A confused and agitated 18-year-old woman presented to the emergency unit with orolingual movements, eye deviation, and a temperature of 38°C. The symptoms had begun 2 weeks prior to the admission when she developed a severe headache associated with pathologic laughing and intermittent episodes of upgaze deviation. A urine pregnancy test was positive and a transvaginal ultrasonography showed a 9-week-old fetus. An MRI of the brain was unremarkable and results of the CSF analysis were also unremarkable apart from a CSF pleocytosis (62 lymphocytes) and slightly elevated protein (55 mg/dL; normal range 0–45 mg/dL). Extensive microbiologic and serologic studies with CSF were all negative. She gradually lost consciousness, experienced respiratory failure, and was intubated. There were semirhythmic movements consisting of complex patterns of mouth opening, chewing, facial grimacing, synchronous flexion-extension, and supination-pronation limb movements, which persisted during the period of unresponsiveness. She also had generalized hyperreflexia, persistent hyperthermia, and a full bladder. Three EEGs showed diffuse slow waves with no epileptic discharges. A diagnosis of anti-NMDA receptor (NMDAR) encephalitis was made on clinical grounds and strongly positive serum NMDAR antibodies.
Three courses of IV immunoglobulin and one course of pulsed methylprednisolone were given along with other antidystonic and antichoreic drugs. The abnormal movements partially improved following treatment. Immunosuppressive drugs could not be implemented due to recurrent aspiration pneumonia. Neither ovarian nor mediastinal masses were found on MRI or CT scans. The patient delivered a baby at gestational age 34 weeks due to uteroplacental insufficiency. After the birth, the patient's movements diminished in severity and frequency. The patient was transferred to a hospital in her hometown but died shortly thereafter due to superimposed infection.
The baby had Apgar scores of 4, 7, 7 and weighed 1,755 g at birth. She had intermittent episodes of continuous fine abnormal movements that were spontaneous and were also precipitated by auditory stimuli. Phenobarbital was temporarily used to control the movements, which gradually diminished and disappeared. When the medicine was stopped after 2 weeks, the movements did not recur. The baby's serum was tested for NMDAR antibodies 2 days after birth and the titer was at the same level as the mother's (1:450). The titer declined at 2 months (1:150) and was negative at 1 year. At 2 years, the infant was delayed in global development and experienced generalized seizures. An EEG showed mildly diffuse encephalopathy and generalized epileptiform discharges. According to the Denver II assessment criteria, her developmental assessment at 3 years of age was comparable to the level of a 1-year-old. An MRI of the brain showed small low signal intensities (SI) on T1 and high SI on T2 images at the right superior frontal gyrus with well-demarcated gray–white differentiation suggestive of cortical dysplasia (figure).
Figure. Brain MRI of the infant.
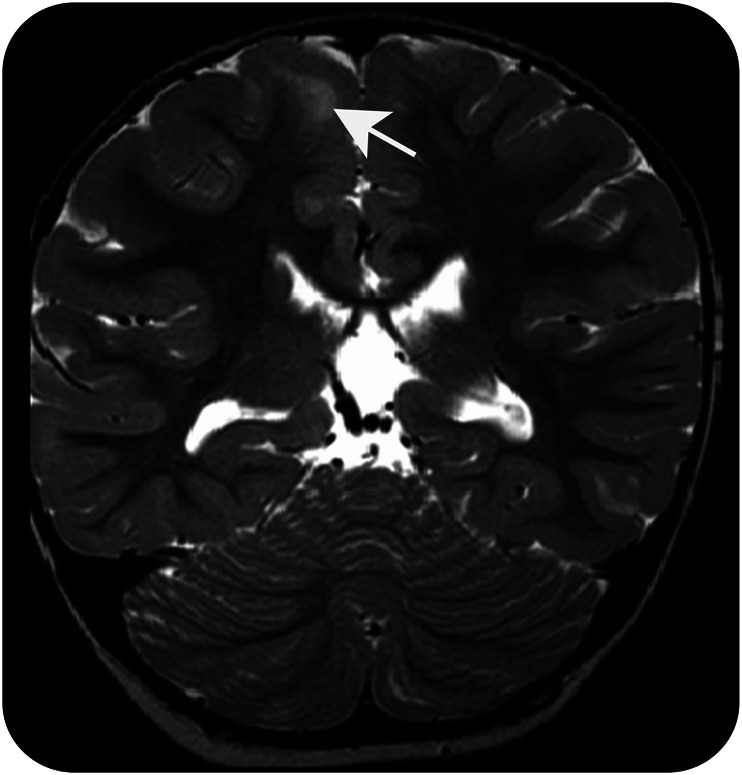
T2-weighted coronal MRI of the brain shows high signal intensities at the right superior frontal gyrus with well-demarcated gray–white differentiation suggestive of cortical dysplasia.
