 4 | WHO |
| Kim H et al [5] | South Korea | 1996–2005 | 43 | 0 | 35 | 48.8 | 7.9 | 7.4/… | 74.4 | 2.3 | 55.8 | WHO |
| Kliiman et al [25] | Estonia | 2003–2005 | 54 | 3.7 | 45 | 25.9 | 7 | … | … | … | … | WHO |
| Kwon et al [26] | South Korea | 1995–2004 | 27 | 0 | 35.8 | 44 | 5 | 6/2 | 88.9 | 3.7 | 48 | WHO |
| Mitnick et al [27] | Peru | 1999–2002 | 47 | 0 | 32 | 35.4 | 8.4 | 5.3/5.3 | 91.5 | 0 | 14.6 | WHO |
| Shah et al [28] | US | 1993–2008 | 83 | 53 | 41.2 | 36 | … | … | … | … | … | US National TB Surveillance Methods |
NOTE. FQ, fluoroquinolone; HIV, human immunodeficiency virus; WHO, World Health Organization.
Mean number of drugs included in the XDR TB treatment regimen/mean number of drugs “likely active” included in the XDR TB treatment regimen.
Percentage of patients in each study who received a later-generation FQ (levofloxacin, moxifloxacin, or sparfloxacin) as part of their XDR TB treatment regimen.
Percentage of patients in each study who received linezolid as part of their XDR TB treatment regimen.
Percentage of patients in each study who underwent surgery as part of their XDR TB treatment.
The WHO [29] defines cure as at least 5 consecutive negative cultures during the last 12 months of treatment; US National TB Surveillance Methods report completion of treatment only for favorable outcomes.
All patients met the definition for infection with XDR TB (Table 2). For second-line drug testing, all studies reported testing results for at least ofloxacin and kanamycin. Drug-susceptible concentration cutoffs reported were consistent across studies. The majority of the studies did not include HIV-infected patients. The mean age of subjects ranged from 30.5 to 47.5 years. The mean number of drugs to which isolated organisms were resistant ranged from 5 to 10.5. All patients reportedly were treated for XDR TB under close supervision, in hospital settings or on an ambulatory basis. In all 13 studies, patients received at least 12 months of therapy after culture conversion. The mean number of drugs included in the XDR TB treatment regimens ranged from 3.6 to 7.4, and the mean number of “likely active drugs,” as reported in 8 studies, ranged from 1.9 to 5.3. The percentage of patients receiving a later-generation fluoroquinolone ranged from 0 to 91.5, the percentage of patients receiving linezolid ranged from 0 to 100, and the percentage undergoing surgery ranged from 4 to 60.
The definition of cure varied among the studies (Table 2). Nine of the 13 studies followed the current World Health Organization standard definition of at least 5 consecutive negative cultures during the last 12 months of treatment [29]. One study required 3 negative cultures and no clinical evidence of TB at the end of therapy [20]; one study required treatment completion plus 1 negative culture [21]; and 2 studies from the United States reported only treatment completion and did not provide any data on microbiological status at the end of therapy [18, 28].
A total of 208 patients had favorable outcomes. The weighted proportion of favorable outcomes was 43.7% (95% CI, 32.8%–54.5%) (Figure 2). The heterogeneity of this effect estimate (I2) was 84.3% of the variance. A total of 125 patients died. The weighted proportion of patients who died was 20.8% (95% CI, 14.2%–27.3%), with a heterogeneity of effect estimate (I2) of 67.7% of the total variance (Figure 3).
Figure 2.

Weighted proportion of favorable outcomes for the selected studies. CI, confidence interval.
Figure 3.
