Abstract
Though haemangioma of cheek is not a very uncommon entity, here we are presenting a case series of four such cases of haemangioma cheek of completely different presentation. One of which is classical maxillary haemangioma and the rest of the others have different and unusual presentations. They all have different radiological features and were managed successfully by different surgical approaches without any recurrence.
Keywords: Vascular tumors, Hemangioma, Sclerotherapy, Para nasal sinus, Maxillectomy
Introduction
International Society for the study of vascular anomalies has divided vascular anomalies in two main types: vascular tumors (the most common type is infantile hemangioma) and vascular malformations [1]. They have defined haemangioma as a benign vascular tumour. Histologically cavernous haemangioma are generally composed of sinusoidal cavities filled with blood. Haemangioma involving the cheek are rare. Cheek swelling due to haemangioma are usually haemangioma within maxilla or arising outside maxilla. Dahlin [2], in a review of 3,947 cases of bone tumours, found 47 cases of osseous haemangioma out of which only three involved the upper jaw. Smith [3] reported only 10 cases of haemangioma of the maxilla till 1959 and few isolated cases have been reported since then [4]. We present here case series of four hemangiomas over a period of 8 years in a tertiary referral institute of Kolkata, one of which was a case of classical osseous hemangioma and rest of the three cases were present in and around the maxilla which had atypical clinical presentations.
Case Series
Case 1
A 75-year-old female presented to Otorhinolaryngology clinic with nasal obstruction for last 1 year, progressive swelling over the left cheek for last 6 months and intermittent episodes of nasal bleeding for last 4 months. There was no history of difficulty in vision, headache, fever, difficulty in opening the mouth or pain over the swelling.
Locoregional examination revealed an ill defined swelling (5 cm × 3 cm) over the left cheek. The swelling was hard, non-tender, without any sinus, fistula or ulceration over the swelling. On anterior rhinoscopy, a reddish mass was seen in the left nostril which pushed the septum toward the opposite side. The mass was arising from the lateral wall, was soft to firm, with irregular surface and bled to touch. Posterior rhinoscopy, Ophthalmological and rest of the systemic examination was within normal limit.
CECT scan of Nose and Paranasal sinus showed hyperdense mass with significant contrast uptake in the left maxillary antrum with destruction of all walls and extension into the nasal cavity, orbit, soft tissue of cheek, oral cavity and infratemporal fossa. The paranasal sinuses of opposite side was normal.
Nasal endoscopic examination was suggestive of a vascular mass, which was corroborated by CECT of nose and PNS.
We planned to manage this case by enbloc removal of mass by total maxillectomy under general anesthesia. After lid plication, Weber Ferguson incision was made and skin flap elevated. Subsequently maxilla was separated by cutting the frontal process, zygomatic process, hard palate and pterygoid plate. Then left maxilla was removed, the orbit was preserved, temporary reconstruction of hard palate was done with guttapurcha and the space was packed with gel foam and anterior nasal packing was applied to prevent post operative bleeding. Closure was made in layers with appropriate sutures. The specimen was sent for histopathological examination (Fig. 1).
Fig. 1.

