Abstract
In 2006, the US Centers for Disease Control and Prevention issued recommendations supporting routine HIV testing in health care settings for all persons aged 13 to 64 years. Despite these recommendations, physicians are not offering HIV testing routinely. We apply a model that has previously identified 3 central, inter-related factors (knowledge-, attitude-, and behavior-related barriers) for why physicians do not follow practice guidelines in order to better understand why physicians are not offering HIV testing routinely. This model frames our review of the existing literature on physician barriers to routine HIV testing. Within the model, knowledge barriers include lack of familiarity or awareness of clinical recommendations, attitude barriers include lack of agreement with guidelines, while behavioral barriers include external barriers related to the guidelines themselves, to patients, or to environmental factors. Our review reveals that many physicians face these barriers with regards to implementing routine HIV testing. Several factors underscore the importance of determining how to best address physician barriers to HIV testing, including: provisions of the Affordable Care Act that are likely to require or incentivize major payers to cover HIV testing, evidence which suggests that a physician’s recommendation to test for HIV is a strong predictor of patient testing behavior, and data which reveals that nearly 20% of HIV-positive individuals may be unaware of their status. In April 2013, the US Preventive Services Task Force released a recommendation supporting routine HIV testing; strategies are needed to help address ongoing physician barriers to testing.
Keywords: HIV testing, guidelines, physician, CDC, USPSTF
HIV Testing Recommendations and Policies
In April 2013, the US Preventive Services Task Force (USPSTF) released a recommendation for routine testing of all adolescents and adults aged 15 to 65 years.1 Notably, in 2006, the US Centers for Disease Control and Prevention (CDC) issued recommendations supporting routine HIV testing for all persons aged 13 to 64 years.2 Since then, several professional medical organizations have issued policy statements supporting routine HIV testing.3–6 Although modest improvements in national HIV testing prevalence have been made since 2006, HIV testing prevalence has been decreasing since 2010 (Figure 1). Nearly 1 in 5 people with HIV still remain unaware of their HIV-positive status8 because they have not yet been tested, and nearly a third of those tested for HIV are diagnosed late—near the onset of AIDS.9 While gains have been made in HIV testing, the inconsistent adoption of the 2006 CDC HIV testing recommendations by primary care providers has held back more universal efforts to improve routine HIV testing in the United States. A 2012 national survey found that more than 40% of those surveyed have never talked with a doctor or health care provider about HIV or AIDS.10 It is also important to note that the CDC and USPSTF recommendations apply broadly to clinical settings; nurses and other providers are increasingly providing primary care and will undoubtedly play a role in the future of expanding HIV testing programs and adherence to these recommendations. However, data suggest that the recommendation of a physician in particular can and does play a unique and strong role in an individual’s decision to get tested.10–16 As such, this article focuses on physicians’ barriers to HIV testing. A letter by the HIV Testing Reimbursement Subcommittee of the HIV Health Care Access Working Group (affiliated with the Federal AIDS Policy Partnership) states that “due to the provisions of the [Affordable Care Act], all major payers will be either required to or incentivized to cover HIV Testing.”17(pl) Furthermore, a recent study suggests providers are much more willing to provide HIV testing services when reimbursement is offered.18 This again emphasizes how critical it is to understand the barriers that have thus far limited more universal physician-led implementation of routine HIV testing.
Figure 1.
