Abstract
This manuscript captures the discussion and recommendations that came out of a special Afro Asian symposium involving 13 countries. Unmet needs and cost-effective solutions with special emphasis on training form the backbone of practical next steps.
Keywords: Cancer burden, cost effective, health policy, training, unmet needs
Introduction
An Afro-Asian symposium was conducted at the Apollo Cancer Conference at the beginning of 2014. Several countries came together to discuss their oncology situation and needs. This manuscript captures the current scenario and important deliberations during that session. The objective is to seek a common ground for mutual cooperation that will help us learn from each other as well as find unique solutions that would optimize patient management with the available resources.
Materials and Methods
The discussion during the symposium focused on the current scenario of cancer challenges faced by each participating country, their priority areas, and unmet needs. Thereafter, each country representative oncologist was sent an 18-item questionnaire to formally capture salient features of their cancer burden, most common cancers faced, available human resource, oncology education, infrastructure, priority areas (in service, education, and research) as well as their wish list to address unmet needs. The replies were tabulated and analyzed. After further discussion among the respondents, this manuscript was developed as a road map for future cooperation.
Results
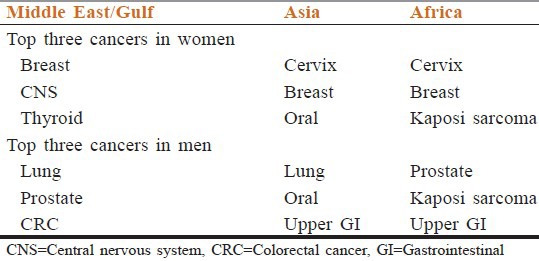
Of the 16 participants in the symposium, 13 countries replied to the questionnaire [Figure 1]. The population of these 13 countries totals 1,980,900,000 people-amounting to 29.35% of the world's human being.[1] The total annual cancer incidence of these countries is 1,474,900 new cases. Of this 64.4% are from India (almost two-third of the burden).[2] The remaining countries were divided into three groups, other south Asian countries, Middle East (Gulf) countries, and African countries. They share 21, 1, and 14% of the region's cancer burden, respectively. Table 1 shows the population and cancer burden of each of these countries. Key highlights of infrastructure, human resource, and ongoing anticancer strategies are summarized in Table 2.[2,3,4,5,6,7,8,9] The number of cancer hospitals in each country varies from zero in Kenya and Zimbabwe to 27, the highest in India. The number of radiotherapy machines available range from zero (in Bhutan) to 300 in India. Formal oncology degree training is not available in four countries. Official cancer management guidelines are available in three countries, present for a single disease in two more, and have not been developed in the remaining. While only two countries do not have a cancer registry, the majority have only hospital-based ones. Figure 2 shows the ratio of new cancer patients per oncologist per year in each of the countries. As expected, the Gulf countries have more qualified oncologists, each one having to cater to 33 (UAE) to 42 (Oman) new cancer patients per year. The most challenging situation is for Uganda (10,800), Nigeria (3,915), and Kenya (2,800). Table 3 also outlines the available number of oncologists per 100,000 of each country's population. Table 4 compares the three most common cancers in each country among the males and females. Among the females, breast cancer remains in the top three for all regions and highest in gulf countries. Cervical cancer which is the commonest in Asia and Africa does not feature as an important type in the Gulf. Among men, lung cancer, prostate cancer, and gastrointestinal cancers are the common thread. As expected, Kaposi's sarcoma is highly prevalent in Africa, where human immunodeficiency virus (HIV) is still a major healthcare issue. The high incidence of oral cancer in Asia reflects the use of smokeless tobacco.
Figure 1.
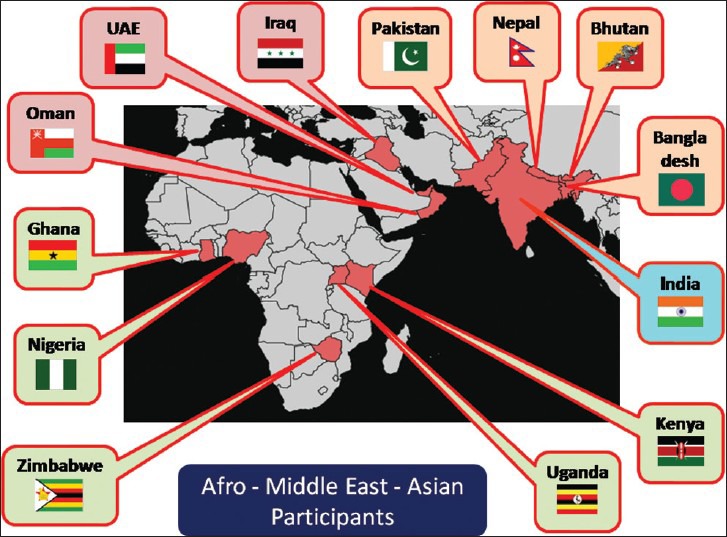
Geographical location of the 13 countries contributing to this manuscript
Table 1.