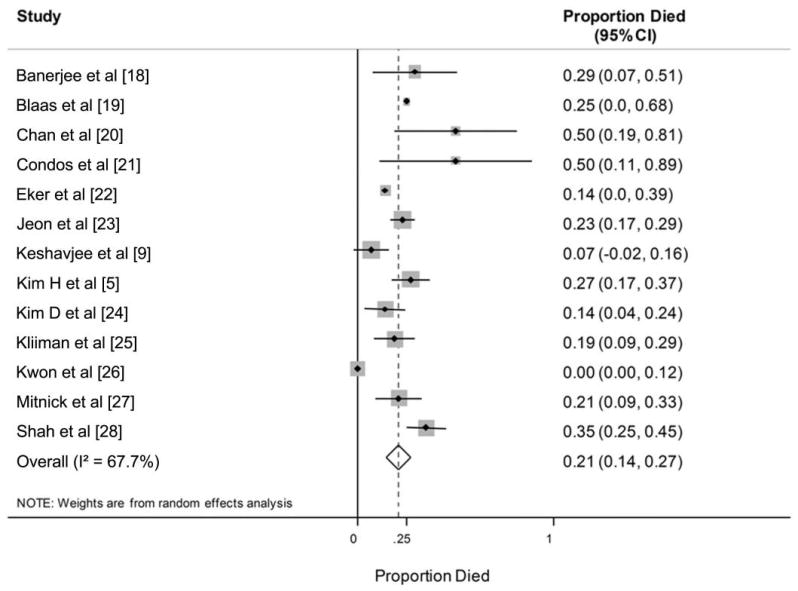
Weighted proportion of deaths for the selected studies. CI, confidence interval.
Shah et al [28] reported on all US outcomes between 1993 and 2008, and Banerjee et al [18], Chan et al [20], and Condos et al [21] reported outcomes in US-based studies that overlapped with these dates. When we reassessed the summary statistic of favorable outcomes, removing the smaller studies from the analysis, we found that the results changed from 43.7% to 45.6%, which is a <5% change.
Kim et al [24] reported on patients who received a diagnosis between 2000 and 2002 from all national TB hospitals, all Korean National Tuberculosis Association chest clinics, and 8 randomly selected university hospitals near Seoul, South Korea. Since this cohort potentially overlapped with the 3 other Korean studies [5, 23, 26], we contacted Kim et al, who noted that a small number of subjects overlapped with those in the studies by Jeon et al [23] and Kwon et al [26]. When we performed a sensitivity analysis removing these 2 studies, we found that the favorable outcomes summary statistic changed from 43.7% to 44.4%.
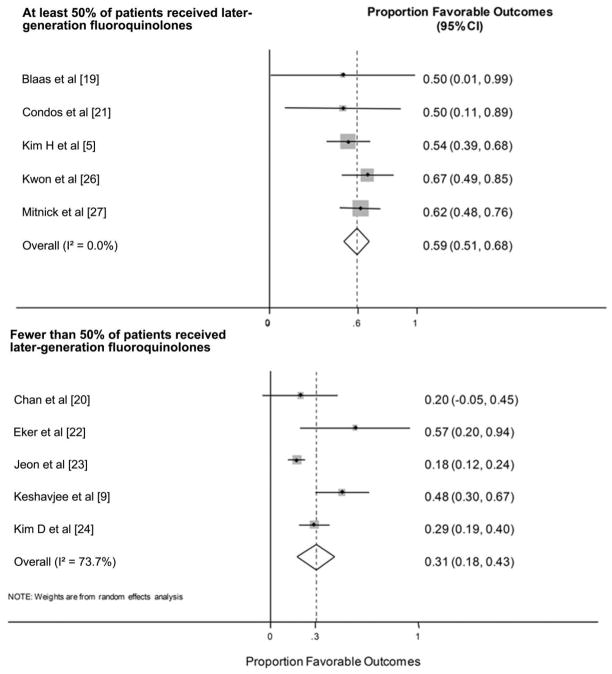
Table 3 shows that those studies in which a higher proportion of patients received a later-generation fluoroquinolone reported significantly higher proportions of favorable treatment outcomes (P = .012). With each 10% increase in the proportion of patients receiving a later-generation fluoroquinolone, we observed a 4% increase in the proportion of those with favorable outcomes. For those studies in which at least 50% of patients received a later-generation fluoroquinolone, the weighted proportion of favorable outcomes was 59.3% (95% CI, 50.8%–67.8%; I2 = 0), whereas, in those studies in which <50% of the patients received a later-generation fluoroquinolone, the weighted proportion of favorable outcomes was only 30.6% (95% CI, 17.7%–43.5%; I2 = 73.7%) (Figure 4).
