Abstract
BACKGROUND
Increased attention has been given to pulse pressure (PP) as a potential independent risk factor for cardiovascular disease (CVD). We examined the relationship between the three indices of blood pressure consisting of systolic blood pressure (SBP), diastolic blood pressure (DBP), and PP (= SBP – DBP), respectively, and incident acute coronary heart disease (CHD).
METHODS
Participants in the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study, a national cohort study of 30,239 black and white participants > 45 years of age, were enrolled between 2003 and 2007. The participants’ SBP, DBP, and PP values were separated into the four groups of < 45mm Hg, 45–54.9mm Hg, 55–64.9mm Hg, and ≥ 65mm Hg, and were analyzed on a groupwise basis. Reported CHD events were confirmed by expert adjudication. Cox proportional hazards models were used to examine the association of incident CHD (first acute CHD event) for the four groups of BP measurements with multivariate-adjusted sociodemographic and clinical risk factors.
RESULTS
Analyses were done for 22,909 men and women (40.4% black, 44.6% male) ≥ 45 years of age (mean age = 64.7±9.4 years) without prevalent CHD at baseline. Associations were found for 681 CHD events, over a mean 3.4 years of follow-up (maximum 6 years), with each unadjusted PP group (hazard ratio [HR] with 95% confidence limits for PP of 45–54.9mm Hg, 55–64.9mm Hg, and ≥ 65mm Hg, respectively, of 3.82, 3.08, and 4.73 as compared with PP < 45mm Hg; P < 0.0001 for linear trend), and this persisted after full adjustment, including that for SBP (1.50, 1.08, 2.09; P trend < 0.01). Subgroup analyses showed no statistically significant differences across age, race, or region of the country, but did suggest the possibility that men were more sensitive to PP than were women.
CONCLUSIONS
Pulse pressure is positively and independently (particularly so with regard to independence from SBP) associated with incident CHD, and there were no significant racial or regional differences in this association.
Keywords: blood pressure, CVD death, fatal and non-fatal myocardial infarction (MI), hypertension, incident CHD, pulse pressure.
Current definitions of hypertension (HTN) are primarily based on systolic blood pressure (SBP) and diastolic blood pressure (DBP) but not on pulse pressure (PP). More recently, increased attention has been given to PP as a predictor of cardiovascular risk. Pulse pressure is an indicator of the stiffness of large arteries, especially the aorta.1–4 Both SBP and DBP increase with age in a parallel manner until the age of approximately 60 years, after which SBP continues to rise and DBP begins to decrease. This age-related phenomenon results in the large increase in PP after age 60 years, and in an increase in the prevalence of isolated systolic hypertension (ISH).5 As a result, PP may be a key blood-pressure–related variable in older individuals and may be important as a risk factor for cardiovascular disease (CVD), including stroke, myocardial infarction (MI), and death.3 Some evidence suggests that PP may be an independent predictor of CHD-related events even independently of SBP. We have already reported the association of PP with incident stroke and found that although PP was positively associated with stroke, this association was attenuated after multivariate adjustment, which included adjustment for SBP, DBP, and MAP.6
Although a possible relationship between PP and the occurrence of acute CHD-related events (definite and probable MI, as well as death from CHD) has been studied, most such studies have included predominantly white populations.2,5 Few data on this subject are available for African–Americans (AA), and it is unclear whether an association exists between PP and the incidence of acute CHD in the AA population. Differences have also been reported in the association of PP with CHD in women as compared with men.1
The primary purpose of the REasons for Geographic And Racial Differences in Stroke (REGARDS) study was to further investigate whether PP is a useful predictor of the risk of acute CHD-related events. We also postulate that differences in PP, independently of SBP, may represent a factor contributing to the racial differences in risk of acute CHD-related events. In view of this, we felt that the REGARDS study would provide valuable information about whether racial differences exist relative to PP, and their effect on incident acute CHD. We also wanted to explore whether AAs have a greater CHD risk at the same PP than do whites (i.e., a differential susceptibility as compared with that of whites), and whether there are regional differences in that association.
METHODS
Study population
The REGARDS study is a national, population-based, biracial, longitudinal cohort study designed to examine underlying causes for racial and regional differences in stroke and CHD. The study enrolled only AAs and white persons, and oversampled AAs and persons living in the Stroke Belt region of the United States, an area that has stroke mortality rates higher than those in the rest of the country. Between January 2003 and October 2007, 30,239 individuals were enrolled in the REGARDS study, 42% of whom were AAs and 58% white persons, and 45% of whom were men and 55% women. Of the study participants, 21% were from the Stroke Belt Buckle (the coastal-plain region of North Carolina, South Carolina, and Georgia), 35% from the Stroke Belt states (remainder of North Carolina, South Carolina, and Georgia, plus Alabama, Mississippi, Tennessee, Arkansas, and Louisiana), and the remaining 44% from the other 40 contiguous states (referred to as non-Belt states) of the United States. Participants in the REGARDS study were selected from commercially available lists (Genesys, Grand Blanc, Michigan). A letter and brochure informed participants of the study, and was followed by a telephone call to inform them of its approach. During that call, verbal consent was obtained and a 45-minute questionnaire was administered. The telephone response rate, including an estimate of eligibility among participants who were not reached, was 33%; the cooperation rate among those with confirmed eligibility was 49% (which was similar to that in the Multi-Ethnic Study of Atherosclerosis, which had a 39.8% participation rate among persons contacted and to whom the study was explained).
