Abstract
Chloroquine (CQ) is used as a first-line therapy for the treatment of Plasmodium falciparum malaria in Nicaragua. We investigated the prevalence of molecular markers associated with CQ and sulfadoxine-pyrimethamine (SP) resistance in P. falciparum isolates obtained from the North Atlantic Autonomous Region of Nicaragua. Blood spots for this study were made available from a CQ and SP drug efficacy trial conducted in 2005 and also from a surveillance study performed in 2011. Polymorphisms in P. falciparum CQ resistance transporter, dihydrofolate reductase, and dihydropteroate synthase gene loci that are associated with resistance to CQ, pyrimethamine, and sulfadoxine, respectively, were detected by DNA sequencing. In the 2005 dataset, only 2 of 53 isolates had a CQ resistance allele (CVIET), 2 of 52 had a pyrimethamine resistance allele, and 1 of 49 had a sulfadoxine resistance allele. In the 2011 dataset, none of 45 isolates analyzed had CQ or SP resistance alleles.
Introduction
The incidence of malaria in the Americas increased steadily after eradication efforts in the 1960s and then stabilized in the 1990s.1 In 1998, more than 1.2 million cases of malaria were reported in this region. However, this figure decreased to less than 600,000 cases in 2008 after comprehensive control efforts accelerated in 2005 in line with the Roll Back Malaria Global Strategic Plan.2 Meso-America is the northernmost sub-region of malaria endemicity in the Americas, spanning the contiguous landmass from Mexico through Panama. Plasmodium vivax malaria is far more common than P. falciparum malaria in this sub-region. Nonetheless, the parasite population in this area is unique in that it is one of the last remaining areas of endemic chloroquine (CQ)–sensitive P. falciparum.
The drug treatment policy for uncomplicated P. falciparum malaria in most of Meso-America, including Nicaragua, is a combination of CQ and primaquine as the first-line therapy, and artesunate plus sulfadoxine-pyrimethamine (SP) or artesunate plus mefloquine as second-line therapies. There is currently no clinical evidence of treatment failure associated with this treatment regimen for P. falciparum infections acquired in Nicaragua. However, there have been epidemics of P. falciparum malaria in Panama, east of the Panama Canal, where molecular markers of resistance to CQ and SP were detected.3
Polymorphisms in positions 72, 74, 75, and 76 of the P. falciparum CQ resistance transporter (pfcrt) gene have been associated with reduced parasite susceptibility to CQ.4 Therefore, pfcrt alleles are often described by their amino acid sequence at positions 72–76. CVMNK is generally regarded the wild-type pfcrt allele and is associated with CQ sensitivity. The pfcrt K76T polymorphism is considered the most critical change that confers CQ resistance and is often a reliable indicator of CQ treatment failure, particularly in low-transmission settings with non-immune populations.5,6 Notably, it was the K76T polymorphism that was associated with treatment failure in Panama.3 The pfcrt alleles SVMNT and CVMNT are found in South America; SVMNT is the most common.7 The CVMET genotype is found in Colombia. The CVIET genotype is common in Southeast Asia and Africa and has been reported at low prevalences in parts of South America.8
Polymorphisms in the P. falciparum dihydrofolate reductase (pfdhps) and P. falciparum dihydropteroate synthase (pfdhfr) genes been associated with decreased parasite sensitivity to sulfadoxine and pyrimethamine, respectively. The S108N polymorphism in pfdhfr is sufficient to cause low-level pyrimethamine resistance in vitro and in vivo.9–11 The progressive addition of polymorphisms, including C50R, N51I, C59R, and I164L, in pfdhfr can yield higher levels of pyrimethamine resistance.11–16 Alleles consisting of multiple polymorphisms, such as the C50R, N51I, S108N type and the C50R, N51I, S108N, I164L type, have been identified in Brazil, Peru, and Venezuela.17,18 In pfdhps, polymorphisms, including S436A/F, A437G, K540E, A581G, and A613S/T, have been shown to affect parasite susceptibility to sulfadoxine.19–21 All sulfadoxine resistance pfdhps alleles that have been identified in the Americas have the A437G polymorphism alone or in combination with K540E and/or A581G.
