Abstract:
We investigated relation of the site of obstruction detected on Muller maneuver (MM) with polysomnography (PSG) and physical examination findings. Data of 703 patients admitted to Ankara Numune Education and Research Hospital Sleep Laboratory between 2008 and 2013 were analyzed retrospectively; 394 patients with apnea-hypopnea indexes (AHI) ≥5/h were included. Site of collapse on MM was determined at retrolingual level at anteroposterior (M1) and lateral–lateral (M2) directions; at retropalatal level at anteroposterior (M3) and lateral–lateral (M4) directions. There were 125 (31.7 %) females and 269 (68.3 %) males. BMI had significant positive correlations with M2 (p < 0.001) and M4 (p = 0.002) scores, ESS (p = 0.013) and AHI (p = 0.001). AHI had significant positive correlations with ESS (p = 0.003), M2 (p < 0.001), M3 (p = 0.037) and M4 (p < 0.001) scores and NC (p = 0.001). Minimum oxygen saturation had significant reverse correlations with M1 (p = 0.046), M2 (p < 0.001), M3 (p = 0.003), M4 (p < 0.001), AHI (p < 0.001), ESS (p = 0.003) and BMI (p = 0.001). In OSAS patients, increased BMI, NC and AHI are correlated with lateral pharyngeal wall (LPW) collapse in retropalatal and retrolingual levels on MM. LPW collapse is more valuable to predict OSAS compared to anteroposterior collapse. LPW collapse on MM may be used as a selection criterion for ordering PSG. Further studies are needed to better clarify importance of LPW in OSAS surgery.
Keywords: Body mass index, Epworth sleepiness scale, Muller’s maneuver, Obstructive sleep apnea, Polysomnography
Introduction
Obstructive sleep apnea syndrome (OSAS) is characterized by repetitive sleep- related upper airway obstructions resulting in sleep fragmentation and decrease in blood oxygen saturation. It is seen approximately in 1–5 % of adult men and in 1.2–2.5 % of adult women [1, 2].
Polysomnography (PSG) is the gold standard for the diagnosis of OSAS [3], providing information about the severity of OSAS and the degree of sleep fragmentation, but it does not provide any information for the level or the degree of upper airway obstruction. To date, various methods have been used to investigate the site of upper airway obstruction in patients with OSAS including magnetic resonance imaging, computerized tomography, lateral cephalometry and nasopharyngoscopy [4–8]. These methods provide important information for the site of the upper airway obstruction. In particular, upper airway endoscopy helps us to evaluate the dynamic examination of the nose, naso-, oro-, and hypopharynx during forced inspiration against closed mouth and nose, and the level and degree of obstruction in these regions can be determined [4]. This examination is called Muller’s maneuver (MM) when performed on the awake patient [9]. Muller maneuver helps us to evaluate the level and degree of upper airway narrowing and it has also been shown to be a predictive value for the OSAS surgery [4, 10–12]. Muller maneuver is a beneficial technique for the deciding to type of surgery procedure which we use in OSAS patients.
Sleep laboratories usually have long waiting lists since OSAS is a frequent disease and one night is needed for each patient for PSG. Therefore, using a questionnaire or an examination finding to select patients who must be given priority is wise, and a number of studies have been performed on this issue. In addition, the success of surgical treatment for OSAS is directly related with correct determination of the upper airway obstruction site and selection of an optimal surgical technique for this site.
The aim of this study is to investigate the relation of the site of the obstruction detected on Muller maneuver with PSG and physical examination findings.
Methods
In this study, the data of 703 consecutive patients who admitted to Ankara Numune Education and Research Hospital Sleep Laboratory between April 2008 and May 2013 with the complaints of daytime sleepiness and witnessed sleep apnea were analyzed retrospectively using the charts of the patients. The protocol was approved by the Ethics Committee of Ankara Numune Education and Resarch Hospital (project no: 554-2013). All of the patients had a detailed otorhinolaryngologic examination including fiberoptic nasopharyngoscopy with MM, and then they underwent overnight PSG.
The patients were divided into three groups according to their apnea hypopnea indexes (AHI) as “Mild OSAS” (5 ≤ AHI < 15), “moderate OSAS” (15 ≤ AHI < 30) and “severe OSAS” (AHI ≥ 30).