Participants were considered to be enrolled in the study if they completed the telephone questionnaire and the in-person physical examination at the study baseline. Demographic information and a medical history of each participant were obtained by trained interviewers through a computer-assisted telephone interview (CATI). Consent for participation was obtained verbally by telephone and subsequently in writing during a follow-up visit in the participant’s home. A brief physical examination, including anthropometric and blood pressure measurements, blood samples, and an electrocardiogram (EKG), was conducted in person at 3–4 weeks after the telephone interview. Participants were followed by telephone at 6-month intervals for surveillance of medical events. Reports of a potential CHD-related event prompted the retrieval of medical information for the relevant study participant, and reports of death triggered interviews with the next-of-kin or other proxies, in addition to the retrieval of any hospital records that corresponded to a hospitalization near the time of the participant’s death. The National Death Index was also queried for the cause of participants’ deaths. Study methods were reviewed and approved by all involved institutional review boards. Additional details of the study methodology are provided elsewhere.7
Main outcomes
The primary dependent variables in the study were acute CHD (incident fatal and non-fatal MI); acute CHD plus CVD death; CVD; and fatal and non-fatal MI separately. Definitions of the outcomes were based on international consensus.8 Myocardial infarction was classified and grouped as definite or probable if a biomarker for MI (almost always troponin) exhibited a rising or falling pattern with its peak concentration being twice the lowest established upper limit of normal, in addition to the presence of at least one of the following: symptoms or signs suggestive of ischemia or changes in the EKG that were consistent with acute ischemia. If the EKG showed diagnostic changes and ischemic signs or symptoms were present but the values for biomarkers were either unavailable or equivocal, an event was classified as a probable MI. Death from acute CHD was defined as definite fatal MI if death occurred within 28 days of hospital admission in cases of definite MI, or was defined on the basis of postmortem findings consistent with MI within 28 days of death. The designation of probable CVD-related death was applied to out-of-hospital cases of sudden cardiac death or to deaths suggestive of CHD in which the study subject had a history of CHD and no other plausible cause of death, or to fatal stroke or fatal congestive heart failure. Outcomes that were analyzed included incident acute CHD, which included both fatal and nonfatal events; and, fatal or nonfatal incident CHD, which was analyzed separately. For the purpose of the study, incident events were defined as those occurring among participants without CHD at baseline (with CHD defined as a self-reported history of MI, coronary artery bypass surgery, percutaneous coronary intervention, or electrocardiographic evidence of MI).
Main exposure
The primary independent variable in the study was PP, which was divided into 10-mm Hg increments (< 45mm Hg, 45–54.9mm Hg, 55–64.9mm Hg, and ≥ 65mm Hg).1 Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were defined as the average of two measurements of SBP or DBP taken by a trained technician using a standard protocol and a regularly tested aneroid sphygmomanometer, and measured in the fasting state (except that there was no prohibition of coffee) after the participant was seated for 5 minutes. The protocol used in the REGARDS study was that set forth in the Seventh Report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure (JNC 7) of “At least two measurements should be made and the average recorded.”1 Quality control of blood pressure recording was monitored by central examination of digit preference and retraining of technicians as necessary.
Demographic factors recorded in the study included age (defined in 10-year strata beginning at age 45 years), race, and gender.
Other covariates
Measures of socioeconomic status used in the study included annual household income and education (defined in strata, see Table 1). Cardiovascular risk factors included self-reported perceived health (on a 5-point scale ranging from Poor to Excellent), hypertension (SBP ≥ 140mm Hg or DBP ≥ 90mm Hg, or self-reported use of antihypertensive medications),9 diabetes (fasting glucose ≥ 126mg/dl or non-fasting glucose ≥ 200mg/dl or self-reported use of diabetes medications10), dyslipidemia (total cholesterol ≥ 240mg/dl, low-density lipoprotein cholesterol ≥160mg/dl, high density lipoprotein cholesterol < 40mg/dL, or self-reported use of lipid-lowering medications), smoking status (never, past, or current), and alcohol use (never, past, or current). Systolic blood pressure was also included, as a separate variable.
Table 1.