At present, there have been few in vivo or in vitro studies examining antimalarial resistance in Meso-America, these studies involved areas of high transmission. Recent surveys suggest that most of the P. falciparum malaria burden in Meso-America is concentrated in parts of Honduras and the North Atlantic Autonomous Region (NAAR) in Nicaragua.22 In 2004, Nicaragua reported 6,899 cases of malaria, of which 1,200 (17.4%) were caused by P. falciparum. Furthermore, the regional Sistema Local de Atencion Integral en Salud reported that 32% of all malaria cases and 50% of P. falciparum cases in Nicaragua occurred in the NAAR. In 2011, a total of 925 confirmed cases of malaria, including 150 cases of P. falciparum and mixed infections combined, were reported in Nicaragua. In this study, we characterized molecular markers of resistance for CQ and SP by using parasite isolates from a drug efficacy trial conducted in NAAR during November 2005–February 2006 and also parasite samples available from a routine surveillance study conducted in 2011 in the same region.
Methods
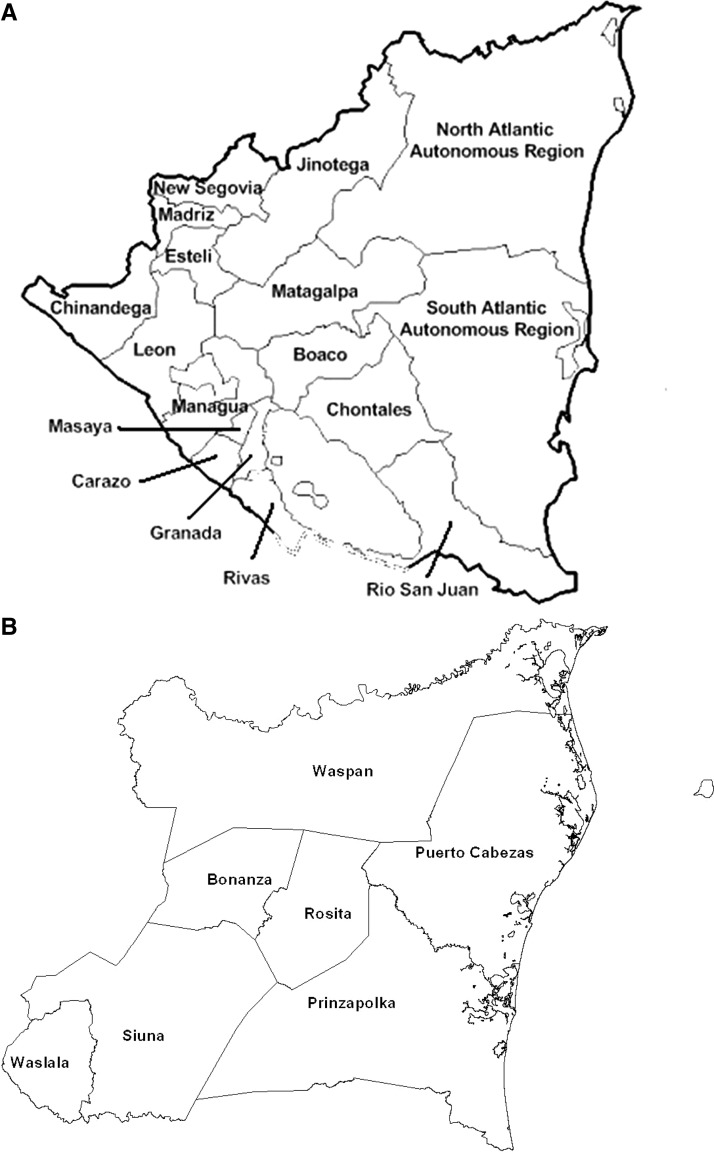
The 2005 drug efficacy trial was conducted in Siuna, Rosita, and Bonanza municipalities of NAAR, Nicaragua, during December 2005–February 2006 (Figure 1). Inclusion criteria were being a patient ≥ 6 months of age who had fever within the previous 48 hours, smear-confirmed P. falciparum mono-infection, and parasitemia < 100,000 asexual forms/μL. Patients were also selected based on their willingness to attend follow-up visits for 28 days and willingness to sign an informed consent form. Exclusion criteria were pregnancy or lactation (pregnancy test was performed for women of child-bearing age); signs of severe malaria, such as altered mental status or seizure within 24 hours of presentation; or excessive nausea and vomiting. Patients were also excluded for underlying chronic disease, alternative foci of infection or fever, or history of hypersensitivity or intolerance to CQ or SP.
Figure 1.
A, Map of Nicaragua showing study sites. B, Municpalities in the North Atlantic Autonomous Region of Nicaragua where the in vivo drug efficacy trial and surveillance studies were conducted.