The maxillectomy specimen comprising of the hemangiomatous mass of case (Case 1)
The histopathological examination showed mucoid material, degenerated material and a lesion composed of vascular channel of various size suggestive of maxillary sinus haemangioma (Fig. 2). There is no evidence of recurrence after 12 months of follow up.
Fig. 2.
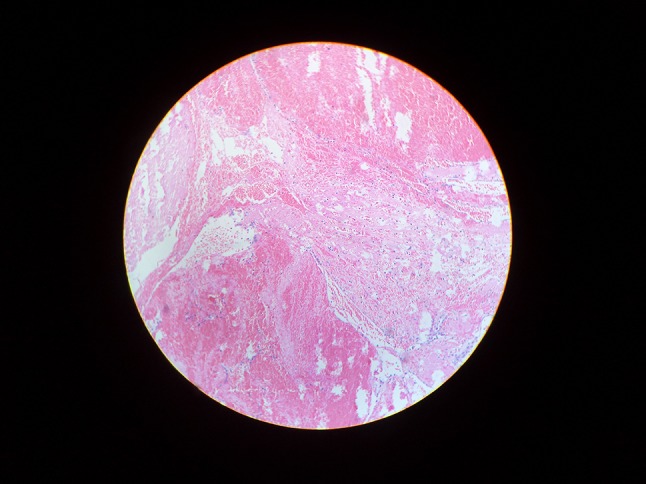
Histopathological examination showing vascular channel of various size suggestive of maxillary sinus haemangioma (Case 1)
Case 2
KD, a 55 years old female, was admitted with complaint of a gradually progressive swelling over right cheek without epistaxis for last 2 years. The patient was hypertensive and anaemic. A firm ill-defined cystic swelling was present over right maxilla. It was 5 cm × 5 cm in size with well defined margins and smooth surface. Overlying skin was non-adherent. The lateral wall of the right nasal cavity showed a diffuse bulge, resulting in restricted right nasal airway. Anterior rhinoscopy was suggestive of medial bulging of the lateral wall. The palate, teeth, and the orbit were clinically uninvolved. Rest of the ENT examination including the nervous system and the visual examinations revealed nothing abnormal. Hypertension was controlled and blood transfusion given to correct anaemia.
CT scan of the nose and paranasal sinuses revealed a predominantly heterogenously enhancing right maxillary antral mass with low attenuating cystic areas, interspersed with a few high attenuating areas. A cystic area was noted lying just outside the bony wall (Fig. 3). In one of the axial cuts there was slight dehiscence of the anterolateral wall of the maxilla.
Fig. 3.

CT scan of nose and paranasal sinus (Axial cut) showing predominantly heterogenously enhancing right maxillary antral mass with a cystic area outside the bony wall (Case 2)
We decided to remove the mass following the routine operative steps as detailed above. During the operation, cystic mass containing serous fluid was encountered initially. Further exploration in the dehiscent anterior wall of maxilla revealed a fleshy mass (Fig. 4). Lateral wall, posterior wall, the roof and the floor of the antral cavity seemed to be intact. The mass was removed enbloc and sent for histopathological study. Histopathological features were compatible with haemangioma. Postoperative healing was uneventful (Fig. 5).
Fig. 4.

Per operative photograph of the mass being removed by the lateral rhinotomy approach (Case 2)
Fig. 5.

Post operative clinical photograph of the patient (Case 2)
Case 3
SB, a 46-year-old lady presented to the ENT OPD with a pulsatile swelling in front of right cheek. It was 5 cm × 5 cm size with ill-defined margin. The surface of the swelling was smooth, temperature slightly raised, non tender on superfical palpation and consistency was soft (Fig. 6). There was no adhesion to the overlying skin or underlying structures. FNAC was suggestive of haemangioma. Sclerotherapy was done with sodium dodecylsulfate under supervision in order to reduce the size of the lesion. After considerable reduction in the size and consistency, we decided to remove the mass under GA.
Fig. 6.

Clinical photograph of the patient showing illdefined smooth swelling in front of the right maxilla (Case 3)
After proper dressing and draping, Moore’s incision was made starting from midpoint between medial canthus and root of the nose downwards along the nasomaxillary groove up to the ala. The haemangiomatous mass was exposed and feeding vessels were ligated (Fig. 7).The entire specimen was removed en mass (Fig. 8). HPE confirmed it to be hemangioma.
Fig. 7.

Per operative photograph showing the haemangiomatous mass being exposed and feeding vessels being ligated (Case 3)
Fig. 8.

Specimen of the hemangiomatous mass (Case 3)
Case 4
BD, a 27 years old male attended OPD with a soft swelling of 5 cm × 4 cm size in between zygoma and anterior border of masseter of the right side. The swelling was illdefined and compressible (Fig. 9). CT scan was suggestive of heterogenously enhancing, well encapsulated vascular mass lateral to the anterolateral wall of maxilla (Fig. 10). FNAC, as in previous cases, was suggestive of haemangioma.
Fig. 9.

Clinical photograph of the patient (Preop) (Case 4)
Fig. 10.

Preoperative CT scan showing the mass (Case 4)
The haemangioma was excised under general anaesthesia (Fig. 11) and the HPE confirmed the same.
Fig. 11.