Baseline characteristics of participants in the REasons for Geographic And Racial Differences in Stroke study by levels of pulse pressure
| Overall (n = 22,909) | Pulse pressure (mm Hg) | ||||
|---|---|---|---|---|---|
| < 45 (n = 8,099) | 45–54.9 (n = 7,539) | 55–64.9 (n = 4,421) | ≥ 65.0 (n = 2,850) | ||
| Age, years (mean ± SD) | 64.1±9.30 | 61.2±8.89 | 63.7±8.86 | 66.5±8.93 | 69.5±8.84 |
| BMI, kg/m2 (mean ± SD) | 29.3±6.20 | 28.6±6.07 | 29.5±6.09 | 29.8±6.33 | 29.7±6.45 |
| SBP, mmHg (mean ± SD) | 127.0±16.4 | 114.2±10.3 | 126.3±9.4 | 135.9±10.5 | 151.6±16.4 |
| Black (%) | 41.7 | 37.0 | 41.7 | 45.2 | 49.7 |
| Female (%) | 58.3 | 61.0 | 57.0 | 57.1 | 55.6 |
| Region (%) | |||||
| Belt | 34.8 | 33.2 | 35.6 | 35.6 | 36.5 |
| Buckle | 21.0 | 22.8 | 20.9 | 18.8 | 19.4 |
| Non-belt | 44.2 | 44.0 | 43.5 | 45.6 | 44.1 |
| Income (%) | |||||
| Less than $20K | 16.9 | 13.9 | 15.4 | 20.2 | 24.2 |
| $20K-$34K | 23.6 | 20.8 | 23.3 | 26.3 | 28.5 |
| $35K-$74K | 30.4 | 31.7 | 32.0 | 28.0 | 25.8 |
| $75K + | 17.0 | 22.3 | 17.5 | 12.0 | 8.2 |
| Refused | 12.1 | 11.3 | 11.8 | 13.5 | 13.3 |
| Education (%) | |||||
| Less than high school | 11.4 | 8.1 | 10.6 | 13.9 | 18.3 |
| High-school graduate | 25.3 | 23.2 | 25.0 | 27.9 | 28.1 |
| Some college | 27.0 | 26.6 | 27.4 | 27.7 | 26.1 |
| College graduate and above | 36.4 | 42.1 | 37.0 | 30.4 | 27.5 |
| General Health Status (%) | |||||
| Poor | 2.6 | 2.1 | 2.4 | 2.9 | 3.9 |
| Fair | 13.1 | 11.0 | 12.4 | 15.3 | 17.4 |
| Good | 34.3 | 31.7 | 34.4 | 36.8 | 37.5 |
| Very good | 32.3 | 34.5 | 32.7 | 30.7 | 27.9 |
| Excellent | 17.7 | 20.7 | 18.1 | 14.3 | 13.3 |
| Smoke (%) | |||||
| Never | 47.6 | 50.1 | 47.5 | 45.2 | 44.5 |
| Past | 38.4 | 35.8 | 39.0 | 40.2 | 41.4 |
| Current | 14.0 | 14.1 | 13.5 | 14.6 | 14.0 |
| Alcohol consumptiona (%) | |||||
| None | 62.0 | 58.3 | 62.2 | 65.5 | 66.6 |
| Moderate | 33.8 | 37.8 | 33.5 | 29.7 | 29.4 |
| Heavy | 4.2 | 3.9 | 4.3 | 4.8 | 4.0 |
| Medication adherence (%) | 63.7 | 62.3 | 64.6 | 65.3 | 62.6 |
| AHT Therapy (%) | 54.4 | 43.9 | 54.2 | 63.4 | 71.0 |
| Hypertension (%) | 56.1 | 40.3 | 52.0 | 70.4 | 89.8 |
| Diabetes (%) | 19.3 | 12.8 | 18.7 | 24.4 | 31.5 |
| Dyslipidemia (%) | 55.1 | 51.1 | 55.9 | 58.7 | 59.0 |
Abbreviations: AHT, antihypertensive; BMI, body mass index; SBP, systolic blood pressure; SD, standard deviation.
aAlcohol consumption (based on drinks per week categorization by the National Institute on Alcohol Abuse and Alcoholism): None = 0, Moderate = 1–7 drinks for women, 1–14 drinks for men, Heavy = 7+ drinks for women, 14+ drinks for men.