The sample size for this study was determined by assuming a CQ and SP failure rate of 15% in a population of infinite size, a power of 80%, and significance level of 5%. A target sample size of 49 patients in each treatment arm of the group was calculated based on these parameters. A total of 27,500 patients with symptoms compatible with malaria came to the health facilities and participated in the 2005 drug efficacy trial. Of those patients, 687 were positive for P. vivax malaria and 147 were positive for P. falciparum malaria by microscopy. Among P. falciparum–infected patients, 136 had P. falciparum mono-infection. Of these patients, 58 met inclusion criteria, were randomly assigned to a study arm, and completed follow-up: 30 in the CQ arm and 28 in the SP arm (Table 1 ).
Table 1.
Characteristics of study participants enrolled in the in vivo drug efficacy study in the North Atlantic Autonomous Region, Nicaragua 2005–2006*
| Variable | CQ arm, n = 30 | SP arm, n = 28 |
|---|---|---|
| Median age, years (range) | 16 (8–23) | 8 (6–12) |
| Males (%) | 53.3 | 46.4 |
| Fever at admission, axillary temperature > 37.5°C (%) | 66.7 | 78.3 |
| Geometric mean parasite density at day 0, (parasites/μL) | 3,336.2 | 6,183.2 |
| Mean time to clear parasitemia, days | 2.8 | 2.6 |
CQ = chloroquine; SP = sulfadoxine-pyrimethamine. No early or late treatment failures were observed. Parasitemias did not develop in any of the participants during the follow-up period.
Blood smears were stained with 3% Giemsa for 30 minutes at room temperature and analyzed by experienced technicians. Parasite density was calculated per Pan American Health Organization–World Health Organization (PAHO-WHO) criteria assuming 6,000 leukocytes/μL. Pre-treatment blood spots were collected on day 0 by using Whatman (Brentford, United Kingdom) number 3 filter paper, and were dried and stored at −20°C until use for molecular analysis. Although blood spots were collected from all 58 enrolled patients on the day of enrollment, only 57 blood spots were available for molecular analysis. We were unable to extract DNA from four blood spots from Rosita, which left a maximum of 53 DNA isolates for analysis: 36 from Siuna and 17 from Rosita. No samples from Bonanza were available for inclusion in this study. The staffs conducting the molecular analysis of antimalarial resistance markers were blinded to the results of the drug efficacy trial.
The treatment schedule for the CQ arm of the study was 25 mg/kg of body weight divided into daily doses over three days: 10 mg/kg on day 1, 10 mg/kg on day 2, and 5 mg/kg on day 3. Sulfadoxine-pyrimethamine was given to the patients in the SP arm of the study at a single dose of 25 mg/kg of sulfadoxine and 1.25 mg/kg of pyrimethamine. Supervised treatment was administered to all patients, followed by clinical and parasitologic evaluation on days 0, 2, 3, 7, 14, 21, and 28. Therapeutic response was determined by using definitions described in the standard PAHO-WHO protocol.23 Of the 58 patients that completed follow-up, all responded clinically within 7 days of treatment and none showed development of parasitemia through day 28 of the study, indicating 100% drug efficacy in the CQ and SP arms.
The 2011 samples were collected as part of a national surveillance to confirm malaria cases identified in the primary health centers. The municipalities included in the study were Siuna, Rosita, Waspan, Bonanza, and Prinzapolka (Figure 1). Blood samples collected on Whatman number 3 filter paper for molecular analysis before antimalarial treatment was available. Forty-five samples confirmed to be P. falciparum based on 18S ribosomal RNA gene polymerase chain reactions (PCRs) were available in this study: 6 from Prinzapolka, 5 from Rosita, 18 from Siuna, 1 from Bonanza, and 15 from Waspan. Both studies were approved by the Ethical Board of Nicaraguan Ministry of Health and conducted according to the guidelines of PAHO.23
For molecular analysis, DNA was extracted from filter paper by using the QIAamp DNA Minikit (QIAGEN, Valencia, CA). These isolates were then used to determine the genotype of key codons implicated in CQ (pfcrt codons 72–76), sulfadoxine (dhps codons 436, 437, 540, 581, and 613), and pyrimethamine (dhfr codons 50, 51, 59, 108, and 164) resistance. Described primers and methods were used for the amplification of pfcrt24 and dhps.25 The dhfr gene fragment was amplified using a nested-PCR approach. The first round of PCR was carried out by using 5′-TCCTTTTTATGATGGAACAAG-3′ (F) and 5′-AGTATATACATCGCTAACAGA-3′(R) primers and the following cycling parameters: initial denaturation at 94°C for 5 minutes, followed by 35 cycles of denaturation at 95°C for 30 seconds, annealing at 50°C for 30 seconds, and extension at 68°C for 1 minute. This parameter was followed by a final extension at 68°C for 5 minutes. Secondary PCR was performed by using 5′-TTTATGATGGAACAAGTCTGC-3′ (F) and 5′- ACTCATTTTCATTTATTTCTGG-3′ (R) primers. The cycling parameters for the secondary reaction were the same as for primary reaction, except that the annealing temperature was set at 52°C for 30 seconds and number of cycles was reduced to 30. Sequencing of all gene fragments was conducted for both strands with their respective primers, following standard sequencing protocols, on an ABI 3130xl Genetic Analyzer (Applied Biosystems, Foster City, CA) and analyzed using DNA Star Lasergene software as described.24,25
Results
Of the 2005 drug efficacy study samples, 53 DNA samples were available for genetic analysis. All 53 samples were successfully amplified for pfcrt, 52 for pfdhfr, and 49 for pfdhps. All 45 isolates obtained from 2011 study collections were successfully amplified for pfcrt, pfdhfr, and pfdhps. Alleles were denoted by their amino acids in key positions for each gene. For pfcrt, the allele is described by amino acid positions 72, 73, 74, 75, and 76. For dhfr, the allele is described by amino acid positions 50, 51, 59, 108, 164. For, dhps the allele is described by amino acid positions 436, 437, 540, 581, and 613.
