Abstract
Background:
The present study evaluates the effectiveness of an ultrasound (US) practice course based on a sheep brain cadaver. Neurosurgical education is considerably restrained following patient safety objections and work time restrictions. It is therefore of vital importance to offer residents an opportunity to practice certain US techniques in a controlled environment without ethical or legal restrictions. We developed an US training model based on a sheep brain cadaver in order to demonstrate the feasibility of such a model, facilitate crucial anatomic knowledge, and demonstrate a learning curve from it.
Methods:
Over the course of 2 months from December 2012-January 2013, a total of 13 residents took part in a three part training session, each consisting of 20-30 min of individual US-training and performance evaluation based on a biological phantom. The first cadaver was a physiologic sheep brain. After initial familiarization with the US, the residents performed an US on a second cadaveric brain and tried to find a 0.5 cm big (in diameter) echogenic structure. In a third brain they were asked to identify a cyst (Fogarty catheter filled with water).
Results:
Thirteen neurosurgical residents participated in the study. After the first training session, the learning curve improved significantly in the second and the third session. The ability to actuate the US device, the time needed to display crucial anatomic landmarks, and to locate the two different artificial masses increased, and respectively decreased remarkably by up to 80%.
Conclusion:
After 2 months and three training sessions, the handling of the US from the residents was excellent in the operating room. The accuracy and the dexterity in use of the US improved significantly. The participants found the model to be realistic and agreed on the need for further promotion of such courses.
Keywords: Cadaver brain model, education, residency training, sheep brain, ultrasound
INTRODUCTION
According to medical surveys in Germany, up to 40% of surgical residents evaluate their training as inadequate and up to 70% as unstructured, which underlines the need for further improvement. Furthermore, 60% consider their theoretical and practical skills as “basic-poor”.[1,16]
The reasons therefore are multifaceted and have to be considered by the German Working Hours Act, changing nightshifts and resulting rest periods restrict the effective working time a priori. In neurosurgery with its consistently growing complexity the classical paradigm “see one, do one, teach one” cannot be applied, so that new concepts of teaching have to be explored. Intraoperative teaching might lead to extended surgical time and can increase intraoperative morbidity. At the same time Leach et al. pointed out correctly, that patient safety must never be sacrificed for educational purposes.[21]
Achieving skills in neurosurgical procedures commonly depends on intraoperative education. However, several techniques can be learnt outside the operating theatre to avoid extended and delayed learning curves. According to the Accreditation Council of Graduate Medical Education (ACGME) practice-based learning is also one of the six cornerstones in medical training.[21] Ingenious repeatable simulations and training models in a controlled environment can be medically sensible for neurosurgical training, the objective evaluation, and certification of skills and the refreshment thereof.
The application of varying adjuvant electronic devices during neurosurgical procedures, such as the intraoperative ultrasound (IOUS) requires extensive training and well anatomic knowledge. Since the widespread introduction of the IOUS into neurosurgery in the 1980s,[3,5] multiple studies have demonstrated its efficacy in localizing intracranial lesions and resection control among many other applications, especially since frame-based and frameless stereotactic surgery and an intraoperative magnetic resonance imaging (MRI) are not available in most developing countries.[9,12,15,17,18,19,20] Therefore biological in vivo and in vitro models, as well as artificial and virtual reality neurosurgical training tools can provide suitable assistance in various training settings, carrying their own unique advantages and disadvantages.[2,4,6,8,10,11,16,21]
Objective
Since there is a gap in education according to several medical surveys concerning achieving neurosurgical skills, the aim of our study was to develop a biological IOUS training model for neurosurgical procedures on a sheep brain and evaluate its efficacy. The presented model is the only one that resembles the echogenicity, the haptics and the size of the human brain adequately [Figures 1 and 2], while being relatively ubiquitous and easy to obtain and affordable.
Figure 1.
