Abstract
A broodmare showed mild signs of abdominal discomfort and anemia after normal delivery. Ultrasonographic examination revealed a massive hematoma within the broad ligament adjacent to the uterine horn. Internal bleeding into the peritoneal cavity (hemoabdomen) was not seen. Following treatment, the clinical signs improved. Hemorrhage caused by rupture of the arteries within the broad ligament of the uterus may be a cause of hematoma. Prepartum and postpartum rupture of the arteries supplying the reproductive organs in the mare, which is not uncommon, can be fatal if severe hemoabdomen occurs. In the present case, the hematoma was considered to be tightly encapsulated between two serosal membrane layers of the broad ligament, and the membranes had remained intact. Thus, the serosal membranes did not split open, and massive bleeding into the peritoneal cavity did not occur. For this reason, the present broodmare avoided potentially fatal hemorrhagic shock.
Keywords: arterial rupture, broodmare, postpartum hematoma
Periparturient, pre-, and postpartum hemorrhage [1, 4, 5, 8, 9] in broodmares is often encountered in veterinary practice [9], and can be fatal if massive internal bleeding into the peritoneal cavity (hemoabdomen or hemoperitoneum) persists for a prolonged period. Such hemorrhage can result from rupture of the arteries supplying mainly the female reproductive organs, i.e., the uterine, ovarian, vaginal, and internal or external iliac artery [3, 10, 11]. Mares that have suffered this type of arterial rupture are often found dead, but may be discovered in shock [11]. Many of these mares will subsequently die, but approximately 50% of the mares may survive with treatment [11]. Mares that die from uterine artery rupture reveal a large volume of hemorrhage with free blood and clots into the abdominal cavity [3, 10, 11]. Mares that survive likely have a smaller arterial tear, with the small amount of hemorrhage in the abdomen and small hematoma confined within the broad ligament of the uterus [11]. This problem typically occurs in multiparous aged mares (usually aged more than10 years old) and is believed to result from weakening of the wall of the artery as a result of advanced age and the repeated enlargement and shrinkage of the vessels associated with multiple pregnancies over the lifetime of the mare [3, 10, 11]. There is an anecdote that mares that survive from uterine artery rupture have a tendency of failure to become pregnant in spite of mating. In this report, we describe a non-fatal and non-multiparous aged mare of large volume of hemorrhage accompanied by formation of a massive intra-serous membranous hematoma within the broad ligament of the uterus, possibly caused by rupture of an artery supplying the reproductive tract during parturition or after normal delivery, but without hemoabdomen.
Case History
The horse affected was a 7-year-old thoroughbred mare. The animal had no history of disease while being bred and reared as a broodmare on a stud farm in Japan, and had a history of two normal deliveries. The last pregnancy in a subsequent estrus to foal heat had been uneventful, and the foal was delivered at a gestational age of 339 days in early February, 2006. The interval from parturition in 2006 to delivery in 2007 was 1 year and 1 month. No specific problems had been reported during the pregnancy, which resulted in the unaided delivery of a clinically normal female foal in early March 2007. No signs of difficulty were observed during parturition or after birth. A small amount of bleeding from the vulva was observed, but this ceased after about 1 hr. However, after the delivery, the horse appeared unsettled, and showed signs of mild to moderate abdominal discomfort and anxiety-related behavior. The initial veterinary examination was performed 1 hr after delivery. The horse was treated in accordance with the guidelines for humane use and care equivalent to the NIH Guide for the Care and Use of Laboratory Animals.