The patients who were diagnosed with simple snoring (AHI < 5), had already undergone an operation for OSAS, the ones with missing data, have any mental and neurological pathology were excluded. A total of 394 patients who had an AHI ≥ 5 were included. There were 269 males and 125 females, with a mean age of 48.7 years (range 28–73 years).
The age, sex, neck circumference (NC) (measured in centimeters at level of the cricothyroid membrane), body mass index (BMI), and Epworth sleepiness scale score (ESS) scores of the patients were recorded. The ESS scores of the patients were calculated after the patients completed the validated Turkish version of the questionnaire [13]. Excessive daytime sleepiness was considered if the ESS score was ≥10.
PSG was performed under the supervision of a sleep technician during spontaneous sleep. Electroencephalogram, submental and bilateral tibialis anterior electromyograms, electrooculogram, nasal airflow, thoracic and abdominal respiratory efforts, blood oxygen saturation (pulse oximetry) and body positions were recorded. The PSG data were scored manually according to the standard criteria set by the American Academy of Sleep Medicine [14] by an ENT physician who had a sleep diseases and PSG certificate.
The MM was performed when the patient was in sitting position, following topical nasal anesthesia achieved with 4 % lidocaine and 0.5 % ephedrine spray. A flexible endoscope (Olympus ENF, type GP) was inserted through the anesthetized nasal cavity into the nasopharynx and then advanced to oro- and hypopharynx. The site of collapse was assessed during a maximal inspiratory effort against a closed mouth and sealed nose (reverse Valsalva). The collapse of the upper airway was determined at the retrolingual level at anteroposterior (base of tongue—Muller’s 1 score) and lateral to lateral (lateral pharyngeal walls—Muller’s 2 score) directions. Similarly, retropalatal level was also investigated for collapse at anteroposterior (soft palate—Muller’s 3 score) and lateral to lateral (lateral pharyngeal walls—Muller’s 4 score) directions. The degree of obstruction was evaluated in a semi-quantitative manner and classified as follows:
no obstruction = 0,
approximately 25 % obstruction = 1,
approximately 50 % obstruction = 2,
approximately 75 % obstruction = 3 and
100 % obstruction = 4 [9].
The relations of the obstruction site on Muller’s maneuver with BMI, neck circumference, ESS and PSG findings were investigated.
The analysis of the data was performed using Statistical Package for Social Science (SPSS) for Windows 11.5 package program. The descriptive data were presented as mean ± standard deviation or as median (minimum–maximum) for continuos variables, and as number (n) percent (%) for nominal ones. The correlation between the variable pairs was analyzed using Spearman’s correlation test. The significance level was set at ` < 0.05.
Results
There were 125 (31.7 %) females and 269 (68.3 %) males. The mean age was 48.67 years (range 28–73), the mean BMI was 30.82 kg/m2 (range 21.1–53.4 kg/m2), the mean AHI was 33.44/hr (range 5.1–125.2), the mean ESS score was 8.1 ± 5.6 (range 0–24), the mean minimum (Min) O2 saturation was 77.4 % (range 24–93 %) and the mean NC was 39.7 cm (range 31–51) (Table 1).
Table 1.
Age, BMI, NC, ESS scores, PSG findings and Muller’s scores of the patients
| Mean | Std. deviation | Median | Minimum | Maximum | |
|---|---|---|---|---|---|
| Age (years) | 48.72 | 10.06 | 49.00 | 19.00 | 81.00 |
| BMI | 30.82 | 4.91 | 30.40 | 21.10 | 53.40 |
| NC | 39.71 | 3.00 | 40.00 | 31.00 | 51.00 |
| ESS | 8.05 | 5.54 | 8.00 | 0.00 | 24.00 |
| AHI | 33.44 | 26.36 | 25.10 | 5.10 | 125.20 |
| Min O2 | 77.24 | 11.84 | 81.00 | 24.00 | 93.00 |
| Muller’s 1 | 1.78 | 0.88 | 2.00 | 0.00 | 4.00 |
| Muller’s 2 | 2.21 | 0.90 | 2.00 | 0.00 | 4.00 |
| Muller’s 3 | 2.41 | 1.04 | 2.00 | 0.00 | 4.00 |
| Muller’s 4 | 2.64 | 0.99 | 3.00 | 0.00 | 4.00 |
The degree of obstruction on MM; no obstruction = 0, approximately 25 % obstruction = 1, approximately 50 % obstruction = 2, approximately 75 % obstruction = 3 and 100 % obstruction = 4
BMI body mass index (kg/m2), NC neck circumference (cm), ESS epworth sleepiness scale score, AHI apnea hypopnea index, Min O 2 minimum oxygen saturation (%), Muller’s 1 anteroposterior collapse (base of tongue) at retrolingual level, Muller’s 2 lateral pharyngeal wall collapse at retrolingual level, Muller’s 3 anteroposterior collapse (soft palate) at retropalatal level, Muller’s 4 lateral pharyngeal wall collapse at retropalatal level
The patients were divided into three groups according to their AHI: “Mild OSAS” (5 ≤ AHI < 15) (29.2 % of the patients), “moderate OSAS” (15 ≤ AHI < 30) (27.1 % of the patients) and “severe OSAS” (AHI ≥ 30) (43.7 % of the patients). The mean ESS increased and mean Min O2 saturation decreased as the severity of OSAS increased (Table 2).
