Abstract
Objective
Varus thrust visualized during walking is associated with a greater medial knee and an increased risk of medial knee osteoarthritis (OA) progression. Little is known about varus thrust presence determined by visual observation relates to quantitative gait kinematic We hypothesized that varus thrust presence is associated with greater knee frontal plane dynamic movement during the stance phase of gait.
Methods
Participants had knee OA in at least one knee. Trained examiners assessed participants for varus thrust presence during ambulation. Frontal plane knee motion during ambulation captured using external passive reflective markers and an 8-camera motion analysis system. To examine the cross-sectional relationship between varus thrust and frontal plane knee motion, used multivariable regression models with the quantitative motion measures as dependent variables and varus thrust (present/absent) as predictor; models were adjusted for age, gender, BMI, gait speed, and knee static alignment.
Results
236 persons [mean BMI: 28.5 kg/m2 (SD 5.5), mean age: 64.9 years (SD 10.4), 75.8% women] contributing 440 knees comprised the study sample. 82 knees (18.6%) had definite varus thrust. Knees with varus thrust had greater peak varus angle and greater peak varus angular velocity during stance than knees without varus thrust (mean differences 0.90° and 6.65°/sec, respectively). These patterns remained significant after adjusting for age, gender, BMI, gait speed, and knee static alignment.
Conclusion
Visualized varus thrust during walking was associated with a greater peak knee varus angular velocity and a greater peak knee varus angle during stance phase of gait.
Keywords: Knee osteoarthritis, Instability, Varus thrust, Gait analysis
INTRODUCTION
Excessive loading during weight-bearing activities plays an important role in the pathogenesis of knee osteoarthritis (OA)1–4. Defined as the dynamic worsening or abrupt onset of varus (bow-leg) alignment as the limb accepts weight (stance phase), with a return to less varus and more neutral alignment during lift-off and the non-weight-bearing (swing) phase of gait, varus thrust is a potent mechanical risk factor for medial knee OA progression5. The presence of a varus thrust during gait may represent knee frontal plane dynamic instability and malalignment, possibly resulting from insufficient neuromuscular and peri-articular stabilization1.
In theory, reduced knee frontal plane stability and increased knee varus motion can lead to acute elevation of medial compartment load during the stance phase of gait and possibly accelerate structural damage. This theory is consistent with results of previous studies that showed knees with a visually observed varus thrust had a greater external knee adduction moment, a major determinant of medial compartment mechanical load during gait, than those without a thrust5–7. Varus thrust presence has also been associated with a 4-fold increase in the odds of medial OA radiographic disease progression5, demonstrating a deleterious effect of this abnormal lateral knee movement observed in walking. Knees with varus thrust have been reported to be at least 4 times more likely to have pain during weight-bearing activities than those without a varus thrust8.
Varus thrust observed during walking is a clinical finding that may identify some individuals with greater medial knee load and a higher risk for disease progression. Observation of gait is simple, quick, and inexpensive compared with measuring knee frontal plane dynamic instability in a laboratory using costly equipment and quantitative gait analysis. However, whether varus thrust presence determined by visual observation corresponds to a greater knee varus motion measured in quantitative gait analysis has not been investigated. Using non-invasive 3-dimensional motion analysis, knee frontal plane varus motion can be quantified by the peak varus angle and peak varus angular velocity during the stance phase. The peak knee varus angle represents the maximum knee varus position in stance. Defined as the change of angular position over time or as the time derivative of angular position, the peak knee varus angular velocity characterizes both the knee movement direction and speed (i.e., how fast the knee is moving into greater varus) in the frontal plane9, similar to what is seen with an observed varus thrust.
Increased knee varus motion during gait may represent an objective sign of the failure of the knee’s neuromuscular and peri-articular stabilizing mechanisms, manifested as a varus thrust, under dynamic and weight-bearing conditions. We hypothesized that varus thrust presence determined by visual observation is associated with a greater knee varus dynamic movement measured in quantitative gait analysis during the stance phase of gait.