Clinical Course
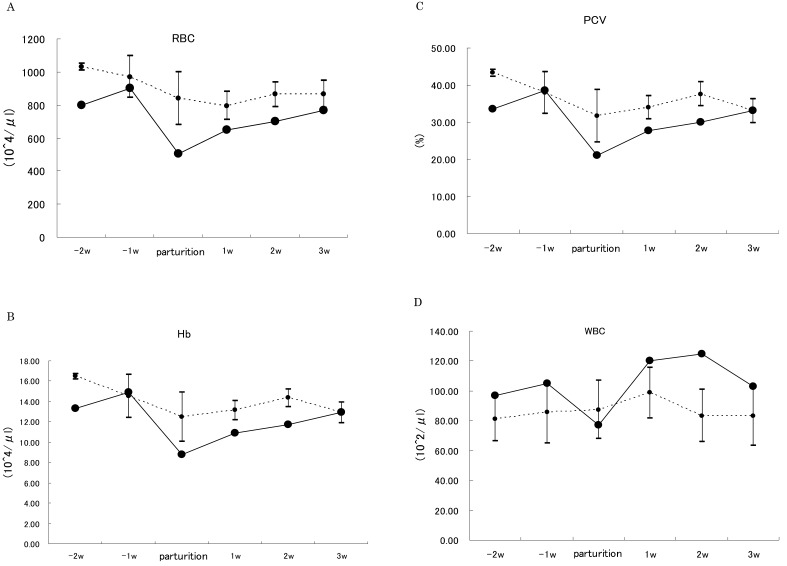
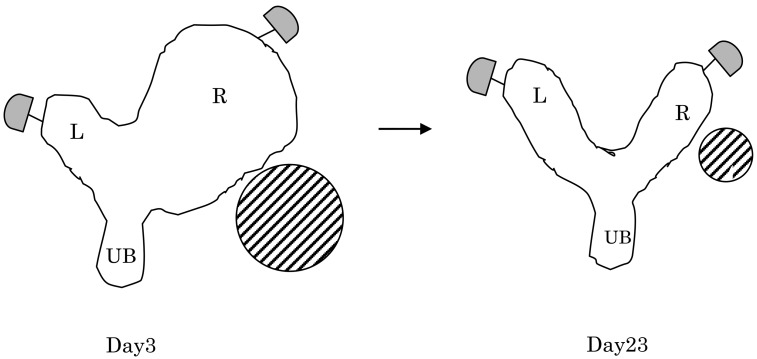
Apart from the above-mentioned unsettled behavior, the horse had a normal rectal temperature (38.1°C) and slight perspiration on the neck and the surrounding area. Palpation of the four limbs revealed a slightly cold sensation. Mild tachycardia (heart rate, 70–80 beats per min) and mild respiratory distress (respiratory rate, 15–20 breaths per min) were evident. The visible mucous membranes were slightly pale, and the oral mucosa was slightly dry. Auscultation of the abdomen revealed slight borborygmus. Auscultation of the chest revealed no abnormality. No other unusual findings were evident. The hematological parameters on the day of delivery (day 0) were: red blood cell count (RBC), 5.06 × 104/μl; RBC morphology, normal; hemoglobin concentration (Hb), 8.7 g/dl; packed cell volume (PCV), 21.1%; white blood cell count (WBC), 7,600/μl; mean corpuscular volume (MCV), 41.7 μm3 (fl); and mean corpuscular Hb concentration (MCHC), 41.7%. On the day of delivery, PCV, RBC count, and Hb were found to be lowered as compared with the reference value [2] and three age-matched Thoroughbred broodmares controls (Controls. 1–3) without previous abnormal breeding history (Figs. 1-A, -B, -C, -D), and no changes were observed in the periparturient period. Hence, hematologic findings of this case indicated mild anemia caused by hemorrhage. Per rectal palpation on day 3 revealed findings highly indicative of a massive hematoma within the broad ligament of the uterus. The palpated hematoma mass was as large as a volleyball and located in the area adjacent to the right uterine horn (Fig. 2). On day 3, trans-rectal ultrasonographic examination was performed with a 5.0-MHz probe to evaluate the abdomen and the genital tract of the mare. Ultrasonographic examination on day 3 revealed a large hyperechoic mass measuring 20 × 15 cm, extending directly to the right uterine horn from the body of the uterus (Figs. 2, 3). The hematoma increased slightly in size between days 3 and 8. The mass became harder by day 15, and then decreased to a size smaller than that of a handball by day 23, finally becoming grapefruit-sized by day 45. By day 30, the high echo region had gradually changed to several low-echo regions separated by fibrin-like elements (Fig. 4). The hematoma was palpable as a baseball-sized hard mass for up to 5 months after the event, and at approximately 6 months after delivery the mass had almost disappeared, as revealed by rectal and ultrasonographic examination. Ultrasonography revealed no blood