Statistical analysis
The study participants’ demographic, socioeconomic, lifestyle, and vascular risk factors were calculated according to the level of their PP. Cumulative incidence curves were constructed for each outcome and compared with PP levels; a log-rank test of equality was performed for each set of curves. Standard Cox proportional hazards regression was used to estimate the hazard ratios (HRs) for incident acute CHD, CVD-related death, nonfatal MI, and fatal MI relevant to PP level (45–54mm Hg, 55–64mm Hg, and ≥ 65mm Hg, with each outcome measure compared with its value for a PP < 45mm Hg), in a series of incremental models. Models were first adjusted for age, race, gender, region, income, and education, and then, as added adjustments, for adherence to medication regimens, general health status, body mass index (BMI), HTN, diabetes, dyslipidemia, smoking, alcohol use, and antihypertensive therapy, and finally with an added adjustment for systolic BP. To establish the independent contribution of PP to a CHD-related outcome, HRs were obtained from the final models with and without adjustment for SBP. Incident first events were analyzed, with nonfatal and fatal cases of MI taken as mutually exclusive outcomes. For standard Cox regression analyses, time to first nonfatal MI, time to fatal MI, and time to death from CVD were calculated. For the combined acute CHD-related outcome of study participants, the time to an event was defined as the date of the first nonfatal MI, fatal MI, or CVD-related death; that data of participants who did not experience one of these events were censored at their date of death or last follow-up. In a sensitivity analysis, we used competing risks regression to adjust risk estimates because of the competing risk of all-cause mortality.11,12
Proportional hazards assumptions were tested by including log-transformed terms for the interaction of PP with time in the multivariate Cox and competing risks regression models. Collinearity of PP and SBP was assessed with the Pearson correlation coefficient and subsequently by calculating the variance inflation factor in fully adjusted linear regression models for each outcome. Additional demographic subgroup results and interactions were assessed as secondary analyses. Statistical tests were interpreted at alpha = 0.05. Descriptive statistics and standard Cox regression models were calculated with SAS version 9.3 (SAS Institute, Cary, NC), and cumulative incidence curves and competing risks regression models (command: stcrreg) were generated with Stata version 12 (StataCorp, College Station, TX).
RESULTS
Of the total REGARDS population sample (n=30,239), 5,239 participants reported a history of prevalent CHD and were excluded from the primary analysis of the study data. After further exclusion for errors in consent (n=56), missing follow-up data (n=543), missing covariate data (n=1,408), and missing SBP and/or DBP (n=84) data, the analytic sample consisted of 22,909 subjects (Figure 1). The characteristics of the study sample are shown in Table 1 by PP group. Age increased in accordance with increased PP. The percent of subjects with an annual household income < $20,000 increased with increasing PP categories, in contrast to the trend for subjects making more than $75,000 per year, for whom the percent of subjects decreased with increasing PP, a trend also seen with level of education as a correlative variable.
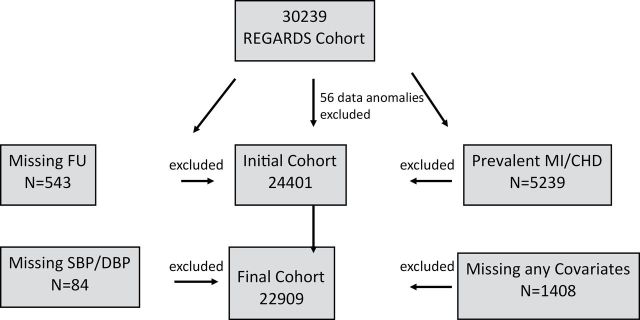
Figure 1. Exclusionary Cascade.
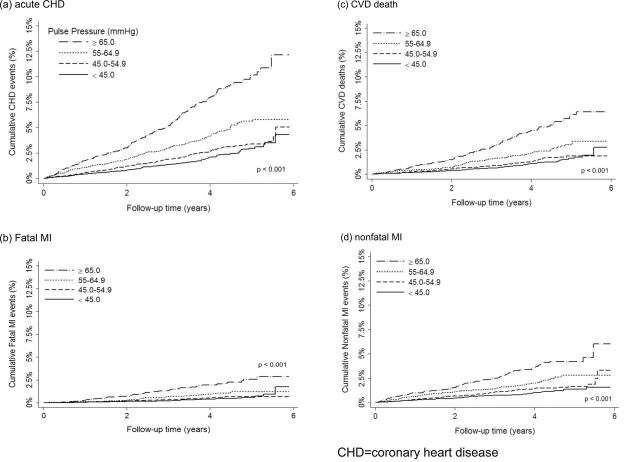
Unadjusted cumulative incidence curves comparing PP categories and acute CHD, fatal and nonfatal MI, and CVD-related death are shown in Figure 2. The results of the primary multivariate analyses are presented in Table 2, which presents the HRs for the PP groups in relation to all acute CHD-related events, and also but separately for fatal MI, nonfatal MI, and CVD-related death. Also noted in Table 2 is that there were 681 cases of acute incident CHD plus CVD, among which there were 357 deaths from CVD, 147 fatal MIs, and 331 nonfatal MIs (as defined above). For any acute CHD-related event, and for each of the components of acute CHD included in the study, the HR increased with each group of increasing PP, both in the unadjusted model and adjusted models, except for death from CVD in the fully adjusted model, which includes SBP, for which the HR in comparing a PP ≥ 65mm Hg vs. a PP < 45mm Hg was 1.45 (95% confidence interval [CI]: 0.92, 2.27), although the P for trend was 0.04. There was no evidence that violated the proportional hazards assumption. Additionally, we determined that although the unadjusted correlation between PP and SBP was strong (r=0.81), the variance inflation factor (VIF) for the PP groups and for SBP indicated an independent value of each factor; in fully adjusted linear regression models, the values of VIF for PP and SBP were 2.4 and 2.6, respectively.