METHODS
Sample
Study participants are enrolled in an ongoing natural history study of knee OA, the MAK-3 Study (Mechanical Factors in Arthritis of the Knee - Study 3) and were recruited from the community using advertising in periodicals targeting elderly persons, neighborhood organizations, letters to members of the registry of the Buehler Center on Aging and Illinois Women’s Health Registry, and via medical center referrals.
The MAK-3 cohort inclusion criteria were: definite tibiofemoral osteophyte presence, i.e., Kellgren/Lawrence (K/L) radiographic scoring system10 grade ≥ 2, in one or both knees; and a Likert category of at least “a little difficulty” for two or more items in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) physical function scale11. Exclusion criteria were: use of assistive ambulatory devices for more than 50% of the time during walking; corticosteroid injection within the previous three months; history of avascular necrosis, rheumatoid or other inflammatory arthritis, periarticular fracture, Paget’s disease, villonodular synovitis, joint infection, ochronosis, neuropathic arthropathy, acromegaly, hemochromatosis, gout, pseudogout, osteopetrosis, or meniscectomy; or exclusion criteria for magnetic resonance imaging (MRI) such as presence of a pacemaker, artificial heart valve, aneurysm clip or shunt, metallic stent, implanted device (e.g., pain control/nerve stimulator, defibrillator, insulin/drug pump, ear implant), or any metallic fragment in an eye.
Approval was obtained from the Office for the Protection of Research Subjects Institutional Review Boards of Northwestern University and Evanston Northwestern Healthcare. All participants gave written, informed consent.
Acquisition and Reading of Knee Radiographs
All participants underwent bilateral, anteroposterior, weight-bearing knee radiographs at baseline in the semi-flexed position with fluoroscopic confirmation of superimposition of the anterior and posterior plateau lines of the medial tibia and centering of the tibial spines within the femoral notch12. To describe the knees, the K/L radiographic score was used (0 = normal; 1 = possible osteophytes; 2 = definite osteophytes without definite joint space narrowing; 3 = definite joint space narrowing, some sclerosis, and possible attrition; and 4 = large osteophytes, marked narrowing, severe sclerosis and definite attrition). Reliability for radiographic grading for the single x-ray reader was high with a Kappa coefficient of 0.86.
Gait Observation for Varus and Valgus Thrust
Gait was observed for varus and valgus thrust presence by one of the two trained and experienced examiners (AC and KM) following a standardized protocol and script. To mirror regular daily walking, the participants wore their own gym shoes. Participants did not use any assistive devices during gait observation. Wearing a pair of shorts to expose the knees, the participant walked at a comfortable speed towards the examiner, away, and again towards the examiner in a dedicated 10-meter hallway. The examiner determined for each limb whether a varus thrust was present or not, whether a valgus thrust was present or not, and the level of confidence in the assessment, using a Likert scale of “very confident”, “somewhat confident”, “not very confident”, or “not at all confident”. The examiners were blinded to the knee disease status and the knee frontal plane motion data. For quality control purposes, the two examiners met every three months to observe three participants together. We have previously reported good intra-rater reliability for similarly trained examiners (Kappa 0.81)5.
Quantitative Gait Analysis
Gait analysis was performed in the Jesse Brown VA Medical Center Motion Analysis Research Laboratory (VAMC-MARL). Kinematic data were collected at 120 Hz, using an 8-camera, Eagle Digital Real-Time motion measurement system from Motion Analysis Corporation (MAC). At a sampling rate of 960 Hz, ground reaction forces and moments were measured with six AMTI (Advanced Mechanical Technology Inc., Watertown, MA, USA) force platforms embedded flush with the floor as participants walked along a 35×4 foot walkway. Following the Helen Hayes full-body marker set, a widely used, standardized marker arrangement for 3-dimensional (3-D) motion analysis13, an experienced examiner placed external passive reflective markers bilaterally on the tip of the acromion process, lateral humeral epicondyle, centered between the styloid processes of the radius and ulna, anterior superior iliac spine, superior aspect of the sacrum at the L5/sacral interface, lower thigh, along the flexion/extension axis of rotation at the lateral femoral condyle, lower leg, along the flexion/extension axis of rotation at the lateral malleolus, posterior calcaneus, c enter of the foot between the 2nd and 3rd metatarsals. OrthoTrak gait analysis software (MAC) was used to calculate 3-D joint angles and temporal-spatial parameters of gait. Knee angles were calculated using Euler (fixed axis) rotations performed in the following sequence – flexion/extension, abduction/adduction, internal/external rotation.