Most (96.2%, 51 of 53), of the total isolates examined in the 2005 sample set had the wild-type, CQ-sensitive pfcrt allele CVMNK (Table 2 ). A similar proportion (96.2%, 50 of 52) had the wild-type dhfr allele CNCSI and 97.9% (48 of 49) of the isolates examined had the wild-type dhps allele SAKAA. One isolate with the CQ resistance pfcrt allele CVIET was detected in Siuna. This isolate also had the N51I, C59R, and S108N polymorphisms in dhfr and the A437G polymorphism in dhps. One isolate that had a single S108N polymorphism in dhfr was also found in Siuna. However, this isolate had the wild-type pfcrt and dhps alleles (Table 3 ). The second isolate with a CQ resistance pfcrt allele found in Rosita was also CVIET. However, this isolate had the wild-type dhfr and dhps alleles. No SP resistance dhfr or dhps alleles were found in Rosita. All three of the patients with drug-resistant parasite genotypes noted above were enrolled in the CQ arm of the drug efficacy trial and were all successfully treated with CQ. In the 2011 surveillance study dataset, all 45 isolates from all locations examined had wild-type pfcrt, pfdhfr, and pfdhps gene loci.
Table 2.
Resistance allele frequencies in the in vivo drug efficacy study in the North Atlantic Autonomous Region, Nicaragua, 2005–2006*
| Gene (key positions) | Alleles | Municipality | Total, no. (%) | |
|---|---|---|---|---|
| Siuna, no. (%) | Rosita, no. (%) | |||
| pfcrt | CVMNK† | 35 (97.2) | 16 (94.1) | 51 (96.2) |
| (72, 73, 74, 75, 76) | CVIET | 1 (2.8) | 1 (5.9) | 2 (3.8) |
| Total | 36 | 17 | 53 | |
| pdhfr | CNCSI† | 33 (94.3) | 17 (100) | 50 (96.2) |
| (50, 51, 59, 108, 164) | CNCNI | 1 (2.85) | 0 (0) | 1 (1.9) |
| CIRNI | 1 (2.85) | 0 (0) | 1 (1.9) | |
| Total | 35 | 17 | 52 | |
| pdhps | SAKAA† | 35 (97.2) | 13 (100) | 48 (97.9) |
| (436, 437, 540, 581, 613) | SGKAA | 1 (2.8) | 0 (0) | 1 (2.1) |
| Total | 36 | 13 | 49 | |
Alleles are described by amino acids in key positions for each gene. Amino acid changes indicating polymorphism are underlined. pfcrt = Plasmodium falciparum chloroquine resistance transporter; pdhfr = P. falciparum dihydrofolate reductase; pdhps = P. falciparum dihydropteroate synthase.
Denotes wild-type allele.
Table 3.
Summary of parasite isolate genotypes containing resistance-associated alleles in the in vivo drug efficacy study in the North Atlantic Autonomous Region, Nicaragua 2005–2006*
| Isolate | Location | Allele | ||
|---|---|---|---|---|
| pfcrt | pdhfr | pdhps | ||
| Wild type | CVMNK | CNCSI | SAKAA | |
| Isolate 1 | Rosita | CVIET | CNCSI | SAKAA |
| Isolate 2 | Siuna | CVIET | CIRNI | SGKAA |
| Isolate 3 | Siuna | CVMNK | CNCNI | SAKAA |
Alleles described by amino acids in key positions for each gene as in Table 2. Amino acid changes indicating polymorphism are underlined. pfcrt = Plasmodium falciparum chloroquine resistance transporter; pdhfr = P. falciparum dihydrofolate reductase; pdhps = P. falciparum dihydropteroate synthase.