Comparison of population and cancer incidence in different regions
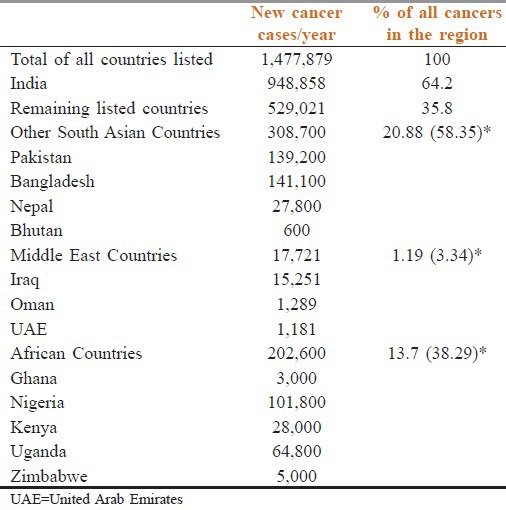
Table 2.
Insight into oncology status of various countries
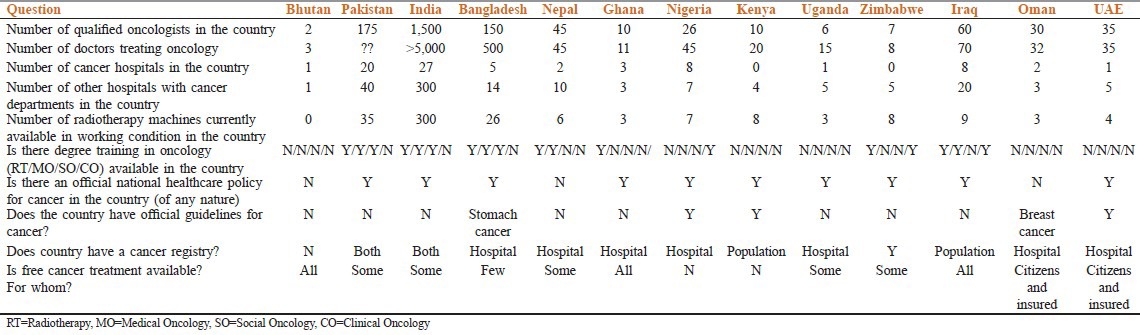
Figure 2.
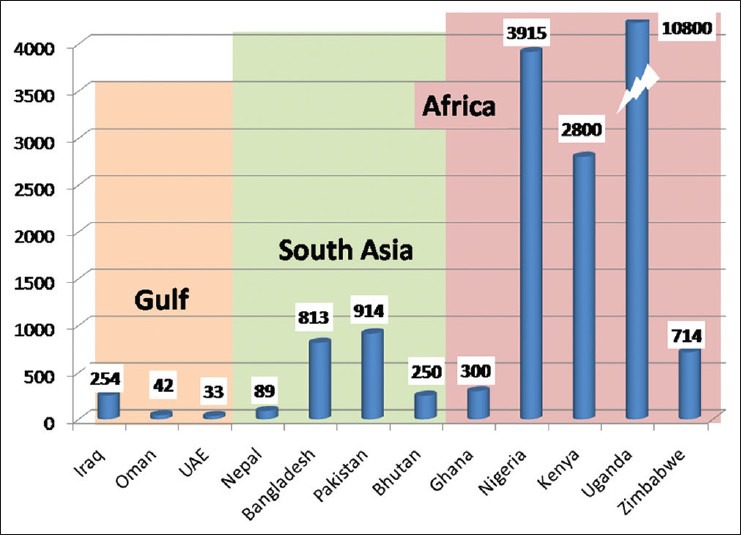
Ratio of new cancer patients per oncologist per year in each country
Table 3.
