Abstract
Le Fort I osteotomy has become a routine procedure in elective orthognathic surgery. This procedure is often associated with significant but rare post-operative complications. The study was conducted to evaluate the rate of post-operative complications following conventional Le Fort I osteotomy. Twenty-five healthy adult patients who had to undergo Le Fort I osteotomy without segmentalization of maxilla were included in the study based on indications of surgery. All the patients were followed up for a period of 6 months post-operatively to assess the rate of various post-operative complications such as neurosensory deficit, pulpal sensibility, maxillary sinusitis, vascular complications, aseptic necrosis, unfavourable fractures, ophthalmic complications and instability or non-union of maxilla, etc. The results of our study showed a post-operative complications rate of 4 %. Neurosensory deficit and loss of tooth sensibility were the most common findings during patient evaluation at varying follow-up periods while one patient presented with signs and symptoms of maxillary sinusitis post-operatively. Neurosensory as well as sinusitis recovery took place in almost all the patients within 6 months. It was concluded that thorough understanding of pathophysiological aspects of various complications, careful assessment, treatment planning and the use of proper surgical technique as well as instrumentation may help in further reducing the complication rate.
Keywords: Le Fort I osteotomy, Orthognathic surgery, Complications
Introduction
Orthognathic surgery has evolved into one of the standards of care in oral and maxillofacial surgery. Since its first description by Von Langenback in 1859, now called Le Fort I osteotomy, this procedure has become the main stay for correction of almost any kind of dentofacial deformity [1]. The versatility of this procedure has been described by many authors in literature.
Inspite of all the advancements made in orthognathic surgical field, a variety of complications have been documented. These include maxillary sinusitis, loss of tooth vitality, sensory nerve morbidity, aseptic necrosis, vascular complications like arteriovenous fistulae or haemorrhage, nasal septal deviation, unfavourable fractures of base of the skull and pterygoid plates, various ophthalmic complications including blindness and others like malpositioning, non-union or instability of maxilla and relapse, etc [1, 2]. Descriptive information relative to these complications is sparse, therefore, a quantitative assessment of complications might be helpful for the patient, the orthodontist and the surgeon to estimate the benefit of an elective surgical procedure versus risks involved. Knowledge of complications also might help to prevent their occurrence and facilitate their management [2].
Overall complication rate has been reported to range from 6.1 to 9 % [3, 4] which can vary to a large extent for various individual complications. This variability may be owing to the difference in surgical skill and technique or diagnostic criteria used. The aim of the study was to report the incidence of various post-operative complications of Le Fort I osteotomy and to explain their pathophysiological and preventive aspects.
Materials and Methods
Twenty-five healthy patients (Table 1) who underwent conventional Le Fort I osteotomy without any segmentalization of maxilla were investigated with respect to complications associated with this procedure both prospectively and retrospectively. For retrospective analysis, all the data pertaining to this study was collected from the department records and thoroughly evaluated. The following were the criteria for selection of patients for study.
Table 1.
Patient data
| Total number of patients | 25 |
| No. of males | 3 |
| No. of females | 22 |
| Mean age ± SD | 21.64 ± 4.2 years |
| Age range | 18–35 years |
Inclusion Criteria
Patients with vertical maxillary excess or deficiency and patients with prognathic or retrognathic maxilla.
Patients with clinically healthy maxillary sinus and with no previous neurosensory deficit of extra oral or intraoral region.
Patients with routine blood and urine examination revealing no abnormal values.
Exclusion Criteria
Patients with cleft lip and palate.
Patients with systemic complications such as bleeding disorders, cardiovascular disease, gastrointestinal lesion and diabetes mellitus, etc.
Patients who underwent anterior or posterior segmental osteotomies in conjunction with Le Fort I osteotomy.
Adverse changes in morphology of lip and nose were not evaluated.
Method of Collection of Data
Twenty-five adults (22 females and 3 males), average age 21.64 year (range 18–35 years) undergoing Le Fort I down fracture between 2001 and 2008 were selected the study. Various complications following Le Fort I osteotomies were assessed clinically along with the help of other diagnostic aids wherever necessary. All prospective tests and examinations were carried out by a single operator to rule out any interobserver bias and patient’s consent was obtained before carrying out any examination.
Surgical Procedure
Under general anaesthesia, the soft tissue access was gained by a horizontal incision high in the buccal sulcus from first molar to first molar after injecting 2 % lignocaine hydrochloride with 1:80,000 adrenaline along the proposed incision line.
Subperiosteal dissection was carried out to expose the anterior and lateral walls of the maxillary antrum and extended superiorly to identify the infra-orbital neurovascular bundle and was carefully retracted. Posteriorly the soft tissue was tunnelled to the pterygo-maxillary junction. The subperiosteal dissection extended into the nasal cavity to lift the nasal mucosa from the floor of the nose, from the lateral nasal walls and from the base of the nasal septum.