Table 2.
Mean ESS, AHI and Min O2 values in relation with OSAS severity
| OSAS severity | Mean ESS | Mean AHI | Mean Min O2 (%) |
|---|---|---|---|
| Mild OSAS | 7.06 | 9.46 | 83.67 |
| Moderate OSAS | 7.98 | 20.95 | 80.52 |
| Severe OSAS | 8.76 | 57.24 | 70.88 |
OSAS obstructive sleep apnea, ESS epworth sleepiness scale score, AHI apnea hypopnea index, Min O 2 minimum oxygen saturation %
Muller’s 2 and Muller’s 4 scores indicating retropalatal and retrolingual collapse of the lateral pharyngeal walls increased as BMI increased (Muller’s 2: r = 0.211, p < 0.001; Muller’s 4: r = 0.156, p = 0.002). Similarly, Muller’s 2, Muller’s 3 and Muller’s 4 scores increased as AHI increased; Muller’s 2 and 4 indicating lateral walls’ collapse being highly significant (Muller’s 2: r = 0.226, p < 0.001; Muller’s 3: r = 0.105, p = 0.037; Muller’s 4: r = 0.203, p < 0.001). Muller’s 4 score increased as the NC increased (r = 0.109, p = 0.031). All Muller’s scores had statistically significant negative correlations with Min O2 saturation (Muller’s 1: r = −0.101, p = 0,046; Muller’s 2: r = −0.240, p < 0,001; Muller’s 3: r = −0.149, p = 0,003; Muller’s 4: r = −0.181, p < 0.001). On the other hand, there was no significant correlation between Muller’s scores and ESS (p > 0.05) (Table 3).
Table 3.
The correlation coefficients and p values among Muller’s scores and ESS, AHI, BMI, NC and Min O2 saturation
| Muller’s 1 | Muller’s 2 | Muller’s 3 | Muller’s 4 | ||
|---|---|---|---|---|---|
| ESS | Correlation coefficient | −0.047 | 0.033 | 0.034 | 0.057 |