accumulation in the ventral abdominal cavity, suggesting absence of hemoperitoneum. The PCV level was maintained within the range 33–39% for at least 3 weeks (Fig. 1-C). Treatments included a combination of quiet stall rest, fluid administration, analgesics, hemostatic agents as follows. To correct a blood loss, 4 liters of warmed isotonic saline solution was administered intravenously. To alleviate discomfort, the analgesic flunixin meglumine (50 mg/dl) was administered intravenously at 1.1 mg/kg body weight once daily for 4 days, starting on day 0. Tranexamic acid dissolved in distilled water at 50 mg/ml was also administered intravenously for 2 days to prevent acute blood loss by inhibiting the fibrinolytic action of plasminogen. A salt of maleic acid, ergometrine, was administered intravenously to promote uterine involution and hemostasis. In addition, 20 g of an oral powder formulation of bovine lactoferrin (Morinaga Milk Industry Co., Ltd., Japan) as a nutritional supplement (an iron-binding glycoprotein having multifunctional biological roles including an increase of hemoglobin and total serum iron values [7] and anti-inflammatory activity [7, 8]) was administered twice daily for 21 days after delivery. Most of the hematological parameters returned to almost normal by day 21. The horse’s appetite and drinking behavior were normal from day 3 to day 30, i.e., the day on which medical care was terminated. The blood progesterone concentrations at 8 and 19 days after delivery were 0.5 ng/ml and 5.2 ng/ml, respectively. Rectal palpation and ultrasound examination after delivery indicated the presence of follicles at 8 days (foaling heat) and corpus luteum at 19 days (later estrus) after delivery, suggesting that foal heat and ovulation had occurred normally.
Fig. 1.
A: Changes in the erythrocyte (RBC) counts of a broodmare during the periparturient period. B: Changes in hemoglobin concentration (Hb) of the broodmare during the periparturient period. C: Changes in packed cell volume (PCV) of the broodmare during the periparturient period. D: Changes in the leukocyte (WBC) counts of the broodmare during the periparturient period. Solid line indicates an affected mare. Dot lines indicate three age-matched Thoroughbred broodmares controls without previous abnormal breeding history. Values are expressed as the means ± SEM in controls.
Fig. 2.
Schematic presentation of the hematoma within the broad ligament adjacent to the right uterine horn on days 3 and 23. Diagonally striped circles indicate hematoma. R: Right uterine horn (pregnant horn), L: Left uterine horn, UB: Uterine body.