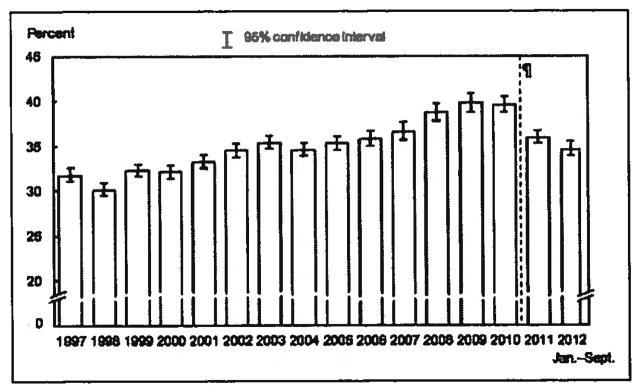
Percentage of adults aged 18 years and older who had ever been tested for HIV: United States, January 1997 to September 2012.7
Methods
An Internet search through both Google Scholar and PubMed was conducted for literature related to HIV testing guidelines, physician adherence to HIV testing guidelines, and physician barriers to HIV testing. Literature was also gathered from the HIV Literature ListServ released by Dr Robert Malow, a well-known resource within the field of HIV/AIDS research. We excluded articles related to HIV testing exclusively in prenatal, pediatric, and/or emergency settings, instead focusing on articles that revealed information about HIV testing and guidelines in and for adult primary care settings. Although adolescents and pregnant women are within the age-group addressed by the recommendations, our focus was to assess the state of and adherence and barriers to testing uniquely in adult primary care settings. We excluded non-US–based studies since physicians in other countries may face different and unique barriers.
Are Primary Care Providers Offering HIV Tests in the Routine Testing Era?
Despite the 2006 CDC HIV testing recommendations and support from several physicians’ organizations, physicians are still not offering HIV testing routinely. In the following section, we review data collected from physician surveys on the frequency of HIV testing after the release of the 2006 CDC HIV testing recommendations. In a 2007 survey of New York city internal medicine resident physicians, only 35.8% of participants reported routinely testing their patients in line with the 2006 CDC recommendations.19 This study also found that 64.2% of participants still used risk-based testing—an approach no longer universally recommended by the 2006 CDC recommendations. In a 2007 San Francisco study of medical providers, only 20.3% of participants reported offering routine HIV testing to all patients.20 In a 2009 study of general internists, respondents reported HIV testing in only a median 2% of patients they had seen in the previous 30 days.21 Additionally, only 52.3% of participants reported increasing routine HIV testing since revised CDC recommendations were published. In a 2007 to 2009 retrospective review of San Francisco Department of Public Health data, only 9.6% to 15.1% of patients were tested for HIV from 2007 to 2009.22 This study also found that no clinic reported to have formally implemented the CDC recommendations to offer routine HIV testing to every patient aged 13 to 64 years. A 2009 study of internal medicine physicians found that only 63.3% of respondents reported that they test patients for HIV regardless of risk factors.23 In the same survey, physicians reported that only 37.4% of participants practice in clinics that have screened more than 25% of its patients. In a 2010 study of internal medicine physicians at the University of Cincinnati Academic Health Center, only 29.2% of internal medicine physicians reported routinely offering HIV testing.24 In a 2011 study of Health Resources and Services Administration (HRSA)-funded health center sites, survey responses showed that several health center sites had not fully adopted all 4 practices recommended by CDC for routine HIV testing.25
Barriers to Guideline and Recommendation Implementation
Despite the 2006 CDC HIV testing recommendations being intended to allay previously recognized HIV testing barriers, research shows that physicians still face barriers to routine HIV testing. Cabana et al26 have identified 3 central and interrelated factors for why physicians do not follow practice guidelines (Figure 2); these factors may help explain why physicians are not offering HIV testing routinely. According to the Cabana model, knowledge, attitudes, and behavioral skills are individual and interacting factors that affect physicians’ behaviors.26 Our literature review has grouped study findings into these categories in order to provide a more theoretical framework for studying barriers to routine HIV testing. According to the Cabana model, “A physician may still encounter barriers that limit his/her ability to perform the recommended behavior due to patient, guideline, or environmental factors.”26(pl462) Within the model, there is acknowledgment that there are barriers that exist externally to the provider. This review specifically focused on physician-level barriers involving categories as defined by Cabana for knowledge, attitudes, and behaviors.
Figure 2.