| p Value | 0.350 | 0.515 | 0.500 | 0.258 | |
| AHI | Correlation coefficient | 0.042 | 0.226 | 0.105 | 0.203 |
| p Value | 0.410 | ≤0.001 | 0.037 | ≤0.001 | |
| BMI | Correlation coefficient | 0.066 | 0.211 | 0.099 | 0.156 |
| p Value | 0.191 | ≤0.001 | 0.050 | 0.002 | |
| NC | Correlation coefficient | 0.036 | 0.096 | 0.007 | 0.109 |
| p Value | 0.473 | 0.056 | 0.895 | 0.031 | |
| Min O2 | Correlation coefficient | −0.101 | −0.240 | −0.149 | −0.181 |
| p Value | 0.046 | ≤0.001 | 0.003 | ≤0.001 |
Spearman’s correlation test p < 0.05. BMI body mass index (kg/m2), NC neck circumference (cm), ESS epworth sleepiness scale score, AHI apnea hypopnea index, Min O 2 minimum oxygen saturation, Muller’s 1 anteroposterior collapse (base of tongue) at retrolingual level, Muller’s 2 lateral pharyngeal wall collapse at retrolingual level, Muller’s 3 anteroposterior collapse (soft palate) at retropalatal level, Muller’s 4 lateral pharyngeal wall collapse at retropalatal level
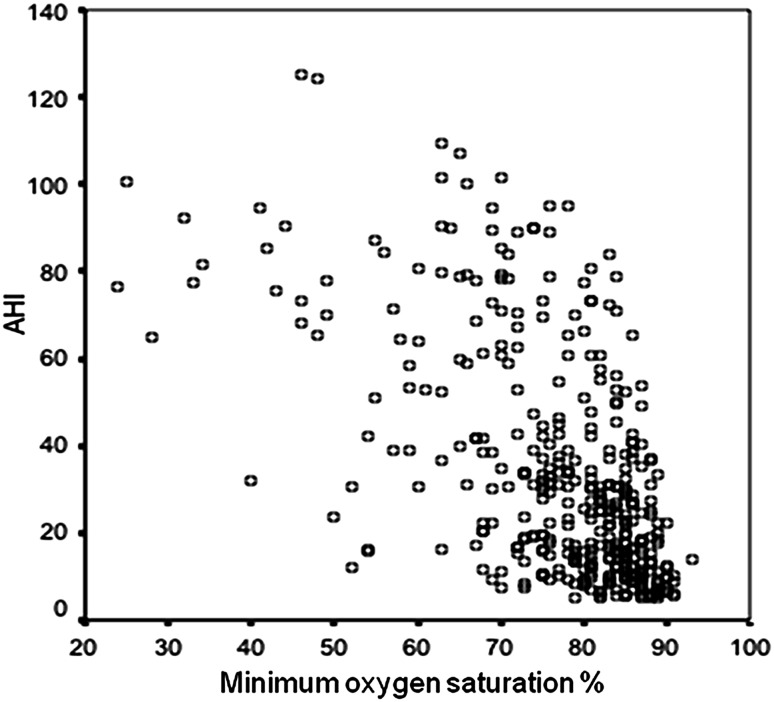
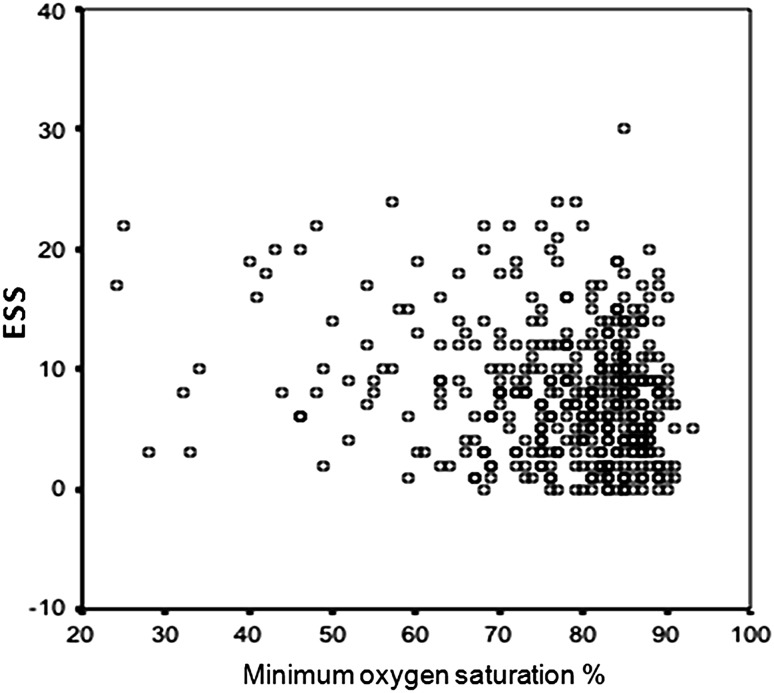
AHI showed significant negative correlations with Min O2 saturation (r = −0.568, p < 0.001) and ESS (r = −0.149, p = 0.003) (Fig. 1). Min O2 saturation was also negatively correlated with BMI (r = −0.361, p = 0.001). As ESS increased, Min O2 saturation decreased significantly (r = 0.150, p = 0.003) (Fig. 2) (Table 4).
Fig. 1.
The distribution of the cases for minimum oxygen saturation and apnea hypopnea index (AHI)
Fig. 2.
The distribution of the cases for minimum oxygen saturation and Epworth sleepiness scale (ESS) scores
Table 4.