Discussion.
There have been only a few cases of anti-NMDAR encephalitis reported in pregnant women.1–4 Here, we report a case of transplacental transfer of the NMDAR antibodies. Of the 5 newborns reported in the literature, only one was tested for the antibodies in the umbilical cord blood, serum, and CSF, and the results were negative.3 In one case, the pregnancy was terminated because of the severity of neurologic symptoms and the early stage of pregnancy.3 All babies were reported to be normal except one infant who was found to have torticollis and strabismus at 4 and 6 months of age.1 The maximum follow-up period in these reports was 6 months but we have followed this girl for 3 years up to the present time.
Concern for the fetus and newborn is high in this disorder since there is evidence that immunoglobulin G (IgG)1 and IgG3 can cross the placenta by binding to an Fc neonatal receptor present in syncytiotrophoblasts from 13 weeks of gestation onwards, and NR1 antibodies from patients can decrease NMDAR clusters in in vitro and animal models.5,6 NMDARs have a major role in brain development. Too low or too high NMDAR function can cause abnormalities in brain development.7 However, it is not possible to say whether movement disorders in the perinatal period and the subsequent cortical dysplasia and developmental delay resulted from the transfer of maternal antibodies, maternal medication, or the indirect effect of maternal illness; equally challenging is how to prevent these occurring in future cases. Long-term follow-up of infants with mothers who develop anti-NMDAR encephalitis during pregnancy is indicated and may provide answers to these questions.
Acknowledgments
Acknowledgment: The authors thank Dr. Leslie Jacobson for testing the antibodies and their titrations.
Footnotes
Author contributions: Dr. Jagota: research project conception, organization, and execution, statistical analysis design and execution, writing of the first draft. A. Vincent: research project execution and manuscript review and critique. Dr. Bhidayasiri: research project organization and execution, statistical analysis review and critique, and manuscript review and critique.
Study funding: The Rachadaphiseksompot Endowment Fund of the “Strengthen CU's Researcher's Project” and Chulalongkorn University, Research Unit (RU) grant number GRU 56-012-30-002, to the Chulalongkorn Center of Excellence on Parkinson's Disease & Related Disorders, Bangkok, Thailand.
Disclosure: P. Jagota reports no disclosures relevant to the manuscript. A. Vincent and the University of Oxford hold patents and receive royalties and payments for antibody tests. R. Bhidayasiri serves as an associate editor of BMC Neurology and was an editor-in-chief of Thai Journal of Neurology, and receives funding from the Rachadaphiseksomphot Endowment Fund part of the “Strengthen CUs Researchers Project” and Research Unit (RU) grant of Chulalongkorn University, Bangkok, Thailand, royalties from International Neurology (Wiley-Blackwell) and Movement Disorders: A Video Atlas (Humana Press), and honoraria from Boehringer-Ingelheim, Glaxo-SmithKline, Abbott, and Novartis Pharmaceuticals. Go to Neurology.org for full disclosures.
References
- 1.Magley J, Towner D, Tache V, Apperson ML. Pregnancy outcome in anti-N-methyl-D-aspartate receptor encephalitis. Obstet Gynecol 2012;120:480–483. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy A, Dineen J, McKenna P, et al. Anti-NMDA receptor encephalitis with associated catatonia during pregnancy. J Neurol 2012;259:2632–2635. [DOI] [PubMed] [Google Scholar]
- 3.Kumar MA, Jain A, Dechant VE, et al. Anti-N-methyl-D-aspartate receptor encephalitis during pregnancy. Arch Neurol 2010;67:884–887. [DOI] [PubMed] [Google Scholar]
- 4.Ito Y, Abe T, Tomioka R, Komori T, Araki N. Anti-NMDA receptor encephalitis during pregnancy [in Japanese]. Rinsho Shinkeigaku 2010;50:103–107. [DOI] [PubMed] [Google Scholar]
- 5.Roopenian DC, Akilesh S. FcRn: the neonatal Fc receptor comes of age. Nat Rev Immunol 2007;7:715–725. [DOI] [PubMed] [Google Scholar]
- 6.Hughes EG, Peng X, Gleichman AJ, et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci 2010;30:5866–5875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aida T, Ito Y, Takahashi YK, Tanaka K. Overstimulation of NMDA receptors impairs early brain development in vivo. PloS One 2012;7:e36853. [DOI] [PMC free article] [PubMed] [Google Scholar]