For the walking trial, each participant wore his/her own gym shoes and walked at a self-selected comfortable speed across the walkway without using any assistive devices. A minimum of five trials having clean foot strikes on the force platforms for the left and right feet were acquired, with rest between trials. The knee angular velocity was computed by taking the time derivative of knee angle in the frontal plane. For knee frontal plane dynamic motion measures, we identified the peak knee varus angle during the entire stance and during each sub-phase of stance14,15 (early stance: 0–16% of stance; mid stance: 17–50%; terminal stance: 51–83%; pre-swing: 84–100%), and peak knee varus angular velocity during stance, using custom Matlab programs. The reliability of measuring peak knee varus and valgus angle during stance was excellent with an intraclass correlation coefficient (ICC) of 0.98–0.99.
Acquisition and Measurement of Knee Mechanical Alignment as a Covariate
To assess knee static alignment, a single anteroposterior radiograph of both lower extremities was obtained using a 51×14–inch graduated-grid cassette, which was large enough to capture the hip-knee-ankle joints of all participants, even the tallest. All radiographs were obtained in the same unit by two trained technicians. Alignment (i.e., the hip–knee–ankle angle) was measured as the angle formed by the intersection of the line connecting the centers of the femoral head and intercondylar notch with the line connecting the centers of the surface of the ankle talus and tips of the tibial spines. Image analysis16 was completed by one of three trained readers using a customized program (Surveyor 3; OAISYS Inc, Kingston, Ontario, Canada), blinded to all other data. In a reliability study of 200 full-limb pairs assessed by these three readers, the inter- and intra-reader ICCs were 0.95 and 0.9617. In our analyses, varus was defined as 178°or less, valgus as 182°or greater and neutral as 178–182°.
Statistical Analysis
Characteristics of study participants are summarized using means and standard deviations (SDs) for continuous variables [age and body mass index (BMI)], and percentages for dichotomous/categorical variables. For knee level variables, similar summary statistics are used: disease severity is summarized via K/L grade distribution, knee mechanical alignment is analyzed as a continuous variable and presence of varus thrust is a dichotomous variable.
Varus thrust presence was defined as a very confident assessment of varus thrust recorded by the examiner; the comparison group consisted of knees without any thrust or with a valgus thrust, each with a very confident assessment. In the knee-based analysis, we used multivariable regression models to examine the cross-sectional relationships between knee frontal plane dynamic motion measures (dependent variables) obtained in quantitative gait analysis and varus thrust presence (dichotomous predictor variable). All models were fit using generalized estimating equations (GEE) methodology to account for correlations between knees within each person18. All regression analyses were done first as unadjusted models, and then adjusted for age, gender, BMI, and gait speed, and finally further adjusted for knee alignment. Results are reported as the estimated mean differences and associated 95% confidence intervals in the knee frontal plane dynamic motion measures between the varus thrust positive and negative groups.
RESULTS
Of the original MAK-3 sample of 250 persons, 4 who did not undergo gait observation were excluded. Of the remaining 492 knees from 246 persons, based upon the definitions of varus thrust presence and absence, 52 knees were excluded due to a gait observation confidence level other than “very confident”, resulting in the analysis sample of 440 knees from 236 persons. The mean BMI and age were 28.5 kg/m2 (SD 5.5) and 64.9 years (SD 10.4), respectively. 75.8% were women. Of the 440 knees, 22 (5.0%) were K/L grade 0, 75 (17.0%) were K/L 1, 199 (45.2%) were K/L 2, 57 (13.0%) were K/L 3, 72 (16.4%) were K/L 4, and 15 (3.4%) did not undergo K/L reading, primarily due to total knee replacement. The mean knee mechanical alignment was 1.05 degrees (SD 4.14) in the varus direction. 82 (18.6%) of the knees had a definite varus thrust, i.e., for each of these knees, the examiner was “very confident” that the knee demonstrated a varus thrust. Twenty-four persons had bilateral and 34 persons had unilateral varus thrust observed during gait. Twelve knees (2.7%) had a definite valgus thrust. Table 1 shows person-level and knee-level characteristics of those with and without a varus thrust.