Table 3.
Change in Favorable Outcomes as a Function of Individual Study Characteristics
| Study characteristic (no. of studies reporting) | Favorable outcomes improvement, % (95% CI) | P |
|---|---|---|
| HIV prevalence,a % (13) | 0.27 (−6.6 to 7.1) | .93 |
| Mean age,a years (13) | −20 (−35 to −3.8) | .019 |
| Percentage femalea (12) | 2.5 (−3.7 to 8.8) | .39 |
| Mean no. of drugs in treatment regimen (10) | 0.21 (−14.9 to 15.3) | .98 |
| Mean no. of “likely active drugs” in treatment regimen (8) | 5.5 (−8.6 to 20) | .38 |
| Percentage who received fluoroquinolonesa (10) | 3.7 (1.1 to 6.4) | .012 |
| Percentage who received linezolida (10) | 1.2 (−3.9 to 6.4) | .55 |
| Percentage who underwent surgerya (10) | 1.9 (−4.9 to 8.7) | .65 |
NOTE. CI, confidence interval.
Per 10-unit change.
Figure 4.
Weighted proportion of favorable outcomes for those studies in which at least 50% of patients received a later-generation fluoroquinolone, compared with those studies in which <50% of patients received a later-generation fluoroquinolone. CI, confidence interval.
Studies in which patients were younger on average also reported significantly higher proportions of favorable outcomes (P = .019), with an increase in the proportion of favorable outcomes of 20% for every 10 years younger of mean patient age. HIV prevalence, the proportion of female patients, the mean number of drugs, the mean number of “likely active drugs,” the percentage of patients who received linezolid, and the percentage of patients who underwent surgery were not associated with favorable treatment outcomes in univariate analysis.
We performed a multivariate meta-regression including the 2 significant covariates in univariate meta-regression: age and proportion of patients receiving later-generation fluoroquinolones. However, the 2 variables were highly correlated in these 2 studies (r = −0.66); therefore, we were unable to evaluate their effects independently.
DISCUSSION
To date, XDR TB treatment outcomes have been examined only in small, observational studies. We used meta-analysis to summarize these findings, reporting on 13 studies that included 560 patients. The proportion of patients who experienced favorable outcomes ranged from 18% to 67%, and the percentage of patients who received a later-generation fluoroquinolone was significantly associated with the proportion with favorable outcomes. We found that a cohort in which all patients received later-generation fluoroquinolones would have a 40% increase in favorable outcomes, compared with a cohort in which no patients received later-generation fluoroquinolones. Although this finding is potentially confounded by age, it nevertheless raises an important clinical question, since it suggests that the addition of a later-generation fluoroquinolone, even in the presence of representative fluoroquinolone resistance, might significantly improve outcomes. Moreover, this is an intervention that can be implemented and assessed immediately.
This finding reaffirms the potential importance of fluoroquinolones in the treatment of MDR TB [30]. Drug susceptibility testing for fluoroquinolones is routinely performed for the early-generation drugs ofloxacin and ciprofloxacin, the formulations most often given globally for TB and for infections in general. Resistance to these drugs is conferred by mutations in the M. tuberculosis gyrA and gyrB genes [31, 32]. Few centers reliably do testing for susceptibility to later-generation fluoroquinolones; therefore, it is rarely checked and is known for very few of the isolates in this study. In vitro and in vivo studies have identified differences in the efficacy of the various fluoroquinolones in TB treatment. Treatment studies in mice have shown moxifloxacin to be the most bactericidal, followed by sparfloxacin, levofloxacin, and then ofloxacin [33, 34]. Clinically significant resistance (minimum inhibitory concentration >2 μg/mL) to ciprofloxacin or ofloxacin is conferred by a single gyrase mutation, whereas at least 2 mutations in gyrA or mutations in gyrA and gyrB are required for high-level resistance [33, 35]. Although cross-resistance among all fluoroquinolone classes has been documented in vitro [36], the higher levels of bactericidal activity of later-generation fluoroquinolones may overcome low-level resistance, and the requirement for secondary mutations to achieve high-level resistance may explain their continued efficacy despite the decreased potency of ofloxacin and ciprofloxacin.
