Abstract
Introduction
The administration of pre and post-operative antibiotics for open reduction and internal fixation of facial fracture is the usual norm followed. Although the benefit of antibiotic has been established in the literature, the value of post-operative administration has been questioned and yet not extensively studied or investigated. There are rising concerns over the duration and undesired effects of antibiotics. The purpose of the study was to evaluate necessity and/or efficacy of post-operative antibiotics in the open reduction of zygomatic and mandibular fracture.
Methods
Sixty patients who underwent open reduction and internal fixation were divided into two groups for the trial. Ab group (30 patients) received pre, intra and post-operative antibiotics. Non-Ab group (30 patients) did not receive post-operative antibiotics though pre and intra-operative antibiotics were administered. Patients were evaluated for post-op infection at the end of 1st and 3rd week after operation.
Results
Among 60 patients, 2 patients (1 from Ab group and 1 from non-Ab group) were infected; so statistically no significant difference in result was obtained (Fisher’s exact test, P value = 1).
Conclusion
In this trial, the use of post-operative antibiotics in the open reduction and internal fixation of facial fracture was shown to confer no benefit/efficacy in reducing the chances of infection.
Keywords: Post-operative antibiotic, Trauma, Zygoma, Mandible, Infection
Introduction
In a developing country, rapid urbanization and increase in motor vehicles with poor road conditions in many places have added to increased number of road traffic accidents. The overall numbers of maxillofacial injuries are alarming. Statistics show that maxillofacial injuries make up to 42 % of all injuries. Zygomatic fracture represents either the most common facial fracture or the second in frequency after nasal fractures. According to some studies, the rate of mandibular fracture also may be as high as 70 %. It makes no doubt that zygomatic maxillary complex (ZMC) and mandibular make bulk of facial fracture.
Most studies indicate a male predilection, with a ratio of ~4:1 over females [1].
In the open reduction and internal fixation of facial fracture, prevention of infection is one of the primary aims of treatment. Therefore strict asepsis and sterilization protocol is mandatory. Also antimicrobial agents can be given to try to prevent post-operative infections [2].
The accepted post-operative infection rate in open reduction and internal fixation of mandibular fractures is ~6.1–6.78 % [3]. The benefit of pre and peri operative antibiotics in the treatment of open fracture (of mandible) has been established in the literature [4, 5]. At the same time there are rising concerns over the adverse effects of antibiotics viz. toxicity, impairment of immune defense mechanism, reactions to normal gut flora, resistance and their duration of administration. Emphasis has been laid on shortening the duration to no longer than necessary period.
The necessity of post-operative antibiotics has not been extensively studied or investigated in the literature (except one noted study) when treating facial fracture (by open reduction and internal fixation). Additionally, if antibiotics are indicated post-operatively, no clear data has been produced to establish a guideline for duration of administration [6].
Excessive, prophylactic and/or over durated use of antibiotics in current clinical practice needs to be investigated and addressed to reduce cost and adverse reactions such as toxicity, impairment of immune defense mechanism, adverse reaction to normal gut flora and induction of resistance or selection of resistant bacteria. In addition, following benefits may be realized; [a] reduced drug administration and handling time, [b] reduced adverse drug reactions and interactions, [c] reduced therapeutic agents, [d] reduced medical and legal liability for surgery associated drug or infectious morbidity in the current practice environment, which is sensitive to adverse clinical outcome [7].
Materials and Methods
Among the cases who reported from 2008 to 2010, for operative treatment of facial fractures ZMC and mandibular fracture were taken in this study as representative of facial fractures as they are most commonly found); those who met the inclusion criteria and who gave consent by own free were included in this study. Thirty patients who were diagnosed to have sustained zygomatic maxillary complex fractures and 30 who were having mandibular fracture were selected. Institutional review board approval was obtained. All data were analyzed by a biomedical statistician.
Inclusion Criteria
Patients above 15 years and below 65 years of age.
Open reduction and internal fixation of either mandibular (at least 1 fracture) or ZMC fracture with or without minimally displaced other facial bone fracture which requires intervention
Patients reporting for follow-up till at least 3 weeks post-operatively
Patients with controlled hypertension/diabetes mellitus.
Exclusion Criteria
Fractures infected at the time of treatment.
Severely displaced/or comminuted zygomatic fracture
Severely comminuted mandibular fracture
Patients failing to report for follow-up till 3 weeks post-operatively
Patients with immuno-compromising status
Fracture purely pathologic (pathologic fracture)
The patients meeting the inclusion criteria were divided into two groups, both groups received pre and intraoperative antibiotics. One surgeon operated all the cases.
Ab-group: receiving post operative antibiotics.
- Non-Ab group: not receiving post-operative antibiotics.
- Sample size was 30 for each group (each group consisted of 15 zygomatic fractures +15 mandibular fractures)
- Patients shall be evaluated for post-op infection at the end of 1st and 3rd week after operation.