The correlation coefficients and p values among ESS, AHI, BMI, NC and Min O2 saturation
| Variables | ESS | AHI | Min O2 | |||
|---|---|---|---|---|---|---|
| Correlation coefficient | p Value | Correlation coefficient | p Value | Correlation coefficient | p Value | |
| AHI | 0.150 | 0.003 | – | – | −0.568 | ≤0.001 |
| Min O2 | −0.149 | 0.003 | −0.568 | ≤0.001 | – | – |
| BMI | 0.126 | 0.013 | 0.230 | ≤0.001 | −0.361 | ≤0.001 |
| NC | 0.003 | 0.948 | 0.183 | ≤0.001 | 0.084 | 0.094 |
Spearman’s correlation test p < 0.05. BMI body mass index (kg/m2), NC neck circumference (cm), ESS Epworth sleepiness scale score, AHI apnea hypopnea index, Min O 2 minimum oxygen saturation
BMI and ESS (r = 0.126, p = 0.013), BMI and AHI (r = 0.230, p = 0.001), AHI and ESS (r = 0.150, p = 0.003) and NC and AHI (r = 0.183, p = 0.001) showed significant positive correlations. However, ESS and NC had no correlation (p > 0.05) (Table 4).
Discussion
OSAS is characterized by sleep-related apnea episodes and oxygen desaturations, and it may result in a number of significant morbidities including neurologic and cardiovascular complications.
MM has been first applied by Borowiecki and Sassin in patients with OSAS (5). Fiberoptic pharyngolaryngoscopy with Muller’s maneuver has been advocated as a practical, clinically applicable, preoperative dynamic diagnostic method for assessing the site of collapse. However, this technique has been criticized since it cannot show different obstruction levels at the same time, it is performed when the patient is awake and in a sitting position, and every patient cannot create an optimal negative pressure. Thong and Pang reported that MM findings were in correlation with AHI, and the maneuver can be used for determining patients with OSAS and can guide the treatment [15]. We found that Muller’s 2, 3 and 4 scores increased with increased AHI; Muller’s 2 and 4 indicating lateral walls’ collapse being highly significant (Muller’s 2: r = 0.226, p < 0.001; Muller’s 3: r = 0.105, p = 0.037; Muller’s 4: r = 0.203, p < 0.001).
In literature, some studies indicated that retroglossal collapse was correlated with AHI [16]. Hori et al. [5] studied 57 patients and analyzed their endoscopic examination using a computer program. The authors stated that retropalatal collapse was in association with OSAS due to increased collapsibility of the lateral pharyngeal walls in this region. Li et al. [6] investigated the pharyngeal anatomy in 30 obstructive sleep apnea patients under general anesthesia using magnetic resonance imaging, and reported that increased tissue volume at retropalatal region and lateral pharyngeal walls were related with OSAS. In our study, we studied lateral pharyngeal wall collapse in both retropalatal and retrolingual regions with MM, and found that Muller’s 2 and 4 scores indicating retrolingual and retropalatal lateral pharyngeal wall collapse were strongly correlated with AHI (for Muller’s 2 p < 0.001, for Muller’s 4 p < 0.001). Considering this finding, we suggest that lateral pharyngeal wall collapse may be used as a selection criterion for planning PSG and must be considered when planning surgery.
We found that BMI and AHI (r = 0.230, p = 0.001), and NC and AHI (r = 0.183, p = 0.001) had significant positive correlations. Dixon et al. [17] investigated the relation of obesity and AHI and found significant positive correlations between BMI, NC and AHI. The authors stated that increased NC had a more significant correlation with AHI when compared to BMI [17]. Similarly, Davies and Stradling found that increased BMI and NC were associated with OSAS, and noted that NC increased as the BMI increased, and this changed the fat distribution in the upper airways increasing fat tissue in the retropalatal area, i.e. around soft palate and uvula [7]. An interesting finding of our study is that Muller’s 2 and Muller’s 4 scores indicating retropalatal and retrolingual collapse of the lateral pharyngeal walls increased as BMI increased (Muller’s 2: r = 0.211, p < 0.001; Muller’s 4: r = 0.156, p = 0.002). Similarly, Muller’s 2, Muller’s 3 and Muller’s 4 scores increased as AHI increased; Muller’s 2 and 4 indicating lateral walls’ collapse being highly significant (Muller’s 2: r = 0.226, p < 0.001; Muller’s 3: r = 0.105, p = 0.037; Muller’s 4: r = 0.203, p < 0.001). These findings indicate that obesity causing increased fat amount in the neck causes collapse mainly in the lateral pharyngeal walls, both in oropharynx and hypopharynx. In a smaller patient cohort consisting of 87 patients, Ozdas et al. [18] found a significant correlation between BMI and AHI, and similarly suggested that increased BMI caused increased fat tissue in the lateral pharyngeal regions causing collapse of lateral pharyngeal walls both in oropharyx and hypopharynx on MM. Kim et al. [19] also reported that collapse of the lateral pharyngeal walls was associated with high AHI, however lateral pharyngeal walls could also collapse in non-obese patients.