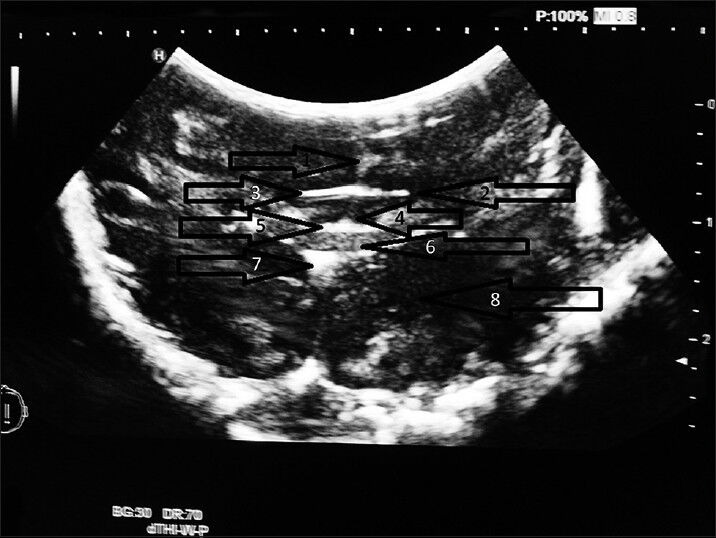
Specimen A, frontal, coronary cut 1. Corpus callosum 2. Lateral ventricle 3. Fornix 4. Third ventricle 5. Thalamic taenia and adjacent thalamic nuclei 6. Rhomboid thalamic nucleus
Figure 2.
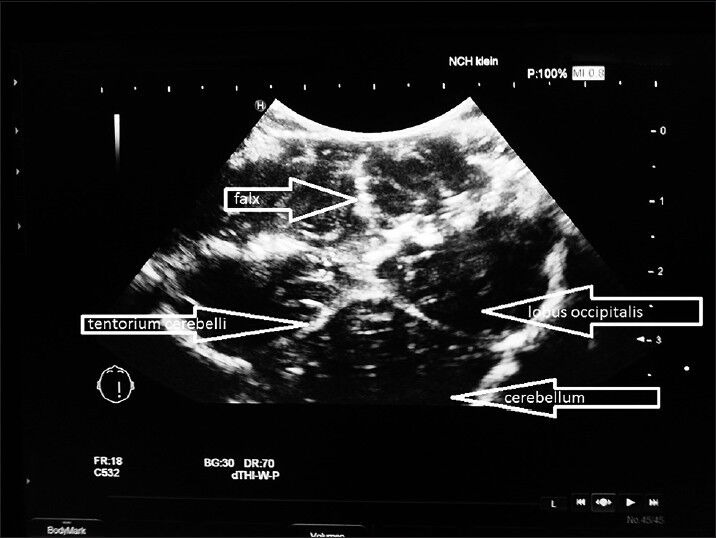
Specimen B, tentorium cerebelli, coronary cut
Research for this model was done using PubMed.com with the following keywords: Intraoperative ultrasound neurosurgery, neurosurgery training model, virtual reality neurosurgery.
Although some models concerning vascular neurosurgery, ventriculostomy, and spine-surgery have been published, the represented model is the first of its kind to allow intracranial ultrasound (US) training in neurosurgery.
We used the HI VISION Preirus (Hitachi Medical Corporation®) with a phased-array-scanner 4-8 MHz (36 23 mm), which is mostly used in neonatology, pediatrics, and intraoperatively. The study was designed to evaluate all neurosurgical residents at the Wedau Kliniken Duisburg, regardless of their year of residency (YOR) and prior knowledge.
MATERIALS AND METHODS
Specimen
For the training model, we used untreated merino sheep heads from a local farmer. We performed a craniotomy at the in-house forensic department. The specimen was placed into a sponge filled cardbox. The first specimen (specimen A) was left untouched. We implanted an artificial echogenic tumor made out of graphite and glue with a diameter of approximately 0.5 cm into the second specimen (specimen B). The third specimen was prepared with a fogarty catheter with a balloon capacity of 3 ml. The catheter was inflated with water to create an anechoic cystic mass (specimen C). The boxes were covered with drapes to avoid any biases under the participants [Figure 3].
Figure 3.
