All free‐living organisms are regulated by the 24‐h light and dark cycle produced by Earth’s rotation. In mammals, circadian rhythms are indispensble for the regulation of physiological and biochemical processes in the body. In 1972, the suprachiasmatic nucleus was shown to be required for daily rhythms in animal behavior1. Light signals through the optic nerves give the cue to set the clock and to synchronize the various behavioral outputs. Interstingly, both the central nervous system and almost all peripheral tissues and cells express the circadian oscillator transcriptional factors CLOCK and BMAL1, which regulate cellular functions. CLOCK and BMAL1 heterodimerize and activate downstream target genes rhythmically, including the period (Per1, Per2 and Per3) and cryptochrome (Cry1 and Cry2) genes2. All cells in the body are regulated by this clock gene system according to the day–night cycle in an organized way. Several findings in mammals have suggested that clocks outside the brain paticipate in metabolic regulation. For example, expression of the receptors, transporters and enzymes that regulate key steps of cellular metabolism are under circadian regulation. In addition, circadian clocks outside the suprachiasmatic nucleus rely on feeding cues rather than light signals. Disruption of this molecular clock system has been shown to induce deleterious metabolic outcomes, diseases and tumors.
Because disruption of clock genes affects both locomotor activity and feeding behavior, and also might indirectly change metabolism3, it has been considered that clocks outside the brain have a local function and that an effect on metabolism is slight. Recent work on organ‐specific inactivation of genes, such as BMAL1, have shown this for liver circadian clocks in glucose metabolism; however, many questions regarding circadian activity outside the brain remain to be answered.
Recently, Marcheva et al.4 reported that disruption of the clock componets, CLOCK and BMAL1, leads to diabetes (Figure 1). They showed evidence that the mouse pancreas has a functional circadian clock; pancreatic islets also show robust rhythmical activity, even if they are excluded from the tissue environment. This mammalian islet clock regulates the expression of genes involved in glucose sensing, insulin secretion, and islet cell growth and development.
Figure 1.
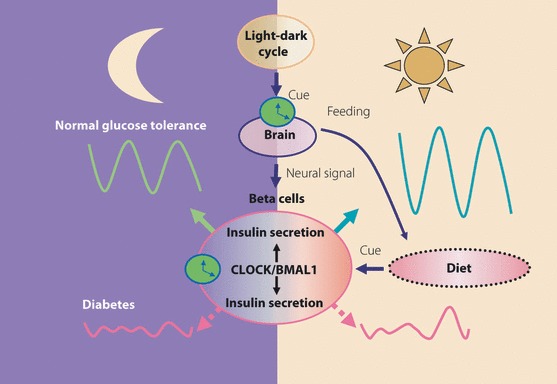
Pancreatic clock machinery and glucose metabolism. Regulatory mechanisms of CLOCK/BMAL1 in pancreatic insulin secretion in day and night through the step of insulin granule exocytosis. Disruption of this mechanism leads to diabetes as a result of a defect in gene expression in the regulaion of insulin secretion, and development of pancreatic islets.
An insulin secretory defect should result from β‐cell dysfunction or reduction in β‐cell mass5. Morphometric studies indicate that type 2 diabetes patients have lost approximately 50% of their β‐cells. As a 50%β‐cell loss in experimental animals does not produce the fasting hyperglycemia regulary seen in type 2 diabetes, additional factors, such as dysfunction of the remaining β‐cells or concomittent insulin resistance, might contribute6. It has long been recognized that normal glucose‐induced insulin secretion in humans varies across the day–night cycle, and that disruption of the circadian oscillation of glucose metabolism is a feature of type 2 diabetes7. Marcheva et al.4 described the mechanism of this pathophysiological state. The authors showed that mice in which the circadian clock is disrupted produce less insulin in the resting state and secrete less insulin in response to glucose. In addition, morphometric analyses show that the pancreatic islets are smaller and that production of insulin is reduced. These results suggest direct involvement of the islet clock in the production of insulin. Although an impaired acute insulin response to intravenous glucose challenge is typical in human type 2 diabetes, non‐glucose stimulated insulin secretion is also reduced when plasma glucose levels are matched by either a glucose infusion in normal sujects or an insulin infusion in type 2 diabetic subjects. Animals with conditional pancreatic clock ablation represent an interesting form of diabetes – the islets show not only an impaired insulin response to glucose, but to KCl and the adenylate cyclase activators, froskolin and exendin‐4, which suggests a defect in insulin exocytosis, but not in glucose metabolism.
