Abstract
Objectives
To estimate the prevalence of daytime sleepiness and circadian preferences, and to examine the extent to which caffeine consumption and Khat (a herbal stimulant) use are associated with daytime sleepiness and evening chronotype among Ethiopian college students.
Methods
A cross-sectional study was conducted among 2,410 college students. A self-administered questionnaire was used to collect information about sleep, behavioral risk factors such as caffeinated beverages, tobacco, alcohol, and Khat consumption. Daytime sleepiness and chronotype were assessed using the Epworth Sleepiness Scale (ESS) and the Horne & Ostberg Morningness /Eveningness Questionnaire (MEQ), respectively. Linear and logistic regression models were used to evaluate associations.
Results
Daytime sleepiness (ESS≥10) was present in 26% of the students (95% CI: 24.4–27.8%) with 25.9% in males and 25.5% in females. A total of 30 (0.8%) students were classified as evening chronotypes (0.7% in females and 0.9% in males). Overall, Overall, Khat consumption, excessive alcohol use and cigarette smoking status were associated with evening chronotype. Use of any caffeinated beverages (OR=2.18; 95%CI: 0.82–5.77) and Khat consumption (OR=7.43; 95%CI: 3.28–16.98) increased the odds of evening chronotype.
Conclusion
The prevalence of daytime sleepiness among our study population was high while few were classified as evening chronotypes. We also found increased odds of evening chronotype with caffeine consumption and Khat use amongst Ethiopian college students. Prospective cohort studies that examine the effects of caffeinated beverages and Khat use on sleep disorders among young adults are needed.
Introduction
Sleep is a key component in maintaining one’s state of physical and mental well-being [1]. Good sleep has been associated with reduced risks of mental and social disorders, and can improve one’s overall productivity [2]. Achieving an ideal amount of sleep can be elusive for college students with demanding academic, social, and work commitments. The combination of these time intensive activities can result in fatigue and daytime sleepiness due to sleep deprivation [3]. In addition to changes in lifestyle, many college students also deal with novel challenges arising from changes of adolescent physiology such as a biologically driven delayed sleep phase [4]. These changes can impact an individual’s preferred sleep timing. Circadian preference can fall into two chronotypes: morning preference – those that naturally retire and arise early, and evening chronotype – those who prefer being active in the evenings [5]. Past work on daytime sleepiness, circadian preference and social jet lag (the difference between one’s natural sleep preference and the circadian cycle needed for daily responsibilities) has been primarily conducted in high-income countries (HICs). Such studies have indicated that students increase their consumption of caffeinated beverages, increase their multitasking habits, and use over the counter medications to adjust their sleep cycle to accommodate their academic, employment and social activities [2, 6]. Work by Cheng et al in Taiwan revealed the modulation of sleep patterns related to cigarette smoking, alcohol consumption, and excessive internet use [7]. A recent study among Ethiopian college students documented a high prevalence of caffeinated beverage consumption and an increased risk of poor sleep quality with consumption of such beverages [8]. In addition, Ethiopian students were shown to use Khat, a local herbal stimulant, and caffeine to manipulate their sleep patterns [9].
Caffeine, a widely used stimulant, can promote general wakefulness. Khat, also a stimulant, is an evergreen plant that has amphetamine-like metabolic effects is commonly used for social recreation and to improve work performance [10–12]. It has strong ties to Eastern African and middle-eastern cultures, and is used widely in Ethiopia [9, 13]. It is often used among college students and, like caffeine, Khat promotes wakefulness [12].
A number of biological mechanisms have been proposed through which stimulant use may lead to sleep disorders. One mechanism of how Khat may lead to sleep disorders stems from Khat’s active ingredient cathinone. The release of cathinone into the blood stream of an individual via chewing stimulates the central nervous system (CNS) of the user. Stimulation of the CNS promotes the release of dopamine, serotonin, noradrenaline, which result in the user feeling happy and energetic. The release of these neurochemicals also inhibits the sleep pathways of an individual. This, in turn, results in prolonged wakefulness and sleep disorders. [14]. Caffeinated beverages work in a similar manner by preventing adenosine, a sleep inducing chemical, from binding to receptors in the brain [8, 15]. The prolonging of one’s sleepless time via these stimulants could relate to having an evening chronotype and experiencing daytime sleepiness as the body is delayed in its endeavor to replenish itself via sleep.
