Abstract
Background:
Closure of the dura defect may be easy to perform in open lumbar surgery but could be difficult in minimally invasive transforaminal lumbar interbody fusions (MIS-TLIF) since MIS-TLIF was done through a small tube, which limited the use of standard dural repair instruments. We used nonpenetrating titanium clips that were originally designed for the vascular anastomoses to repair the dura defect, which is never described in the literature.
Methods:
We presented a case of spinal stenosis with incidental durotomy while performing MIS-TLIF. We closed the dura laceration with three medium-sized nonpenetrating titanium clips (AnastoClip Vessel Closure System, LeMaitre Vascular, Inc., Burlington, MA).
Results:
Nonpenetrating titanium clips have the benefits of being technically easy to use, reduced durotomy repair time, decreased bed rest due to related medical complications, superior postoperation with immediate hydrostatic strength, and better reapproximation if it fails to clip successfully. As for the postoperation follow up, clips are tiny and reveal no obvious artifact, especially in cases where the pedicle screws are already causing much artifact.
Conclusion:
Primary dural closure during MIS-TLIF with clips is an effective way in cases that involve limited tubular space.
Keywords: Durotomy, minimally invasive lumbar fusion, nonpenetrating titanium clips
INTRODUCTION
The incidence of durotomy in lumbar surgery varies from 1% to 17% and generally results in poor long-term clinical outcomes.[6] The neurologic sequelae of durotomy ranged from asymptomatic to pseudomeningocele, cerebrospinal fluid (CSF) fistula, and nerve root injury. Primary closure of the dura defect was considered the gold standard of durotomy management to prevent the neurologic sequelae. Closure of the dura defect may be easy to perform in open lumbar surgery but could be difficult in minimally invasive transforaminal lumbar interbody fusions (MIS-TLIF), which are now commonly performed procedures for the patients with spinal stenosis. Since MIS-TLIF was done through a small tube, which limited the use of standard dural repair instruments, we try to find a safe and quick method to solve the problems. In previous literature review, there are several techniques noted addressing methods of dura repair in a limited space.[2,4] In our case report, we used nonpenetrating titanium clips that were originally designed for the vascular anastomoses to repair the dura defect while performing MIS-TLIF. This is the first report that describes this procedure in the literature where nonpenetrating titanium clips are used for dural closure in a patient with iatrogenic spinal durotomy and CSF leakage in performing MIS-TLIF.
MATERIALS AND METHODS
A 67-year-old female, with worsening neurogenic claudication in 6 months, underwent MIS-TLIF for L3-4 and L4-5 spinal stenosis. We use Medtronic Quandrant retractor system for unilateral approach bilateral decompression of the narrow lumbar spinal canal, and Medtronic Sextant system for pedicle screws fixation. Incidental durotomy was noted when removing posterior lateral part of yellow ligament over L3-4 level. The durotomy length was about 0.5 cm. We used a small patty to press the bulging nerve root coming from the dura defect and put the edge of the dura defect together by using an atraumatic everting forceps. This allows for the dural edges to come together. After identifying that there was no nerve root present between the clip tips, we close the dura laceration with three medium-sized nonpenetrating titanium clips (AnastoClip Vessel Closure System, LeMaitre Vascular, Inc., Burlington, MA) with 2-mm gaps [Figure 1]. No additional tissue glues were used. Valsalva maneuvers were used to confirm the complete dura closure. The wound was then closed in a layered fashion without a subfacial drain.
Figure 1.
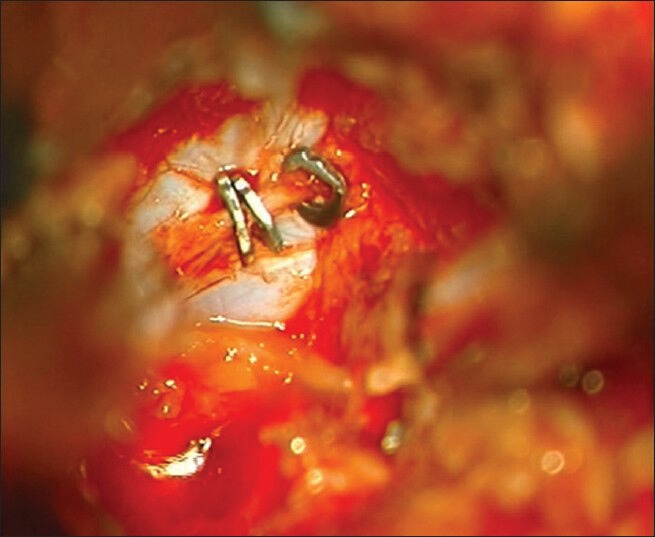
Incidental durotomy was repaired with nonpenetrating clips utilizing the quadrant retractor system
RESULTS
Postoperatively, the patient's wound remained dry and no spinal headache was noted and also there was discharge 3 days later. Immediate postoperation X-ray revealed tiny clips without obvious artifact [Figure 2]. Follow up magnetic resonance imaging (MRI) at postoperation 3 months revealed no epidural effusion [Figure 3].