Postoperatve photograph of the specimen (Case 4)
Discussion
Haemangioma in the Maxillo-facial region is uncommon with only few cases reported in the medical literature. As far as the incidence is concerned, intra-osseous Hemangiomas constitutes <1 % of the all Osseous tumors. According to Sandra et al. [5], haemangiomas account for 10 % of primary benign neoplasm of the skull bones. Considering the rarity of the disease entity at this site, this series requires special emphasis.
Hemangiomas were originally classified as vascular neoplasm. Now they are grouped with hamartomas with anomalous proliferation of endothelium lined channels of blood vessels.
Swelling of the upper jaw, which is hard on palpation, recurrent episodes of epistaxis, pressure effects on adjoining structures and cosmetic malformations are all classical manifestations of intra osseus hemangioma. We present here a series in which the first case is the typical presentation as mentioned. However rest of the three cases presented with atypical features which deserves special mention.
An interesting part of the discussion on this topic is about sex predilection. Sandra et al. [5] reported a female preponderance (M:F in 1:3 ratio). In contrast slightly more male preponderance was reported by Al-Khateeb et al. [6] in Jordanian children and adolescent population. Another interesting data from Tel Aviv from Zlotogorski et al. [7] reveals an equal distribution among male and female population. Considering the rare incidence of the disease, it is however not possible to generalize the overall sex incidence. In our series, three patients were females and one was male with the ratio of 3:1, consistent with the literature.
In the second case of our series, the patient had a cystic mass outside the maxilla, which was in continuation with the intramaxillary component. The pressure effect with associated hyperemic decalcification might have caused the erosion. Such a case of hemangioma with cystic degeneration of the anterior part have not yet been reported in literature. Absence of epistaxis in this case is also worth mention.
The third and the fourth cases had no intramaxillary involvement, with only the subcutaneous plane involved.
CECT is the investigation of choice which reveals nonhomogenous enhancing lesion in maxillary sinus [8]. The lesion may cause bone erosion which can mislead to diagnosis of malignant tumors. Gadolinium enhanced MRI may show hyper intense signal on T2-weighted images. MR Angiography is used in cases of larger mass, to identify the feeder vessels and hence for consideration of embolisation as part of treatment [9].
Differential diagnosis include malignancies of epithelial or other mesothelial tissue origin, bone cysts, dysplasia or other benign lesion etc. All these can be excluded by radiological investigations as mentioned above.
The treatment modalities includes invasive and non invasive procedures. Complete surgical excision is always the treatment of choice, which can be done by the suitable surgical approaches like Caldwel Luc [10, 11], Weber Ferguson [12], lateral rhinotomy [13, 14] or endoscopic removal [15] can be done depending upon the site and extent of the lesion and encroachment of the hemangioma into the adjacent structures. Non invasive techniques include systemic or intra lesional corticosteriod and interferon alpha2, however long term follow up in the literature is not available [16]. Photocoagulation or cryotherapy have not been proven effective in these areas considering the depth of the maxillary sinus [16].
A brief mention about sclerotherapy as a possible alternative option needs a brief mention. Various chemical agents have been used like ethanol, polidocanol and Bleomycin [17, 18]. Percutaneous USG guided intralesional Bleomycin infiltration had a remarkable success rate for treatment of facial hemangiomas as minimal size reduction or partial fibrosis of the lesion may be enough to achieve subjective clinical improvement [18].