In light of the increasing sleep problems among college students and the scarcity of epidemiologic studies evaluating the contribution of caffeinated beverages and Khat use on sleep disorders in sub-Saharan Africa, we conducted this study to evaluate the prevalence and distribution of daytime sleepiness and circadian preferences among Ethiopian college students. We further sought to examine the extent to which, if at all, caffeine consumption and Khat use are associated with daytime sleepiness and evening chronotype.
Methods and Materials
Study Population and Sampling
A cross-sectional study was conducted at the Universities of Gondar and Haramaya, Ethiopia between the months of November, 2010 and January, 2011. The study sampling procedures were previously described [8]. Briefly, a multistage sampling design by means of probability proportional to size (PPS) was used to select departments and all students from those departments were invited to participate. A total of 2,817 students who provided informed consent participated in the study. After excluding students with incomplete data on sleep disorders and caffeine use, a total of 2,410 students remained for analysis. The demographic (i.e. age and sex,) and lifestyle characteristics (i.e. caffeine use, khat use, smoking, alcohol consumption, and physical activity) of students included and excluded from the final analysis were similar. The procedures used in this study were approved by the institutional review boards of Addis Continental Institute of Public Health and Gondar University, Ethiopia and the University of Washington, USA. The Harvard School of Public Health Office of Human Research Administration, USA, granted approval to use the de-identified data for analysis.
Data Collection and Variables
A self-administered questionnaire was used to collect information for this study. The questionnaire ascertained demographic information including age, sex, and education level. Questions regarding behavioral risk factors, such as caffeinated beverages, tobacco, alcohol, and Khat consumption were also included. Participants’ anthropometric measurements including height, weight, waist, and hip circumference were taken by research nurses using standard protocols. Height and weight were measured without shoes or outerwear. Height was measured to the nearest 0.1 cm and weight was measured to the nearest 0.1 kg. All anthropometric values consisted of the mean of three measurements.
Epworth Sleep Scale (ESS)
The ESS is an 8-item questionnaire designed to capture an individual’s propensity to fall asleep during commonly encountered situations on a scale ranging from 0 to 3 [16]. The scores for the eight questions are added together to obtain a single total score that can range from 0 to 24. In adults, an ESS score ≥10 is taken to indicate increased daytime sleepiness [16]. The ESS has been widely used globally among different study populations including college students in sub-Saharan Africa [17, 18].
Morningness-Eveningness Questionnaire (MEQ)
Circadian preference was assessed using the Horne and Ostberg MEQ [19], a 19-item questionnaire that identifies morningness-eveningness preference. The scores range from 16 to 86 and participants can be classified in five categories: definite and moderate evening-type, neutral type, and moderate and definite morning-type. Higher values on MEQ indicate stronger morningness preference. In this study we used the following cut offs: (1) 16 to 30 for definite evening preference; (2) 31 to 41 for moderate evening preference; (3) 42 to 58 for intermediate preference; (4) 59 to 69 for moderate morning preference, and (5) 70 to 86 for morning preference.
Use of Caffeinated Beverages and Khat
Participants were first asked if they consumed any stimulant or caffeine containing beverages during the past week. Participants answering “yes” were further asked to identify the specific type of caffeinated beverages. These included coffee, espresso, spris (coffee mixed with tea), macchiato, cappuccino, Coke, and Pepsi. The questionnaire also ascertained information about current Khat consumption (no versus yes)
Other Covariates
Body mass index (BMI) was calculated as weight (kg)/height squared (m2). BMI thresholds were set according to the World Health Organization (WHO) protocol (underweight: <18.5 kg/m2; normal: 18.5–24.9 kg/m2; overweight: 25.0–29.9 kg/m2; obese≥30 kg/m2). We defined alcohol consumption as none (<1 alcoholic beverage a week), mild (1–7), moderate (1–19 alcoholic beverages a week), and high to excessive consumption (>19 alcoholic beverages a week). The other covariates included: age (years), sex, smoking history (never versus ever), and regular participation in moderate or vigorous physical activity (no versus yes).