Table 1.
Master chart for group Ab
| Patient no | Age | Sex | Fracture location | Medical co-morbidity | Interval between injury and operation | Approach | Infection |
|---|---|---|---|---|---|---|---|
| 1 | 22 years | M | Lt ZMC | None | 7 days | Intraoral | No |
| 2 | 33 years | M | Lt ZMC | None | 8 days | Intraoral + extraoral | No |
| 3 | 28 years | M | Lt ZMC + orthopaedic | None | 2 days | Intraoral | No |
| 4 | 23 years | M | Rt ZMC | HBSAg positive | 2 days | Intraoral | No |
| 5 | 27 years | M | Lt ZMC | None | 1 day | Intraoral | No |
| 6 | 45 years | M | Lt ZMC + Lt parasymphysis | None | 4 days | Intraoral + extraoral | No |
| 7 | 32 years | M | Lt ZMC + Lt frontal bone + dentoalveolar | None | 6 days | Intraoral | No |
| 8 | 43 years | M | Rt ZMC + orthopaedic | None | 4 days | Intraoral | No |
| 9 | 25 years | M | Rt ZMC | None | 5 days | Intraoral + extraoral | No |
| 10 | 23 years | M | Rt ZMC | None | 3 days | Intraoral + extraoral | No |
| 11 | 28 years | M | Lt ZMC | None | 7 days | Intraoral + extraoral | No |
| 12 | 46 years | M | Lt ZMC | None | 5 days | Intraoral + extraoral | No |
| 13 | 30 years | M | Lt ZMC | None | 1 day | Intraoral | No |
| 14 | 20 years | M | Rt ZMC | None | 1 day | Intraoral + extraoral | No |
| 15 | 25 years | M | Lt ZMC | None | 27 days | Intraoral | No |
| 16 | 22 years | F | Parasymphysis | None | 3 days | Intraoral | No |
| 17 | 24 years | M | Parasymphysis | None | 5 days | Extraoral | No |
| 18 | 28 years | M | Parasymphysis | Asthma | 8 days | Intraoral | No |
| 19 | 47 years | M | Parasymphysis | DM | 5 days | Intraoral | No |
| 20 | 36 years | M | Parasymphysis | HTN | 7 days | Intraoral | No |
| 21 | 28 years | M | Parasymphysis + Angle | None | 1 day | Intraoral + extraoral | No |
| 22 | 28 years | M | Parasymphysis + subcondylar | None | 3 days | Intraoral + extraoral | Yes |
| 23 | 40 years | M | Parasymphysis | HTN | 6 days | Extraoral | No |
| 24 | 19 years | M | Parasymphysis | None | 4 days | Intraoral | No |
| 25 | 28 years | M | Body + angle | None | 3 days | Intraoral | No |
| 26 | 32 years | M | Parasymphysis | DM | 2 days | Intraoral | No |
| 27 | 33 years | M | Parasymphysis | DM | 6 days | Intraoral | No |
| 28 | 22 years | M | Parasymphysis + angle | None | 3 days | Intraoral | No |
| 29 | 42 years | M | Parasymphysis | None | 3 days | Intraoral | No |
| 30 | 38 years | M | Parasymphysis + subcondylar | None | 4 days | Intraoral | No |
| Patient no. | Age/sex | 1st week follow-up | 3rd week follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Fever | Swelling | Purulent discharge | Fistulae | Fever | Swelling | Purulent discharge | Fistulae | ||
| 1 | 22/M | No | No | No | No | No | No | No | No |
| 2 | 33/M | No | No | No | No | No | No | No | No |
| 3 | 28/M | No | No | No | No | No | No | No | No |
| 4 | 23/M | Yes | No | No | No | No | No | No | No |
| 5 | 27/M | No | No | No | No | No | No | No | No |
| 6 | 45/M | No | No | No | No | No | No | No | No |
| 7 | 32/M | No | No | No | No | No | No | No | No |
| 8 | 43/M | No | No | No | No | No | No | No | No |
| 9 | 25/M | No | No | No | No | No | No | No | No |
| 10 | 23/M | No | No | No | No | No | No | No | No |
| 11 | 28/M | No | No | No | No | No | No | No | No |
| 12 | 46/M | No | No | No | No | No | No | No | No |
| 13 | 30/M | No | No | No | No | No | No | No | No |
| 14 | 20/M | No | No | No | No | No | No | No | No |
| 15 | 25/M | No | No | No | No | No | No | No | No |
| 16 | 22/F | No | No | No | No | No | No | No | No |
| 17 | 24/M | No | No | No | No | No | No | No | No |
| 18 | 28/M | No | No | No | No | No | No | No | No |
| 19 | 47/M | No | No | No | No | No | No | No | No |
| 20 | 36/M | No | No | No | No | No | No | No | No |
| 21 | 28/M | No | No | No | No | No | No | No | No |
| 22 | 28/M | No | Yes | Yes | No | No | No | No | No |
| 23 | 40/M | No | No | No | No | No | No | No | No |
| 24 | 19/M | No | No | No | No | No | No | No | No |
| 25 | 28/M | No | No | No | No | No | No | No | No |
| 26 | 32/M | No | No | No | No | NO | No | No | No |
| 27 | 33/M | No | No | No | No | No | No | No | No |
| 28 | 22/M | No | No | No | No | No | No | No | No |
| 29 | 42/M | No | No | No | No | No | No | No | No |
| 30 | 38/M | No | No | No | No | No | No | No | No |
Table 2.