Trained oncologists available per population and their cancer patients (other than India)
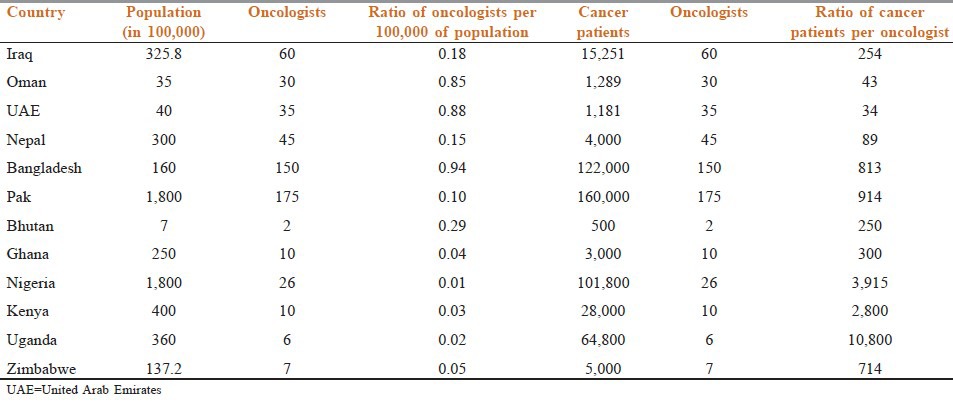
Table 4.
Top three cancers among women and men in the three regions
Discussion
Since the participating countries represent almost 30% of the global population, our unique circumstances and experiences can be the basis of mutual learning and problem solving. With most countries having limited resources, finding cost-effective and impactful solutions becomes even more crucial. With India experiencing 64.4% of the regions cancer burden, it has a leading role to play in compiling and sharing success stories in tackling this rising menace.[2] For instance India has 27 dedicated cancer hospitals and an additional 300 general or multispecialty hospitals that provide care to cancer patients. Cancer is the fourth leading cause of death in India in the 25-69 year age group, and 1,500 trained oncologists manage this disease under its official national cancer control program. With 2.4 million persons with cancer at any given point of time in India, the ratio of cancer patients to oncologists is high, that is, 1,600:1. Our region's cancer burden is expected to grow due to unhealthy lifestyle, aging of the population as well as the increase in the number of cancer survivors. Coupled with our collective current limitations (financial, administrative, and others) we must accept that our preparedness for the future, is at best woefully inadequate. That published global figures (Globocan, International Agency for Research on Cancer (IARC), World Health Organization (WHO), etc.) are an underestimate of cancer incidence in our countries heightens the gaps.[9] If we take the example of breast cancer in India, Indian Council of Medical Research's Population Based Cancer Registry of New Delhi shows the incidence to be 29.3 per 100,000 of the population in 1994-1995.[10,11] And the Indian Cancer Society's Maharashtra Population Based Registry shows it to be 26.8 per 100,000 of the population in 2001.[11,12] Both these figures are higher than the <19.5 incidence per 100,000 population showed in Globocan 2002 data.[9]
A three-pronged strategy will require attention to service, education, and research. The first step remains education. This should be at various levels-right from training and updating cancer specialists to primary physicians, nurses, and even lay public (especially those at high risk for malignancies, e.g., tobacco users). While all countries do this in some manner, a systematic approach is required. This will allow a uniform message to be conveyed as well as impact monitoring/evaluation. The joint ASCO ICON NCI, USA (ASCO = American Society of Clinical Oncology, ICON = Indian Cooperative Oncology Network, NCI = National Cancer Institute) meetings at Chicago are an example of how strategies are devised. The ICON, SFO (SAARC Federation of Oncologists), Arab Medical Association Against Cancer (AMAAC), and UAE Cancer Congress initiative with annual meetings is the logical extension to pass on the resources at the regional level. Annual Shaukat Khanum Cancer Conference (Lahore) and Muscat International Oncology Conference (Muscat) are the third logical step for dissemination at national levels (using the expertise of national and international faculty). “Promote” oncology training of family physicians (www.oncologyindia.org) and “Prerna” oncology training for oncology nurses (www.prerna.asia) are novel approach developed by ICON and rolled out jointly with SFO as a systematic approach with built-in monitoring and evaluation in an objective manner. A group of key opinion leaders get together to finalize the agenda, handouts, PowerPoint slide decks, and speaker notes. Training of trainers is then conducted among oncology colleagues who agree to follow the program guidelines and devote time to be faculty. Training programs are then carried out nationally using the same slides and the same speaker notes to convey identical messages. Participants are evaluated using pre and post session multiple-choice questionnaires (MCQs). Participants also have the opportunity to give feedback about the program as well as the faculty. Interactive sessions include video demonstrations and hands-on training using mannequins. A total of 140 Promote and 56 Prerna sessions have already been carried out with a very positive feedback (personal communication Dr. Kumar Prabhash, Managing Trustee of ICON and Secretary General of SFO).