Younger mean age also predicted improved treatment outcomes. This finding has been reported for drug-susceptible disease and likely reflects the overall improved health and greater tolerance of therapy toxicity in younger patients [37]. However, previous studies have not found age to be a predictor of outcome for MDR TB [38]. The majority of the studies that reported higher late-generation fluoroquinolone use also reported younger mean age. Because of the small number of studies in the meta-regression, we were unable to assess the effects of the 2 covariates independently. However, we believe that both variables may have independently significant effects on outcome, because there is no clear biological reason that treatment plans would disproportionately contain later-generation fluoroquinolones dependent on age.
Although we found no association between HIV infection and poor outcomes, only 3 studies included HIV-infected patients; thus, our study may have been underpowered to detect an impact of HIV. Another potential limitation for generalizability is that the majority of these studies were done in high-income countries with low to middle TB burden. However, it seems unlikely that the progression of disease or effect of therapy would differ significantly across settings unless susceptibility testing or drugs were not reliably available. The lack of association between the mean number of drugs given or the mean number of “likely active drugs” and treatment outcomes may be due to the low number of active drugs given and the small number of studies included. Our evaluation of the use of linezolid in treatment regimens was limited by the small number of patients who received the drug. Although we found no benefit of surgery in this study, we could not control for individual patient factors that varied among those who underwent surgery and those who did not.
Overall, the random effects meta-analytic model estimated treatment success at 43.7% (95% CI, 32.8%–54.5%), well below the 62%–70% reported for patients with MDR TB [39, 40]. The summary estimate of patients who died—20.8% (95% CI, 14.2%–27.3%)—is also higher than that reported for MDR TB populations, further corroborating the higher lethality of this form of the disease [40].
This study provides preliminary evidence that later-generation fluoroquinolones may improve treatment outcomes for patients with XDR TB and suggests that further study of their efficacy is urgently needed. To our knowledge, this is one of the first reports of a positive association between any treatment intervention and improved XDR TB treatment outcomes. When XDR TB does occur, testing for resistance to later-generation fluoroquinolones, systematic reporting of treatment interventions and outcomes, treating with a later-generation fluoroquinolone, and pooling of smaller cohorts are needed to strengthen the evidence base for treatment of this virulent form of the disease.
Acknowledgments
We thank the following for their personal communication on individual study details for this project: Sidney Atwood, Ritu Banerjee, Peter Ceglielski, Ed Chan, Kai Kliiman, Hye-Ryoun Kim, Won-Jung Koh, Christoph Lange, Tae Sun Shim, and Matthew Strand.
Financial support. National Institutes of Health (T32 to K.R.J. and D.B.T.).
Footnotes
Potential conflicts of interest. All authors: no conflicts.
References
- 1.Centers for Disease Control and Prevention (CDC) Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs—worldwide, 2000–2004. MMWR Morb Mortal Wkly Rep. 2006;55:301–5. [PubMed] [Google Scholar]
- 2.World Health Organization. Countries that had reported at least one XDR-TB case by end. Mar, 2009. [Accessed 17 November 2009]. http://www.who.int/tb/challenges/xdr/xdr_map_mar09.pdf.