Data Analysis
We first explored frequency distributions of socio-demographic and behavioral characteristics of study subjects. Continuous variables were expressed as mean ± standard deviation. Student’s t-tests were used to evaluate the difference in mean values of MEQ and ESS scores across socio-demographic and lifestyle characteristics. Multiple linear regression models were also used to evaluate the relationship between socio-demographic and lifestyle characteristics and ESS and MEQ scores. Categorical variables were expressed as counts and percentages. Chi-squared tests were used to evaluate the differences in the distribution of categorical variables for study groups. Prevalence estimates of evening chronotype and daytime sleepiness across age and sex were reported. Using previously described methods, 95% confidence intervals (95% CIs) for prevalence estimates were determined [20]. Multivariate logistic regression models were used to estimate odds ratios (ORs) and 95% CIs for daytime sleepiness and evening chronotype according to use and non-use of stimulants. All statistical analyses were performed using SPSS (version 21.0, IBM SPSS Inc. Chicago, IL, USA). All reported p-values are two tailed and confidence intervals are calculated at the 95% confidence level.
Results
Amongst the 2,410 students (mean age = 21.66±1.70 years) included in this study, three-fourths were males (76.5%), fewer than 4% of students reported smoking cigarette, and 13% reported alcohol usage. None of the study participants were found to be obese, while 1.4% of them were in the overweight range, and 38.9% fell in the underweight BMI category. One-third of the population (28%) reported little to no moderate or vigorous physical (Table 1).
Table 1.
Characteristics of Study Sample
| Characteristic | N=2,410 n |
% |
|---|---|---|
| Age (Mean± SD) | 21.66±1.70 | |
| Age (years) | ||
| 18–19 | 122 | 5.1 |
| 20 | 494 | 20.5 |
| 21 | 665 | 27.6 |
| ≥ 22 | 1,129 | 46.8 |
| Sex | ||
| Male | 1,844 | 77.6 |
| Female | 533 | 22.4 |
| Cigarette smoking status | ||
| Never | 2,323 | 96.4 |
| Former | 12 | 0.5 |
| Current | 75 | 3.1 |
| Caffeinated beverage consumption | ||
| No | 465 | 19.4 |
| Yes | 1,938 | 80.6 |
| Alcohol consumption | ||
| <1 drink/month | 2,075 | 86.1 |
| 1–7 drinks/month | 237 | 9.8 |
| 8–19 drinks/month | 68 | 2.8 |
| ≥ 20 drinks/month | 30 | 1.3 |
| Body mass index (kg/m2) | ||
| Underweight (<18.5) | 938 | 39.0 |
| Normal (18.5–24.9) | 1,432 | 59.6 |
| Overweight (25.0–29.9) | 33 | 1.4 |
| Khat consumption | ||
| No | 1,895 | 89.5 |
| Yes | 223 | 10.5 |
| Any physical activity | ||
| No | 637 | 27.9 |
| Yes | 1,643 | 72.1 |
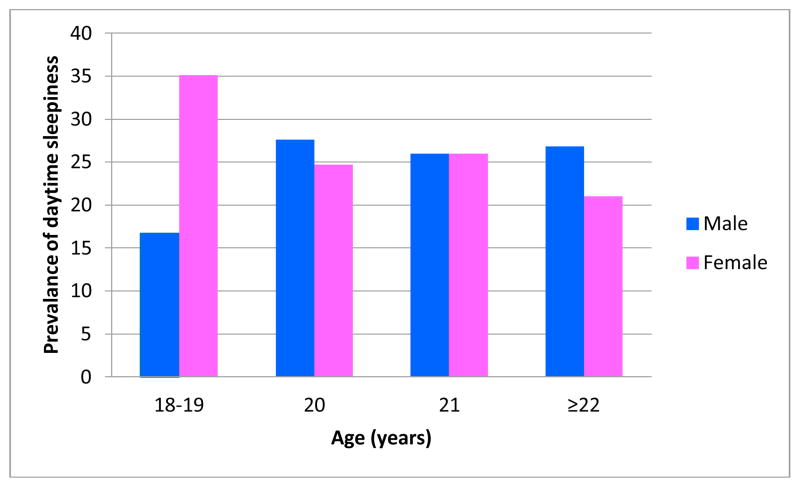
Overall, daytime sleepiness (ESS≥10) was present in 26.1% of the students (95% CI: 24.4–27.8). The prevalence of daytime sleepiness was relatively evenly distributed across age groups and sex, except for the 18–19 age group where over 30% of female respondents indicated daytime sleepiness while only 18% of males indicated similar characteristics (Figure 1).