Discussion
Therapeutic efficacy of CQ and SP in Nicaragua was assessed in 2005–2006 as part of a drug efficacy trial; the results were reported to PAHO and WHO.23,26 In this study, we analyzed samples collected from this drug trial and a 2011 surveillance study to determine if there is any evidence for the presence of CQ- or SP-resistance alleles circulating in this region of Nicaragua. This effort is part of the Amazon Network for Monitoring Antimalarial Drug Resistance that is partially supported by the Amazon Malaria Initiative of the United States Agency for International Development. As the prevalence of P. falciparum malaria has decreased to low levels in Central America, this network has adopted molecular surveillance as a complementary approach for detecting early signs of emergence of drug-resistant parasites. However, it is well recognized that WHO-recommended in vivo drug efficacy trials are critical for policy changes. Our results indicate that wild-type CQ-sensitive pfcrt, pyrimethamine-sensitive pfdhfr, and sulfadoxine-sensitive pfdhps alleles are highly prevalent in the samples we tested. The 2005 drug efficacy trial showed only three parasite isolates containing resistance alleles, all of which were isolated from patients in the CQ arm of the study and who were successfully treated with CQ with no signs of therapeutic resistance. The 2011 surveillance study showed only wild-type alleles for all parasite isolates examined. These observations are consistent with reports of continued CQ and SP efficacy in Nicaragua and current national drug policy for treatment of P. falciparum malaria.
Limitations must be highlighted for these results to be viewed in the appropriate context. First, the sampling structures in the 2005 drug efficacy trial and the 2011 surveillance study were designed to assess therapeutic efficacy of antimalarial drugs and prevalence of malaria, respectively, in NAAR. Therefore, our results cannot be generalized to represent population-based prevalence of drug resistance polymorphisms in Nicaragua as a whole. Second, the DNA isolates were derived from blood spots; thus, in vitro assessments of CQ susceptibility were not feasible. Third, microsatellite analysis was not pursued because the low number of resistance alleles sampled herein would not permit a meaningful assessment of selection.
In the current study, we identified two isolates from the 2005 drug efficacy trial that had the pfcrt allele CVIET. One of these isolates also had the triple mutant pfdhfr allele CIRNI and single mutant pfdhps allele SGKAA. The CVIET pfcrt allele is common in Southeast Asia and Africa.27 Although the CVIET allele is not common in South America, rare occurrence has been reported in Brazil,28 Venezuela,7,13 and recently in Haiti.29 The study reporting CVIET alleles in Brazil found that the haplotypes for these isolates did not cluster spatially with isolates that had other pfcrt alleles, suggesting that they were recently introduced from abroad.28 A study conducted during 2008–2009 in Honduras showed no drug resistance pfcrt alleles in parasite isolates derived from local infections.30 Drug resistance pfcrt and dhfr alleles were identified in another study conducted in Honduras; however, it was determined that the infections harboring these resistance alleles were acquired in the Pacific and in West Africa.31 It cannot be confirmed if the parasite isolates containing the pfcrt CVIET, pfdhfr CIRNI allele, and pfdhps SGKAA alleles in this study were derived from imported cases of malaria.