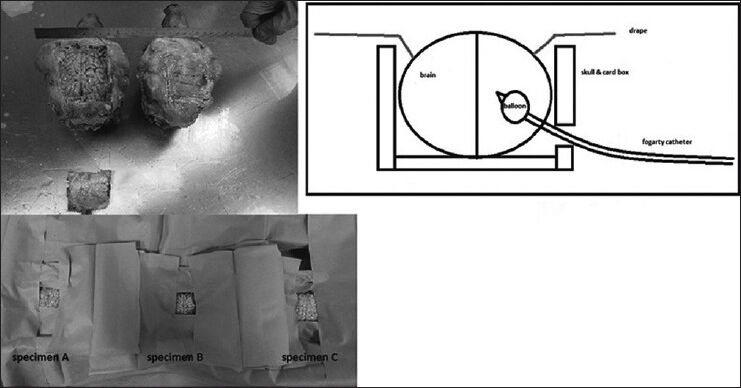
Preparations, illustration of specimen C, set-up
Studyprotocol and conduct
The study protocol was divided into a short questionnaire and an interactive part. The resident was asked to assess his own subjective US skills and grade his overall contentment with his current neurosurgical training from 1 (being the best possible) to 6. After the questionnaire, the resident had to apply the US device on specimen A following a checklist of seven needed preparations and commonly used functions (1. selecting the US-probe, 2. suppression of artefacts, 3. gel-connection, 4. frequency adjustment, 5. brightness adjustment, 6. depth adjustment, and 7. focus adjustment). For each successful and voluntarily performance, the participant was given a point, with a maximum score of 7 (part 1). The next objective was to locate and display four anatomical landmarks (1. lateral ventricles, 2. tentorium cerebelli, 3. septum pellucidum, and 4. corpus callosum) with the device within a timeframe of 20 min in specimen A. The required time in which the resident was able to depict all four structures was noted (part 2). In specimen B and C we timed the duration to locate the masses within 10 min (part 3, Figures 4 and 5). Once displayed on the monitor, the resident had to differentiate between solid or cystic and had to perform a three dimensional size measurement. Each resident was guided appropriately if the task was not executed. The test series was repeated three times over the course of 3 months. The collected data (scores and length of time) was analysed using the mean with standard deviation (SD). The individual results were correlated with the YOR with the Fisher's test. Statistical significance was estimated with a P value of <0.05.
Figure 4.
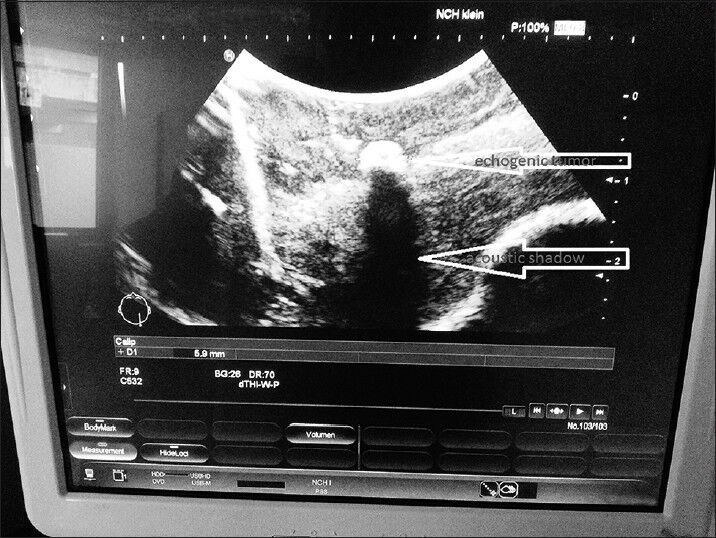
Specimen B, solid tumor
Figure 5.