Figure 1.
Prevalence of Daytime Sleepiness According to Age and Sex
A total of 30 (0.8%) students were classified as evening chronotypes (0.7% in females and 0.9% in males) while the majority of students reported behaviors that indicated morning type or intermediate type preference (Table not shown). There was no statistically significant difference in distribution of morning and evening chronotypes between males and females.
Summary statistics of ESS scores by demographic and lifestyle characteristics are presented in Table 3. Mean ESS scores were not statistically significantly associated with demographic and lifestyle characteristics of participants. Likewise, summary statistics of MEQ scores by demographic and lifestyle characteristics are presented in Table 4. Overall, mean MEQ scores were found to be significantly associated with age, cigarette smoking, alcohol consumption, and Khat use.
Table 3.
Morningness /Eveningness Questionnaire (MEQ) Scores According to Demographic and Lifestyle Characteristics
| Covariate |
MEQ Score
|
p-value | |
|---|---|---|---|
| Mean | SD | ||
| Age (years) | |||
| 18–19 | 53.96 | 6.57 | <0.001 |
| 20 | 55.69 | 6.51 | |
| 21 | 55.85 | 5.84 | |
| ≥ 22 | 56.39 | 6.32 | |
| Sex | |||
| Male | 56.06 | 6.29 | 0.117 |
| Female | 55.58 | 6.18 | |
| Cigarette smoking status | |||
| Never | 56.13 | 6.19 | <0.001 |
| Former | 52.50 | 6.82 | |
| Current | 51.61 | 6.73 | |
| Caffeinated beverage consumption | |||
| No | 57.18 | 6.41 | <0.001 |
| Yes | 55.68 | 6.19 | |
| Alcohol consumption | |||
| <1 drink/month | 56.16 | 6.17 | <0.001 |
| 1–7 drinks/month | 55.78 | 6.19 | |
| 8–19 drinks/month | 52.95 | 7.64 | |
| ≥ 20 drinks/month | 51.53 | 6.70 | |
| Khat consumption | |||
| No | 56.26 | 6.20 | <0.001 |
| Yes | 53.50 | 6.69 | |
| Body mass index (kg/m2) | |||
| Underweight (<18.5) | 55.84 | 6.32 | 0.271 |
| Normal (18.5–24.9) | 56.11 | 6.21 | |
| Overweight (25.0–29.9) | 54.61 | 6.91 | |
| Any physical activity | |||
| No | 56.03 | 6.48 | 0.702 |
| Yes | 55.92 | 6.17 | |
Table 4.