Malaria transmission in Nicaragua has changed dramatically in recent years. The total number of malaria cases reported in Nicaragua decreased from 6,617 cases in 2005 to 236 cases in 2012.1 Because most of the P. falciparum malaria burden in Nicaragua occurs along the coast and the border with Honduras, control efforts focused in this region could help further reduce the P. falciparum malaria burden in Nicaragua. With such low levels of transmission, most of the Nicaraguan population will lack immunity to Plasmodium infection, making the region more prone to malaria epidemics after introduction of drug-resistant parasites, similar to what was seen in Panama in 2003.3 Therefore, if reports of CQ or SP therapeutic resistance or failure emerge, they must be addressed rapidly and aggressively to avoid selection and spread of highly resistant parasite pocket populations as described in other settings.32
Molecular surveillance continues to be a valuable tool for monitoring the emergence and spread of drug-resistant parasite isolates worldwide. However, the utility of these markers in correlating with in vivo antimalarial resistance varies on the basis of many factors, including local malaria transmission and immunity. Low transmission and absence of in vivo antimalarial resistance in Nicaragua mean that genotype resistance and genotype failure indices cannot be validated in this setting, as has been validated in other regions such as Mali.33 Given the progress that Nicaragua has made towards malaria elimination in many parts of the country and the low number of P. falciparum cases in the country, a directed molecular surveillance approach in areas such as NAAR and rest of the country with malaria transmission will be useful, as has been proposed for a molecular surveillance network in Mali.33
Nicaragua is an active partner in the Amazon Network for Monitoring Antimalarial Drug Resistance along with the collaboration of PAHO, and continued partnership in this network will enhance surveillance efforts to monitor emergence of CQ- and SP-resistant parasites in this region. A targeted and responsive molecular surveillance infrastructure can strengthen the overall malaria control program in areas at risk for epidemics by promptly determining if parasites harboring resistance alleles are being introduced or are circulating in the population. Nonetheless, parts of Nicaragua are prone to malaria epidemics. Therefore, ongoing monitoring of therapeutic efficacy with standardized methods and rigorous quality controls will remain as an important component of the overall strategy for making evidence-based policy considerations.
ACKNOWLEDGMENTS
We thank Dr. Francisco Acevedo and all the field staff who participated in conducting the clinical trial, members of the department of health of Gracias a Dios and of the Hospital of Puerto Lempira for assistance with sample collection, and Amanda Poe for help with laboratory work in sequencing some of the samples.
Footnotes
Financial support: This study was supported by the United States Agency for International Development under the Amazon Malaria Initiative, the Pan American Health Organization, the Network for Surveillance of Antimalarial Drug Resistance, the Ministry of Health of Nicaragua, and the Atlanta Research and Education Foundation (Decatur, GA). Sankar Sridaran was also partly supported by the Centers for Disease Control and Prevention Emerging Infectious Diseases Fellowship.
Authors' addresses: Sankar Sridaran, Case Western University School of Medicine, Cleveland, OH, E-mail: sxs973@case.edu. Betzabe Rodriguez, National Reference and Diagnosis Center, Ministry of Health, Managua, Nicaragua, E-mail: parasitología@minsa.gob.ni. Aida Mercedes Soto, Pan American Health Organization, Managua, Nicaragua, E-mail: sotoa@nic.ops-oms.org. Alexandre Macedo De Oliveira and Venkatachalam Udhayakumar, Malaria Branch, Centers for Disease Control and Prevention, Atlanta, GA, E-mails: acq7@cdc.gov and vxu0@cdc.gov.
References
- 1.World Health Organization . World Malaria Report, 2012. Geneva: World Health Organization; 2012. [Google Scholar]
- 2.World Health Organization . Global Strategic Plan 2005–2015. Geneva: Roll Back Malaria (RBM) Partnership; 2005. [Google Scholar]
- 3.Samudio F, Santamaria AM, Obaldia N, 3rd, Pascale JM, Bayard V, Calzada JE. Prevalence of Plasmodium falciparum mutations associated with antimalarial drug resistance during an epidemic in Kuna Yala, Panama, Central America. Am J Trop Med Hyg. 2005;73:839–841. [PubMed] [Google Scholar]