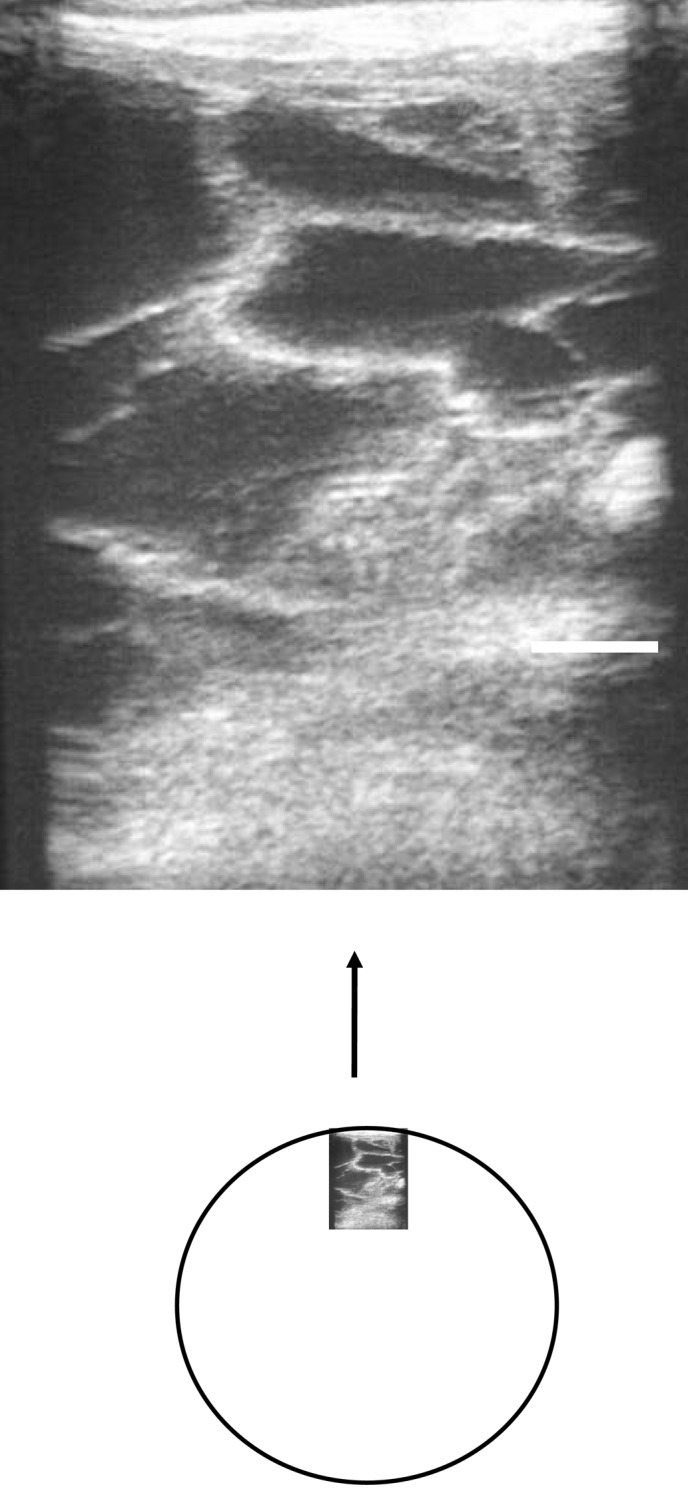
Fig. 3.
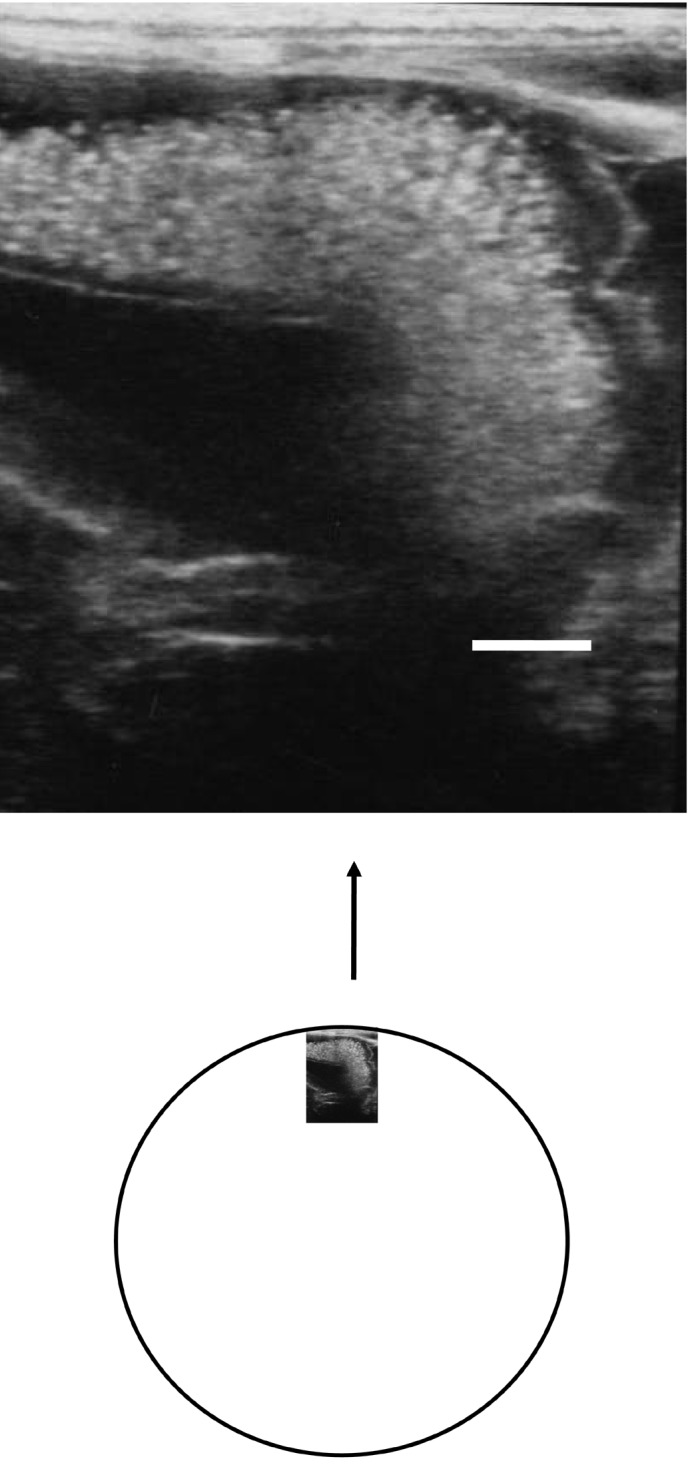
Ultrasonography performed on day 3 demonstrates a large hyperechoic mass, suggesting hematoma. As shown in a schema of whole part of hematoma as large as volley ball beside the right pregnant uterine horn. A hyperechoic area of surface part of hematoma, suggesting a clotted blood of hematoma. The inner part of hematoma indicates unclotted hematoma. Bar indicates 1 cm.
Fig. 4.
Ultrasonography of the hematoma on day 23 reveals loculated hyperechoic spaces surrounding anechoic areas. As shown in a schema, loculated hyperechoic parts (areas of clotted and/or organizing hematoma) inside surrounding anechoic parts (areas of unclotted hematoma) were visible. A size of the whole part of hematoma including unclotted and clotted hematoma was smaller than that of a handball. Bar indicates 1 cm.
Outcome
On day 30 after delivery, the treatment was discontinued. Afterwards, the horse was pasture-sound and required no medication. On day 80 after parturition, she was covered by a stallion and became pregnant in the same season. The mare had bred a healthy term foal through the normal delivery in the next season. No definite areas of hematoma within the broad ligament of the uterus after delivery either by rectal palpation or ultrasonography were revealed.