Evening Chronotype and Daytime Sleepiness in Relation to Stimulant Use
| Evening Chronotype
|
Daytime Sleepiness
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Morning N=868 |
Evening N=30 |
Unadjusted OR (95% CI) |
Adjusted* OR (95% CI) |
No N=1,702 |
Yes N=594 |
Unadjusted OR (95% CI) |
Adjusted* OR (95% CI) |
|
| Caffeinated beverages | % | % | % | % | ||||
| No | 98.1 | 1.9 | 1.00 (Reference) | 1.00 (Reference) | 72.2 | 27.8 | 1.00 (Reference) | 1.00 (Reference) |
| Yes | 96.0 | 4.0 | 2.18 (0.82–5.77) | 2.21 (0.83–5.87) | 74.8 | 25.2 | 0.87 (0.71–1.08) | 0.86 (0.69–1.06) |
| Khat consumption | ||||||||
| No | 97.5 | 2.5 | 1.00 (Reference) | 1.00 (Reference) | 74.6 | 25.7 | 1.00 (Reference) | 1.00 (Reference) |
| Yes | 84.1 | 15.9 | 7.43 (3.28–16.98) | 7.30 (3.08–17.32) | 74.7 | 25.3 | 0.98 (0.71–1.35) | 0.94 (0.64–1.39) |
Adjusted for age, sex, BMI, smoking, alcohol consumption, and physical activity
As shown in Table 5, there was no evidence of an association between consumption of caffeinated beverages and evening chronotype (OR=2.21; 95%CI: 0.83–5.87). However, current Khat consumption was associated with a 7-fold increased odds of evening chronotype (OR=7.30; 95%CI: 3.07–17.32). No statistically significant associations were noted for Khat use or caffeinated beverages with daytime sleepiness.
Discussion
Daytime sleepiness (ESS≥10) was present in 26% of the students (95% CI: 24.4–27.8%) with 25.9% of males and 25.5% of females reporting daytime sleepiness. A total of 30 (0.8%) students were classified as evening chronotypes (0.7% in females and 0.9% in males). Overall, Khat consumption, excessive alcohol use and cigarette smoking status were associated with evening chronotype.
Overall, our study findings are in agreement with previously reported prevalence estimates of daytime sleepiness amongst young adults and students in both HICs low-and middle-income countries (LMICs) [5, 21, 22]. For instance, Digdon reported a 19.3% to 45.5% prevalence of daytime sleepiness amongst students in Canada [21]. Other studies from HICs have reported similar prevalence estimates [23, 24]. Similar prevalence estimates have been reported in emerging economies. For instance Schneider et al [25], in their study of Brazilian college students, reported that 50.8% of students were daytime sleepers, while Chung et al [26] reported 42% daytime sleepiness in their study among Hong Kong Chinese Adolescents. Italian investigators have reported prevalence estimates of daytime sleepiness ranging from 13.7% to 16.6% [22]. The prevalence of daytime sleepiness in our study is lower than estimated reported for students in Estonia, China, and Brazil [25, 26]. Our estimates, however, are higher than estimates reported for students in Italy and Germany [27]. Collectively, despite variations in data collection methodologies, socio-demographic and lifestyle characteristics of study subjects, daytime sleepiness amongst young adults is a prevalent and growing problem across the globe.
Studies assessing sleep patterns of college students have documented high prevalence of evening chronotype [5, 21–23, 28]. Our study finding of a 0.8% prevalence of evening chronotype is lower than previously reported values [5, 21–23, 28]. Roeser et al, in their study of German students, reported a 34.1% prevalence of evening chronotype [23]. Similarly, other investigators have reported 34.3% evening chronotype amongst Canadian students while Giannotti et al reported 11.1% eveningness amongst Italian students [21, 22]. In Brazil, 39.3% of respondents indicated an evening preference [5]. We do not have a clear explanation for the varying estimates of evening chronotype across study settings. The Horne & Östberg MEQ used in our study might not have a comprehensive cross-cultural applicability to our student population in Eastern Africa. Evaluating the validity of the instrument using classical and contemporary psychometric methods is warranted. To the best of our knowledge this is the first study to evaluate chronotype amongst African college students. It is possible that the MEQ used in our study might exclude factors necessary for determining chronotype in an African context [28]. The concordance of our ESS results with those from other studies that have included racially, ethnically and geographically diverse population [5, 21–24], however, serve to attenuate these concerns. It also important to note that sleeping environment of college students might play an important role on chronotype. In our student population, the majority of students live in dormitory rooms. Future studies need to evaluate the effect of sleeping environment on chronotype among colleges students.