- 4.Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, Ursos LM, Sidhu AB, Naude B, Deitsch KW, Su XZ, Wootton JC, Roepe PD, Wellems TE. Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell. 2000;6:861–871. doi: 10.1016/s1097-2765(05)00077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Djimde A, Doumbo OK, Cortese JF, Kayentao K, Doumbo S, Diourte Y, Dicko A, Su XZ, Nomura T, Fidock DA, Wellems TE, Plowe CV, Coulibaly D. A molecular marker for chloroquine-resistant falciparum malaria. N Engl J Med. 2001;344:257–263. doi: 10.1056/NEJM200101253440403. [DOI] [PubMed] [Google Scholar]
- 6.Schneider AG, Premji Z, Felger I, Smith T, Abdulla S, Beck HP, Mshinda H. A point mutation in codon 76 of pfcrt of P. falciparum is positively selected for by chloroquine treatment in Tanzania. Infect Genet Evol. 2002;1:183–189. doi: 10.1016/s1567-1348(01)00021-1. [DOI] [PubMed] [Google Scholar]
- 7.Cortese JF, Caraballo A, Contreras CE, Plowe CV. Origin and dissemination of Plasmodium falciparum drug-resistance mutations in South America. J Infect Dis. 2002;186:999–1006. doi: 10.1086/342946. [DOI] [PubMed] [Google Scholar]
- 8.Wootton JC, Feng X, Ferdig MT, Cooper RA, Mu J, Baruch DI, Magill AJ, Su XZ. Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature. 2002;418:320–323. doi: 10.1038/nature00813. [DOI] [PubMed] [Google Scholar]
- 9.Cowman AF, Morry MJ, Biggs BA, Cross GA, Foote SJ. Amino acid changes linked to pyrimethamine resistance in the dihydrofolate reductase-thymidylate synthase gene of Plasmodium falciparum. Proc Natl Acad Sci USA. 1988;85:9109–9113. doi: 10.1073/pnas.85.23.9109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterson DS, Walliker D, Wellems TE. Evidence that a point mutation in dihydrofolate reductase-thymidylate synthase confers resistance to pyrimethamine in falciparum malaria. Proc Natl Acad Sci USA. 1988;85:9114–9118. doi: 10.1073/pnas.85.23.9114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reeder JC, Rieckmann KH, Genton B, Lorry K, Wines B, Cowman AF. Point mutations in the dihydrofolate reductase and dihydropteroate synthetase genes and in vitro susceptibility to pyrimethamine and cycloguanil of Plasmodium falciparum isolates from Papua New Guinea. Am J Trop Med Hyg. 1996;55:209–213. doi: 10.4269/ajtmh.1996.55.209. [DOI] [PubMed] [Google Scholar]
- 12.Basco LK, Eldin de Pecoulas P, Wilson CM, Le Bras J, Mazabraud A. Point mutations in the dihydrofolate reductase-thymidylate synthase gene and pyrimethamine and cycloguanil resistance in Plasmodium falciparum. Mol Biochem Parasitol. 1995;69:135–138. doi: 10.1016/0166-6851(94)00207-4. [DOI] [PubMed] [Google Scholar]
- 13.Contreras CE, Cortese JF, Caraballo A, Plowe CV. Genetics of drug-resistant Plasmodium falciparum malaria in the Venezuelan state of Bolivar. Am J Trop Med Hyg. 2002;67:400–405. doi: 10.4269/ajtmh.2002.67.400. [DOI] [PubMed] [Google Scholar]
- 14.Cortese JF, Plowe CV. Antifolate resistance due to new and known Plasmodium falciparum dihydrofolate reductase mutations expressed in yeast. Mol Biochem Parasitol. 1998;94:205–214. doi: 10.1016/s0166-6851(98)00075-9. [DOI] [PubMed] [Google Scholar]
- 15.Khalil I, Ronn AM, Alifrangis M, Gabar HA, Satti GM, Bygbjerg IC. Dihydrofolate reductase and dihydropteroate synthase genotypes associated with in vitro resistance of Plasmodium falciparum to pyrimethamine, trimethoprim, sulfadoxine, and sulfamethoxazole. Am J Trop Med Hyg. 2003;68:586–589. doi: 10.4269/ajtmh.2003.68.586. [DOI] [PubMed] [Google Scholar]
- 16.Sirawaraporn W, Sathitkul T, Sirawaraporn R, Yuthavong Y, Santi DV. Antifolate-resistant mutants of Plasmodium falciparum dihydrofolate reductase. Proc Natl Acad Sci USA. 1997;94:1124–1129. doi: 10.1073/pnas.94.4.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Urdaneta L, Plowe C, Goldman I, Lal AA. Point mutations in dihydrofolate reductase and dihydropteroate synthase genes of Plasmodium falciparum isolates from Venezuela. Am J Trop Med Hyg. 1999;61:457–462. doi: 10.4269/ajtmh.1999.61.457. [DOI] [PubMed] [Google Scholar]
- 18.Vasconcelos KF, Plowe CV, Fontes CJ, Kyle D, Wirth DF, Pereira da Silva LH, Zalis MG. Mutations in Plasmodium falciparum dihydrofolate reductase and dihydropteroate synthase of isolates from the Amazon region of Brazil. Mem Inst Oswaldo Cruz. 2000;95:721–728. doi: 10.1590/s0074-02762000000500020. [DOI] [PubMed] [Google Scholar]