Table 1.
Characteristics of persons and knees with vs. without a definite varus thrust
| Person-level characteristics | With definite varus thrust n=58 Mean (SD) | Without varus thrust n=178 Mean (SD) | |
| Age (year) | 65.6 (8.6) | 64.7 (10.9) | |
| Gender | 38 (female) vs. 20 | 141 (female) vs. 37 | |
| BMI (kg/m2) | 30.7 (6.0) | 27.8 (5.2) | |
| Knee-level characteristics | With definite varus thrust n=82 | Without varus thrust n=358 | |
| K/L grade 0, no. (row %) | 4 (18%) | 18 (82%) | |
| 1 | 6 (8%) | 69 (92%) | |
| 2 | 24 (12%) | 175 (88%) | |
| 3 | 15 (26%) | 42 (74%) | |
| 4 | 33 (46%) | 39 (54%) | |
| No reading | 0 (0%) | 15 (100%) | |
| Knee alignment (°), mean (SD) | 4.7 (4.3) | 0.3 (3.7) | |
SD: standard deviation.
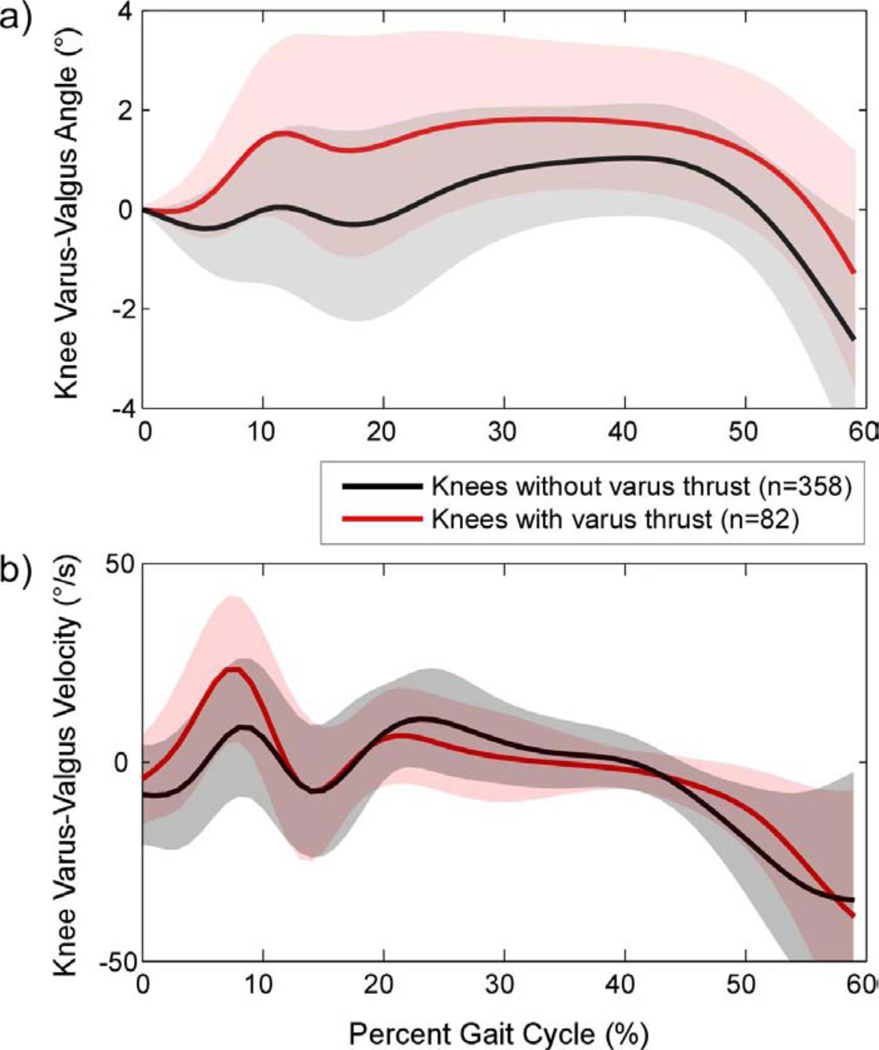
Figure 1 shows the ensemble average curves for the knee varus-valgus angle (Figure 1a) and angular velocity (Figure 1b) during the stance phase of gait cycle for knees with positive varus thrust vs. knees without a varus thrust. Table 2 summarizes the results of each knee frontal plane quantitative motion measure overall, and stratified by varus thrust status.