An osteotomy cut was made with straight hand piece using long shank straight fissure bur through the lateral and anterior antral wall from piriform aperture to the pterygo-maxillary junction on both sides. The lateral nasal walls were divided with an osteotome. The nasal septum was separated with an osteotome directed along the nasal floor. Pterygomaxillary dysjunction was performed using curved pterygoid chisel and simultaneously placing a finger on the palatal side in the region of hamular notch to make sure that position of pterygoid chisel is correct and to avoid any untoward fractures of pterygoid plate. Maxilla was then down fractured in one segment. Bone trimming was carried out as appropriate to reposition the Le Fort I segment in a predetermined position and bone graft placed wherever necessary. Fixation was achieved by using four mini-plates one in the buttress region and an other near lateral wall of piriform rim bilaterally. Alar cinch suture was placed and final closure was carried out. All the patients were put on maxillomandibular fixation for a period of 6 weeks to stabilize the osteotomized segments.
The various complications taken into consideration, their methods of evaluation and follow-up periods are as given below:
-
(A)
Neurosensory testing for intraoral and extraoral soft tissue Modalities of sensation tested include fine touch response with brush stroke, pin prick using sharp probing and two point discrimination test using a divider at 10 days, 8 and 24 weeks post-operatively.
Protocol for testing:- Skin of face Three sites were tested on each side i.e. infraorbital region, lateral alar region and superior labial region corresponding to branches of infraorbital nerve trunk. Response was recorded as positive or negative. Even if one region was showing negative response it was considered as negative i.e. parasthesia of infraorbital nerve of the respective side (Fig. 1).
-
(B)
Buccal mucosa Again three sites were tested on each side below the incision line i.e. in incisor region, premolar region and molar region corresponding to anterior superior alveolar, middle superior alveolar and posterior superior alveolar nerve (Fig. 2).
-
(C)
Tooth sensibility The central incisors, first premolars and first molars were examined with an electric pulp stimulator and ethyl chloride spray bilaterally on preoperative day, 10 days, 8 and 24 weeks post-operatively (Fig. 3). When a tooth was missing, bore a crown, was root filled or did not respond to electric pulp tester or ethyl chloride spray preoperatively, an adjacent tooth supplied by the same nerve branch was examined. When a patient felt pain during stimulation of a tooth the pulpal sensibility of the tooth was judged as positive.
-
(D)
Maxillary sinusitis The condition of maxillary sinus was assessed based on the most common occurring signs and symptoms like sinus pain, nasal obstruction, anterior or post-nasal drainage, heaviness or fullness of the sinus region. Patients were examined preoperatively, 10 days, 8 and 24 weeks post-operatively.
-
(E)
Vascular complications Most common vascular complications like epistaxis and haemorrhage were assessed clinically post-operatively till first week as most of the vascular complications are known to occur during the first 24 h.
-
(F)
Aseptic necrosis Any clinical signs suggestive of aseptic necrosis like sloughing of tissue, periodontal defects were checked 10 days and 8 weeks post-operatively.
-
(G)
Unfavourable fractures Any unfavourable fractures like tuberosity fracture, untoward pterygoid plate fracture and sphenoid bone fracture i.e. base of skull were assessed clinically on operation table and any suspected positive findings were confirmed radiographically.
-
(H)
Ophthalmic complications Various ophthalmic complications assessed were diplopia, abnormal or restricted movements of eye balls, decrease in visual acuity or even blindness in immediate post-operative period and 8 weeks post-operatively.
-
(I)
Instability or non-union of maxilla Instability of maxilla was assessed manually at 8 and 24 weeks post-operatively and graded as positive if present.
Rest of the complications associated with Le Fort I osteotomy were considered under miscellaneous and were clinically evaluated. The above eight complications were examined at various time intervals specified and the data was statistically analyzed.
Fig. 1.