- 19.Berglez J, Iliades P, Sirawaraporn W, Coloe P, Macreadie I. Analysis in Escherichia coli of Plasmodium falciparum dihydropteroate synthase (DHPS) alleles implicated in resistance to sulfadoxine. Int J Parasitol. 2004;34:95–100. doi: 10.1016/j.ijpara.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Triglia T, Menting JG, Wilson C, Cowman AF. Mutations in dihydropteroate synthase are responsible for sulfone and sulfonamide resistance in Plasmodium falciparum. Proc Natl Acad Sci USA. 1997;94:13944–13949. doi: 10.1073/pnas.94.25.13944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Triglia T, Wang P, Sims PF, Hyde JE, Cowman AF. Allelic exchange at the endogenous genomic locus in Plasmodium falciparum proves the role of dihydropteroate synthase in sulfadoxine-resistant malaria. EMBO J. 1998;17:3807–3815. doi: 10.1093/emboj/17.14.3807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.PAHO/WHO . Report on Situation of Malaria in Americas, 2008. Washington, DC: Pan American Health Organization, and Geneva: World Health Organzation; 2009. [Google Scholar]
- 23.PAHO/WHO . Generic Protocols and Flow Diagram for In Vivo Antimalarial Drug-Efficacy Studies in the Americas. 2003. http://www.paho.org/english/AD/DPC/CD/mal-antimalarials.htm Available at. Accessed June 3, 2010. [Google Scholar]
- 24.Griffing S, Syphard L, Sridaran S, McCollum AM, Mixson-Hayden T, Vinayak S, Villegas L, Barnwell JW, Escalante AA, Udhayakumar V. pfmdr1 amplification and fixation of pfcrt chloroquine resistance alleles in Plasmodium falciparum in Venezuela. Antimicrob Agents Chemother. 2010;54:1572–1579. doi: 10.1128/AAC.01243-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vinayak S, Alam MT, Mixson-Hayden T, McCollum AM, Sem R, Shah NK, Lim P, Muth S, Rogers WO, Fandeur T, Barnwell JW, Escalante AA, Wongsrichanalai C, Ariey F, Meshnick SR, Udhayakumar V. Origin and evolution of sulfadoxine resistant Plasmodium falciparum. PLoS Pathog. 2010;6:e1000830. doi: 10.1371/journal.ppat.1000830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization . Global Report on Antimalarial Efficacy and Drug Resistance: 2000–2010. Geneva: World Health Organization; 2010. [Google Scholar]
- 27.Wongsrichanalai C, Pickard AL, Wernsdorfer WH, Meshnick SR. Epidemiology of drug-resistant malaria. Lancet Infect Dis. 2002;2:209–218. doi: 10.1016/s1473-3099(02)00239-6. [DOI] [PubMed] [Google Scholar]
- 28.Vieira PP, Ferreira MU, Alecrim MG, Alecrim WD, da Silva LH, Sihuincha MM, Joy DA, Mu J, Su XZ, Zalis MG. pfcrt polymorphism and the spread of chloroquine resistance in Plasmodium falciparum populations across the Amazon Basin. J Infect Dis. 2004;190:417–424. doi: 10.1086/422006. [DOI] [PubMed] [Google Scholar]
- 29.Londono BL, Eisele TP, Keating J, Bennett A, Chattopadhyay C, Heyliger G, Mack B, Rawson I, Vely JF, Desinor O, Krogstad DJ. Chloroquine-resistant haplotype Plasmodium falciparum parasites, Haiti. Emerg Infect Dis. 2009;15:735–740. doi: 10.3201/eid1505.081063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mejia Torres RE, Banegas EI, Mendoza M, Diaz C, Bucheli ST, Fontecha GA, Alam MT, Goldman I, Udhayakumar V, Zambrano JO. Efficacy of chloroquine for the treatment of uncomplicated Plasmodium falciparum malaria in Honduras. Am J Trop Med Hyg. 2013;88:850–854. doi: 10.4269/ajtmh.12-0671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jovel IT, Mejia RE, Banegas E, Piedade R, Alger J, Fontecha G, Ferreira PE, Veiga MI, Enamorado IG, Bjorkman A, Ursing J. Drug resistance associated genetic polymorphisms in Plasmodium falciparum and Plasmodium vivax collected in Honduras, Central America. Malar J. 2011;10:376. doi: 10.1186/1475-2875-10-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maude RJ, Pontavornpinyo W, Saralamba S, Aguas R, Yeung S, Dondorp AM, Day NP, White NJ, White LJ. The last man standing is the most resistant: eliminating artemisinin-resistant malaria in Cambodia. Malar J. 2009;8:31. doi: 10.1186/1475-2875-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Djimde AA, Barger B, Kone A, Beavogui AH, Tekete M, Fofana B, Dara A, Maiga H, Dembele D, Toure S, Dama S, Ouologuem D, Sangare CP, Dolo A, Sogoba N, Nimaga K, Kone Y, Doumbo OK. A molecular map of chloroquine resistance in Mali. FEMS Immunol Med Microbiol. 2010;58:113–118. doi: 10.1111/j.1574-695X.2009.00641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]