The NC is supposed to reflect local fat tissue amount, however increased NC may be due to increase of subcutaneous fat or visceral fat. Some authors report that NC measurement was important for determining the tissue thickness surrounding the pharyngeal region and the adipose tissue around the neck [8]. Some others claim that visceral fat, rather than subcutaneous fat was related to abnormal respiratory functions including sleep apnea [20]. We found that increased NC had a positive correlation with Muller’s 4 score, indicating lateral pharyngeal wall collapse in the retropalatal region. When we consider the correlations of BMI and NC with AHI altogether, we can hypothesize that increased BMI causes increased collapsibility at the lateral pharyngal walls both in oropharynx and hypopharynx, however increased NC puts its effect mainly at the lateral pharyngeal walls of the oropharynx.
Chiner et al. [21] found a strong correlation between AHI and Min O2 saturation levels. Velasco Suarez et al. [22] stated that Min O2 saturation measured by pulse oximetry was a highly sensitive method for the diagnosis of OSAS in children with adenotonsillary hypertrophy. We found a significant negative correlation between AHI and Min O2 saturation (p < 0.001).
As mentioned before, we found positive correlations between AHI and Muller’s 2, Muller’s 3 and Muller’s 4 scores; Muller’s 2 and 4 being highly significant. We also found that Min O2 saturation had negative significant correlations with all Muller’s scores; Muller’s 2 and 4 having stronger correlations (Muller’s 1: r = −0.101, p = 0.046; Muller’s 2: r = −0.240, p < 0.001; Muller’s 3: r = −0.149, p = 0.003; Muller’s 4: r = −0.181, p < 0.001). In other words, AHI and Min O2 saturation had stronger correlations with lateral pharyngeal wall collapse when compared to anteroposterior collapse. Therefore, a high level of collapse, especially a lateral pharyngeal wall collapse on MM, can be used as a patient selection criterion for PSG.
Multiple sleep latency test and Maintenance of wakefulness test objectively measure daytime sleepiness, however they are time consuming and performed in the sleep laboratory. Therefore, ESS is a widely used subjective measure for daytime sleepiness and it is validated in Turkish [13]. There are conflicting results in the literature concerning the correlation of ESS with AHI [23–26]. In our study, ESS showed significant correlations with AHI (r = 0.150, p = 0.003), Min O2 saturation (r = 0.150, p = 0.003) and BMI (r = 0.126, p = 0.013). Kapur et al. [27] performed a multicenter study on 6,440 patients and found that ESS and AHI had a statistically significant positive correlation. On the other hand, we could not find a significant correlation between ESS and NC (p > 0.05). It has been claimed that daytime sleepiness and fatigue were primarily due to metabolic and physiologic factors rather than apnea and sleep fragmentation in OSAS [28, 29]. Inflammatory cytokines and mediators released as a result of metabolic syndrome were also reported to cause daytime sleepiness [30, 31]. Therefore, despite presence of a significant correlation between ESS and BMI, lack of a significant correlation between NC and ESS in our study makes us think that mediators and cytokines released due to metabolic syndrome may be responsible of daytime sleepiness in our patient population.
Conclusion
In OSAS patients, increased BMI and NC are correlated with lateral pharyngeal wall collapse in retropalatal and retrolingual levels. Lateral pharyngeal wall collapse on MM is related to high AHI scores and is more valuable to predict OSAS compared to anteroposterior collapse. It appears that the target area of fat deposition in the neck is lateral pharyngeal regions in OSAS. In addition, Min O2 saturation on PSG shows a stronger correlation with lateral pharyngeal wall collapse compared to anteroposterior collapse. On the first admission of the patient, presence of lateral pharyngeal wall collapse on MM may be used as a selection criterion for PSG. Further studies are needed to better clarify the importance of lateral pharyngeal walls in OSAS surgery.