- 3.World Health Organization. Ebooks Corporation; 2008. [Accessed 17 November 2009]. Anti-tuberculosis drug resistance in the world, fourth global report: the WHO/IUATLD Global Project on Anti-Tuberculosis Drug Resistance Surveillance. WorldCat.org entry. http://www.worldcat.org/oclc/437123756&referer=brief_results. [Google Scholar]
- 4.Shah NS, Wright A, Bai GH, et al. Worldwide emergence of extensively drug-resistant tuberculosis. Emerg Infect Dis. 2007;13:380–7. doi: 10.3201/eid1303.061400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim HR, Hwang SS, Kim HJ, et al. Impact of extensive drug resistance on treatment outcomes in non–HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007;45:1290–5. doi: 10.1086/522537. [DOI] [PubMed] [Google Scholar]
- 6.Andrews JR, Gandhi NR, Moll AP, et al. High mortality among patients with multidrug and extensively drug-resistant tuberculosis in rural South Africa [abstract PS72041-12]. Program and abstracts of the 38th Union World Conference Lung Health; Cape Town, South Africa. 2007. [Google Scholar]
- 7.Migliori GB, Besozzi G, Girardi E, et al. Clinical and operational value of the extensively drug-resistant tuberculosis definition. Eur Respir J. 2007;30:623–6. doi: 10.1183/09031936.00077307. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi NR, Moll A, Sturm AW, et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006;368:1575–80. doi: 10.1016/S0140-6736(06)69573-1. [DOI] [PubMed] [Google Scholar]
- 9.Keshavjee S, Gelmanova IY, Farmer PE, et al. Treatment of extensively drug-resistant tuberculosis in Tomsk, Russia: a retrospective cohort study. Lancet. 2008;372:1403–9. doi: 10.1016/S0140-6736(08)61204-0. [DOI] [PubMed] [Google Scholar]
- 10.Sotgiu G, Ferrara G, Matteelli A, et al. Epidemiology and clinical management of XDR-TB: a systematic review by TBNET. Eur Respir J. 2009;33:871–81. doi: 10.1183/09031936.00168008. [DOI] [PubMed] [Google Scholar]
- 11.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Emergency update 2008. Geneva: World Health Organization; 2008. Guidelines for the programmatic management of drug-resistant tuberculosis. [Google Scholar]
- 13.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 14.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat. 1998;52:119–26. [Google Scholar]
- 15.Cochran W. The combination of estimates from different experiments. Biometrics. 1954;10:101–29. [Google Scholar]
- 16.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 17.Statacorp. Stata statistical software: release 10. College Station, TX: Statacorp; 2007. [Google Scholar]
- 18.Banerjee R, Allen J, Westenhouse J, et al. Extensively drug-resistant tuberculosis in California, 1993–2006. Clin Infect Dis. 2008;47:450–7. doi: 10.1086/590009. [DOI] [PubMed] [Google Scholar]
- 19.Blaas SH, Mutterlein R, Weig J, et al. Extensively drug resistant tuberculosis in a high income country: a report of four unrelated cases. BMC Infect Dis. 2008;8:60–7. doi: 10.1186/1471-2334-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan ED, Strand MJ, Iseman MD. Multidrug-resistant tuberculosis (TB) resistant to fluoroquinolones and streptomycin but susceptible to second-line injection therapy has a better prognosis than extensively drug-resistant TB. Clin Infect Dis. 2009;48:e50–2. doi: 10.1086/597010. [DOI] [PubMed] [Google Scholar]
- 21.Condos R, Hadgiangelis N, Leibert E, et al. Case series report of a linezolid-containing regimen for extensively drug-resistant tuberculosis. Chest. 2008;134:187–92. doi: 10.1378/chest.07-1988. [DOI] [PubMed] [Google Scholar]
- 22.Eker B, Ortmann J, Migliori GB, et al. Multidrug- and extensively drug-resistant tuberculosis, Germany. Emerg Infect Dis. 2008;14:1700–6. doi: 10.3201/eid1411.080729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeon DS, Kim DH, Kang HS, et al. Survival and predictors of outcomes in non-HIV-infected patients with extensively drug-resistant tuberculosis. Int J Tuberc Lung Dis. 2009;13:594–600. [PubMed] [Google Scholar]