Master chart for group non Ab
| Patient no | Age | Sex | Fracture location | Medical co-morbidity | Interval between injury and operation | Approach | Infection |
|---|---|---|---|---|---|---|---|
| 1 | 28 years | M | Lt ZMC | None | 2 days | Intraoral | No |
| 2 | 32 years | M | Rt ZMC + Lt parasymphysis | None | 2 days | Intraoral + extraoral | No |
| 3 | 32 years | M | Lt ZMC | None | 2 days | Intraoral | No |
| 4 | 22 years | M | Lt ZMC | None | 5 days | Intraoral | No |
| 5 | 20 years | M | Lt ZMC | None | 1 day | Intraoral + extraoral | No |
| 6 | 35 years | M | Rt ZMC | None | 5 days | Intraoral + extraoral | No |
| 7 | 25 years | M | Rt ZMC | None | 23 day | Intraoral | No |
| 8 | 38 years | M | Lt ZMC | None | 2 days | Intraoral | No |
| 9 | 18 years | M | Rt ZMC + B/L nasal bone | None | 2 days | Intraoral | No |
| 10 | 42 years | M | Rt ZMC | None | 1 day | Intraoral | No |
| 11 | 28 years | M | Lt ZMC | None | 3 days | Intraoral | No |
| 12 | 34 years | M | Lt ZMC | None | 1 day | Intraoral + extraoral | No |
| 13 | 32 years | M | Rt ZMC | None | 2 days | Intraoral | No |
| 14 | 30 years | F | Lt ZMC | None | 5 days | Intraoral + extraoral | No |
| 15 | 28 years | M | Rt ZMC | None | 1 day | Intraoral | No |
| 16 | 35 years | M | Parasymphysis + subcondylar | None | 3 days | Intraoral | No |
| 17 | 18 years | F | Body | None | 2 days | Intraoral | No |
| 18 | 34 years | M | Parasymphysis | DM | 4 days | Extraoral | No |
| 19 | 30 years | M | Parasymphysis + subcondylar | DM | 4 days | Intraoral | Yes |
| 20 | 23 years | M | Parasymphysis + angle | None | 1 day | Intraoral + extraoral | No |
| 21 | 23 years | M | Parasymphysis + angle | None | 2 days | Intraoral + extraoral | No |
| 22 | 42 years | M | Parasymphysis | None | 9 days | Intraoral | No |
| 23 | 35 years | F | Parasymphysis | None | 6 days | Extraoral | No |
| 24 | 21 years | M | Angle | None | 5 days | Intraoral | No |
| 25 | 24 years | M | Parasymphysis + angle | None | 3 days | Intraoral + extraoral | No |
| 26 | 25 years | M | Angle | None | 1 day | Intraoral + extraoral | No |
| 27 | 28 years | M | Parasymphysis | None | 3 day | Intraoral | No |
| 28 | 34 years | M | Angle | HTn | 5 days | Intraoral | No |
| 29 | 27 years | M | Parasymphysis | None | 2 days | Intraoral | No |
| 30 | 35 years | M | Parasymphysis + angle | None | 3 days | Intraoral | No |
| Patient no | Age/sex | 1st week follow-up | 3rd week follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Fever | Swelling | Purulent discharge | Fistulae | Fever | Swelling | Purulent discharge | Fistulae | ||
| 1 | 28/M | No | No | No | No | No | No | No | No |
| 2 | 32/M | No | No | No | No | No | No | No | No |
| 3 | 32/M | No | No | No | No | No | No | No | No |
| 4 | 22/M | No | No | No | No | No | No | No | No |
| 5 | 20/M | Yes | No | No | No | No | No | No | No |
| 6 | 35/M | No | No | No | No | No | No | No | No |
| 7 | 25/M | No | No | No | No | No | No | No | No |
| 8 | 38/M | No | No | No | No | No | No | No | No |
| 9 | 18/M | No | No | No | No | No | No | No | No |
| 10 | 42/M | No | No | No | No | No | No | No | No |
| 11 | 28/M | No | No | No | No | No | No | No | No |
| 12 | 34/M | No | No | No | No | No | No | No | No |
| 13 | 32/M | No | No | No | No | No | No | No | No |
| 14 | 30/F | No | No | No | No | No | No | No | No |
| 15 | 28/M | No | No | No | No | No | No | No | No |
| 16 | 35/M | No | No | No | No | No | No | No | No |
| 17 | 18/F | No | No | No | No | No | No | No | No |
| 18 | 34/M | No | No | No | No | No | No | No | No |
| 19 | 30/M | No | No | No | No | No | Yes | Yes | No |
| 20 | 23/M | No | No | No | NO | No | No | No | No |
| 21 | 23/M | No | No | No | No | No | No | No | No |
| 22 | 42/M | No | No | No | No | No | No | No | No |
| 23 | 35/F | No | No | No | No | No | No | No | No |