Acknowledgments
There is no acknowledgment in this study.
Footnotes
This article was presented at 35th Turkish National Congress of Otorhinolaryngology and Head and Neck Surgery Congress, November 2–6, 2013, Antalya, Turkey.
References
- 1.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 2.Gislason T, Benediktsdottir B, Bjornsson JK, Kjartansson G, Kjeld M, Kristbjarnarson H. Snoring, hypertension, and the sleep apnea syndrome. An epidemiologic survey of middle-aged women. Chest. 1993;103(4):1147–1151. doi: 10.1378/chest.103.4.1147. [DOI] [PubMed] [Google Scholar]
- 3.Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276. [PMC free article] [PubMed] [Google Scholar]
- 4.Stanford W, Galvin J, Rooholamini M. Effects of awake tidal breathing, swallowing, nasal breathing, oral breathing and the Muller and Valsalva maneuvers on the dimensions of the upper airway. Evaluation by ultrafast computerized tomography. Chest. 1988;94(1):149–154. doi: 10.1378/chest.94.1.149. [DOI] [PubMed] [Google Scholar]
- 5.Hori Y, Shizuku H, Kondo A, Nakagawa H, Kalubi B, Takeda N. Endoscopic evaluation of dynamic narrowing of the pharynx by the Bernouilli effect producing maneuver in patients with obstructive sleep apnea syndrome. Auris Nasus Larynx. 2006;33(4):429–432. doi: 10.1016/j.anl.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Ye J, Li T, Lin N, Wang Z, Liang C, Sperry A, Han D. Anatomic predictors of retropalatal mechanical loads in patients with obstructive sleep apnea. Respiration. 2011;82(3):246–253. doi: 10.1159/000327176. [DOI] [PubMed] [Google Scholar]
- 7.Davies RJ, Stradling JR. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. Eur Respir J. 1990;3(5):509–514. [PubMed] [Google Scholar]
- 8.Shelton KE, Woodson H, Gay S, Suratt PM. Pharyngeal fat in obstructive sleep apnea. Am Rev Respir Dis. 1993;148(2):462–466. doi: 10.1164/ajrccm/148.2.462. [DOI] [PubMed] [Google Scholar]
- 9.Borowiecki BD, Sassin JF. Surgical treatment of sleep apnea. Arch Otolaryngol. 1983;109(8):508–512. doi: 10.1001/archotol.1983.00800220014004. [DOI] [PubMed] [Google Scholar]
- 10.Schwab RJ, Gefter WB, Hoffman EA, Gupta KB, Pack AI. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148(5):1385–1400. doi: 10.1164/ajrccm/148.5.1385. [DOI] [PubMed] [Google Scholar]
- 11.Sher AE, Thorpy MJ, Shprintzen RJ, Spielman AJ, Burack B, McGregor PA. Predictive value of Muller maneuver in selection of patients for uvulopalatopharyngoplasty. Laryngoscope. 1985;95(12):1483–1487. doi: 10.1288/00005537-198512000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Aboussouan LS, Golish JA, Wood BG, Mehta AC, Wood DE, Dinner DS. Dynamic pharyngoscopy in predicting outcome of uvulopalatopharyngoplasty for moderate and severe obstructive sleep apnea. Chest. 1995;107(4):946–951. doi: 10.1378/chest.107.4.946. [DOI] [PubMed] [Google Scholar]
- 13.Izci B, Ardic S, Firat H, Sahin A, Altinors M, Karacan I. Reliability and validity studies of the Turkish version of the Epworth Sleepiness Scale. Sleep Breath. 2008;12(2):161–168. doi: 10.1007/s11325-007-0145-7. [DOI] [PubMed] [Google Scholar]
- 14.Iber C, Ancoli-Israel S, Chesson A, Quan S. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Darien: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 15.Thong JF, Pang KP. Clinical parameters in obstructive sleep apnea: are there any correlations? J Otolaryngol Head Neck Surg. 2008;37(6):894–900. [PubMed] [Google Scholar]