- 24.Kim DH, Kim HJ, Park SK, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008;178:1075–82. doi: 10.1164/rccm.200801-132OC. [DOI] [PubMed] [Google Scholar]
- 25.Kliiman K, Altraja A. Predictors of poor treatment outcome in highly drug-resistant pulmonary tuberculosis. Eur Respir J. 2009;33:1085–94. doi: 10.1183/09031936.00155708. [DOI] [PubMed] [Google Scholar]
- 26.Kwon YS, Kim YH, Suh GY, et al. Treatment outcomes for HIV-uninfected patients with multidrug-resistant and extensively drug-resistant tuberculosis. Clin Infect Dis. 2008;47:496–502. doi: 10.1086/590005. [DOI] [PubMed] [Google Scholar]
- 27.Mitnick CD, Shin SS, Seung KJ, et al. Comprehensive treatment of extensively drug-resistant tuberculosis. N Engl J Med. 2008;359:563–74. doi: 10.1056/NEJMoa0800106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah NS, Pratt R, Armstrong L, et al. Extensively drug-resistant tuberculosis in the United States, 1993–2007. JAMA. 2008;300:2153–60. doi: 10.1001/jama.300.18.2153. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. The Stop TB strategy: building on and enhancing DOTS to meet the TB-related millenium development goals. Geneva: World Health Organization; 2006. [Google Scholar]
- 30.Yew WW, Chan CK, Chau CH, et al. Outcomes of patients with multidrug-resistant pulmonary tuberculosis treated with ofloxacin/levofloxacin-containing regimens. Chest. 2000;117:744–51. doi: 10.1378/chest.117.3.744. [DOI] [PubMed] [Google Scholar]
- 31.Alangaden GJ, Manavathu EK, Vakulenko SB, Zvonok NM, Lerner SA. Characterization of fluoroquinolone-resistant mutant strains of Mycobacterium tuberculosis selected in the laboratory and isolated from patients. Antimicrob Agents Chemother. 1995;39:1700–3. doi: 10.1128/aac.39.8.1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Takiff HE, Salazar L, Guerrero C, et al. Cloning and nucleotide sequence of Mycobacterium tuberculosis gyrA and gyrB genes and detection of quinolone resistance mutations. Antimicrob Agents Chemother. 1994;38:773–80. doi: 10.1128/aac.38.4.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ginsburg AS, Grosset JH, Bishai WR. Fluoroquinolones, tuberculosis, and resistance. Lancet Infect Dis. 2003;3:432–42. doi: 10.1016/s1473-3099(03)00671-6. [DOI] [PubMed] [Google Scholar]
- 34.Shandil RK, Jayaram R, Kaur P, et al. Moxifloxacin, ofloxacin, sparfloxacin, and ciprofloxacin against Mycobacterium tuberculosis: evaluation of in vitro and pharmacodynamic indices that best predict in vivo efficacy. Antimicrob Agents Chemother. 2007;51:576–82. doi: 10.1128/AAC.00414-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kocagoz T, Hackbarth C, Unsal I, et al. Gyrase mutations in laboratory-selected, fluoroquinolone-resistant mutants of Mycobacterium tuberculosis H37Ra. Antimicrob Agents Chemother. 1996;40:1768–74. doi: 10.1128/aac.40.8.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Devasia RA, Blackman A, May C, et al. Fluoroquinolone resistance in Mycobacterium tuberculosis: an assessment of MGIT 960, MODS and nitrate reductase assay and fluoroquinolone cross-resistance. J Anti-microb Chemother. 2009;63:1173–8. doi: 10.1093/jac/dkp096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rieder HL, Cauthen GM, Comstock GW, Snider DE. Epidemiology of tuberculosis in the United States. Epidemiol Rev. 1989;11:79–98. doi: 10.1093/oxfordjournals.epirev.a036046. [DOI] [PubMed] [Google Scholar]
- 38.Raviglione MC. Tuberculosis, fourth edition: the essentials. New York: Informa Healthcare; 2009. [Google Scholar]
- 39.Nathanson E, Lambregts-van Weezenbeek C, Rich ML, et al. Multi-drug-resistant tuberculosis management in resource-limited settings. Emerg Infect Dis. 2006;12:1389–97. doi: 10.3201/eid1209.051618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Orenstein EW, Basu S, Shah NS, et al. Treatment outcomes among patients with multidrug-resistant tuberculosis: systematic review and meta-analysis. Lancet Infect Dis. 2009;9:153–61. doi: 10.1016/S1473-3099(09)70041-6. [DOI] [PubMed] [Google Scholar]