| 24 | 21/M | No | No | No | No | No | No | No | No |
| 25 | 24/M | No | No | No | No | No | No | No | No |
| 26 | 25/M | No | No | No | No | No | No | No | No |
| 27 | 28/M | No | No | No | No | No | No | No | No |
| 28 | 34/M | No | No | No | No | No | No | No | No |
| 29 | 27/M | No | No | No | No | No | No | No | No |
| 30 | 35 | No | No | No | No | No | No | No | No |
Criteria for infection include:
Purulent drainage from surgical or fracture site
Increased facial swelling beyond post-op day 7
Fistula formation at surgical or fracture site with evidence of drainage/pus accumulation
Fever/malaise associated with local evidence of infection viz. swelling, erythema, tenderness or foul smell, etc.
Patients with any of these criteria were considered infected (though post-op swelling beyond day 7 could be due to non-infective reason rarely, which was ruled out if at all).
Patients were randomly assigned to both groups.
The selected cases were treated by open reduction and internal fixation with titanium miniplate, using intraoral/extra oral approach or through existing lacerations or combination of the above.
Antibiotics administered were:
Inj. Cefotaxime 1 g/IV/BD
Inj. Metronidazole 100 ml (500 mg)/IV/TID
Method
Case History Review
A standard proforma was used to collect necessary information regarding each case.
Photographic Records
Photographic record was maintained for all patients by taking pre operative photograph of facial profile, fracture site, intra operative photographs, immediate post operative photograph of suture line, photograph of suture line at the end of the 1st and 3rd week after operation.
Radiographic Records
Pre operative para-nasal sinus (PNS) view and sub-mento vertex (SMV) view for evaluation of fracture segment and its displacement were taken. Immediate post-operative PNS radiograph was taken to evaluate the fracture reduction and the position of the plate(s) (Table 3).
Table 3.
Location of fractures
| Location of fracture | No. of cases in Ab group | No. of cases in non-Ab group | Total no. of fractures | No. of infections |
|---|---|---|---|---|
| Parasymphysis | 14 | 11 | 25 | 1 (Ab) + 1(non-Ab) |
| Body | 1 | 1 | 2 | 0 |
| Angle | 3 | 7 | 10 | 0 |
| Condyle | 2 | 2 | 4 | 0 |
| Total | 20 | 21 | 41 | 2 |
| (Zygomatic fracture) | ||||
| Lt ZMC | 10 | 8 | 19 | 0 |
| Rt ZMC | 5 | 7 | 11 | 0 |
| Total | 15 | 15 | 30 | 0 |
Examination of the Patient
Complete case history, neurological evaluation to rule out head/cervical spine injury (Table 4)
General physical examination to ascertain the absence of any associated injury of thorax, abdomen, genitourinary tract or long bones
Table 4.
Any habits
| Habit | No. of cases in Ab group | No. of cases in non-Ab group | No. of infections |
|---|---|---|---|
| Cigarettes smoking | 3 | 1 | 0 |
| Tobacco chewing | 2 | 2 | 1 |
| Alcohol intake | 4 | 2 | 0 |
| More than 1 habit | 9 | 9 | 1 |
| None | 12 | 16 | 0 |
Local Examination
Inspection and palpation of the soft tissues followed by examination of the underlying hard tissue (Table 5).
Presence of oedema, ecchymosis, hematoma
Presence of extra or intra oral wounds
Jaw opening/tenderness at injury site
Ocular/orbital findings
Presence of infection/facial asymmetry if at all
Table 5.
Teeth involved in line of fracture (for mandibular)
| Nature of injury | No. of cases in Ab group | No. of cases in non-Ab group | No. of infections |
|---|---|---|---|
| Avulsion | 2 | 2 | 1 (Ab) + 1(non-Ab) |
| Tooth fracture | 1 | 1 | 0 |
| Fracture line between 2 teeth | 15 | 16 | 0 |
| Total | 18 of 20 fractures | 19 of 21 fractures | 2 of 41 fractures |
Investigations
PNS, SMV radiograph
PA mandible/OPG
PA view of chest radiograph
Apart from these, routine blood and urine investigations, electrocardiogram and all standard investigations required for general anaesthesia were done.