One of the major issues in the circadian clock’s role in diabetes is whether disruption of CLOCK or BMAL 1 leads to metabolic defects by affecting circadian rhythms or by mechanisms not related to their clock function. To answer this question is essential – if disruption of clock genes is involved in development of diabetes by affecting circadian rhythms directly, industrialized, modern lifestyle itself has a pathological impact. Unusual rhythms of eating, fasting, sleeping, wakefulness and activity are more or less forced on more and more individuals by requirements of living, especially by shift work. From a clincal point of view, an epidemiological study of circadian disruption by shift work or other lifestyle disruptions of the day–night cycle in the development of diabetes and related disorders in the developed and developing world is required. Several reports have shown that CLOCK and BMAL1 are associated with features of metabolic syndrome. Polymorphisms in the clock gene have been correlated with predisposition to obesity, and two BMAL1 haplotypes are associated with type 2 diabetes and hypertension2. Shift work involves 20–25% of the employees in the manufacturing industry worldwide, and is becoming increasingly prevalent in contemporary life. Although a precise definition of shift work is lacking, most studies classify shift workers as those who work regularly outside the usual daytime shift hours. Shift work is thought to be associated with several health problems, such as metabolic syndrome, diabetes mellitus and cardiovascular disease, that are possibly the result of impaired biological circadian rhythms. Indeed, a higher prevalence of metabolic syndrome has recently been shown among shift workers8. Some Japanese reports have shown shift work to be an independent risk factor for impaired glucose metabolism and higher prevalence of diabetes mellitus. Other problems of 24‐h contemporary life have been investigated, such as night eating and breakfast skipping, which are suggested to have an association with obesity and visceral adiposity in overweight youth9,10. Sleep disorders (short duration and/or poor quality sleep) also have a profound impact on the development of type 2 diabetes and obesity2. Thus, the mechanism by which disruption of CLOCK‐related genes affects circadian rhythms directly might underlie the recent rapid increase of diabetes worldwide. Technical developments that allow modification of specific and selective controls of clock function are required, in addition to continued study of the physiological and pathphysiological significance of circadian rhythms in the development of diabetes mellitus.
Acknowledgement
The authors have no competing financial interests to disclose.
References
- 1.Stephan FK, Zucker I. Circadian rhythms in drinking behavior and locomotor activity of rats are eliminated by hypothalamic lesions. Proc Natl Acad Sci USA 1972; 69: 1583–1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Green CB, Takahashi JS, Bass J. The meter of metabolism. Cell 2008; 134: 728–742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ikeda H, Yong Q, Kurose T, et al. Clock gene defect disrupts light‐dependency of autonomic nerve activity. Biochem Biophys Res Commun 2007; 364: 457–463 [DOI] [PubMed] [Google Scholar]
- 4.Marcheva B, Ramsey KM, Buhr ED, et al. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 2010; 466: 627–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rorsman P. Insulin secretion: function and therapy of pancreatic beta‐cell in diabetes. Br J Diabetes Vasc Dis 2005; 5: 187–191 [Google Scholar]
- 6.Ahren BO, Taborsky GJ. Chapter 4. Beta‐cell function and insulin secretion In: Porte D, Sherwin RS, Baron A, Ellengerg M, Rifkin H (eds). Ellenberg and Rifkin’s Diabetes Mellitus, 6th edn Mc Graw‐Hill, New York, 2003, 43–66 [Google Scholar]
- 7.Polonsky KS, Given BD, Hirsch LJ, et al. Abnormal patterns of insulin secretion in non‐insulin‐dependent diabetes mellitus. N Engl J Med 1988; 318: 1231–1239 [DOI] [PubMed] [Google Scholar]
- 8.Szosland D. Shift work and metabolic syndrome, diabetes mellitus and ischemic heart disease. Int J Occup Med Environ Health 2010; 23: 1–5 [DOI] [PubMed] [Google Scholar]
- 9.Alexander KE, Ventura EE, Spruijt‐Metz D, et al. Association of breakfast skipping with visceral fat and insulin indices in overweight Latino youth. Obesity (Silver Spring) 2009; 17: 1528–1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morse SA, Katon WJ, Ciechanowski PS, et al. Isn’t this just bedtime snacking? The potential adverse effects of night‐eating symptoms on treatment adherence and outcomes in patients with diabetes. Diabetes Care 2006; 29: 1800–1804 [DOI] [PubMed] [Google Scholar]