The broodmare we have reported developed a massive hematoma within the broad ligament of the uterus, possibly formed by blood released from the site of a rupture of the uterine arteries, during or just after normal delivery. The fact that the hematoma increased in size between days 3 and 8 suggests that the initial bleeding had filled and distended the space between the two serosal membrane layers in the broad ligament during this period, thus creating the massive hematoma. The subsequent decrease in size and hardening of the mass were considered to indicate that hematoma was heavily encapsulated, and became organized and consolidated between the two serosal membrane layers. The primary cause of the mild anemia was probably the uterine arterial rupture within the broad ligament. The horse probably survived because the membranes of the broad ligament remained intact and did not split, thus avoiding massive hemorrhage into the peritoneal cavity, and subsequent hemorrhagic shock. Why the pressure did not cause rupture of the broad ligament, allowing a large volume of hemorrhage into the abdomen remains to be determined. Antemortem diagnosis of uterine artery rupture can be made on the basis of clinical signs, careful rectal palpation, ultrasound examination, and abdominocentesis. However, uterine vessel rupture can be a devastating occurrence and no prevention is known. Therefore, for prognostication in pregnant mares, regardless of their clinical condition, it seems valuable to determine whether hematoma exists within the broad ligament, particularly near the uterine horn, during the periparturient period, as this will have a bearing on whether catastrophic rupture or a non-fatal course will ensue [9, 10].
The arterial rupture is distinctly age related, the probability increasing with each succeeding pregnancy beyond 10 years of age [10, 11]. Recent investigations have revealed that some broodmares with subclinical hemoperitoneum (silent hemorrhage) show clinical signs of mild anemia [1]. This type of bleeding occurs around the time of parturition. Minor intraperitoneal hemorrhage caused by a small rupture in the arteries located within the broad ligament can develop with no noticeable clinical symptoms. From a clinical viewpoint, the present case appeared to simulate such silent uterine postpartum hemorrhage [1].
In conclusion, the findings in the present case suggest that the mares should be closely monitored during periparturient period, and that the broodmare seems to be of value in confirming vascular rupture in the genital tract and the broad ligament of the uterus regardless of the age and breeding history in order that treatment can be quickly instituted.
References
- 1.Britt B.L.2003. Postpartum hemorrhage. pp. 327– 330. In: Current Therapy in Equine Medicine 5. (Robinson, N.E. ed.), W. B. Saunders, Philadelphia.
- 2.Parry B.W.2003. Normal clinical pathology data. pp. 870–886. In: Current Therapy in Equine Medicine 5. (Robinson, N.E. ed.), W. B. Saunders, Philadelphia.
- 3.Dwyer R.1993. Postpartum deaths of mares. Equine Dis. Q. 2: 5 [Google Scholar]
- 4.Frazer G.S.2004. Periparturient hemorrhage. pp. 1112–1114. In: Equine Internal Medicine. 2nd ed. (Reed, S.M., Bayly, W.M. and Sellon, D.C. eds.), Saunders, St. Luis.
- 5.Lofstedt R.1994. Haemorrhage associated with pregnancy and parturition. EquineVet. Educ. 6: 138–141 [Google Scholar]
- 6.Morn D.E.2009. Lactoferrin and other antimicrobial proteins. pp.142–143. In: Large Animal Internal Medicine, 4th ed. (Smith, B.P. ed.), Mosby, St. Luis.
- 7.Paesano R., Torcia F., Berlutti F., Pacifici E., Ebano V., Moscarini M., Valenti P.2006. Oral administration of lactoferrin increases hemoglobin and total serum iron in pregnant women. Biochem. Cell Biol. 84: 377–380 [DOI] [PubMed] [Google Scholar]
- 8.Perkins N.R., Frazer G.S.1994. Reproductive emergencies in the mare. Vet. Clin. North Am. Equine Pract. 10: 643–670 [DOI] [PubMed] [Google Scholar]
- 9.Roberts S.J.1986. Hemorrhage of pregnancy. p.710. In: Current Therapy in Theriogenology 2. (Morrow, D.A. ed.), W. B. Saunders, Philadelphia.
- 10.Rooney J.R., Robertson J.L.1996. Rupture of the uterine, ovarian, iliac arteries. pp. 237–238. In: Equine Pathology (Rooney, J.R. and Robertson, J.L. eds.). Iowa State University Press, Ames.
- 11.Williams N.2001. Uterine artery rupture. Equine Dis. Q. 10: 5–6 [Google Scholar]