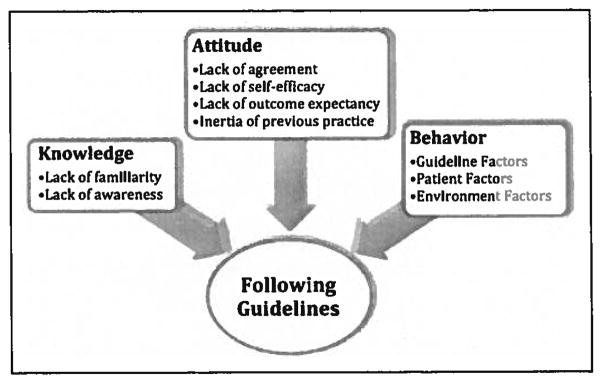
Primary care provider barriers to adherence to practice guidelines, adapted from Cabana et al.26
HIV Testing Barriers: Knowledge
According to Cabana et al,26 knowledge barriers include lack of familiarity or lack of awareness of clinical recommendations. A 2007 study of New York city internal medicine resident physicians found that only 32.6% of respondents were aware of the 2006 testing recommendations.19 Another 2007 study of primary care providers at a San Francisco public hospital found that only 31.5% knew of the updated CDC recommendations.20 A 2007 to 2009 San Francisco qualitative study of medical doctors, administrators, and directors found that some but not all medical directors were aware of CDC’s most current HIV testing recommendations.22 A 2008 study of Indian Health Service physicians and nurses found that only 27.3% of participants were familiar and 30.7% were somewhat familiar with the 2006 CDC testing recommendations.27 A 2009 study of internal medicine physicians found that 88.0% of respondents were aware of the revised CDC testing recommendations.21 A 2010 study of internal medicine physicians at the University of Cincinnati Academic Health Center found that only 26.0% of its internal medicine residents and 41.7% of its internal medicine attending physicians were aware of the current CDC HIV testing recommendations, while only 31.0% of physicians were able to accurately identify the specific CDC recommendations.24 Another 2010 survey of health care providers in the largest primary care network in King County, Washington, showed that 76.0% of the respondents were aware of the CDC recommendations.28 A 2010 qualitative study of Los Angeles county primary care providers revealed that about half of the group had never heard of the 2006 recommendations.29 A 2010 study of VA primary care providers found that nearly 40% of providers were unaware of the 2006 CDC recommendations.30
HIV Testing Barriers: Attitudes
According to Cabana et al, attitude barriers to following guidelines include lack of agreement with specific guidelines or with guidelines in general, lack of self-efficacy in performing the guideline tasks, lack of outcome expectancy, and inertia of previous practice.26 A 2007 study of San Francisco medical providers found that 14.0% of its physicians believed that a low prevalence of HIV among their patients was a reason to not offer an HIV test.20 In a 2007 to 2009 San Francisco qualitative study of medical doctors, administrators, and directors found that respondents believed a robust HIV testing infrastructure was already in place and that providers were unsure of the added value of routine testing.22 A 2008 qualitative study of primary care providers in Veterans’ Affairs Medical Centers found that several providers felt ill prepared to raise the topic of HIV testing with patients.31 In a 2010 Los Angeles-based qualitative study, primary care providers raised doubts about the CDC recommendations.29 Providers noted an inner conflict related to a cost–benefit analysis of routine testing and/or not believing the “proof” that testing was “necessary.” These Los Angeles primary care providers mentioned a lack of trust in the CDC because the providers followed different professional organization’s clinical guidelines.29 A 2010 study of Washington health care providers found that 57.0% of respondents agreed that the perception that their patient population is low risk for HIV limits the number of HIV tests performed.28 A 2011 study of HRSA-funded health center sites found a barrier to testing at these sites was the physician’s perception of patient discomfort associated with HIV testing.25
HIV Testing Barriers: Behavioral Skills
According to Cabana et al,26 behavioral barriers that prevent physicians from adhering to recommendations include external barriers related to the guidelines themselves, to patients, or to environmental factors. Within the Cabana model, “behavioral” barriers may not necessarily stem from the provider themselves and so, at times, may also be thought of as systemic factors in the way that they influence physician behavior. A 2007 study of San Francisco medical providers found the following common physician barriers to HIV testing: insufficient time to do HIV testing (33.9%), no systematic follow-up for disclosure of results (26.9%), and not relevant to visit (24.2%).20 A 2007 study of New York city internal medicine resident physicians found that the most frequently identified barriers mentioned in this study were lack of time (40.6%), time-consuming/burdensome consent process (26.8%), language barriers (20.2%), and hard to find written HIV consent forms (19.1%).19 In a 2007 to 2009 San Francisco qualitative study of medical doctors, administrators, and directors, barriers to testing included doctors relying on patient requesting the test themselves, physicians’ inexperience in HIV care, time-consuming consent/counseling process, the burden of delivering test results, and competing clinical priorities.22 In a 2008 study of Indian Health Service physicians and nurses, 29.3% of respondents felt that an HIV-positive result would cause a patient to be rejected by the local community, while 43.0% thought HIV-related confidentiality would be difficult to maintain.27 Providers in this study were also concerned about confidentiality, false-positive HIV results, state regulations, and staffing constraints. A 2009 study of general internists showed that the top 3 barriers to HIV testing included competing priorities at the time of visit (79%), lack of time (63.9%), and perceived patient reluctance/refusal (63.9%).21 A 2008 study of Veterans’ Affairs Medical Center primary care providers found that providers agreed that requiring written informed consent forms represented a time-consuming obstacle to routine HIV testing.31 This study also found that providers viewed pretest counseling as a barrier to HIV testing because it took up “precious primary care minutes.” A 2010 study of internal medicine physicians at the University of Cincinnati Academic Health Center revealed the following top 3 barriers to HIV testing: not medically indicated to test every patient (53.1%), lack of time (37.1 %), and not high enough priority in my practice (23.5%).24 A 2010 study of Los Angeles primary care providers showed that provider barriers included time constraints, financial reimbursement, and difficult procedures for ordering HIV tests.29 In a 2010 study of Washington health care providers, 13% of respondents agreed that concern about reimbursement posed a barrier to HIV testing.28 A 2011 study of HRSA-funded health center sites found that barriers to HIV testing included limited financial resources of sites and of patients. About one-third (32%) of these HRSA-funded health center sites reported that they could offer only a limited number of free or reduced cost tests.25
Primary Care Providers Can Improve HIV Testing Rates
Several studies suggest that primary care providers’ recommendations to get tested for HIV can influence an individual’s intention of testing. In a national survey, among persons reporting having been HIV tested, 37% of respondents indicated they were tested because a doctor or health care provider recommended it.10 Conversely, the same survey found that of those who were not tested, 36% of respondents reported that their biggest reason for not being tested was that their doctor never recommended it. In a study of Hispanic men in South Florida, physician endorsement was the strongest predictor of an intention to test in the next 6 months, with 85.6% of patients reporting they would agree to be tested if a doctor recommended HIV testing.11 In a survey conducted in a general internal medicine clinic in Atlanta, previously HIV-tested women were more likely to report that their physician had recommended HIV testing compared to those women who had not been tested.12 In a survey of patients identified by the Collaborative Ambulatory Research Network, 48% of patients reported being tested based on their obstetrician or gynecologist recommendation.13 In a New York city community health survey, patients were more likely to have been recently tested if a doctor recommended an HIV test in the past year.14 In a survey of adults at 9 internal medicine clinics, 92.4% of those who reported getting tested for HIV also reported that their physician had recommended HIV testing.15 In a survey of African American men in Wisconsin, a doctor’s recommendation was the strongest predictor of having been tested: 96.5% of those who had a regular doctor who recommended HIV testing at the time of the study had been tested.16 This accumulation of evidence highlights the importance of a physician recommendation for promoting HIV testing.