- 16.Pang KP, Terris DJ, Podolsky R. Severity of obstructive sleep apnea: correlation with clinical examination and patient perception. Otolaryngol Head Neck Surg. 2006;135(4):555–560. doi: 10.1016/j.otohns.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 17.Dixon JB, Schachter LM, O’Brien PE. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest. 2003;123(4):1134–1141. doi: 10.1378/chest.123.4.1134. [DOI] [PubMed] [Google Scholar]
- 18.Ozdas T, Ozcan KM, Ozdogan F, Ozcan I, Selcuk A, Cetin MA, Dere H. Investigation of lateral pharyngeal walls in OSAS. Eur Arch Otorhinolaryngol. 2013;270(2):767–771. doi: 10.1007/s00405-012-2212-3. [DOI] [PubMed] [Google Scholar]
- 19.Kim HY, Bok KH, Dhong HJ, Chung SK. The correlation between pharyngeal narrowing and the severity of sleep-disordered breathing. Otolaryngol Head Neck Surg. 2008;138(3):289–293. doi: 10.1016/j.otohns.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Hoffstein V, Mateika S. Differences in abdominal and neck circumferences in patients with and without obstructive sleep apnoea. Eur Respir J. 1992;5(4):377–381. [PubMed] [Google Scholar]
- 21.Chiner E, Signes-Costa J, Arriero JM, Marco J, Fuentes I, Sergado A. Nocturnal oximetry for the diagnosis of the sleep apnoea hypopnoea syndrome: a method to reduce the number of polysomnographies? Thorax. 1999;54(11):968–971. doi: 10.1136/thx.54.11.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Velasco Suarez CT, Figueroa Turienzo JM, Len F, Mansilla E. Pulse oximetry recording in children with adenotonsillar hypertrophy: usefulness in the diagnostic of obstructive sleep apnea syndrome. Arch Argent Pediatr. 2013;111(3):196–201. doi: 10.5546/aap.2013.eng.196. [DOI] [PubMed] [Google Scholar]
- 23.Osman EZ, Osborne J, Hill PD, Lee BW. The Epworth Sleepiness Scale: can it be used for sleep apnoea screening among snorers? Clin Otolaryngol Allied Sci. 1999;24(3):239–241. doi: 10.1046/j.1365-2273.1999.00256.x. [DOI] [PubMed] [Google Scholar]
- 24.Kingshott R, Douglas N, Deary I. Mokken scaling of the Epworth Sleepiness Scale items in patients with the sleep apnoea/hypopnoea syndrome. J Sleep Res. 1998;7(4):293–294. doi: 10.1046/j.1365-2869.1998.00126.x. [DOI] [PubMed] [Google Scholar]
- 25.Chervin RD, Aldrich MS. The Epworth Sleepiness Scale may not reflect objective measures of sleepiness or sleep apnea. Neurology. 1999;52(1):125–131. doi: 10.1212/WNL.52.1.125. [DOI] [PubMed] [Google Scholar]
- 26.Fong SY, Ho CK, Wing YK. Comparing MSLT and ESS in the measurement of excessive daytime sleepiness in obstructive sleep apnoea syndrome. J Psychosom Res. 2005;58(1):55–60. doi: 10.1016/j.jpsychores.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ. Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep. 2005;28(4):472–477. doi: 10.1093/sleep/28.4.472. [DOI] [PubMed] [Google Scholar]
- 28.Basta M, Vgontzas AN. Metabolic abnormalities in obesity and sleep apnea are in a continuum. Sleep Med. 2007;8(1):5–7. doi: 10.1016/j.sleep.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Vgontzas AN, Basta M. Board Review Corner: the case of the sleepy middle-aged woman. J Clin Sleep Med. 2007;3(1):85. [PubMed] [Google Scholar]
- 30.Vgontzas AN, Bixler EO, Tan TL, Kantner D, Martin LF, Kales A. Obesity without sleep apnea is associated with daytime sleepiness. Arch Intern Med. 1998;158(12):1333–1337. doi: 10.1001/archinte.158.12.1333. [DOI] [PubMed] [Google Scholar]
- 31.Resta O, Foschino Barbaro MP, Bonfitto P, Giliberti T, Depalo A, Pannacciulli N, De Pergola G. Low sleep quality and daytime sleepiness in obese patients without obstructive sleep apnoea syndrome. J Intern Med. 2003;253(5):536–543. doi: 10.1046/j.1365-2796.2003.01133.x. [DOI] [PubMed] [Google Scholar]