Figure 2.
Exclusionary Cascade. Cumulative incidence curves comparing pulse pressure categories for acute CHD, CVD death, fatal myocardial infarction, and nonfatal MI. P-values reported are for a Wilcoxon test of equality.
Table 2.
Risks of incident coronary heart disease and cardiovascular disease-related death associated with pulse pressure levels in participants in the REasons for Geographic And Racial Differences in Stroke study as calculated with standard Cox regression methods
| Pulse pressure (mm Hg) | P for trend | ||||
|---|---|---|---|---|---|
| <45 (n=8,099) | 45–54.9 (n=7,539) | 55–64.9 (n=4,421) | ≥ 65.0 (n=2,850) | ||
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| Any acute CHD- related event | |||||
| Events (n) | 139 | 173 | 166 | 203 | |
| Unadjusted | 1 (Ref) | 1.28 (1.02, 1.59) | 2.06 (1.65, 2.58) | 3.82 (3.08, 4.74) | <0.001 |
| Demo.-SES adjusteda | 1 (Ref) | 1.08 (0.86, 1.35) | 1.49 (1.19, 1.88) | 2.32 (1.85, 2.91) | <0.001 |
| Fully adjustedb | 1 (Ref) | 1.05 (0.83, 1.32) | 1.36 (1.07, 1.72) | 2.12 (1.66, 2.70) | <0.001 |
| Fully adjusted + SBP | 1 (Ref) | 0.95 (0.75, 1.21) | 1.15 (0.88, 1.50) | 1.57 (1.12, 2.18) | 0.01 |
| CVD death | |||||
| Events (n) | 72 | 86 | 86 | 113 | |
| Unadjusted | 1 (Ref) | 1.21 (0.89, 1.66) | 2.03 (1.48, 2.78) | 3.99 (2.97, 5.36) | <0.001 |
| Demo.-SES adjusteda | 1 (Ref) | 0.96 (0.70, 1.32) | 1.28 (0.93, 1.76) | 1.96 (1.44, 2.66) | <0.001 |
| Fully adjustedb | 1 (Ref) | 0.91 (0.66, 1.25) | 1.17 (0.84, 1.63) | 1.81 (1.31, 2.51) | <0.001 |
| Fully adjusted +SBP | 1 (Ref) | 0.85 (0.60, 1.18) | 1.04 (0.72, 1.50) | 1.45 (0.92, 2.27) | 0.04 |
| Fatal MI | |||||
| Events (n) | 29 | 33 | 35 | 50 | |
| Unadjusted | 1 (Ref) | 1.16 (0.70, 1.91) | 2.06 (1.26, 3.37) | 4.40 (2.78, 6.95) | <0.001 |
| Demo.-SES adjusteda | 1 (Ref) | 0.96 (0.58, 1.59) | 1.46 (0.89, 2.41) | 2.60 (1.61, 4.20) | <0.001 |
| Fully adjustedb | 1 (Ref) | 0.91 (0.54, 1.54) | 1.36 (0.81, 2.30) | 2.40 (1.43, 4.02) | 0.001 |
| Fully adjusted +SBP | 1 (Ref) | 0.93 (0.54, 1.60) | 1.40 (0.78, 2.51) | 2.52 (1.25, 5.07) | 0.008 |
| Nonfatal MI | |||||
| Events (n) | 68 | 90 | 82 | 91 | |
| Unadjusted | 1 (Ref) | 1.36 (1.00, 1.87) | 2.10 (1.53, 2.90) | 3.54 (2.59, 4.85) | <0.001 |
| Demo.-SES adjusteda | 1 (Ref) | 1.24 (0.91, 1.71) | 1.77 (1.27, 2.46) | 2.75 (1.97, 3.83) | <0.001 |
| Fully adjustedb | 1 (Ref) | 1.21 (0.88, 1.67) | 1.56 (1.11, 2.20) | 2.41 (1.69, 3.43) | <0.001 |
| Fully adjusted + SBP | 1 (Ref) | 1.09 (0.77, 1.53) | 1.30 (0.88, 1.92) | 1.74 (1.07, 2.83) | 0.11 |
Abbreviations: CHD, coronary heart disease; CI, confidence interval; Demo.-SES, demographic and socioeconomic status variables; HR, hazard ratio; SBP, systolic blood pressure.
aModel adjusted for age, race, gender, region, income, and education.
bModel adjusted for age, race, gender, region, income, education, medication adherence, general health status, body mass index, hypertension, diabetes, dyslipidemia, smoking, alcohol use, and antihypertensive therapy.
Table 3 provides the subgroup analyses (age, race, sex) for the full model, and Figure 2 provides the subgroup analysis for PP ≥ 65mm Hg for all acute CHD-related events with and without the additional adjustment for SBP. There were no regional differences in the results of these analyses (data not shown).