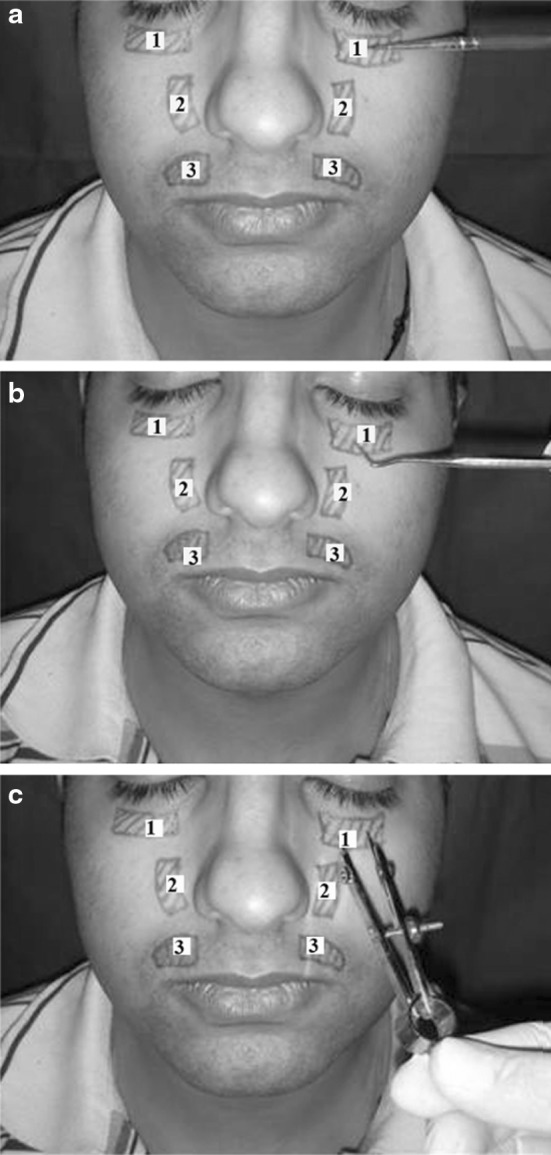
Evaluation of neurosensory deficit of infraorbital nerve using a soft bristle brush stroke, b sharp probing and c two point discrimination
Fig. 2.
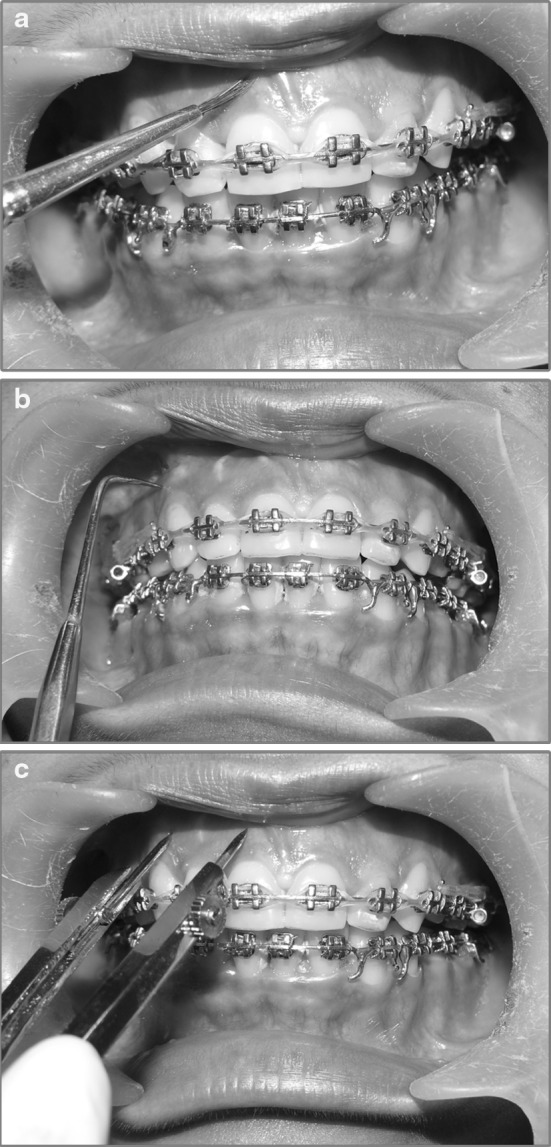
Evaluation of neurosensory recovery in buccal mucosa using a Brush stroke. b Sharp probing. c Two point discrimination
Fig. 3.