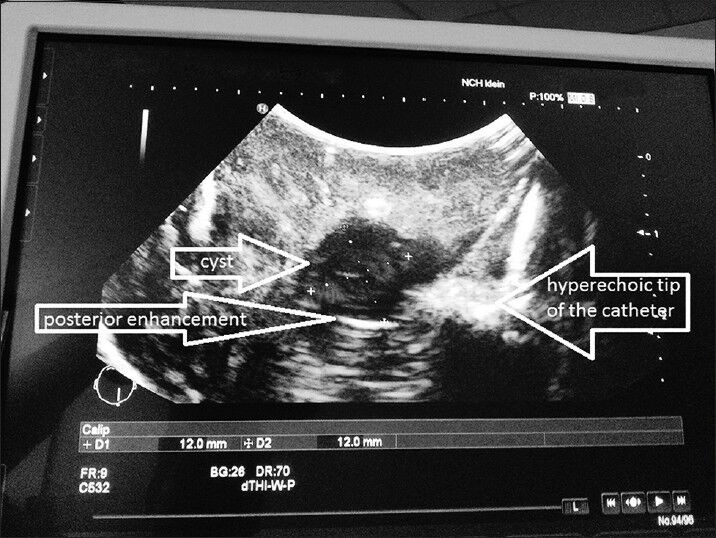
Specimen C, cystic tumor
RESULTS
In total, 13 residents took part in this study. Nine of them passed the test series a second time, and eight a final third time. The learning curves for the parts 1-3 were remarkable and showed the success of the model. All mean performance scores and required times improved significantly (percentages represent successful and therefore evaluated residents): “Handling” from 1-5 (21.4%) to 6 (85.7%) (part 1), “anatomical structures” from 348 s in 53.8% to 114 s in 75% (part 2) and “tumors” from 478 s in 15.4% to 60.8 s in 100% in B and from 82 s in 100% to 48 s in 100% in C (part 3).
The initial mean handling score of the US device in part 1 was 1.5 points with a SD of 1.7 (21.4% of tasks). This increased to a mean of 4 (SD 1.9) in the second trail and an excellent mean of 6 (SD 0.9) in the last session (85.7%) [Figure 6].
Figure 6.
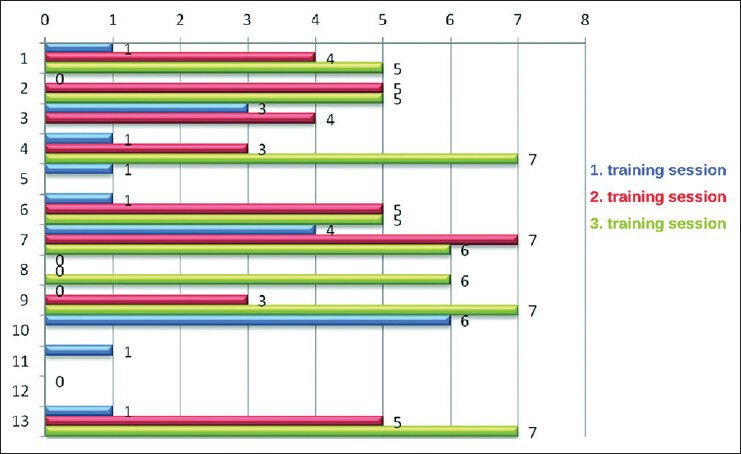
Scores for handling of the ultrasound device in specimen A over the three training sessions (1st: Blue, 2nd: Red, 3rd: Green)
These results correlated significantly and positively with the YOR in the first session (r 0.29, P < 0.05), but after the third session it had changed to a negative correlation (r -0.5; P = 0.05).
The mean time needed to display the anatomical landmarks in specimen A was 348 s (SD: 144 s; P < 0.5). Of the nine participants, six (66%) were able to show the anatomical landmarks in the second session with an already remarkably decreased mean time of 154 s (SD 73.9). These results showed no correlation to the YOR, as well (P < 0.5). Of the eight, six (75%) depicted the four anatomical structures in the third session with a mean time of 114 s (SD 56.9) [Figure 7]-Interestingly, there was a significant positive correlation with the YOR (r 0.3; P < 0.5). The overall mean time reduction after three sessions was 67%.
Figure 7.