We expected stimulant usage (caffeine and Khat) to be associated daytime sleepiness and evening chronotype. Only Khat consumption showed a strong association with evening chronotype; those who reported using Khat had 7-fold higher odds of evening chronotype. This association is statistically imprecise (as reflected by the wide 95% CI), due to the relatively small number of students identified as evening chronotypes. Khat is typically consumed in social settings. Investigators have reported that the average Khat usage session lasts between 2.5 to 3 hours [29]. The time used to consume Khat such social settings prolongs evening activities, delays user’s sleep and decreases their overall productivity [11, 30, 31]. Investigators also note that Khat is often used while studying because of its amphetamine-like stimulatory effects, however, psychosis and delusions are also known to be triggered by long term usage [12].
We did not observe clear evidence of an association of caffeinated beverage consumption with evening chronotype. We submit that this null observation should be interpreted in light of our relatively low statistical power for that analysis (i.e., there were only 30 students classified as having evening chronotypes). Traditionally, coffee is consumed in Ethiopian as part of social event involving intensive social interactions and engagements. Typical work and school days in Ethiopia include regularly scheduled coffee/tea breaks; and the traditional coffee ceremony is widely practiced amongst Ethiopians of all social and economic backgrounds. In the collegiate setting caffeinated beverages are also incorporated into students’ study regime; and this specific late evening consumption may prolong delay bedtime and promote chronic sleep debt and circadian misalignment. Recently, there has been an increased use of energy drinks with higher levels of caffeine. This is particularly true in middle income countries such as Thailand [32]. As adoption of these products increases amongst Ethiopians, we may expect to see worsening sleep patterns and increased daytime sleepiness and evening chronotype in this population.
The findings of our study should be interpreted in light of some study limitations. First, given the cross-sectional nature of our study, it is difficult to delineate whether daytime sleepiness or evening chronotypes are a result of alcohol consumption, smoking status, and Khat usage, or whether these lifestyle characteristics resulted as a way to cope with the effects of social jet lag. Second, we did not use random sampling. Rather, we considered subjects who were willing to participate in the study, thus our findings may be subject to volunteer bias. In addition, social desirability bias may have contributed to some degree of errors in reporting stimulant use.
Finally, our use of a self-administered survey that relied on subjective measures of sleep disorders and other covariates may have introduced some degree of error in reporting. Future studies that use objective measurements of sleep disorders will be needed to more thoroughly assess their association with stimulant usage.
In conclusion, the prevalence of daytime sleepiness among our study population was high and ultimately adds to the limited data in sub-Saharan Africa. Our study also showed an increased evening chronotype with consumption of Khat amongst Ethiopian college students. Large well-designed prospective cohort studies that allow for the comprehensive examination of caffeinated beverages and Khat consumption in relation to sleep disorders among young adults are warranted. Enhanced understanding of the epidemiology of stimulant use and sleep disorders is expected to provide important information that can be used to design health promotion and disease prevention activities amongst Ethiopian adolescents and college students.
Table 2.
Epworth Sleepiness Scale (ESS) Scores According Demographic and Lifestyle Characteristics
| Covariates |
EES Score
|
p-value | |
|---|---|---|---|
| Mean | SD | ||
| Age (years) | |||
| 18–19 | 7.28 | 3.56 | 0.980 |
| 20 | 7.29 | 3.75 | |
| 21 | 7.22 | 3.48 | |
| ≥ 22 | 7.29 | 3.49 | |
| Sex | |||
| Male | 7.27 | 3.54 | 0.877 |
| Female | 7.30 | 3.56 | |
| Cigarette smoking status | |||
| Never | 7.28 | 3.54 | 0.446 |
| Former | 8.27 | 2.69 | |
| Current | 6.92 | 3.71 | |
| Alcohol consumption | |||
| <1 drink/month | 7.22 | 3.51 | 0.110 |
| 1–7 drinks/month | 7.50 | 3.63 | |
| 8–19 drinks/month | 7.21 | 4.04 | |
| ≥ 20 drinks/month | 8.67 | 4.05 | |
| Caffeinated beverage consumption | |||
| No | 7.24 | 3.76 | 0.680 |
| Yes | 7.25 | 3.49 | |
| Khat consumption | |||
| No | 7.26 | 3.51 | 0.737 |
| Yes | 7.18 | 3.60 | |
| Body mass index (kg/m2) | |||
| Underweight (<18.5) | 7.25 | 3.53 | 0.460 |
| Normal (18.5–24.9) | 7.27 | 3.56 | |
| Overweight (25.0–29.9) | 8.03 | 3.16 | |
| Any physical activity | |||
| No | 7.32 | 3.68 | 0.747 |
| Yes | 7.27 | 3.48 | |
Acknowledgments
D. R. was a research training fellow with the Multidisciplinary International Research Training (MIRT) Program of the Harvard University School of Public Health when this research study was completed. The Multidisciplinary International Research Program is supported by an award from the National Institutes of Health, National Institute on Minority Health and Health Disparities (T37-MD000149). The authors thank Addis Continental Institute of Public Health for providing facilities and logistic support throughout the research process.