Conclusion
Although HIV testing prevalence did increase from 35.3% in 2005 to a high of 39.8% in 2009, currently only 34.7% of adults report ever having been tested for HIV.7 In fact, many adults report their health care provider has never offered them HIV testing.10 Furthermore, in the United States, with more than 1 million people infected with HIV today, almost 1 in 5 people are still unaware of their status.8 Although patient factors impact the decision to test for HIV, physician recommendation to test is a chief reason why patients do get tested. Several studies have documented that physicians are missing opportunities to test patients for HIV.32–34 Most recently in 2013, a study published of missed opportunities for HIV testing among newly diagnosed HIV patients—33% of whom had AIDS at the time of diagnosis—found that 71% of patients with HIV had made a health care visit in the previous 12 months and had not been tested for HIV.35 In fact, this group of newly diagnosed, HIV-positive patients had a mean of 2.75 health care visits prior to the visit in which HIV was eventually diagnosed. Seven years after the release of CDC recommendations for routine HIV testing, testing has not become routine in all health care settings. Given that in April 2013 the USPSTF released recommendations in support of routine HIV testing, physician knowledge, attitude, and behavioral barriers must be addressed to see further gains in the number of patients tested and the number tested earlier—prior to the onset of life-threatening AIDS. Because a physician’s recommendation to test for HIV is a strong predictor of patient testing behavior, physicians’ implementation of routine HIV testing is essential to mitigating the current HIV epidemic. This review focused on physician-level barriers, but clinic- or setting-related barriers must also be addressed in future research and programming to make strides in HIV testing performance. Although there are numerous interventions that could improve adherence to the 2006 CDC guidelines, more research is required to determine and implement the most effective (both in cost and in operation) interventions to improve HIV testing for individual and public health.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Baylor-UT Houston Center for AIDS Research (CFAR), an NIH-funded program (AI036211; PI: Arya) and an NIH/NIMH K23 Award (MH094235-01A1; PI: Arya). This work was supported in part by the Houston VA HSR&D Center of Excellence (HFP90-020). The views expressed in this publication are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Reprints and permission: sagepub.com/journalsPermissions.nav
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Moyer VA on behalf of the U S. Preventive services task force. screening for HIV: U.S. preventive services task force recommendation statement. Ann Intern Med. 2013;159(1):51–60. doi: 10.7326/0003-4819-159-1-201307020-00645. [DOI] [PubMed] [Google Scholar]
- 2.Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 3.Qaseem A, Snow V, Shekelle P, Hopkins R, Jr, Owens DK Clinical Efficacy Assessment Subcommittee, American College of Physicians. Screening for HIV in health care settings: a guidance statement from the American college of physicians and HIV medicine association. Ann Intern Med. 2009;150(2):125–131. doi: 10.7326/0003-4819-150-2-200901200-00300. [DOI] [PubMed] [Google Scholar]
- 4.American College of Obstetricians and Gynecologists. ACOG committee opinion: routine human immunodeficiency virus screening. Obstet Gynecol. 2008;112(2 pt 1):401–403. doi: 10.1097/AOG.0b013e318183fbc2. [DOI] [PubMed] [Google Scholar]
- 5.Emmanuel PJ, Martinez J. Adolescents and HIV infection: the pediatrician’s role in promoting routine testing. Pediatrics. 2011;128(5):1023–1029. doi: 10.1542/peds.2011-1761. [DOI] [PubMed] [Google Scholar]
- 6.Society of General Internal Medicine. [Accessed October 31, 2013.];Routine HIV/AIDS testing. 2012 http://www.sgim.org/communities/clinical-practice/hiv-aids.
- 7.Centers for Disease Control and Prevention (CDC) [Accessed October 31, 2013.];National Health Interview Survey Early Release 1997–September 2012. Published March 10, 2013. http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201303_10.pdf.