Surgical Protocol
Surgical Technique
Nasotracheal intubation, opposite to the fracture side, was carried out. The patients were painted and draped according to standard aseptic protocol. Surgical approaches for all the fractures were either through intra oral/extra oral/through existing lacerations/combination of above.
Extra oral Approach
First the site was cleaned using betadine solution and was infiltrated with 2 % xylocaine with 1:80,000 adrenaline. Adequate exposure of the fractured segment was done by appropriate incision in the F-Z (fronto-zygomatic) region or sub-mandibular or pre-auricular or other areas including existing CLW (contused lacerated wound) as required. The segments were manipulated, properly reduced and cheek fullness/prominence (for ZMC#), occlusion (for mandibular #) were checked. Intimate adaptation of the miniplate was done and plate(s) was/were fixed with 2 × 6 mm/2 × 8 mm titanium screws.
Intra oral Approach
First the site was cleaned and infiltrated as mentioned above. Standard intra oral upper/lower vestibular incision was given, adequate dissection carried out and fracture site was exposed. Intimate adaptation of the plate was done to the underlying bone and the plate(s) was/were fixed using 2 × 6 or 2 × 8 mm screws.
Care was taken to remove loose bone fragments (where necessary) and not injure the infra orbital neurovascular bundle. After adequate fixation, the area was irrigated thoroughly with betadine and saline. After haemostasis, the wound was closed with 4-0 vicryl (continuous suture) and the skin with 5-0 ethilon (extra orally, where required). An adhesive pressure bandage was given. (Table 6).
Table 6.
Approach to the fracture site
| Approach | No. of cases in Ab group | No. of cases in non-Ab group | Total no. of cases | No. of infections |
|---|---|---|---|---|
| Intraoral approach | 19 | 19 | 38 | 1(Ab) + 1(non-Ab) |
| Extra oral | 2 | 2 | 4 | 0 |
| Combined intra and extraoral/CLW approach | 9 | 9 | 18 | 0 |
| Total | 30 | 30 | 60 | 2 |
Post Operative Care
Thorough irrigation was done intraorally with betadine and normal saline and/or standard cleaning of extra oral wound post operatively. Patients were advised to be on liquid/semi-solid protein rich diet for 1 week with maintenance of meticulous oral hygiene.
Patients of group Ab were kept post operatively on the following regimen:
Injection cefotaxime 1 g/IV/BD 5 days
Infusion metronidazole 100 ml (500 mg)/IV/TID 5 days
Injection diclofenac sodium 3 cc/IM/BD 3 days
Injection dexamethasone 8 mg/IV stat dose intra-op followed by 4 mg/IV/TID on 1st post operative day and tapered thereafter
Injection ranitidine 2 cc/IV/BD
Chlorhexidine mouthwash QID for 15 days
Injection ondansetron 2 cc/IV/SOS
Patients of group non-Ab were kept in the same regimen but cefotaxime and metronidazole were not administered post-operatively.
During post operative evaluation, patients were examined thoroughly for any sign of infection at the end of 1st and 3rd weeks (Tables 1, 2).
Statistical Analysis
Statistical analysis of obtained data was carried out by Fisher’s exact test. One infection in either group was seen. Both infections were seen in the mandibular fracture patient. Statistically no significant difference was obtained. (Fisher’s exact test, P value = 1).
Result
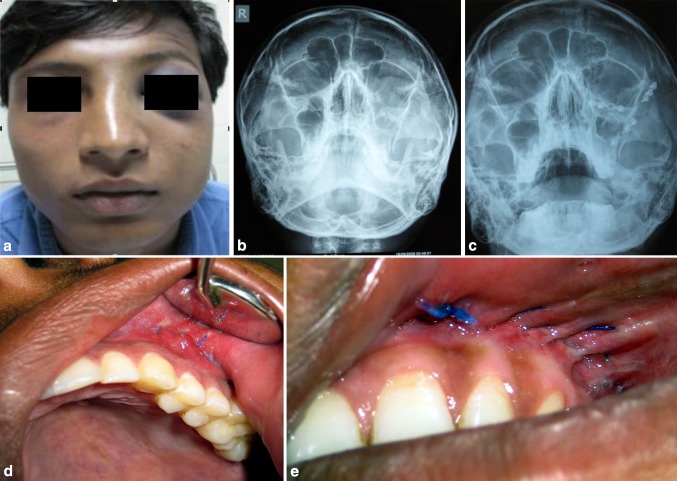
Sixty patients were enrolled in the study, 30 patients having zygomatic maxillary complex fracture (ZMC) and 30 having mandibular fracture(s) (Figs. 1, 2). All patients were followed-up for a minimum of 3 weeks post-operatively. In Ab group 13 patients had additional fracture/more than one fracture (8 ZMC patients had additional fracture elsewhere in the body and 5 patients had more than one fracture of mandible). In non-Ab group, 6 patients had more than one fracture of mandible (all ZMC fracture cases in non-Ab group had no other additional fracture).