Contributor Information
Bivas Adhikary, Email: adhikarybivas@yahoo.co.in.
Shubhrakanti Sen, Email: sen.shubhrakanti@gmail.com.
Pranabashish Banerjee, Email: drpranab_2005@rediffmail.com.
Soumendranath Bandyopadhyay, Email: sban_kolkata@rediffmail.com.
Diptanshu Mukherjee, Email: dipe_medico@rediffmail.com.
Sekhar Bandyopadhyay, Email: sekharb3@gmail.com.
Pradip Kumar, Email: dr_pkpatil@yahoo.co.in.
Aniruddha Majumder, Email: dr.anirudha@yahoo.com.
References
- 1.Enjolras O, Mulliken JB (1997) Vascular tumors and vascular malformations (new issues). Adv Dermatol 13:375–423 [PubMed]
- 2.Dahlin DC (1979) Bone tumours. C. Thomson, Illinois, Springfield, p 100. As quoted by Ghosh et al. 1988
- 3.Smith HW (1959) Hemangioma of jaws. Review of literature and review of a case. Arch Otolaryngol 70:579. As quoted by Ghosh et al. 1988 [DOI] [PubMed]
- 4.Bisaria KK, Misra UC. Haemangioma of the orbit and cheek. Brit J Opthal. 1968;52:628. doi: 10.1136/bjo.52.8.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore SL, Chun JK, Mitre SA, Som PM. Intraosseous Hemangioma of the Zygoma: CT and MR findings. Am J Neuroradiol. 2001;22:1383–1385. [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Khateeb T, Al-Hadi HA, Al masri NM. Oral and maxillofacial tumours in north Jordanian children and adolescents: a retrospective analysis over 10 years. Int J Oral Maxillo-Fac Surg. 2003;32:78–83. doi: 10.1054/ijom.2002.0309. [DOI] [PubMed] [Google Scholar]
- 7.Zlotogorski A, Buchner A, Kaffe I, Schwartz-Arad D. Radiological features of central hemangioma of the jaws. Am J Orthod Dentofac Orthop. 2005;128(3):385–387. doi: 10.1016/j.ajodo.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Kim HJ, Kim JH, Hwang EG. Bone erosion caused by sinonasal cavernous hemangioma: CT findings in two patients. Am J Neuroradiol. 1995;16(5):1176–1178. [PMC free article] [PubMed] [Google Scholar]
- 9.Lahoz Zamarro MT, Galve Royo A (1990) Hemangioma cavernoso de seno maxilar. Acta Otorrinolaringol Esp 41:197–199 [PubMed]
- 10.Most DS. Hemangioma of the maxillary sinus. Oral Surg Oral Med Oral Pathol. 1985;60:485–486. doi: 10.1016/0030-4220(85)90234-8. [DOI] [PubMed] [Google Scholar]
- 11.Cansiz H, Yener M, Kalekoglu N, Dalkilic O. Arteriovenous malformation of the maxillary sinus and mandible: a case report. Ear Nose Throat J. 2003;82(8):608–614. [PubMed] [Google Scholar]
- 12.Ghosh LM, Samanta A, Nandy T, Das S. Hemangiomas of the maxilla. J Laryngol Otol. 1988;102:725–726. doi: 10.1017/S0022215100106280. [DOI] [PubMed] [Google Scholar]
- 13.Raboso E, Rosell A, Plaza G, Martinez-Vidal A. Haemangioma of the maxillary sinus. J Laryngol Otol. 1997;111:638–640. doi: 10.1017/S0022215100138186. [DOI] [PubMed] [Google Scholar]
- 14.Naraghi A, Keene M. Maxillary intraosseous vascular malformation: a case report and literature review. J Laryngol Otol. 2007;121(4):404–407. doi: 10.1017/S0022215107004562. [DOI] [PubMed] [Google Scholar]
- 15.Mussak E, Lin J, Prasad M. Cavernous hemangioma of the maxillary sinus with bone erosion. Ear Nose Throat J. 2007;86:565–566. [PubMed] [Google Scholar]
- 16.Kendel J. Vascular anomalies and linphedema. Selected Readings in Plastic: Surgery; 2000. p. 9. [Google Scholar]
- 17.Winter H, Dräger E, Sterry W. Sclerotherapy for treatment of hemangiomas. Dermatol Surg. 2000;26(2):105. doi: 10.1046/j.1524-4725.2000.98012.x. [DOI] [PubMed] [Google Scholar]
- 18.Spencea J, Kringsa T, terBruggea KG, da Costaa LB, Agida R. Percutaneous sclerotherapy for facial venous malformations: subjective clinical and objective MR imaging follow-up results. Am J Neuroradiol. 2010;31:955–960. doi: 10.3174/ajnr.A1940. [DOI] [PMC free article] [PubMed] [Google Scholar]