Figure 2.
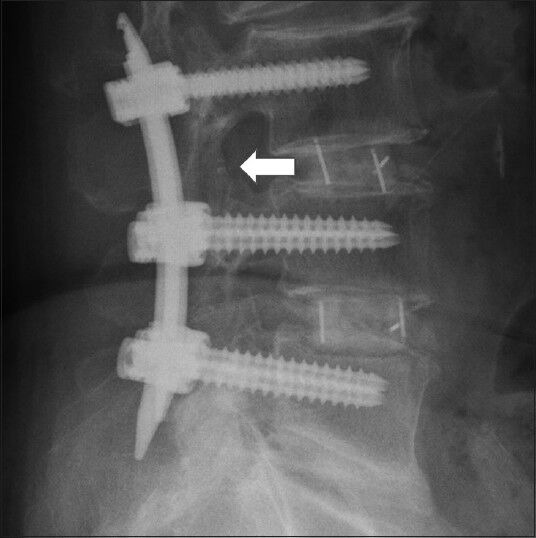
After MIS-TLIF and percutaneous pedicle screw fixation was performed, immediate postoperation lumbar X-ray revealed tiny clips (note the white points) without obvious artifact
Figure 3.
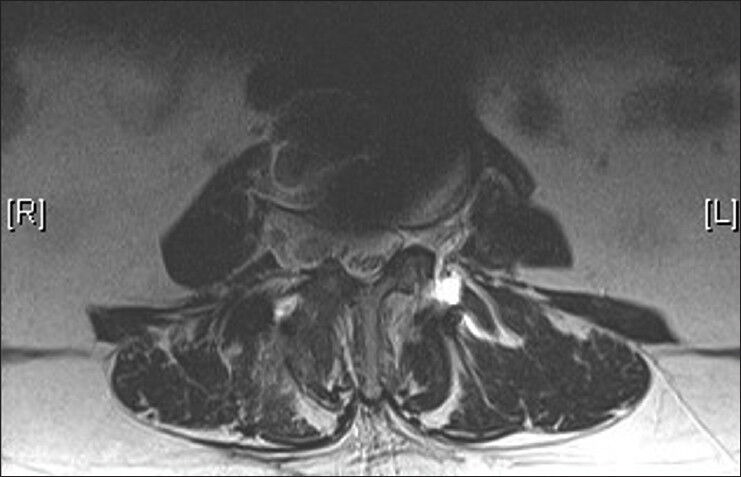
T2-weighted MRI 3 months postoperation revealed no CSF collection around the clip site
DISCUSSION
We all do not want durotomies to happen, but it does. If it is noted during postoperation follow-up, bed rest, epidural blood patch, or lumbar drain may help. If it is noted intraoperatively, primary bring the edges of dura for closure is the preferred method of preventing complications of durotomies. Previous reports support the early management of durotomy for fear of postoperative medical problems such as deep vein thrombosis, infection, and physical decompensation, which is related to prolonged bed rest as the patient is waiting for the durotomy to heal. These risks are resolved with early ambulation, which means that the successful repair of the durotomy is important.
As for durotomies repair, the location of the durotomies may limit the ease of repair. When the durotomy is located along the bone edge, it is hard to close it without extra bone removal. In MIS-TLIF, long tubular quadrant retractor system also limited the conventional instruments manipulation. Alexandra et al.[1] described the application of aneurysm clip to treat such problem but clips slip off problem and the influence of decreased spinal canal cross section by such clips need to be confirmed. By using the nonpenetrating titanium clips, durotomies repair can be done if dura edge could be pulled together by forceps. Since forceps are a long instrument, it is not difficult to pull together the dura edge in a long tubular retractor system. The quality of durotomies is also influenced by the difficulty of repair. If the dura is friable and multiple small tears present, suturing worsens the durotomy, in which clips applied can also easily handle the problem. When compared with penetrating clips such as self-closing nitinol clips,[4] nonpenetrating clips have a number of advantages such as their ease of removal and that they do not cause an additional hole on the dura.