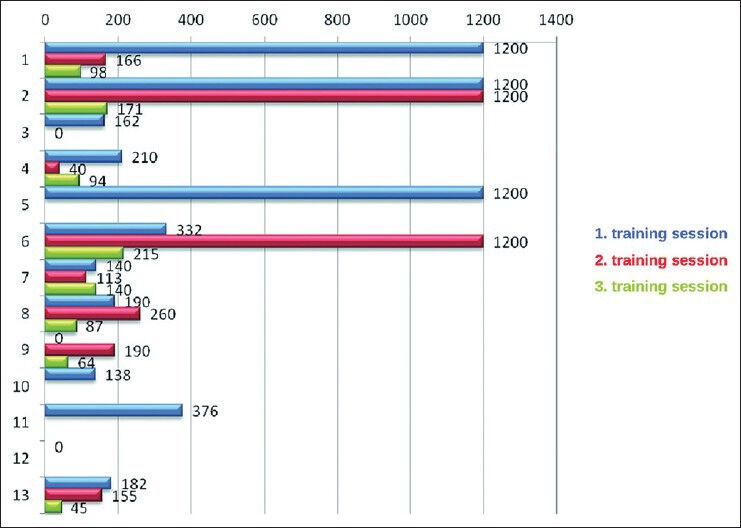
Time (in sec) needed to display the four anatomic structures in specimen A over the three training sessions (1st: Blue, 2nd: Red, 3rd: Green)
In the first session in specimen B, only 2/13 participants (15.4%) were able to detect the “tumor” within 10 min. The mean time was 478 s (SD 144.2). None of them was able to measure the pathology.
Since these two residents were both in their last 6th year of training, a correlation to the YOR was not possible. The apparent deficits in US skills prolonged the first training session considerably. Specimen C (cystic) therefore was not examined.
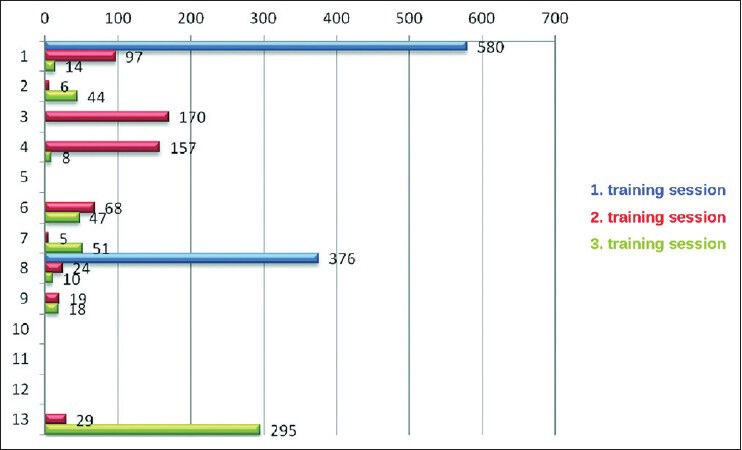
In the second session, all residents detected the mass in both specimens B and C within the time limit. The mean time in specimen B was 63.8 s (SD 63.9) with a significant positive correlation to the YOR (r 0.6; P < 0.5) and in specimen C 82.3 s (SD 86) with a marginal negative but significant correlation (r -0.1; P < 0.5). Of the nine, five participants (55%) were able to measure the masses in all three dimensions.
In the last session, all participants detected the masses again, whereby we noticed a further improvement of the mean required time to 60.8 s (SD 96. The SD was high because one outlier needed 295 s) in specimen B, [Figure 8] and to 48 s (SD 21.3) in specimen C [Figure 9].
Figure 8.
Time (in sec) needed to locate the solid tumor in specimen B over the three training sessions (1st: Blue, 2nd: Red, 3rd:Green)
Figure 9.
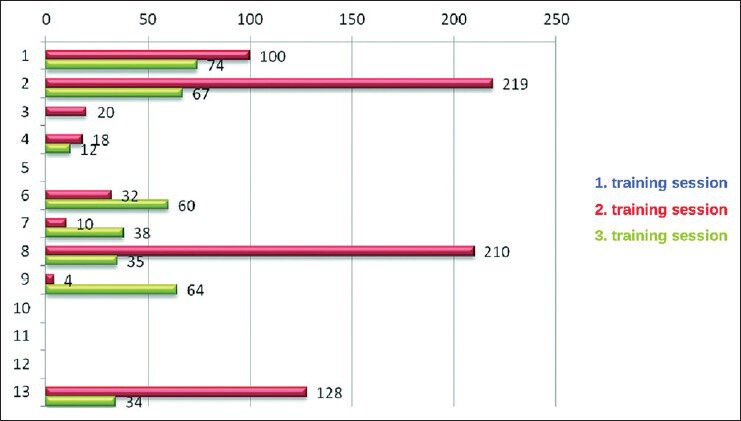
Time (in sec) needed to locate the cystic tumor in specimen C over the three training sessions (1st: Blue, 2nd: Red, 3rd: Green)
The detection rate showed no significant correlation with the YOR in specimen B (r -0.5; P 0.07), while there was a significant slight correlation in specimen C (r 0.1; P < 0.05).