- 8.Centers for Disease Control and Prevention. [Accessed October 31, 2013.];HIV in the United States: At a glance. 2013 Feb; http://www.cdc.gov/hiv/resources/factsheets/PDF/stats_basics_factsheet.pdf.
- 9.Centers for Disease Control and Prevention (CDC) Vital Signs: HIV Testing and Diagnosis Among Adults—United States, 2001–2009. [Accessed October 31, 2013.];Morbidity and Mortality Weekly Report (MWWR) http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5947a3.htm?s_cid=mm5947a3_w. [PubMed]
- 10.Kaiser Family Foundation. [Accessed October 31, 2013.];The Washington Post. Survey of Americans on HIV/AIDS: Summary and Chartpack. 2012 http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8334-f.pdf.
- 11.Fernandez MI, Bowen GS, Perrino T, et al. Promoting HIV testing among never-tested Hispanic men: a doctor’s recommendation may suffice. AIDS Behav. 2003;7(3):253–262. doi: 10.1023/a:1025491602652. [DOI] [PubMed] [Google Scholar]
- 12.Akers A, Bernstein L, Henderson S, Doyle J, Corbie-Smith G. Factors associated with lack of interest in HIV testing in older at-risk women. J Womens Health (Larchmt) 2007;16(6):842–858. doi: 10.1089/jwh.2006.0028. [DOI] [PubMed] [Google Scholar]
- 13.Coleman VH, Morgan MA, Carlson R, Hawks D, Schulkin J. Patient perceptions of obstetrician-gynecologists’ practices related to HIV testing. Matern Child Health J. 2009;13(3):355–363. doi: 10.1007/s10995-008-0374-9. [DOI] [PubMed] [Google Scholar]
- 14.Kim EK, Thorpe L, Myers JE, Nash D. Healthcare-related correlates of recent HIV testing in New York City. Prev Med. 2012;54(6):440–443. doi: 10.1016/j.ypmed.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stefan MS, Blackwell JM, Crawford KM, et al. Patients’ attitudes toward and factors predictive of HIV testing of academic medical clinics. Am J Med Sci. 2010;340(4):264–267. doi: 10.1097/MAJ.0b013e3181e59c3e. [DOI] [PubMed] [Google Scholar]
- 16.Petroll AE, DiFranceisco W, McAuliffe TL, Seal DW, Kelly JA, Pinkerton SD. HIV testing rates, testing locations, and healthcare utilization among urban African-American men. J Urban Health. 2009;86(1):119–131. doi: 10.1007/s11524-008-9339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmid C, Packett HK. The HIV Care Continuum Initiative and Coverage and Reimbursement of HIV Testing. [Accessed October 31, 2013.];Letter to Dr. Grant Colfax, Dr. Howard Koh. http://www.theaidsinstitute.org/sites/default/files/attachments/Care%20Continuum%20HIV%20Testing%20Letter.pdf.