The nonpenetrating titanium clip used in our case is designed from the Anastoclip Vessel Closure System (AnastoClip Vessel Closure System, LeMaitre Vascular, Inc., Burlington, MA), which was originally used for vascular anastomoses. Nowadays, these clips have several new extensive applications in other fields such as neurosurgery, pediatric surgery, and urology.[7] Kaufman et al.[5] reported a retrospective study of their practice of using nonpenetrating titanium clips for dural closure in 27 pediatric cases with diversity in diagnoses regarding spinal surgery. None of the patients experienced CSF leakage and the follow up image study revealed no obvious artifact. Faulkner et al.[3] reported that the dura closure with nonpenetrating titanium clips provides immediate hydrostatic strength similar to intact dura. In conclusion of the previous studies revealed that nonpenetrating titanium clips have the benefits of being technically easy to use, reduced durotomy repair time, decreased bed rest due to related medical complications, superior postoperation with immediate hydrostatic strength, and better reapproximation if it fails to clip successfully. As for the postoperation follow up, clips are tiny and reveal no obvious artifact, especially in cases where the pedicle screws are already causing much artifact. Since MIS-TLIF is gaining in popularity in modern spine surgery to reduce muscle injury while performing such operations, nonpenetrating clips have become a good solution to resolve the durotomies of a limited work space. Although a single case report may not be sufficient to make a conclusion of its advantages and good outcomes. The idea of durotomies repair in the MIS-TLIF may provide us an alternative method of solving the trouble we have met. However, further series studies are needed to confirm the efficiency of this method.
CONCLUSION
In our experience, primary dural closure utilizing standard techniques during MIS-TLIF can be difficult. With the support of clips, we can create an effective dural closure in a MIS-TLIF operation, especially in cases that involve limited tubular space.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/1/36/129161
Contributor Information
Yen-Po Cheng, Email: 134309@cch.org.tw.
Ping-Yi Lin, Email: 69221@cch.org.tw.
Abel Po-Hao Huang, Email: how.how0622@gmail.com.
Chun-Yuan Cheng, Email: 83998@cch.org.tw.
Chien-Min Chen, Email: 96015@cch.org.tw.
Dueng-Yuan Hueng, Email: hondy2195@yahoo.com.tw.
REFERENCES
- 1.Beier AD, Barrett RJ, Soo TM. Aneurysm clips for durotomy repair: Technical note. Neurosurgery. 2010;66(3 Suppl Operative):E124–5. doi: 10.1227/01.NEU.0000365423.19998.3D. [DOI] [PubMed] [Google Scholar]
- 2.Chou D, Wang VY, Khan AS. Primary dural repair during minimally invasive microdiscectomy using standard operating room instruments. Neurosurgery. 2009;64:356–9. doi: 10.1227/01.NEU.0000338942.11337.DA. [DOI] [PubMed] [Google Scholar]
- 3.Faulkner ND, Finn MA, Anderson PA. Hydrostatic comparison of nonpenetrating titanium clips versus conventional suture for repair of spinal durotomies. Spine (Phila Pa 1976) 2012;37:E535–9. doi: 10.1097/BRS.0b013e31824cf756. [DOI] [PubMed] [Google Scholar]
- 4.Ferroli P, Franzini A, Messina G, Tringali G, Broggi G. Use of self-closing U-clips for dural repair in mini-invasive surgery for herniated disc. Acta Neurochir (Wien) 2008;150:1103–5. doi: 10.1007/s00701-008-0018-2. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman BA, Matthews AE, Zwienenberg-Lee M, Lew SM. Spinal dural closure with nonpenetrating titanium clips in pediatric neurosurgery. J Neurosurg Pediatr. 2010;6:359–63. doi: 10.3171/2010.7.PEDS09545. [DOI] [PubMed] [Google Scholar]
- 6.Saxler G, Kramer J, Barden B, Kurt A, Pfortner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976) 2005;30:2298–302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 7.Zeebregts CJ, Kirsch WM, Reijnen MM, Zhu YH, van den Dungen JJ. Expanding use of nonpenetrating clips in various surgical specialities. Surg Technol Int. 2005;14:85–95. [PubMed] [Google Scholar]