All participants (8/8) categorized the masses correctly into solid and cystic and were able to perform a three dimensional measurement. YOR showed no constant reliable correlation with the performances.
CONCLUSION
To the best of the author's knowledge, this is the first US training model based on a brain cadaver. Other models for neurosurgical training like the various virtual reality models,[1] the artificial model by Mori,[13] and the human cadaver model by Olabe[14] are available but not useful for US training. Artificial models lack the similarity in echogenicity and haptic, whereas human cadaver models are simply too costly and not ubiquitous available.
The financial costs are minimal with 5 €/head and require little effort to obtain and store once a suitable slaughterhouse has been found. No ethical requests have to be filed and the set-up is almost anywhere possible with enough room for a table and the US device. Odor nuisance was not an issue as long as the specimen were kept fresh and stored in the freezer, however, the texture of the cortex changed in the freezer and became tarnished. Accordingly, the specimen froze and became rigid, so we recommend storing temperatures between 4°C and 6°C.
Our developed IOUS model appeared as a very reliable training tool, which fulfilled the demanded criteria to simulate an intraoperative setting.
Although we present a rather small cohort, the very fact, that due to night shifts, operations, and emergencies, the number of participants was variable underlines the necessity for an easy accessible in-house training model.
The results are promising and support the notion that US training on a cadaveric sheep brain is feasible and leads to considerable improvements in handling the device, anatomic orientation, and tumor detection referring to the Kalayci et al. study, which showed the benefit of a preoperative phantom-based “training model for lumbal discectomy”.[7]
The training course was generally well received by the participants and the specimens were found to have good resemblance with the human brain. Subsequently other applications are conceivable like the US guided puncturing of an embedded cyst.
In summary it can be stated that our developed IOUS training model is an easy and effective training tool, which enables well education to acquire expertise in handling the US device. After 2 months and three training sessions, the handling of the US improved significantly and represents an important basis for the use during neurosurgical procedures. The accuracy and the dexterity in use of the US improved significantly. The participants found the model to be realistic and agreed on the need for further extend of such models in specific courses.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/1/46/130314
Contributor Information
Jan Vavruska, Email: janvavruska@gmx.de.
Ralf Buhl, Email: buhl@klinikumsolingen.de.
Athanasios K. Petridis, Email: opticdisc@aol.com.
Homajoun Maslehaty, Email: h.maslehaty@gmx.de.
Martin Scholz, Email: Martin.Scholz kdu@Sana.de.
REFERENCES
- 1.Alaraj A, Lemole MG, Finkle JH, Yudkowsky R, Wallace A, Luciano C, et al. Virtual reality training in neurosurgery: Review of current status and future applications. Surg Neurol Int. 2011;2:52. doi: 10.4103/2152-7806.80117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boszczyk BM, Mooij JJ, Schmitt N, Di Rocco C, Fakouri BB, Lindsay KW. Spine surgery training and competence of European neurosurgical trainees. Acta Neurochir (Wien) 2009;151:619–28. doi: 10.1007/s00701-009-0259-8. [DOI] [PubMed] [Google Scholar]
- 3.Dohrmann GJ, Rubin JM. History of intraoperative ultrasound in neurosurgery. Neurosurg Clin N Am. 2000;12:155–66. [PubMed] [Google Scholar]