Figure 1.
Frontal plane knee angle (figure a) and angular velocity (figure b) curves during the first 60% of gait cycle (mainly stance phase of walking) in knees with visually observed varus thrust (red line) vs. knees without thrust (black line). Varus is in the positive direction. Solid lines represent the ensemble averages and shaded areas represent ± one standard deviation around the average values. The initial knee position at the beginning of stance was normalized to “zero” for ease of comparison. In the varus thrust positive group, the maximum knee varus angle occurred near the beginning of the mid stance phase for the ensemble average curve, and remained near the maximum throughout the entire mid stance phase, eventually returning to baseline at the end of stance. Note the corresponding greater increase of knee varus angular velocity. It is important to point out that each knee’s peak varus angle and angular velocity occurred at a slightly different time point during the early to mid stance phase of gait, and thus averaging these magnitudes at each time point likely will attenuate the individual knees’ peak values. Nonetheless, the general trend of greater knee varus angle and angular velocity is evident in knees with a varus thrust compared to knees without a varus thrust.
Table 2.
Means (SDs) of knee frontal plane quantitative motion measures during gait by varus thrust status
| Measures of frontal plane motion during gait | All knees | Knees with varus thrust |
Knees without varus thrust |
|---|---|---|---|
| n = 440 Mean (SD) |
n = 82 Mean (SD) |
n = 358 Mean (SD) |
|
| Peak knee varus angle during stance (°) | 1.77 (1.28) | 2.51 (1.55) | 1.60 (1.15) |
| Peak knee varus angle during early stance (°) | 0.72 (0.98) | 1.55 (1.29) | 0.53 (0.79) |
| Peak knee varus angle during mid-stance (°) | 1.32 (1.50) | 2.27 (1.64) | 1.10 (1.38) |
| Peak knee varus angle during terminal stance (°) | 1.42 (1.22) | 2.03 (1.47) | 1.28 (1.11) |
| Peak knee varus angle during pre-swing (°) | −0.16 (1.51) | 0.66 (1.67) | −0.35 (1.40) |
| Peak knee varus angular velocity (°/sec) | 26.81 (15.24) | 32.23 (14.23) | 25.57 (15.22) |
Knee frontal plane quantitative measures are presented in all knees, in knees with varus thrust only, and in knees without varus thrust.
SD: standard deviation.
As shown in Table 3, knees with a definite varus thrust had a statistically significantly greater peak knee varus angle during the entire stance and each sub-phase as well as greater peak knee varus angular velocity. These patterns remained significant after adjusting for age, gender, BMI, and gait speed. Findings persisted after further adjustment for knee alignment, although with some reduction of the mean difference magnitudes in some instances. Notably, the association between varus thrust and greater knee varus angular velocity was not affected by further adjustment for knee alignment. During ambulation, knees with varus thrust on average had 7 degrees per second faster varus angular velocity than did those without varus thrust.
Table 3.