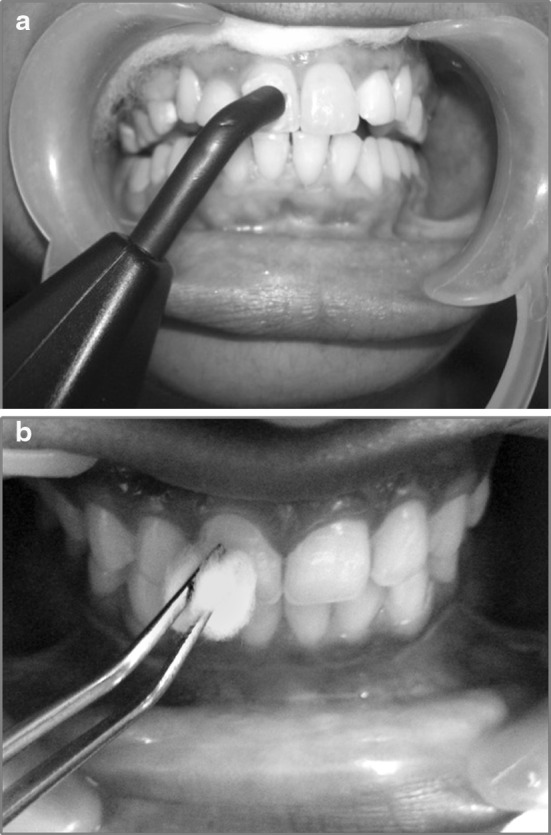
Assessment of pulp sensibility. a Assessment of pulp sensibility using electric pulp stimulator. b Assessment of pulp sensibility using ethyl chloride with cotton applicator
Results
Assessment of neurosensation in buccal mucosa, below the incision line (Table 2) after Le Fort I osteotomy revealed that fine touch sensation, pin prick sensation as well as two point discrimination recovered in 96 % patients at the end of 24 weeks and the results were statistically significant. (Fine touch sensation: χ2 = 55.161, df = 2; Pin prick sensation: χ2 = 52.061, df = 2; Two point discrimination: χ2 = 55.161, df = 2).
Table 2.
Recovery of neurosensation in buccal mucosa below incison line
| 10 Days | 8 Weeks | 24 Weeks | p Value | S/NS | |
|---|---|---|---|---|---|
| Number of patients | 25 | 25 | 25 | ||
| Buccal fine touch sensation present | 2 (8 %) | 2 (8 %) | 24 (96 %) | <0 001 | S |
| Buccal pin prick sensation present | 2 (8 %) | 3 (12 %) | 24 (96 %) | <0.001 | S |
| Two point discrimination present | 2 (8 %) | 2 (8 %) | 24 (96 %) | <0.001 | S |
S Significant, NS Non significant
Table 3 summarizes recovery of facial sensation corresponding to infraorbital nerve distribution after Le Fort I osteotomy. At 10 days 20 patients (80 %), responded to fine touch and two point discrimination test while at the end of 24 weeks, all patients (100 %) responded to both the sensations. Statistically significant difference was observed over a period of 24 weeks in the recovery of facial sensation to fine touch (χ2 = 7.609, df = 2, p = 0.022) and two point discrimination (χ2 = 10.714, df = 2, p = 0.005). Recovery of pin prick sensation at 10 days was (96%), while at 8 and 24 weeks, all patients (100 %) responded to pin prick. No statistically significant difference was observed (χ2 = 2.027, df = 2, p = 0.363).
Table 3.
Recovery of facial sensation along the distribution of infraorbital nerve
| 10 Days | 8 Weeks | 24 Weeks | p Value | S/NS | |
|---|---|---|---|---|---|
| Number of patients | 25 | 25 | 25 | ||
| Facial fine touch sensation present | 2 (8 %) | 2 ( 8%) | 24 (96 %) | 0.022 | S |
| Facial pin prick sensation present | 2 (8 %) | 3 (12 %) | 24 (96 %) | 0.363 | S |
| Facial two point discrimination present | 2 (8 %) | 2 (8 %) | 24 (96 %) | 0.005 | S |
S Significant, NS Non significant
Tooth sensibility after Le Fort I osteotomy following electric pulp testing and ethyl chloride spray testing (Table 4) revealed that recovery took place in 3 patients (12 %) in incisor region at 10 days while only 2 (8 %) patients showed recovery in premolar and molar region by this time, although at the end of 24 weeks, all the patients (100 %) showed full recovery to tooth sensibility. Results for all the three regions were found to be statistically significant over this time period (incisor region: χ2 = 58.069, df = 2, premolar region: χ2 = 62.132, df = 2, molar region: χ2 = 62.132, df = 2).
Table 4.
Recovery of tooth sensibility following electric pulp testing and ethyl chloride (thermal) testing
| 10 Days | 8 Weeks | 24 Weeks | p value | S/NS | |
|---|---|---|---|---|---|
| Number of patients | 25 | 25 | 25 | ||
| Incisor region (positive) | 3 (12 %) | 24 (96 %) | 25 (100 %) | <0.001 | S |
| Pre-molar region (positive) | 2 (8 %) | 24 (96 %) | 25 (100 %) | <0.001 | S |
| Molar region (positive) | 2 (8%) | 24 (96 %) | 25 (100 %) | <0.001 | S |
S Significant, NS Non significant
Only one patient had signs and symptoms of maxillary sinusitis at 10 days and 8 weeks post-operatively, which totally resolved by 24 weeks (Table 5). Radiographic picture was not confirmatory. Statistically no significant difference was observed in maxillary sinusitis following Le Fort I osteotomy over this time interval (χ2 = 1.027, df = 2, p = 0.598).