Table 3.
Risks of incident coronary heart disease and cardiovascular disease-related death across pulse pressure levels, stratified by sex, race, and study region, according to standard Cox regression methodsa,b
| Pulse pressure (mm Hg) | Interaction P-value | |||
|---|---|---|---|---|
| 45–54.9 (n = 7,539) | 55–64.9 (n = 4,421) | ≥ 65.0 (n = 2,850) | ||
| HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| Any acute CHD event | ||||
| Men | 0.96 (0.71, 1.30) | 1.23 (0.87, 1.74) | 2.05 (1.34, 3.13) | 0.27 |
| Women | 0.96 (0.65, 1.42) | 1.09 (0.71, 1.66) | 1.15 (0.68, 1.95) | |
| Black | 0.94 (0.66,1.35) | 1.00 (0.67, 1.50) | 1.61 (1.00, 2.58) | 0.22 |
| White | 0.99 (0.72,1.37) | 1.35 (0.94, 1.95) | 1.59 (0.99, 2.56) | |
| Belt | 0.92 (0.67,1.27) | 0.96 (0.67, 1.39) | 1.26 (0.80, 1.97) | 0.60 |
| Non-Belt | 1.02 (0.71,1.46) | 1.44 (0.97, 2.14) | 2.03 (1.23, 3.32) | |
| CVD death | ||||
| Men | 0.92 (0.59, 1.43) | 1.19 (0.73, 1.97) | 2.20 (1.20, 4.01) | 0.80 |
| Women | 0.76 (0.45, 1.28) | 0.91 (0.52, 1.57) | 0.93 (0.47, 1.85) | |
| Black | 0.90 (0.57, 1.41) | 1.03 (0.63, 1.69) | 1.67 (0.94, 2.99) | 0.67 |
| White | 0.82 (0.49, 1.37) | 1.11 (0.64, 1.95) | 1.32 (0.64, 2.74) | |
| Belt | 0.87 (0.53, 1.40) | 0.86 (0.51,1.47) | 1.01 (0.53, 1.92) | 0.48 |
| Non-Belt | 0.87 (0.54, 1.40) | 1.34 (0.80, 2.24) | 2.10 (1.11, 3.97) | |
| Fatal MI | ||||
| Men | 0.79 (0.40, 1.58) | 1.50 (0.73, 3.07) | 3.33 (1.43, 7.77) | 0.33 |
| Women | 1.18 (0.48, 2.90) | 1.21 (0.44, 3.33) | 1.44 (0.41, 5.08) | |
| Black | 0.85 (0.43, 1.66) | 0.81 (0.37, 1.78) | 2.25 (0.94, 5.41) | 0.09 |
| White | 1.12 (0.44, 2.81) | 2.79 (1.09, 7.12) | 3.23 (0.99, 10.53) | |
| Belt | 0.91 (0.44, 1.89) | 1.02 (0.45, 2.32) | 1.59 (0.60, 4.25) | 0.91 |
| Non-Belt | 0.95 (0.42, 2.14) | 1.90 (0.82, 4.42) | 3.75 (1.37, 10.26) | |
| Nonfatal MI | ||||
| Men | 1.01 (0.66, 1.52) | 1.31 (0.81, 2.13) | 1.88 (1.02, 3.46) | 0.15 |
| Women | 1.34 (0.74, 2.45) | 1.39 (0.72, 2.70) | 1.75 (0.78, 3.93) | |
| Black | 1.07 (0.58, 1.97) | 1.00 (0.50, 2.01) | 1.72 (0.77, 3.83) | 0.24 |
| White | 1.14 (0.76, 1.73) | 1.56 (0.97, 2.52) | 1.76 (0.95, 3.29) | |
| Belt | 1.03 (0.67, 1.58) | 1.11 (0.67, 1.83) | 1.57 (0.85, 2.92) | 0.80 |
| Non-Belt | 1.24 (0.71, 2.16) | 1.69 (0.91, 3.13) | 2.08 (0.94, 4.59) | |
Abbreviations: CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; MI, myocardial infarction.
aReferent group is pulse pressure < 45mm Hg; n = 8,099.
bAdjusted for age, race, gender, region, income, education, medication adherence, general health status, body mass index, hypertension, diabetes, dyslipidemia, smoking, alcohol use, antihypertensive therapy, and systolic blood pressure.
Sensitivity analyses done through competing risks regression produced results similar to those eached with standard Cox regression analysis (Table 2) for acute CHD, CVD-related death, fatal MI, and nonfatal MI. For example, in the fully adjusted (including SBP) competing risks regression model for acute CHD, the sub-hazard ratio and 95% CI for PP levels (as compared with < 45.0mm Hg) of 45–54.9mm Hg, 55–64.9mm Hg, and ≥ 65.0mm Hg were 0.95 (0.75, 1.21), 1.19 (0.91, 1.55), and 1.57 (1.13, 2.19), respectively. There was no evidence that violated the proportional hazards assumption.