Estimated differences in means for knee frontal plane motion measures based on presence vs. absence of varus thrust, from the multiple regression models fit via generalized estimating equations (GEE) (n = 440)
| Measures of frontal plane motion during gait | Difference* (95% confidence interval) |
|||
|---|---|---|---|---|
| Unadjusted | Adjusted for age, gender, and BMI |
Adjusted for age, gender, BMI, and gait speed |
Adjusted for age, gender, BMI, gait speed, and alignment |
|
| Peak knee varus angle during stance (°) | 0.90 (0.51, 1.30) | 0.95 (0.55, 1.36) | 0.96 (0.56, 1.36) | 0.49 (0.13, 0.85) |
| Peak knee varus angle during early stance (°) | 1.02 (0.68, 1.35) | 1.03 (0.69, 1.37) | 1.04 (0.70, 1.38) | 0.58 (0.29, 0.87) |
| Peak knee varus angle during mid-stance (°) | 1.16 (0.72, 1.59) | 1.29 (0.83, 1.75) | 1.28 (0.82, 1.75) | 0.56 (0.19, 0.94) |
| Peak knee varus angle during terminal stance (°) | 0.74 (0.35, 1.13) | 0.81 (0.40, 1.21) | 0.81 (0.41, 1.21) | 0.27 (−0.06, 0.61) |
| Peak knee varus angle during pre-swing (°) | 0.99 (0.55, 1.44) | 0.92 (0.45, 1.38) | 0.91 (0.45, 1.38) | 0.59 (0.12, 1.05) |
| Peak knee varus angular velocity (°/sec) | 6.65 (2.99, 10.31) | 6.76 (2.79, 10.73) | 7.20 (3.56, 10.84) | 6.78 (2.55, 11.01) |
Positive difference indicates greater mean value for knees with varus thrust vs. those without varus thrust.
95% CI that excludes 0 indicates a statistically significant difference between the groups, and is shown in bold font.
Among 440 knees in our analysis sample, 82 (18.6%) had varus thrust with a “very confident” rating and 22 knees (5%) had a varus thrust with a “somewhat confident” rating. A sensitivity analysis using an alternative definition of varus thrust presence during walking by including the additional 22 knees yielded similar results.
DISCUSSION
Varus thrust presence visualized during gait observation was associated with a greater mean peak knee varus angular velocity during stance and a greater mean peak knee varus angle during stance and during most sub-phases of stance measured by 3-D motion analysis. Most the differences remained statistically significant after adjusting for age, gender, BMI, gait speed, and static knee alignment. For example, knees with a varus thrust had an approximately 7 degrees per second greater mean varus angular velocity than knees without a varus thrust, in unadjusted and adjusted analyses. Compared to peak knee varus angle, the peak knee varus angular velocity more closely corresponded to a visualized varus thrust and may be a more suitable index for capturing the dynamic nature of a varus thrust.
This is the first study to investigate whether varus thrust presence determined by visual observation corresponds to a greater knee varus motion measured in quantitative gait analysis. Frontal plane knee angle during ambulation in persons with knee OA has been examined in a limited scope. A few studies explored the cross-sectional relationship between peak knee varus angle and several neuro-mechanical parameters, including muscle strength, joint laxity, proprioceptive acuity, knee static alignment, and external knee adduction moment19–21. In a single case study, Hunt and colleagues demonstrated that the index knee with an observed varus thrust had a greater peak knee varus angle than the contralateral knee without a thrust; and that the peak knee varus angle could be reduced by various gait modification strategies6.
In the current study, both peak knee varus angle and angular velocity were included as indicators of knee frontal plane motion. The knee peak varus angle has been used to quantify frontal plane joint instability6,19,21, however the peak joint varus angle only reveals the position of the knee at one instant of time and does not fully capture the direction and speed of the dynamic movement seen in a varus thrust. The knee varus angular velocity, on the other hand, embodies not only direction but also speed of motion. Our analysis showed that the mean difference in peak knee varus angle between knees with and without a varus thrust was reduced after further adjusting for static knee alignment, but remained significantly different from zero. This makes sense in that greater varus alignment may contribute to a greater peak varus angle during walking. Since varus angular velocity represents speed of movement and is less closely related to knee position, it was not surprising that the difference in angular velocity between knees with and without varus thrust was not explained by static varus alignment. Compared with knees without a thrust, having a varus thrust visualized during gait corresponded to a 7 degrees per second faster mean knee frontal plane movement into greater varus alignment.
The mean peak knee varus angle during stance phase for the entire study sample was 1.77 (SD 1.28) degrees, which falls within the range of 1.37 to 4.51 degrees found in other studies19–21. On average, the peak knee varus angle occurred at 25% time of stance phase, in agreement with the 20–32% time reported in previous research6,20,21. It is important to note that the timing of peak varus angle corresponds with the beginning of mid stance phase where the limb starts to bear full body weight and thrust is most visible. Our cohort had a mean peak knee varus angular velocity of 26.81 (SD 15.24) degrees per second, similar to 21.7 reported in the only previous study measuring the knee frontal plane velocity in 17 participants with knee OA20.