Fig. 1.
Patient 1 (ZMC fracture) group non-Ab, a preoperative photograph, b preoperative and postoperative PNS radiograph, c postoperative follow-up intraoral photograph, d at the end of 1st week, e at the end of 3rd week
Fig. 2.
Patient 2 (mandibular fracture) group Ab, a preoperative photograph, b preoperative intraoral photographs, c preoperative OPG, d 1st week postoperative, e 3rd week postoperative, f 5th week postoperative
The age range was 18–47 years with a mean age of 30 years (Table 7). There were 56 male and 4 female patients (Table 8). The total time taken was <3 h for all cases. There were 2 infections (1 in group Ab and 1 in group non-Ab). Since the number of post-operative infection was found to be same in both the groups, no statistically significant difference was obtained. (Fisher’s exact test, P value = 1).
Table 7.
Age incidence
| Age group | No. of cases in Ab group | No. of cases in non-Ab group | No. of post-operative infections |
|---|---|---|---|
| 15–20 | 2 | 3 | 0 |
| 21–30 | 16 | 14 | 1(Ab) + 1(non-Ab) |
| 31–40 | 7 | 11 | 0 |
| 41–50 | 5 | 2 | 0 |
| Total | 30 | 30 | 2 |
Table 8.
Sex incidence
| Sex | No. of cases in Ab group | No. of cases in non-Ab group | Total no. of cases | No. of infections |
|---|---|---|---|---|
| Male | 29 | 27 | 56 | 1(Ab) + 1(non-Ab) |
| Female | 1 | 3 | 4 | 0 |
| Total | 30 | 30 | 60 | 2 |
Both the infections occurred in males (incidentally both were smokers). Purulent drainage from surgical site and increased facial swelling were observed in both the infected cases. Infection was noted in group Ab at 1st week post-op whereas in group non-Ab it was noted at 3rd week post-op. Both the infected patients had parasymphysis and subcondylar fracture, in both of them closed reduction was done for condylar fractures and only parasymphysis region was exposed which subsequently got infected. The infected surgical sites were successfully treated with local incision and drainage and proper antibiotic therapy. None of the infected patients required hospitalization or hardware removal.
Another unexpected finding was that in 3 patients of group Ab, (all mandibular fracture case) wound gaping was seen at 1st week post-op. No such problem was observed in group non-Ab. For all these cases resuturing was performed after thorough irrigation and the wounds subsequently healed uneventfully. Also noted during follow-up period was evidence of fever at the end of 1st week in 2 patients, 1 each from Ab group and non-Ab group (both ZMC # case). There was no other finding in both the patients that could be indicative of infection; they were treated symptomatically with paracetamol. No antibiotics were given to both of them and they were recalled for observation. It subsided after 1 day.
Discussion
The fast, modern and mechanical life nowadays has led to an increase in the incidence of trauma including that of maxillofacial skeleton significantly (Table 9).
Table 9.
Etiology
| Cause of injury | No. of cases in Ab group | No. of cases in non-Ab group | Total no. of cases | No. of infections |
|---|---|---|---|---|
| RTA | 24 | 26 | 50 | 1(Ab) + 1(non-Ab) |
| Work related/fall | 4 | 1 | 5 | 0 |
| Assault | 2 | 3 | 5 | 0 |
| Sports injury | 0 | 0 | 0 | 0 |
| Miscellaneous | 0 | 0 | 0 | 0 |
| Total | 30 | 30 | 60 | 2 |
In order to achieve satisfactory function and cosmesis, open reduction and internal fixation is often necessary. If not carried out properly, this is associated with significant morbidities including infection, non-union, mal-occlusion, plate fracture, orbital complication, etc. [8]. Out of the various noted complications, post-operative infection has generated concern and controversy and has been investigated again and again throughout world literature [9]. Serious infective complication such as orbital cellulitis has also been reported after ZMC fracture [10].
Routine application of standard surgical principle and strict sterilization will result in low infection rate that are acceptable for most surgical procedures. However, there are surgical procedures that, in spite of strict adherence to surgical protocol, have an unacceptably high incidence of post surgical infection. In these situations, the prudent use of antibiotic prophylaxis will lower the level of infection to acceptable levels [5].
It is important to remember that the establishment of an infection depends upon a balance between the bacterial challenge and the host defences. Inoculation of a surgical wound by a large number of virulent bacterias will result in the establishment of an infection, even when the host defences are intact. Several well known factors, such as prolonged operation time, advanced age, malnutrition and a prolonged preoperative hospital stay causes increased infection rates. The use of short term antibiotic prophylaxis eliminates their influence on the incidence of post-operative infections [5].