Table 5.
Signs and symptoms of maxillary sinusitis
| 10 Days | 8 Weeks | 24 Weeks | p Value | S/NS | |
|---|---|---|---|---|---|
| Number of patients | 25 | 25 | 25 | ||
| Positive | 1 | 1 | 0 | 0.598 | NS |
S Significant, NS Non significant
Patients were evaluated for vascular complications like epistaxis and intra oral bleeding till first week post-operatively and none occurred in any of the patients. No evidence of aseptic necrosis was reported in any of the patients during the post-operative period.
Incidence of unfavourable fractures occurring on the operation table was judged clinically by the operating surgeon. No unfavourable fractures could be detected. Although, the findings were not confirmed by CT scan or other diagnostic modalities. None of the patients revealed any signs of ophthalmic complications like decreased visual acuity, restriction of eyeball movements or diplopia when reviewed during the immediate post-operative period and at 8 weeks post-operatively.
Maxilla was stable in all the 25 patients following rigid fixation of downfractured maxillary segment when checked manually at various post-operative intervals.
The overall post-operative complication rate was 4 %, with neurosensory deficit and loss of tooth vitality being the most frequent findings and recovery taking place in almost all the patients within the given follow-up period. Maxillary sinusitis was reported in 1 patient but the radiological picture was not in conformation with clinical findings.
Discussion
The Le Fort I osteotomy is one of the most frequently performed orthognathic surgical procedure these days. Its technical ease, broad application to resolve many functional and aesthetic problems and dependability of its results has made it the workhorse of orthognathic surgery [5].
Kramer et al. [2] conducted a prospective study on intra and perioperative complications of the Le Fort I osteotomy in a large series of patients and found the overall complication rate to be 6.4 %. The authors concluded that patients with major anatomic irregularities were at an increased risk for intra and perioperative complications.
Individual complications which have been evaluated in the present study, their pathophysiology, intra and post-operative considerations, preventive aspects and comparison with various studies in literature are discussed herewith.
Intraoral Neurosensory Deficit
The Le Fort I osteotomy most often causes an alteration in the sensation in the maxillary teeth, buccal mucosa and the skin of face. The nasopalatine nerve; the anterior, middle, and posterior superior alveolar nerves; and the small terminal nerves in the buccal mucosa along the incision line between the upper 1st molars are always divided. So, neurosensory deficit in buccal mucosa below the incision line is a common finding following Le Fort I osteotomy procedure.
Kahanberg and Engstrom [6] found that sensibility of oral mucosa to pin prick sensation was markedly decreased inferior to vestibular incision during the first two months after Le Fort I osteotomy but returned gradually and was re-established by 6 months.
Shehab Al-Din et al. [7] in their study on 20 patients for buccal gingivae sensation following Le Fort I osteotomy found that fine touch sensation was present in 19 patients at 6 months while 85 % of patients regained some pin prick sensation at 6 months in the buccal mucosa.
Results in our study showed that buccal mucosa responded to pin prick, fine touch as well as to two point discrimination test in 96 % of the patients at the end of 6 months except for 1 patient who did not respond to any of the three testing modalities.
Extraoral Neurosensory Deficit
The infraorbital nerve may be compressed, retracted or transected inadvertently during subperiosteal dissection. Permanent damage to the infra-orbital nerve should be an avoidable complication.
Karas et al. examined facial sensation in 13 patients before and after surgery using static light touch with von Frey hairs, moving touch with a no. 2 sable hair brush and two point discrimination with the Boley’s gauge and reported that after 3 months all the patients achieved a full return to preoperative levels of fine touch. Moving touch showed a similar pattern and two point discrimination improved post-operatively [8].
Similar results were obtained in the study conducted by Kahanberg and Engstrom [6] and Shehab Al-Din et al. [7] wherein cold sensation, pin prick sensation and fine touch sensation on the face returned to the preoperative level in all the patients by 6 weeks post-operatively.
Results of our study are in conformation with the previous studies wherein infraorbital neurosensory recovery took place in 96 % of patients at 2 months while at the end of 6 months all the patients responded to pin prick sensation, fine touch sensation and two point discrimination test.
Tooth Sensibility
A bone-cut within 5 mm of the apices of the teeth should be avoided as this might lead to devitalization of those teeth [6]. However, when superior repositioning of the maxilla by more than 6 mm is indicated, this margin of 5 mm is not always feasible because of the position of the infraorbital foramen [1].
Kahanberg and Engstrom evaluated the post-operative effects of Le fort I osteotomy in relation to tooth sensibility. They concluded that tooth sensibility is lost in over 90 % of teeth immediate post-operatively but gradually returns by 18 months in almost all teeth. At 6 months post-operatively 70–90 % of teeth studied showed a vital response [6].