- 4.Filho FV, Coelho G, Cavalheiro S, Lyra M, Zymberg ST. Quality assessment of a new surgical simulator for neuroendoscopic training. Neurosurg Focus. 2011;30:E17. doi: 10.3171/2011.2.FOCUS10321. [DOI] [PubMed] [Google Scholar]
- 5.Frentzel-Beyme B. Als die Bilder laufen lernten. Hamburger Ärzteblatt. 2005;59:446. [Google Scholar]
- 6.Jerison HJ. USA: Academic Press; 1973. Evolution of the Brain and Intelligence. [Google Scholar]
- 7.Kalayci M, Cagavi F, Gul S, Cagavi Z, Acikgoz B. A training model for lumbar discectomy. J Clin Neurosci. 2005;12:673–5. doi: 10.1016/j.jocn.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Kockro RA, Stadie A, Schwandt E, Reisch R, Charalampaki C, Ng I. A collaborative virtual reality environment for neurosurgical planning and training. Neurosurgery. 2007;61(5 Suppl 2):379–91. doi: 10.1227/01.neu.0000303997.12645.26. [DOI] [PubMed] [Google Scholar]
- 9.Kumar P, Sukthankar R, Damany BJ, Mishra J, Jha AN. Evaluation of intraoperative ultrasound in neurosurgery. Ann Acad Med Singapore. 1993;22(3 Suppl):422–7. [PubMed] [Google Scholar]
- 10.Larsen OV, Haase J, Ostergaard LR, Hansen KV, Nielsen H. The Virtual Brain Project--development of a neurosurgical simulator. Stud Health Technol Inform. 2001;81:256–62. [PubMed] [Google Scholar]
- 11.Lemole GM, Jr, Banerjee PP, Luciano C, Neckrysh S, Charbel FT. Virtual reality in neurosurgical education: Part-task ventriculostomy simulation with dynamic visual and haptic feedback. Neurosurgery. 2007;61:142–8. doi: 10.1227/01.neu.0000279734.22931.21. [DOI] [PubMed] [Google Scholar]
- 12.McGahan JP, Ellis WG, Budenz RW, Walter JP, Boggan J. Brain gliomas: Sonographic characterization. Radiology. 1986;159:485–92. doi: 10.1148/radiology.159.2.3515424. [DOI] [PubMed] [Google Scholar]
- 13.Mori K, Yamamoto T, Oyama K, Nakao Y. Modification of three-dimensional prototype temporal bone model for training in skull-base surgery. Neurosurg Rev. 2009;32:233–8. doi: 10.1007/s10143-008-0177-x. [DOI] [PubMed] [Google Scholar]
- 14.Olabe J, Olabe J, Sancho V. Human cadaver brain infusion model for neurosurgical training. Surg Neurol. 2009;72:700–2. doi: 10.1016/j.surneu.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 15.Ray WZ, Barua M, Ryken TC. Anatomic visualization with ultrasound-assisted intracranial image guidance in neurosurgery: A report of 30 patient. J Am Coll Surg. 2004;199:338–43. doi: 10.1016/j.jamcollsurg.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Regelsberger J, Heese O, Horn P, Kirsch M, Eicker S, Sabel M, et al. Training microneurosurgery-four years experiences with an in vivo model. Cent Eur Neurosurg. 2011;72:192–5. doi: 10.1055/s-0030-1261906. [DOI] [PubMed] [Google Scholar]
- 17.Reinacher PC, van Velthoven V. Intraoperative ultrasound imaging: Practical applicability as a real-time navigation system. Acta Neurochir Suppl. 2003;85:89–93. doi: 10.1007/978-3-7091-6043-5_12. [DOI] [PubMed] [Google Scholar]
- 18.Renner C, Lindner D, Schneider JP, Meixensberger J. Evaluation of intra-operative ultrasound imaging in brain tumor resection: A prospective study. Neurol Res. 2005;27:351–7. doi: 10.1179/016164105X40039. [DOI] [PubMed] [Google Scholar]
- 19.Sosna J, Barth MM, Kruskal JB, Kane RA. Intraoperative sonography for neurosurgery. J Ultrasound Med. 2005;24:1671–82. doi: 10.7863/jum.2005.24.12.1671. [DOI] [PubMed] [Google Scholar]
- 20.Unsgaard G, Gronningsaeter A, Ommedal S, Nagelhus Hernes TA. Brain operations guided by real-time two-dimensional ultrasound: New possibilities as a result of improved image quality. Neurosurgery. 2002;51:4022. [PubMed] [Google Scholar]
- 21.Walker JB, Perkins E, Harkey HL. A novel simulation model for minimally invasive spine surgery. Neurosurgery. 2009;65(6 Suppl):188–95. doi: 10.1227/01.NEU.0000341534.82210.1B. [DOI] [PubMed] [Google Scholar]