The use of antibiotics to control post-operative infection has to be based on sound scientific rationale. Concerns regarding the adverse effects need to be addressed. Question also arises whether these antibiotics are really necessary or not.
Carefully controlled studies in animals and humans initially defined the principles of antibiotic prophylaxis and divided the surgeries on the basis of risk of infection as:
CLASS 1 surgery—clean surgery—has an infection rate of ~2 %
CLASS 2 surgery—clean–contaminated surgery—transoral surgeries are considered to be in this class, expected infection rate is 10–15 %
CLASS 3 surgery—contaminated surgery—fractures of the mandible involving the tooth bearing region. Infection rate here is 20–30 %.
CLASS 4 surgery—dirty surgery—if the patient presents with evidence of infection of the fracture or the fracture treatment, is delayed in receiving treatment, the wound can be classified as a class 4 (infected wound). Infection rate here is nearly 50 %.
Various studies suggested that use of good surgical technique reduces incidence of infection in class 1 to <1 % and excellent technique and prophylactic antibiotics can reduce the incidence of infection in class 2 to 1 % and in class 3 to <10 % [11–13]. A review article states that shortening of antibiotic prophylaxis and therapy needs to be addressed, which is in accordance to our findings; however it also states that it is entirely not clear whether fewer adverse reactions would occur with shorter courses of antibiotic therapy [14].
The reasons for excessively prolonged antibiotic administration could be due to failure to identify and eliminate the foci of infection, failure to appreciate pharmacodynamics, impact of antibiotic trials on duration, limitations of antibiotic studies as cause for overuse, failure to distinguish between contamination, infection, and inflammation [14].
Recommendations for shorter duration of antibiotic administration were given by the Discussion Forum for various general surgical procedures. According to it, conditions representing contamination do not require postoperative administration since the infectious site is dealt with operatively, and bacteria are effectively removed by host’s defences, wound irrigation, pre and intraoperative administration of prophylactic antibiotics. The forum also stated that the practice to continue antibiotics blindly as long as temperature is elevated or WBC count is high should be abandoned [15]. In our study also we found it true as we encountered the problem of elevated temperature in two patients successfully treated without antibiotic administration.
Even if we think of the cost factor, according to an estimation, antibiotic prophylaxis given for 1 or 3 days is 4 or 12 times more expensive than a single dose prophylaxis [14]. Studies recommend that in minor surgeries like removal of impacted molar tooth, prophylactic antibiotics should not be routinely given [16]. Although facial fractures like ZMC fractures are rarely complicated by orbital infection, again there is evidence like case of orbital sub-periosteal abscess (SPA) and blindness complicating minimally displaced zygomatic complex fracture [17].
The basic question still remains to be answered—whether these antibiotics are necessary or not? Despite the documented benefit, the use of prophylactic antibiotics to prevent post-operative infection in head and neck surgery, in general and in oral and maxillofacial surgery, in particular, has and continues to be the subject of controversy. In fact, many believed that prophylactic antibiotics increased the incidence of suprainfection of surgical sites. After reviewing 131 studies published over 16 years, it was concluded that antibiotic prophylaxis was of value only in certain procedures. However, as majority of these studies were retrospective and a wide variety of procedures, different antibiotics, and various durations of therapy were used, the criteria used for diagnosing an infection were mostly subjective and not well defined.
In our study, as we stated earlier, thorough aseptic procedures were followed during the surgery as well as during the post-operative period which is considered an important factor in reducing the chance of infection.
Both the infections were found in parasymphysis region, both the post-operative infection cases were operated within 4 days of injury whereas no post-operative infection was seen in those who were operated after 4 days of injury. Similarly the duration of surgery for all cases was <3 h, so role of prolonged operation time in increasing rate of infection cannot be commented upon based on our study.
The results of our study show that the number of infection is equal in either group, thus statistically no difference or significance was obtained. This indicates that there is no benefit/efficacy of post-operative antibiotics to control/reduce the infection in open reduction and internal fixation of facial fracture. Our result is in accordance with those studies done previously by Abubaker and Rollert [18] and by Miles et al. [6].
Even avoidance of post-operative antibiotic administration reduces hospitalization of patient preventing complication like development of MRSA strain.
Though in our study, two patients, 1 from Ab group and another from non-Ab group had fever at the end of 1st week postoperatively, there were no other signs or symptoms that could indicate the presence of an infection. Both were managed conservatively (with administration of paracetamol alone) and the fever subsided next day. Also the unexpected finding of wound gaping in 3 cases in Ab group could be due to tension in suture line, hematoma formation or mutilation of flap margins prior to suturing. This finding highlights the importance of suturing procedure and hence it should be carried out meticulously.
The statistical analysis by Fisher’s exact test shows the value of P = 1 which is statistically insignificant. This questions the need for administration of post-operative antibiotics in open reduction and internal fixation of facial fracture.
