A good community‐based or hospital‐based program involving physicians and nurses is deemed useful for the management of chronic illnesses, such as diabetes, as this program would reduce health‐care costs, admission rates and emergency room visits1. Therefore, establishment of a health‐care system for the management of diabetes in a highly cost‐effective way is important from the viewpoint of public health. In 1990, the first government‐subsidized diabetes center with educators in Taiwan was founded at the National Taiwan University Hospital, wherein an integrated clinic for screening diabetic complications (retinopathy, microalbuminuria, peripheral neuropathy and ankle‐brachial index) was set up to monitor the outcomes of individuals with diabetes. Because of the increasing rate of diabetes prevalence and its associated chronic complications, the Department of Health commissioned the Diabetes Association of the Republic of China to help set up more diabetes centers in 1991, and 2 years later, the name was changed to Center for Health Promotion of Persons with Diabetes. As smaller units were set up in the regional hospitals and clinics, they were called Classroom for Health Promotion of Persons with Diabetes, and Clinic for Health Promotion of Persons with Diabetes, respectively. To date, 167 small and large units of Health Promotion of Persons with Diabetes have been set up with aid from the Taiwanese Association of Diabetes Educators (TADE), which was established in 1996 to train health professionals. The Bureau of National Health Insurance (BNHI) offers free Health Check‐Up for Adults every 3 years for persons aged over 40 years, and every year for persons aged over 65 years. To improve the quality of care for diabetic patients, a pilot program called Improvement Plan for Diabetes Medical Benefits was launched in November 2001. The pilot program was replaced by a formal program with introduction of a pay‐for‐performance (P4P)2 scheme in 2007. For the first time in the history of diabetes education in Taiwan, the program reimbursed the cost of patient education by a certified nurse and dietitian included in the case management fee, in addition to the usual physician’s fees and the medication fees. To be eligible for this program, the patients must undergo a baseline assessment, and an annual check‐up for a complete biochemical examination and screening for complications. The data of these assessments have to be uploaded to the BNHI website. To date, approximately 30% of diabetic patients in Taiwan have been covered by the improvement program.
There has been a paradigm shift in health care since 1995 with a health insurance reform; the National Health Insurance (NHI) was launched, which is an obligatory program for all individuals in Taiwan. The frequency of undiagnosed diabetes mellitus (DM) was approximately 50% (range 45–56%) in several surveys carried out before 1996. In a very recent survey, the frequency of undiagnosed DM had decreased to 20%, which was a significant drop after 14 years since the establishment of NHI. In this system, nationwide data could be obtained from the NHI claims database. These data are potentially useful for monitoring the various aspects of diabetes management in Taiwan; for example, for estimating the diabetes population and diabetic complications, for quality assessment of process indicators, for determining the health utility and its cost, and for determining the diabetes mortality rate.
In the estimation of the total population with diabetes, we found that the number of people with at least one visit for DM (ICD‐9 250) increased from 0.86 to 1.39 million (an increase of 62%) from 1999 to 2009 (Figure 1). This increasing trend is consistent with the global trend. A detailed analysis showed that the increasing incidence of diabetes could be attributed to the steady increase in the number of young male individuals3. The factors associated with the gender‐specific increase are presently unclear. However, that study identified a target population for prevention, early detection and early intervention. With this, we have developed an easily accessible open website for the identification of high‐risk factors for diabetes and metabolic syndrome on the basis of the Taiwan Diabetes Risk Score validated in our population4 and described in our National Guideline for Clinical Management of Diabetes. After the website was initially established and young people became familiar with its use, we found that nearly 20% of the young adults were at a high risk for metabolic syndrome, and their lifestyle included smoking and less physical activity, which was significantly correlated with the risk of type 2 diabetes mellitus. However, the earlier identified group benefited from better care, and the outcome remains to be further investigated.
Figure 1.
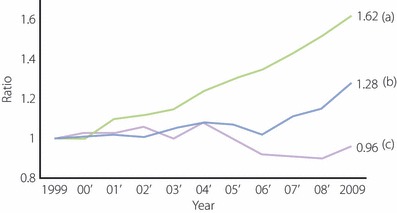
Trends for (a) diabetic patient number, (b) annual rate for emergency and (c) in hospital in Taiwan (baseline 1999 = 1).
For the past 10 years, we have observed a decrease of 3.9% in the hospitalization rate of diabetic individuals (Figure 1). However, the incidence of emergency visits has increased by 28% (Figure 1), potentially as a result of severe hypoglycemia, which is known to be clearly high in patients receiving highly intensive diabetes treatment. Both increasing rates are lower than that of the total diabetic population (Figure 1). In contrast, we also found that there were severe complications, including disease conditions that needed aggressive interventions, when using hospital discharge ICD‐9‐CM diagnostic and procedure codes to identify patients with severe cardiovascular disease (CVD) who had been admitted for myocardial infarction, coronary artery bypass graft and percutaneous transluminal coronary angioplasty or stent. Type 2 diabetic patients with severe peripheral arterial disease were defined as those who had been hospitalized for a peripheral revascularization procedure or lower extremity amputation as a result of non‐traumatic injury. Type 2 diabetic patients with severe eye disease were defined as those with low visual acuity/blindness or with photocoagulation and identified by the outpatient ICD‐9‐CM diagnostic and procedure codes. The inpatient ICD‐9‐CM procedure codes for kidney transplantation and specific codes in outpatient service claims for hemodialysis and peritoneal dialysis were used to identify patients with severe renal complication. These analyses showed an increasing trend of severe CVD and severe renal failure during the past years, whereas the trend of stroke/cerebral vascular disease decreased in recent years (data not shown).