Education is also carried out by encouraging retrospective analysis, medical audit, and publications of high quality. Recently, the Indian Journal of Medical and Pediatric Oncology brought out a special issue on chronic myeloid leukemia (CML) that included original manuscripts from 19 oncology centers across India.[13] The data represented 8,115 patients of CML in chronic phase and is the largest data on this disease from any country. A similar initiative is currently ongoing in lung cancer under the banner of Lung Cancer Consortium Asia (LCCA; www.lungcancerconsortiumasia.com). Making practical sense out of management guidelines is another educational direction. This allows personal experience of leading experts to fine tune the practical implementation of standard-of-care in a manner that optimizes resources and efficacy, while minimizing toxicity. The Oncology Gold Standard Initiative (www.oncologygoldstandard.com) provides such practical consensus recommendations online and free of charge to all healthcare professionals.
Thus, infrastructure and human resource for oncologic care in our countries is slowly improving. By providing a forum to share clinical observations, educational material, research findings, and news of conferences and meetings; we hope to continue sharing our success stories and finding unique solutions to help provide the best care possible to the 29% of the world's population that has this region as their home. All countries would choose to obtain help from India to develop or strengthen their anticancer armament. Of particular interest, as the first concrete step, was the training-of-trainers approach. Four countries would prefer that trainers from India provide this by coming to their country. Two countries would prefer to send their personnel to India for such training. And the remaining six would want to consider both options. The bottom line is that all 13 countries agreed to participate. We now need to develop a framework and find the resources to make this a reality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.PRBs world population datasheet 2011. The world at 7 Billion: A PRB Interactive Map. [Last accessed on 2014 Feb 02]. Available from: www.prb.org .
- 2.Noronha V, Tsomo U, Jamshed A, Hai M, Wattegama S, Baral R, et al. A fresh look at oncology facts on south central Asia and SAARC countries. South Asian J Cancer. 2012;1:1–4. doi: 10.4103/2278-330X.96489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore MA, Ariyaratne Y, Badar F, Bhurgri Y, Datta K, Mathew A, et al. Cancer epidemiology in South Asia-past, present and future. Asian Pac J Cancer Prev. 2010;11:49–66. [PubMed] [Google Scholar]
- 4.Bhurgri Y. Karachi Cancer Registry Data--implications for the National Cancer Control Program of Pakistan. Asian Pac J Cancer Prev. 2004;5:77–82. [PubMed] [Google Scholar]
- 5.Wabinga HR, Parkin DM, Wabwire-Mangen F, Nambooze S. Trends in cancer incidence in Kyadondo County, Uganda, 1960-1997. Br J Cancer. 2000;82:1585–92. doi: 10.1054/bjoc.1999.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al Hasnawi SM, Al Mosawi AJ, Khzaie AA, Unan OF, Fadhil HM, Sami S. Cancer in Iraq: Distribution by primary tumor site. N Iraqi J Med. 2009;5:5–8. [Google Scholar]
- 7.Nooyi SC, Al-Lawati JA. Cancer incidence in Oman, 1998-2006. Asian Pac J Cancer Prev. 2011;12:1735–8. [PubMed] [Google Scholar]
- 8.Wiredu EK, Armah HB. Cancer mortality patterns in Ghana: A 10 year review of autopsies and hospital mortality. BMC Public Health. 2006;6:159. doi: 10.1186/1471-2458-6-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parkin MD, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 10.Raina V, Tyagi B, Manoharan N. Population based cancer registry Delhi. [Last accessed on 2014 Feb 2]. Available from: http://www.icmr.nic.in/ncrp/report_pop_2001-04/05_Delhi%20Pages%20154-173.pdf .
- 11.Nandakumar A, Ramnath T, Roselind F, Shobaba B, Prabhu K. Two year report of the population based cancer registries 1999-2000. [Last accessed on 2014 Feb 2]. Available from: http://www.icmr.nic.in/ncrp/1999-00/PBCR%20Report%201999_00.pdf .
- 12.Kurkure AP, Yoele B, Koyande S. Cancer incidence and mortality in greater Mumbai. 2006. [Last accessed on 2014 Feb 2]. Available from: http://www.indiancancersociety.org/cancer-resgistry/cancer-registry/htm .
- 13.Parikh P, Bansal S. Chronic myeloid leukemia in the Imatinib era: Compilation of Indian data from 22 centers involving 8115 patients. Indian J Med Paediatr Oncol. 2013;34:145–6. doi: 10.4103/0971-5851.123699. [DOI] [PMC free article] [PubMed] [Google Scholar]