Because of the relatively small sample size, the results need to be supported by further studies using a larger sample size and providing more data on various confounding variables before we can finally recommend not using post operative antibiotics in the open reduction and internal fixation of facial fracture.
Conflict of interest
None.
Contributor Information
Shridhar D. Baliga, Phone: +919341102665, Email: baliga1974@rediffmail.co.in
Abhinaba Bose, Phone: +919845656218, Email: abhinaba.maxs@gmail.com.
Saurabh Jain, Phone: +919377770905, Email: dr_saurabhjain@yahoo.com.
References
- 1.Nysingh JG. Zygomatico-maxillary fractures with a report of 200 consecutive cases. Arch Chir Neerl. 1960;12:157. [PubMed] [Google Scholar]
- 2.Crossley K, Gardner LC. Task force on prophylactic antibiotics in surgery: antimicrobial prophylaxis in surgical patients. JAMA. 1981;245:722–726. doi: 10.1001/jama.1981.03310320044024. [DOI] [PubMed] [Google Scholar]
- 3.Zallen RD. Discussion—postoperative antibiotic prophylaxis in mandibular fractures: A preliminary randomized, double blind, and placebo—controlled clinical study. JOMS. 2001;59:1419. doi: 10.1053/joms.2001.28272. [DOI] [PubMed] [Google Scholar]
- 4.Peterson Larry J. Antibiotic prophylaxis against wound infections in oral and maxillofacial surgery. JOMS. 1990;48:617–620. doi: 10.1016/s0278-2391(10)80477-x. [DOI] [PubMed] [Google Scholar]
- 5.Peterson Larry J. Controversies in antibiotic prophylaxis in maxillofacial surgery. In: Controversies in Oral and Maxillofacial Surgery, chap 7, pp 95–100
- 6.Miles Brett A, Potter Jason K, Ellis Edward. The efficacy of postoperative antibiotic regimens in open treatment of mandibular fractures: a prospective randomized trial. JOMS. 2006;64:576–582. doi: 10.1016/j.joms.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Jones Ronald N. Antibiotic prophylaxis for surgical infections: summation. Am J Surg. 1992;164:48S–49S. doi: 10.1016/S0002-9610(06)80058-9. [DOI] [PubMed] [Google Scholar]
- 8.Edward TC. The relationship between fracture severity and complication rate in miniplate osteosynthesis of mandibular fractures. Br J Plast Surg. 1994;47:310. doi: 10.1016/0007-1226(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 9.Abubaker AO. Discussion: antibiotic prophylaxis in orthognathic surgery: a 1 day versus 5 day regimen. JOMS. 1999;57:230–232. doi: 10.1016/s0278-2391(99)90664-x. [DOI] [PubMed] [Google Scholar]
- 10.Dhariwal DK, Kittur MA, Farrier JN, Sugar AW, Aird DW, Laws DE. Post-traumatic orbital cellulitis. BJOMS. 2003;41:21–28. doi: 10.1016/s0266-4356(02)00259-0. [DOI] [PubMed] [Google Scholar]
- 11.Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161. [PubMed] [Google Scholar]
- 12.Polk HC, Lopez-Mayor JF. Postoperative wound infection: a prospective study of determinant factors and prevention. Surgery. 1969;66:97. [PubMed] [Google Scholar]
- 13.Stone HH, Haney BB, Kolb LD. Prophylactic and preventive antibiotic therapy. Ann Surg. 1979;189:691–699. doi: 10.1097/00000658-197906000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wittman Dietmar H, Schein Moshe. Let us shorten antibiotic prophylaxis and therapy in surgery. Am J Surg. 1996;172(suppl. 6A):26S–32S. doi: 10.1016/S0002-9610(96)00347-9. [DOI] [PubMed] [Google Scholar]
- 15.Discussion Forum on antibiotic treatment of postoperative abdominal infections (1996) Eur J Surg 567 (suppl)
- 16.Siddiqi A, Morkel JA, Zafar S. Antibiotic prophylaxis in third molar surgery: a randomized double-blind placebo-controlled clinical trial using split-mouth technique. IJOMS. 2010;39:107–114. doi: 10.1016/j.ijom.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Gilhooly MG, Falconer DT, Wood GA. Orbital subperiosteal abscess and blindness complicating a minimally displaced zygomatic complex fracture. BJOMS. 1995;33:185–188. doi: 10.1016/0266-4356(95)90295-3. [DOI] [PubMed] [Google Scholar]
- 18.Abubaker AO, Rollert MK. Postoperative antibiotic prophylaxis in mandibular fractures: a preliminary randomized double blind, and placebo-controlled clinical study. JOMS. 2001;59:1415–1419. doi: 10.1053/joms.2001.28272. [DOI] [PubMed] [Google Scholar]