References
- 1.Oginska H, Pokorski J. Fatigue and mood correlates of sleep length in three age-social groups: School children, students, and employees. Chronobiol Int. 2006;23:1317–28. doi: 10.1080/07420520601089349. [DOI] [PubMed] [Google Scholar]
- 2.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124–32. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Teixeire L, Lowden A, Aparecida da Luz A, Turte SL, Valente D, Matsumura RJ, Pickersgill de Paula L, Takara MY, Magai-Manelli R, Fischer FM. Sleep patterns and sleepiness of working college students. Work. 2012;10:5550–2. doi: 10.3233/WOR-2012-0879-5550. [DOI] [PubMed] [Google Scholar]
- 4.Gupta R, Bhatia MS, Chhabra V, Sharma S, Dahiya D, Semalti K, Sapra R, Dua RS. Sleep patterns of urban school-going adolescents. Indian J Pediatr. 2008;45:183–9. [PubMed] [Google Scholar]
- 5.Schneider LDM, Vasconcellos DC, Dantas G, Levandovski R, Caumo W, Allebrandt KV, Doring M, Hidalgo MPL. Morningness-evingness, use of stimulants and minor psychiatric disorder among undergraduate students. Int J Psychol. 2011;42:6. doi: 10.1080/00207594.2010.513414. [DOI] [PubMed] [Google Scholar]
- 6.Forquer LM, Camden AE, Gabriau KM, Johnson CM. Sleep patterns of college students at a public university. J Am Coll Health. 2008;56:563–5. doi: 10.3200/JACH.56.5.563-565. [DOI] [PubMed] [Google Scholar]
- 7.Cheng SH, Shih CC, Lee IH, Hou YW, Chen KC, Chen KT, Yang YK, Yang YC. A study on the sleep quality of incoming university students. Psychiatry Res. 2012;197:270–4. doi: 10.1016/j.psychres.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Lemma S, Patel SV, Tarekegn YA, Tadesse MG, Berhane Y, Gelaye B, Williams MA. The Epidemiology of Sleep Quality, Sleep Patterns, Consumption of Caffeinated Beverages, and Khat Use among Ethiopian College Students. Sleep Disord. 2012:583510. doi: 10.1155/2012/583510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alem A, Shibre T. Khat induced psychosis and its medico-legal implication: a case report. Ethiop Med J. 1997;35:137–9. [PubMed] [Google Scholar]
- 10.Belew M, Kebede D, Kassaye M, Enquoselassie F. The magnitude of khat use and its association with health, nutrition and socio-economic status. Ethiop Med J. 2000;38(1):11–26. [PubMed] [Google Scholar]
- 11.Kalix P. Khat: scientific knowledge and policy issues. Br J Addict. 1987;82(1):47–53. doi: 10.1111/j.1360-0443.1987.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 12.Kassim S, Croucher R, Al’Absi M. Khat dependence syndrome: A cross sectional preliminary evaluation amongst UK-resident Yemeni khat chewers. J Ethnopharmacol. 2012:146. doi: 10.1016/j.jep.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Kebede D, Alem A, Mitike G, Enqueselassie F, Berhane F, Abebe Y, Ayele R, Lemma W, Assefa T, Gebremichael T. Khat and alcohol use and risky sex behavior among in-school and out-of-school youth in Ethiopia. BMC Publi Health. 2005:5. doi: 10.1186/1471-2458-5-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colzato LS, Ruiz MJ, van den Wildenberg WPM, Hommel B. Khat Use Is Associated with Impaired Working Memory and Cognitive Flexibility. PLoS ONE. 2011;6(6):e20602. doi: 10.1371/journal.pone.0020602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.William W, Fapa I, Ugochukwu C, Bagot K, Khalili D, Zaky C. ENERGY DRINKS: Psychological Effects and Impact on Well-being and Quality of Life—A Literature Review. Innovative Clinical Neuroscience. 2012;9(1):9. [PMC free article] [PubMed] [Google Scholar]