DISCUSSION
Our analysis of the REGARDS data suggests that PP is an independent risk factor for any acute CHD-related event (HR = 1.57; 95% CI: 1.12, 2.18 in the fully adjusted model that included adjustment for SBP, comparing PP ≥ 65mm Hg with PP < 45mm Hg), and this is also true for the individual components of CHD risk (fatal and nonfatal MI), except for death from CVD, for which the increase in risk was borderline significant. There was a linear increase in risk for combined fatal and nonfatal MI and for the individual components of acute CHD with increasing PP (P for linear trend = 0.0001 for most measures). However, subgroup analysis showed no statistically significant differences in these associations across age and race or region of the country (except for the suggestion that men may be more sensitive to PP than are women).
Cardiovascular mortality and its various clinical manifestations, such as angina, MI, stroke, and cardiac failure, are increased in the presence of elevated blood pressure. Traditionally, this has been measured by sphygmomanometry, which yields two measures of blood pressure: SBP and DBP. It is increasingly argued that neither SBP nor DBP may be as strong a predictor of acute CHD as is PP. Thus, PP may be a key measure of blood pressure, particularly in older individuals, and may increase in importance as a risk factor for CVDE, including stroke, MI, and death. However, arguments persist as to whether PP is independent (particularly from SBP) as a measure of CHD risk.1 The Framingham study, in its longitudinal follow-up of persons over 50 years of age, found that cardiovascular (and in particular coronary) mortality is associated with increased PP.5 In that study, mortality was related independently to initial SBP and DBP, but the strongest association was with PP, and when SBP was initially considered, there was a negative association with DBP. In other words, for a given SBP, a lower DBP was associated with greater mortality.
As Millar and Lever pointed out,13 the superiority of PP as a predictor of cardiac risk in hypertension is supported by “3 strands of evidence,” as follows: 1) PP is a risk factor for coronary events (MI, angina, heart failure, and cardiac death); 2) PP is strongly associated with, and a potential determinant of, several surrogate markers of cardiac risk such as echocardiographically determined left atrial and ventricular mass,14 electrocardiographic indices of ischemia and cardiac size,15 and carotid-wall thickness;16,17 and 3) there is a physiologically plausible mechanism linking increased conduit artery stiffness to cardiac risk via increased PP. In other words, increased arterial-wall stiffness (itself a well-recognized index of cardiovascular mortality18) increases SBP during systole, increases pulse-wave velocity, and promotes early return of the reflected aortic pressure wave during late systole rather than during diastole. These effects increase left ventricular work and oxygen requirements and simultaneously tend to diminish coronary perfusion.19,20 On the other hand, cerebral blood flow occurs throughout the cardiac cycle, and the relationship between PP and stroke is weak.6
There is now increasing evidence that a high PP, reflecting large-artery stiffness, is a significant independent risk factor for cardiovascular and especially coronary mortality in different populations. Madhavan et al. reported that subjects with untreated hypertension and a PP of 63mm Hg had an increased risk of cardiovascular complications.21 In addition, they found that these subjects were at greater risk of MI when there was too great a decrease in DBP after treatment.5 Franklin et al. in a study with a larger population of subjects with treated and untreated hypertension, reported that PP was the only blood pressure measurement independently related to the treatment incidence of MI.7 The link between PP and cardiovascular complications has also been shown in subjects who had MI with left-ventricular dysfunction.1
Our study has several limitations worth noting. Some risk factors not related to laboratory-measured variables were based on self-reports, and individuals without telephones were necessarily excluded from inclusion in the study population. These excluded individuals may have been of lower socioeconomic status, and may therefore have had different risk-factor profiles than those included in the study.