Since 2007, when Taiwan’s NHI system implemented P4P programs to encourage healthcare providers to increase the monitoring and follow‐up care of patients, the P4P program for diabetes has been shown to be associated with a significant increase in regular follow‐up visits and evidence‐based services. The hospitalization costs became significantly low, although the overall cost of care for those in the P4P program was significantly high, with a net increase of $104 per person per year. The long‐term cost‐effectiveness analysis in terms of incremental cost‐effectiveness ratio remains to be evaluated.
Close monitoring of the diabetes mortality rate is also an important health issue as a final assessment of quality care for individuals with diabetes. Importantly, there has been a declining trend in the diabetes mortality rate in recent years, with a decrease in the age‐ and sex‐adjusted diabetes mortality rate from 2000 to 2009. The factors responsible for this reduction in the mortality rate cannot be directly interpreted from the NHI database, as there were no laboratory examination results that could preclude further analyses. One of the quality dimensions is to evaluate the process indicators, such as the adherence to guidelines; for example, regular check‐up of laboratory tests and screening for chronic complications. For this reason, NHI reports the accountability for diabetes care annually. In 2004, the HbA1c (A1C) check‐up rate at least once per year for all diabetic individuals in Taiwan was 53.2%. This rate increased to 83.7% in 2009, and these observations were similar in medical centers, regional hospitals, local hospitals and private clinics. For the patients enrolled in the improvement plan, the rate was almost 100%. Furthermore, the check‐up rates for microalbuminuria, retina and lipid levels improved in this 5‐year period from 2004 to 2009.
As a database of the laboratory test results was absent, we needed to have some representative national surveys for glycemic control (A1C), dyslipidemia (low‐density lipoprotein cholesterol and high‐density lipoprotein cholesterol) and blood pressure control. To date, several surveys for glycemic control have been carried out in Taiwan from 1998 to 2008. The mean A1C was approximately 8.9% in all three surveys carried out by TADE (2002), DiabCare (2003) and TADE (2004). The mean A1C was found to be 7.9% in TADE’s survey in 20065, which was similar to that found in the DiabCare’s survey in 2008. However, a continuous improvement in diabetes care to reach the goal of our national guideline, that is, A1C at 6.5%, remains a challenge. The rates for those achieving goals of lipid and blood pressure control were nearly one‐third. Unfortunately, just 4.1% of our study population achieved all three target goals5 that are effective for reducing diabetic complications and for increasing long‐term survival in the classical Steno‐2 clinical study.
Finally, with support from the Bureau of Health Promotion a new organization for diabetic patients – the Taiwan Association of Patients with Diabetes – was formed in May 2008. The Association represents over 450 diabetic patient groups in different regions of Taiwan, and hopes to improve diabetes self‐care and high‐risk awareness.
In summary, the government plays an instrumental role in diabetes management and care. With a universal health insurance policy, the overall care can be reported by close monitoring of the patient’s and doctor’s adherence to the national guidelines, the cost and the area of high burden. With this information, we can formulate better policies and strategies to tackle clinically significant problems in the case of complex disorders, such as diabetes.
References
- 1.Miller LV, Goldstein J. More efficient care of diabetic patients in a county‐hospital setting. N Engl J Med 1972; 286: 1388–1391 [DOI] [PubMed] [Google Scholar]
- 2.Lee TT, Cheng SH, Lai MS. A pay‐for‐performance program for diabetes care in Taiwan: a preliminary assessment. Am J Manag Care 2010; 16: 65–69 [PubMed] [Google Scholar]
- 3.Chang CH, Shau WY, Jiang YD, et al. Type 2 diabetes prevalence and incidence among adults in Taiwan during 1999–2004: A national health insurance dataset study. Diabet Med 2010; 27: 636–643 [DOI] [PubMed] [Google Scholar]
- 4.Lin JW, Chang YC, Li HY, et al. Cross‐sectional validation of diabetes risk scores for predicting diabetes, metabolic syndrome, and chronic kidney disease in the Taiwanese population. Diabetes Care 2009; 32: 2294–2296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu NC, Su HY, Tsai ST, et al. ABC control of diabetes: survey data from National Diabetes Health Promotion Centers in Taiwan. Diabetes Res Clin Pract 2009; 84: 194–200 [DOI] [PubMed] [Google Scholar]