De Jongh et al. compared electric and thermal pulp testing of 10 patients after Le Fort I osteotomy with 10 matched controls who had not undergone osteotomy. The mean time after surgery was 14 months and they reported that 71% of 128 teeth were responsive to electric and thermal pulp stimulation, as opposed to 93 % of 136 teeth in the controls [9].
In our study all teeth responded to electric pulp stimulation and ethyl chloride (thermal) testing at the end of 6 months post-operatively, while at 10 days post-operatively only 8–12 % of teeth were responsive. This difference in findings may be due to the fact that no segmentalization of maxilla was carried out in our study which has been attributed as the main factor responsible for non-vitality of teeth.
Maxillary Sinusitis
Possible explanations for post-operative maxillary sinusitis following Le Fort I osteotomy were pre-existing sinus disease or due to some non-viable bone fragments left in the maxillary sinus [10]. Significant infections such as abscesses or maxillary sinusitis occurred in 1.1 % patients in a large study conducted by Kramer et al. [2] on 1,000 patients who underwent Le Fort I osteotomy.
In our study, only 1 patient had signs and symptoms of maxillary sinusitis at 10 days and 8 weeks post-operatively, which totally resolved by 24 weeks. Patient complained of mild pain and heaviness in the maxillary sinus region. Water’s view radiograph was taken to confirm the clinical findings but radiographically no significant findings were observed and were not confirmatory of maxillary sinusitis.
It has been observed that careful manipulation of surgical field, proper aseptic technique and keeping sinus free of any non-viable bone fragments may help in preventing such post-operative occurrence of maxillary sinusitis [10].
Vascular Complications
Bleeding after Le Fort I osteotomies primarily takes the form of epistaxis, which can be anterior or posterior or both. Isolated anterior epistaxis may be the result of a traumatic intubation procedure or secondary to stripping the nasal mucosa off the underlying nasal floor and septal areas. Haemorrhage from both nares is suggestive of an injury to an artery posteriorly [11].
Friehofer reported a rate less than 1 % [12] while Kramer et al. [2], in a prospective study of 1,000 patients, described extensive bleeding requiring blood transfusion in 11 (1.1 %) patients. More serious bleeding may arise from the operation area because of incorrect instrumentation, particularly when the bone-cut or the osteotome is placed too high into the pterygopalatine fossa [1]. The internal maxillary artery and their branches i.e. sphenopalatine artery and ascending palatine artery are most vulnerable to damage in their course through pterygopalatine fossa [13]. Use of right angled saw to separate the maxilla from pterygoid plates has been proposed by Lanigan and Guest to improve the safety of dysjunction [14].
Post-operative epistaxis following Le Fort I osteotomy is very rare, with an incidence of 0.75 % [15]. In the series of cases of haemorrhage in literature following Le Fort I osteotomies, the vast majority of initial episodes occurred within the first 14 days post-operatively [11]. In a study conducted by Regan and Bhardwaj [16] no patient had post-operative arterial or venous haemorrhage that required return to operation theatre. In our study all the patients recovered well post-operatively without any vascular complications.
It may be possible to treat the patient with only bed rest and sedation if bleeding is minor in nature. Recurrent bleeding and bleeding that fails to respond, requires definitive therapy. Anterior or posterior nasal packing for 3–5 days is the standard method for treating epistaxis. In case this is unsuccessful in arresting hemorrhage, then packing of maxillary sinus, specific artery ligation, angiography and embolization of the internal maxillary artery, or internal maxillary artery occlusion with transcatheter electrocoagulation could be considered. Ligation of external carotid artery has also been described but this procedure has been criticized as collateral circulation across the midline can allow bleeding to continue even after the external carotid artery ligation [11].
Aseptic Necrosis
The risk of aseptic necrosis is increased with multisegment Le Fort I osteotomies and is unlikely to occur with a one-piece Le Fort I osteotomy.
Kramer et al. in their study on 1,000 patients found that only 2 patients (0.2 %) experienced an aseptic necrosis of the alveolar process. In one case the maxilla was mobilized 9 mm anteriorly after transversal segmentation; in another patient an anterior displacement of 10 mm resulted in a subtotal aseptic necrosis of the maxillary alveolar process [2].
In a study conducted by Mol De et al. [1] on 410 patients, necrosis of part of the maxilla was seen in one case. Lanigan reviewed literature after sending questionnaire pertaining to aseptic necrosis following orthognathic surgery to all oral and maxillofacial surgeons in North America. Fifty-one cases of aseptic necrosis were reported [17].
In our study, post-operative healing in all the patients was good without any signs of necrosis like dehiscence, periodontal defects or complete necrosis of maxillary segment. This may be attributed to selection of cases in which no segmentalization of maxilla was carried out.