- 16.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 17.Adewole OO, Adeyemo H, Ayeni F, Anteyi EA, Ajuwon ZO, Erhabor GE, Adewole TT. Prevalence and correlates of snoring among adults in Nigeria. African Health Sciences. 2008;8:108–13. [PMC free article] [PubMed] [Google Scholar]
- 18.Adewole OO, Hakeem A, Fola A, Anteyi E, Ajuwon Z, Erhabor G. Obstructive sleep apnea among adults in Nigeria. J Natl Med Assoc. 2009;101:720–5. doi: 10.1016/s0027-9684(15)30983-4. [DOI] [PubMed] [Google Scholar]
- 19.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97. [PubMed] [Google Scholar]
- 20.Brown L, Cai T, DasGupta A. Interval Estimation for a Binomial Proportion. Statistical Science. 2001;16(2):32. [Google Scholar]
- 21.Digdon NL, Rhodes S. Methods used to cope with sleepiness may perpetuate sleepiness in college students with an evening type circadian preference. Biol Rhythm Res. 2009;40:129–44. [Google Scholar]
- 22.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 23.Roeser K, Schlarb AA, Kübler A. The Chronotype-Academic Performance Model (CAM): Daytime sleepiness and learning motivation link chronotype and school performance in adolescents. Pers Individ Dif. 2013;54:836–40. [Google Scholar]
- 24.Veldi M, Aluoja A, Vasar V. Sleep quality and more common sleep-related problems in medicial students. Sleep Med. 2005;6:6. doi: 10.1016/j.sleep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Schneider ML, Vasconcellos DC, Dantas G, Levandovski R, Caumo W, Allebrandt KV, Doring M, Hidalgo MP. Morningness-eveningness, use of stimulants, and minor psychiatric disorders among undergraduate students. Int J Psychol. 2011;46:18–23. doi: 10.1080/00207594.2010.513414. [DOI] [PubMed] [Google Scholar]
- 26.Chung KF, Cheung MM. Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep. 2008;31:185–94. doi: 10.1093/sleep/31.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 28.Caci H, Adan A, Bohle P, Natale V, Pornpitakpan C, Tilley A. Transcultural Properties of the composite scale of morningness: the revalance of the “morning affect” factor. Chronobiology international. 2005;22:17. doi: 10.1081/CBI-200062401. [DOI] [PubMed] [Google Scholar]
- 29.Yeshigeta G, Abraham HA. Khat chewing and its socio-demographic correlates among the staff of Jimma University. Ethiopian Journal of Health Development. 2004;18:179–84. [Google Scholar]
- 30.Cox G, Rampes H. Adverse effects of khat: a review. Adv Psychiatr Treat. 2003;9:456–63. [Google Scholar]
- 31.Hoffman R, Al’Absi M. Khat use and neurobehavioral functions: suggestions for future studies. J Ethnopharmaco. 2010;132:554–63. doi: 10.1016/j.jep.2010.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lohsoonthorn V, Khidir H, Casillas G, Lertmaharit S, Tadesse MG, Pensuksan WC, Rattananupong T, Gelaye B, Williams MA. Sleep quality and sleep patterns in relation to consumption of energy drinks, caffeinated beverages, and other stimulants among Thai college students. Sleep Breath. 2012;17:1017–28. doi: 10.1007/s11325-012-0792-1. [DOI] [PMC free article] [PubMed] [Google Scholar]