Varus thrust during walking was present in 17–36% of three separate cohorts of persons with knee OA5,8,22. Biomechanically, an abrupt elevation of medial knee load imparted by a varus thrust with each step may cause cartilage degradation, bone marrow lesions, and meniscal damage. This cyclical dynamic impact during the most common weight-bearing activity, walking, could be more detrimental than static varus malalignment assessed in standing. Among varus-aligned knees, thrust increased the likelihood of medial disease progression 3-fold5, indicating the thrust had an added influence on medio-lateral compartment load balance than varus malalignment alone. In addition, varus thrust had a stronger association with greater overall knee pain, particularly during weight-bearing activities, than did varus malalignment8. Compared with full-limb radiographs for capturing knee mechanical alignment or quantitative gait analysis performed in a lab with costly equipment for measuring knee frontal plane dynamic instability, thrust observation during gait is a simple clinical tool accessible to most clinicians. The findings of this study provide evidence that varus thrust observed during walking is associated with an elevated knee varus angle and angular velocity during the early stance phase of gait, where the limb accepts the full body weight, supporting gait observation for varus thrust.
Our hypotheses dealt with the relationship between observed varus thrust and quantitative knee frontal plane dynamic motion during gait in both knees of persons with knee OA in one or both knees. Having radiographic OA in one knee is associated with a substantially higher risk of having OA in the contralateral knee. There is evidence that many such knees have pre-radiographic OA lesions. To enable generalizing results to persons with OA, we included both knees of participants including the full spectrum of disease severity.
There are several limitations in this study. Even as performed by a trained and experienced examiner, marker placements in quantitative gait analysis can be a potential source of variability in the frontal plane knee motion measures. Despite this potential source of variability, we were able to detect significant differences between knees with and without a varus thrust. Gait observation is a subjective assessment. Therefore, as our primary approach, we included only the “very confident” rating recorded by the examiner for thrust presence vs. absence. A further sensitivity analysis that included both the “very confident” and “somewhat confident” ratings yielded similar results, suggesting a robust relationship between having a varus thrust and increased knee varus movement quantified by motion analysis. We reported good inter-rater reliability of thrust observation, but do not have data on inter-rater reliability. Assignment of examiners to participants was based on schedules and availability of examiners, and we do not anticipate any biases due to this assignment process. Given the expertise of the examiners and the scheduled quality control measures, we expect that the inter-rater reliability would be high. If not, this source of measurement variability would tend to bias our comparisons toward the null hypothesis.
In conclusion, varus thrust presence by clinical gait observation was associated with a greater peak knee varus angular velocity, which captures both the direction and speed of dynamic movement, and a greater peak knee varus angle during stance recorded by a 3-D motion analysis system.
ACKNOWLEDGEMENTS
The authors would like to thank Mr. Clifton Saurel and Ms. Rebecca Stein for assistance in data collection and all study participants for their contribution to the study.
FUNDING SOURCES
Support for this project comes from National Institutes of Health (NIH) P60 AR048098 (PIs: Pope/Sharma), NIH R01 AR054806 (PI: Sharma), and NIH R01 AR048748 (PI: Sharma).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AUTHOR CONTRIBUTIONS
Each author participated in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. All authors have access to the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Chang, Chmiel, Sharma
Acquisition of data. Chang, Moisio, Zhang, Cahue, Sharma
Analysis and interpretation of data. Chang, Chmiel, Moisio, Almagor, Zhang, Cahue, Sharma
COMPETING INTERESTS
The authors declare no competing interests.
Contributor Information
Alison H. Chang, Email: hsini@northwestern.edu.
Joan S. Chmiel, Email: jchmiel@northwestern.edu.
Kirsten C. Moisio, Email: k-moisio@northwestern.edu.
Orit Almagor, Email: o-almagor@northwestern.edu.
Yunhui Zhang, Email: y-zhang3@northwestern.edu.
September Cahue, Email: cahue@ajrr.net.
Leena Sharma, Email: l-sharma@northwestern.edu.