- 18.Sison N, Yolken A, Poceta J, et al. Healthcare provider attitudes, practices, and recommendations for enhancing routine HIV testing and linkage to care in the Mississippi Delta region. AIDS Patient Care STDS. 2013;27(9):511–517. doi: 10.1089/apc.2013.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jain CL, Wyatt CM, Burke R, Sepkowitz K, Begier EM. Knowledge of the centers for disease control and prevention’s 2006 routine HIV testing recommendations among new york city internal medicine residents. AIDS Patient Care STDS. 2009;23(3):167–176. doi: 10.1089/apc.2008.0130. [DOI] [PubMed] [Google Scholar]
- 20.Cohan D, Gomez E, Dowling T, Zetola N, Kaplan B, Klausner JD. HIV testing attitudes and practices among clinicians in the era of updated centers for disease control and prevention recommendations. J Acquir Immune Defic Syndr. 2009;50(1):114–116. doi: 10.1097/QAI.0b013e31818d5f86. [DOI] [PubMed] [Google Scholar]
- 21.Korthuis PT, Berkenblit GV, Sullivan LE, et al. General internists’ beliefs, behaviors, and perceived barriers to routine HIV screening in primary care. AIDS Educ Prev. 2011;23(3 suppl):70–83. doi: 10.1521/aeap.2011.23.3_supp.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers JJ, Koester KA, Dufour MS. Barriers and facilitators to enhancing HIV testing in publicly funded primary care clinics: findings from San Francisco. AIDS Educ Prev. 2011;23(3 suppl):84–95. doi: 10.1521/aeap.2011.23.3_supp.84. [DOI] [PubMed] [Google Scholar]
- 23.Berkenblit GV, Sosman JM, Bass M, et al. Factors affecting clinician educator encouragement of routine HIV testing among trainees. J Gen Intern Med. 2012;27(7):839–844. doi: 10.1007/s11606-012-1985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohajer MA, Lyons M, King E, Pratt J, Fichtenbaum CJ. Internal medicine and emergency medicine physicians lack accurate knowledge of current CDC HIV testing recommendations and infrequently offer HIV testing. J Int Assoc Physicians AIDS Care. 2012;11(2):101–108. doi: 10.1177/1545109711430165. [DOI] [PubMed] [Google Scholar]
- 25.Department of Health and Human Services. [Accessed October 31, 2013.];HIV testing in HRSA-funded health center sites. 2013 Report No.: OEI-06-10-00290. https://oig.hhs.gov/oei/reports/oei-06-10-00290.pdf.
- 26.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? a framework for improvement. JAMA. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 27.Reilley B, Redd JT, Giberson S, Lee JK, Haverkamp D, Cheek J. Physician and nurse perspectives on implementation of universal adult HIV screening guidelines in the Indian health service: results of a randomized survey. J Public Health Manag Pract. 2010;16(5):450–456. doi: 10.1097/PHH.0b013e3181bdec1a. [DOI] [PubMed] [Google Scholar]
- 28.Shirreffs A, Lee DP, Henry J, Golden MR, Stekler JD. Understanding barriers to routine HIV screening: knowledge, attitudes, and practices of healthcare providers in King County, Washington. PLoS One. 2012;7(9):e44417. doi: 10.1371/journal.pone.0044417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hudson AL, Heilemann MV, Rodriguez M. Missed Opportunities for universal HIV screening in primary care clinics. J Clin Med Res. 2012;4(4):242–250. doi: 10.4021/jocmr1014w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arya M, Bush AL, Kallen MA, Rodriguez-Barradas MC, Giordano TP. Are VA primary care providers aware of HIV testing recommendations for veterans? findings at an urban VA primary care clinic. Mili Med. 2013;178(4):e483–e488. doi: 10.7205/MILMED-D-12-00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bokhour BG, Solomon JL, Knapp H, Asch SM, Gifford AL. Barriers and facilitators to routine HIV testing in VA primary care. J Gen Intern Med. 2009;24(10):1109–1114. doi: 10.1007/s11606-009-1078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liddicoat RV, Horton NJ, Urban R, Maier E, Christiansen D, Samet JH. Assessing missed opportunities for HIV testing in medical settings. J Gen Intern Med. 2004;19(4):349–356. doi: 10.1111/j.1525-1497.2004.21251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuo AM, Haukoos JS, Witt MD, Babaie ML, Lewis RJ. Recognition of undiagnosed HIV infection: an evaluation of missed opportunities in a predominantly urban minority population. AIDS Patient Care STDs. 2005;19(4):239–246. doi: 10.1089/apc.2005.19.239. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (CDC). . Missed opportunities for earlier diagnosis of HIV infection—South Carolina, 1997–2005. MMWR Morb Mortal Wkly Rep. 2006;55(47):1269–1272. [PubMed] [Google Scholar]
- 35.Chin T, Hicks C, Samsa G, McKellar M. Diagnosing HIV infection in primary care settings: missed opportunities. AIDS Patient Care STDs. 2013;27(7):392–397. doi: 10.1089/apc.2013.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]