Unfavourable Fractures
Examples of unfavourable fractures include pterygoid plate fracture, sphenoid bone fracture and middle cranial fossa fracture. Lanigan and Guest in their investigations of pterygomaxillary dysjunction using a curved osteotome have described high fractures of pterygoid plates with subsequent disruption of the pterygopalatine fossa and possible fracture extending to base of skull [14]. In our study, no unfavourable fractures were detected clinically on the surgical table although the clinical findings were not confirmed by radiographs or CT scans.
Ophthalmic Complications
Potential ophthalmic complications following Le Fort I osteotomy include decrease in visual acuity, extraocular muscle dysfunction, neuroparalytic keratitis and lacrimal apparatus problems including epiphora [18].
Bendor-Samuel et al. [3] reported a left Occulomotor palsy following a Le Fort I osteotomy occurring as a result of a fracture of the base of skull, leading to a cavernous sinus injury with probable thrombosis and carotid-cavernous fistula. Newlands et al. reported a rare case of an ipsilateral sixth nerve palsy and partial third nerve palsy following a Le Fort I osteotomy and proposed fracture at superior orbital fissure as injury mechanism [19].
No ophthalmic complications were reported clinically in our study. None of the patients revealed any signs of decreased visual acuity, restriction of eyeball movements, diplopia or epiphora when reviewed immediately post-operatively and at 8 weeks post-operatively. This also supports our previous finding of no occurrence of unfavourable fractures which are usually the cause of these ophthalmic complications.
Maxillary Instability
Insufficient bone contact, insufficient bridging of the defect and poor or improper fixation may lead to maxillary instability post-operatively. After 4 weeks of intermaxillary fixation, slight movement of the maxilla is normally noted, disappearing once functional forces are applied to the maxilla [1].
In a retrospective study on the complications by Mol De et al. [1], Sufficient bone-contact was not attained in one case in which the maxilla, mobilized via a Le Fort I osteotomy, was moved upwards, such that after one year a “floating maxilla” was diagnosed, giving rise to chewing problems.
In the present study maxilla was stable in all the 25 patients following fixation of downfractured maxillary segment with four miniplates, two on either side of osteotomy cut. Use of rigid fixation using miniplates, assuring proper bone contact and maxillomandibular fixation for 4–6 weeks can prevent this complication to occur post-operatively. Use of rigid fixation has also been reported to cause a decrease in relapse rate post-operatively [20].
Miscellaneous
Besides the complications mentioned in the study, some rarely occurring complications following Le fort I osteotomy such as nasolacrimal duct injury, blindness, deviated nasal septum, carotid-cavernous fistula and total avulsion of lateral segment of palate have been documented [3]. But new innovative techniques and better understanding of anatomy has led to reduction in the incidence of these complications to almost negligible.
In our study overall complication rate was 4 % although various studies in literature mentioned an overall complication rate of 6–9 % [1, 2]. This small difference may be purely a chance occurrence or may be attributed to small sample size in our study and also to the fact that only post-operative complications have been taken into consideration in this study while most of studies in literature takes into account both intra as well as post-operative complications.
Today’s maxillofacial surgeons have at their disposal modern tools and technology. With proper treatment planning, careful instrumentation and optimal presurgical orthodontic treatment, this complication rate can be reduced still further. The surgeon involved must continually reconsider how to provide safer, more effective care to patients. Seemingly small technical issues in the operating room can significantly affect the outcome.
Acknowledgments
The authors thank Dr. David P. Tauro and Dr. Subha Lakshmi S. of Maxillofacial Plastic and Reconstructive Surgery Department, College of Dental Sciences Davangere (Karnataka) India for their valuable guidance during the course of this study.
Conflict of Interest
None declared.
Funding
None.