REFERENCES
- 1.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 3.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61(7):617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennell KL, Bowles K-A, Wang Y, Cicuttini F, Davies-Tuck M, Hinman RS. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis. 2011;70(10):1770–1774. doi: 10.1136/ard.2010.147082. [DOI] [PubMed] [Google Scholar]
- 5.Chang A, Hayes K, Dunlop D, Hurwitz D, Song J, Cahue S, et al. Thrust during ambulation and the progression of knee osteoarthritis. Arthritis Rheum. 2004;50(12):3897–3903. doi: 10.1002/art.20657. [DOI] [PubMed] [Google Scholar]
- 6.Hunt MA, Schache AG, Hinman RS, Crossley KM. Varus thrust in medial knee osteoarthritis: Quantification and effects of different gait-related interventions using a single case study. Arthritis Care Res (Hoboken) 2011;63(2):293–297. doi: 10.1002/acr.20341. [DOI] [PubMed] [Google Scholar]
- 7.Williams DS, Isom W. Decreased frontal plane hip joint moments in runners with excessive varus excursion at the knee. J Appl Biomech. 2012;28(2):120–126. doi: 10.1123/jab.28.2.120. [DOI] [PubMed] [Google Scholar]
- 8.Lo GH, Harvey WF, McAlindon TE. Associations of varus thrust and alignment with pain knee osteoarthritis. Arthritis Rheum. 2012;64(7):2252–2259. doi: 10.1002/art.34422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winter DA. Biomechanics and Motor Control of Human Movement. 4th ed. Wiley; 2009. Kinematics; pp. 45–81. [Google Scholar]
- 10.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 12.Buckland-Wright C. Protocols for precise radio-anatomical positioning of the tibiofemoral and patellofemoral compartments of the knee. Osteoarthr Cartil. 1995;3(Suppl A):71–80. [PubMed] [Google Scholar]
- 13.Perry J, Burnfield JM. Gait Analysis: Normal and Pathological Function. Second Edition. Slack Incorporated; 2010. Motion analysis; pp. 407–422. [Google Scholar]
- 14.Thorp LE, Wimmer MA, Block JA, Moisio KC, Shott S, Goker B, et al. Bone mineral density in the proximal tibia varies as a function of static alignment and knee adduction angular momentum in individuals with medial knee osteoarthritis. Bone. 2006;39(5):1116–1122. doi: 10.1016/j.bone.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Perry J, Burnfield JM. Gait Analysis: Normal and Pathological Function. Second Edition. Slack Incorporated; 2010. Phases of gait; pp. 9–16. [Google Scholar]
- 16.Cooke TDV, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34(9):1796–1801. [PubMed] [Google Scholar]
- 17.Sled EA, Sheehy LM, Felson DT, Costigan PA, Lam M, Cooke TDV. Reliability of lower limb alignment measures using an established landmark-based method with a customized computer software program. Rheumatol Int. 2011;31(1):71–77. doi: 10.1007/s00296-009-1236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 19.Van der Esch M, Steultjens M, Harlaar J, Wolterbeek N, Knol DL, Dekker J. Knee varus-valgus motion during gait--a measure of joint stability in patients with osteoarthritis? Osteoarthr Cartil. 2008;16(4):522–525. doi: 10.1016/j.joca.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Foroughi N, Smith RM, Lange AK, Baker MK, Fiatarone Singh MA, Vanwanseele B. Dynamic alignment and its association with knee adduction moment in medial knee osteoarthritis. Knee. 2010;17(3):210–216. doi: 10.1016/j.knee.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Kuroyanagi Y, Nagura T, Kiriyama Y, Matsumoto H, Otani T, Toyama Y, et al. A quantitative assessment of varus thrust in patients with medial knee osteoarthritis. Knee. 2012;19(2):130–134. doi: 10.1016/j.knee.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Chang A, Hochberg M, Song J, Dunlop D, Chmiel JS, Nevitt M, et al. Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk of developing knee osteoarthritis. Arthritis Rheum. 2010;62(5):1403–1411. doi: 10.1002/art.27377. [DOI] [PMC free article] [PubMed] [Google Scholar]