In conclusion, in this large national cohort study, we observed that PP was an independent risk factor for acute CHD, and that this risk was consistent across subgroups defined by age and race. For at least some presentations of CHD, men may be more sensitive to PP than are women.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. Benetos A, Safar M, Rudnichi A, Smulyan H, Richard JL, Ducimetrieère P, Guize L. Pulse pressure: a predictor of long-term cardiovascular mortality in a French male population. Hypertension 1997; 30:1410–1415. 10.1161/HYP.30.6.1410 [DOI] [PubMed] [Google Scholar]
- 2. Brown DW, Giles WH, Greenlund KJ. Blood pressure parameters and risk of fatal stroke, NHANES II mortality study. Am J Hypertens 2007; 20:338–341. 10.1016/j.amjhyper.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 3. Geeganage C, Sare G, Bath PM. Pulse pressure as a predictor of stroke. Exp Rev Neurother 2008; 8:165–167. 10.1586/14737175.8.2.165 [DOI] [PubMed] [Google Scholar]
- 4. Verdecchia P, Schillaci G, Reboldi G, Franklin SS, Porcellati C. Different prognostic impact of 24-hour mean blood pressure and pulse pressure on stroke and coronary artery disease in essential hypertension. Circulation 2001; 103:2579–2584. 10.1161/01.CIR.103.21.2579 [DOI] [PubMed] [Google Scholar]
- 5. Franklin SS, Khan SA, Wong ND, Larson MG, Levy D. Is pulse pressure useful in predicting risk for coronary heart Disease? The Framingham Heart Study. Circulation 1999; 100:354–360. 10.1161/01.CIR. 100.4.354 [DOI] [PubMed] [Google Scholar]
- 6. Halberg DL, Sands C, Le A, Howard VJ, Safford M, Glasser SP, Muntner P, Howard G. Pulse and mean arterial pressure as predictors of stroke in the REGARDS Study. Stroke 2012; 43:A2593 [Google Scholar]
- 7. Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 2005; 25:135–143. 10.1159/000086678 [DOI] [PubMed] [Google Scholar]
- 8. Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D, Goldberg RJ, Hand MM, Jaffe AS, Julian DG, Levy D, Manolio T, Mendis S, Mensah G, Pajak A, Prineas RJ, Reddy KS, Roger VL, Rosamond WD, Shahar E, Sharrett AR, Sorlie P, Tunstall-Pedoe H; AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; National Heart, Lung, and Blood Institute. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation 2003; 108:2543–2549. 10.1161/01.CIR.0000100560.46946.EA [DOI] [PubMed] [Google Scholar]
- 9. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. US Department of Health and Human Services, NIH, National Heart Lung and Blood Institute, National High Blood Pressure Education Program.NIH Publication No. 04-5230. Aug. 2004 [PubMed]
- 10. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care 1986; 24:67–74 http://www.jstor.org/stable/3764638 [DOI] [PubMed] [Google Scholar]
- 11. Feinstein M, Ning H, Kang J, Bertoni A, Carnethon M, Lloyd-Jones DM. Racial differences in risks for first cardiovascular events and noncardiovascular death: the Atherosclerosis Risk in Communities study, the Cardiovascular Health Study, and the Multi-Ethnic Study of Atherosclerosis. Circulation 2012; 126:50–59 PMC3437934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94:496–509. 10.1038/bmt.2009.359 [Google Scholar]
- 13. Millar JA, Lever AF. Implications of pulse pressure as a predictor of cardiac risk in patients with hypertension. Hypertension 2000; 36:907–911. 10.1161/01.HYP.36.5.907 [DOI] [PubMed] [Google Scholar]
- 14. Gardin JM, Arnold A, Gottdiener JS, Wong ND, Fried LP, Klopfenstein HS, O’Leary DH, Tracy R, Kronmal R. Left ventricular mass in the elderly. The Cardiovascular Health Study. Hypertension 1997; 29:1095–1103. 10.1161/01.HYP.29.5.1095 [DOI] [PubMed] [Google Scholar]
- 15. Darne B, Girerd X, Safar M, Cambien F, Guize L. Pulsatile versus steady component of blood pressure: a cross-sectional analysis and a prospective analysis on cardiovascular mortality. Hypertension 1989; 13:392–400. 10.1161/01.HYP.13.4.392 [DOI] [PubMed] [Google Scholar]
- 16. Mitchell GF. Pulse pressure, arterial compliance and cardiovascular morbidity and mortality. Curr Opin Nephrol Hypertens 1999; 8:335–342 [DOI] [PubMed] [Google Scholar]
- 17. Zanchetti A, Bond MG, Hennig M, Neiss A, Mancia G, Dal Palù C, Hansson L, Magnani B, Rahn KH, Reid J, Rodicio J, Safar M, Eckes L, Ravinetto R. Risk factors associated with alterations in carotid intima-media thickness in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis. J Hypertens 1998; 16:949–961 [DOI] [PubMed] [Google Scholar]
- 18. Blacher J, Pannier B, Guerin AP, Marchais SJ, Safar ME, London GM. Carotid arterial stiffness as a predictor of cardiovascular and all-cause mortality in end-stage renal disease. Hypertension 1998; 32:570–574. 10.1161/01.HYP.32.3.570 [DOI] [PubMed] [Google Scholar]
- 19. Franklin SS. Cardiovascular risks related to increased diastolic, systolic and pulse pressure. An epidemiologist’s point of view. Pathol Biol (Paris) 1999; 47:594–603 [PubMed] [Google Scholar]
- 20. Safar ME, Siche JP, Mallion JM, London GM. Arterial mechanics predict cardiovascular risk in hypertension. J Hypertens 1997; 15:1605–1611 [DOI] [PubMed] [Google Scholar]
- 21. Madhavan S, Ooi WL, Cohen H, Alderman MH. Relation of pulse pressure and blood pressure reduction to the incidence of myocardial infarction. Hypertension 1994; 23:395–401. 10.1161/01.HYP.23.3.395 [DOI] [PubMed] [Google Scholar]