References
- 1.Mol De, van Otterloo JJ, Tuinzing DB, Greebe RB, Van der Kwast WAM. Intra and early postoperative complications of the Le Fort I osteotomy: a retrospective study on 410 cases. J Craniomaxillofac Surg. 1991;19:217–222. doi: 10.1016/S1010-5182(05)80551-7. [DOI] [PubMed] [Google Scholar]
- 2.Kramer F-J, Baethge C, Swennen G, Teltzrow T, Schulze A, Breten J, Brachvogel P. Intra and perioperative complications of the Le Fort I osteotomy: a prospective evaluation of 1,000 patients. J Craniofac Surg. 2004;15:971–977. doi: 10.1097/00001665-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Bendor-Samuel R, Chen YR, Chen PK. Unusual complications of the Le Fort I osteotomy. Plast Reconstr Surg. 1995;96:1289–1296. doi: 10.1097/00006534-199511000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Wilson MW, Maheshwari P, Stokes K, Wheatley MJ, McLoughlin S, Talbot M, Shults WT, Dailey RA, Wobig JL. Secondary fractures of Le Fort I osteotomy. Ophthal Plast Reconstr Surg. 2000;16:258–270. doi: 10.1097/00002341-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Fonseca RJ (2000) Orthognathic surgery. Oral and maxillofacial surgery; Vol 2, 1st edn. Saunders, London, p 232
- 6.Kahanberg KE, Engstrom H. Recovery of maxillary sinus and tooth sensibility after Le Fort I osteotomy. Br J Oral Maxillofac Surg. 1987;25:68–73. doi: 10.1016/0266-4356(87)90159-8. [DOI] [PubMed] [Google Scholar]
- 7.Shehab Al-Din OF, Coghlan KM, Magennis P. Sensory nerve disturbance following Le Fort I osteotomy. Int J oral Maxillofac Surg. 1996;25:13–19. doi: 10.1016/S0901-5027(96)80005-1. [DOI] [PubMed] [Google Scholar]
- 8.Karas ND, Boyd SB, Sinn DP. Recovery of neurosensory function following orthognathic surgery. J Oral Maxillofac Surg. 1990;48:124–134. doi: 10.1016/S0278-2391(10)80199-5. [DOI] [PubMed] [Google Scholar]
- 9.De Jongh M, Barnard D, Birnie D. Sensory nerve morbidity following Le Fort I osteotomy. J Maxillofac Surg. 1986;14:10–13. doi: 10.1016/S0301-0503(86)80250-8. [DOI] [PubMed] [Google Scholar]
- 10.Bell C, Thrash WJ, Zysset MK. Incidence of maxillary sinusitis following Le Fort I maxillary osteotomy. J Oral Maxillofac Surg. 1986;44:100–103. doi: 10.1016/0278-2391(86)90189-8. [DOI] [PubMed] [Google Scholar]
- 11.Lanigan DT, West RA. Management of postoperative hemorrhage following the Le Fort I maxillary osteotomy. J Oral Maxillofac Surg. 1984;42:367–375. doi: 10.1016/S0278-2391(84)80008-7. [DOI] [PubMed] [Google Scholar]
- 12.Freihofer HP. Latitude and limitation of midface movements. Br J Oral Maxillofac Surg. 1984;22:393–413. doi: 10.1016/0266-4356(84)90047-0. [DOI] [PubMed] [Google Scholar]
- 13.Lanigan DT, Hey JH, West RA. Major vascular complications of orthognathic surgery: hemorrhage associated with Le Fort I osteotomies. J Oral Maxillofac Surg. 1990;48:561–573. doi: 10.1016/S0278-2391(10)80468-9. [DOI] [PubMed] [Google Scholar]
- 14.Lanigan DT, Guest P. Alternative approaches to pterygomaxillary separation. Int J Oral Maxillofac Surg. 1993;22:131–138. doi: 10.1016/S0901-5027(05)80236-X. [DOI] [PubMed] [Google Scholar]
- 15.Solomons NB, Blumgart R. Severe late-onset epistaxis following Le Fort I osteotomy: angiographic localization and embolization. J Laryngol Otol. 1988;102:260–263. doi: 10.1017/S0022215100104670. [DOI] [PubMed] [Google Scholar]
- 16.O’ Regan B, Bhardwaj G. Prospective study of the incidence of serious posterior maxillary haemorrhage during a tuberosity osteotomy in low level Le Fort I operations. Br J Oral Maxillofac Surg. 2007;45:538–542. doi: 10.1016/j.bjoms.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Lanigan DT, Hey JH, West RA. Aseptic necrosis following maxillary osteotomies: report of 36 cases. J Oral Maxillofac Surg. 1990;48:142–156. doi: 10.1016/S0278-2391(10)80202-2. [DOI] [PubMed] [Google Scholar]
- 18.Lanigan DT, Romanchuk K, Olson CK. Ophthalmic complications associated with orthognathic surgery. J Oral Maxillofac Surg. 1993;51:480–494. doi: 10.1016/S0278-2391(10)80502-6. [DOI] [PubMed] [Google Scholar]
- 19.Newlands C, Dixon A, Altman K. Ocular palsy following Le Fort I osteotomy: a case report. Int J oral Maxillofac Surg. 2004;33:101–104. doi: 10.1054/ijom.2002.0444. [DOI] [PubMed] [Google Scholar]
- 20.Yoon HJ, Rebellato J, Keller E. Stability of the Le Fort I osteotomy with anterior internal fixation alone: a case series. J Oral Maxillofac Surg. 2005;63:629–634. doi: 10.1016/j.joms.2004.12.013. [DOI] [PubMed] [Google Scholar]


