Abstract
A prospective study on mid-face fractures was carried out in the Department of Oral and Maxillofacial Surgery at College of Dentistry, Indore, from August 2007 to September 2009 to analyze etiology, incidence and patterns of midface fractures and associated ocular injuries. Two hundred patients were included in this study, amongst those who reported to the Department of OMFS, College of Dentistry, Indore. After confirmed diagnosis of mid face fracture all the patients were stratified according to age, sex, cause of the accident, influence of alcohol, location, type of fractures and associated ocular injuries. The study included 200 patients with a mean age of 29.6 years. The most frequently injured patients belonged to the 21–30 year-old age group. The male predilection was 76 %. Road traffic accident was the most common causative factor (64 %), followed by assault (21 %), cases of fall (9.5 %) and other causes (5.5 %). The most common fracture in this study was found to be zygomatic complex fractures (62.5 %) (more in the age group of 21–30 years). This was followed by Lefort II fractures (23 %), multiple fractures (10 %) and Lefort I fractures (6 %), Lefort III fractures (4.5 %) and Naso-ethmoidal fractures (4 %) in descending order. 84.5 % subjects were having ocular involvement. Subconjunctival hemorrhage was present mostly in 83.5 % followed by remaining as corneal injury 15 %, reduced acuity 11.5 %, diplopia 10.5 %, enophthalmos 8.5 %, telecanthus 5 %, hyphema 3.5 %, blindness 3 % and proptosis 0.5 %. Zygomatic complex fractures were the most frequent type of injury that was complicated by blindness or a serious eye injury (61 %). Collection of data regarding the epidemiology of maxillofacial fractures is important because it may assist healthcare providers to provide necessary information for the development and evaluation of preventive measures. Ocular injuries should have an early ophthalmological examination at the time of trauma to detect any kind of ocular dysfunction.
Keywords: Maxillofacial injuries, Road traffic accidents, Ocular injuries, Mid-face fractures
Introduction
Patients with maxillofacial trauma are amongst the most commonly seen cases in Oral and Maxillofacial Surgery Clinics. Maxillofacial fractures are often associated with severe morbidity, functional deficit, disfigurement, and significant financial cost [15, 17]. The incidence, patterns and etiology of maxillofacial fractures are influenced by geographic location, socio economic status of the cohort, and the period of investigation [8, 11, 14, 22].
In developing nations, road traffic accidents [8, 9, 22, 23] are the most frequent etiology and in developed countries assaults [10, 11, 15] are the most frequent etiology. Injuries to the middle third of the face are frequently complicated by injury to the eye, so, early diagnosis and management of ocular injuries is important for prevention of ocular dysfunction.
Little is known about the current epidemiology of mid-face fractures and associated ocular injuries in Madhya Pradesh state of India. The Department of Oral and Maxillofacial Surgery (OMFS), College of Dentistry, Indore treats an of average 10,248 patients each year of which 230 patients are being managed for maxillofacial fracture.
To investigate this group of patients, a study was carried out to analyze etiology, incidence and patterns of mid-face fractures and associated ocular injuries from August 2007 to September 2009.
Aims and Objectives
To study the epidemiology of mid-face fracture in patients.
To assess associated ocular injuries amongst the patients with mid-face fracture.
To assess the different patterns of ocular injuries amongst the same.
Materials and Methods
Two hundred patients were included in this study.
Selection Criteria
Inclusion criteria All clinically and radiographically confirmed mid-face fracture patients with or without ocular injuries were included in this study.
Exclusion criteria Subjects who had already taken any treatment for the trauma and subjects with isolated, maxillary dentoalveolar fracture and mandibular fractures were not included.
After confirmed diagnosis of mid face fracture all the patients were stratified according to age, sex, cause of the accident, influence of alcohol, location, type of fractures and associated ocular injuries in conjunction with the ophthalmologist on a proforma sheet.
Results
During the study period, 200 patients with mid-face fractures were evaluated. In this study 152 (76 %) were males and 48 (24 %) were females, with a male:female ratio of approximately 3.16:1. The average age was 29.6 years, ranging from 3 to 67 years. The peak incidence (47 %) of mid-face fracture was in the age range of 21–30 years (Table 1).
Table 1.
Age distribution of the patients
| Age group | Male | Female | Total |
|---|---|---|---|
| 0–10 | 05 | 02 | 07 |
| 11–20 | 25 | 10 | 35 |
| 21–30 | 76 | 18 | 94 |
| 31–40 | 22 | 07 | 29 |
| 41–50 | 15 | 07 | 22 |
| 51–60 | 07 | 01 | 06 |
| 61–70 | 02 | 03 | 05 |
| Total | 152 | 48 | 200 |
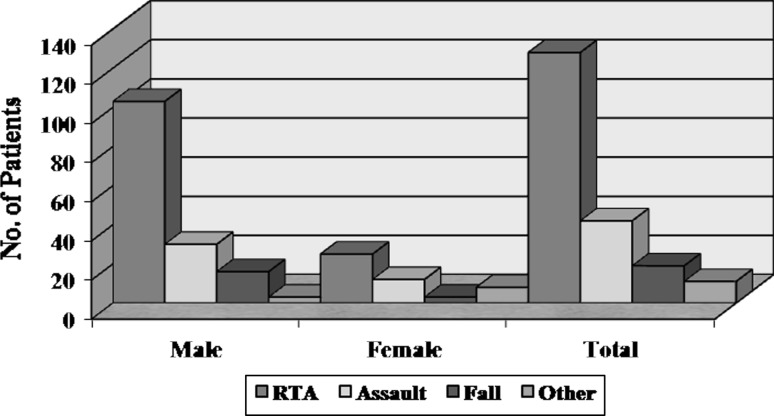
The causes of injury are listed in Graph 1. The most common cause of maxillofacial fracture was road traffic accidents (128 cases; 64 %), followed by assault (42 cases; 21 %), fall (19 cases; 9.5 %), and other causes (11 cases; 5.5 %). Within the category of road traffic accidents, motorcycle accident accounted for 55.4 % followed by collisions of light and heavy vehicles (29.6 %) and bicycle accident accounted for 11.4 % of mid-face trauma (Table 2).
Graph 1.
Distribution of patients according to etiology of the mid face fractures
Table 2.
Type of the road accident in patients with mid face fracture
| Type of RTA | Male | Female | Total |
|---|---|---|---|
| Motorcycle accident | 62 | 09 | 71 |
| Light and heavy vehicle accident | 24 | 14 | 38 |
| Bicycle accident | 14 | 01 | 15 |
| Other | 03 | 01 | 04 |
The incidence of alcoholic patients at the time of injury was 33.5 %. There were 66 males and only one female under the effect of alcohol at the time of injury. There was high incidence of alcohol intake in the age group of 21–30 years.
As shown in Table 3 the most common fracture in this study was found to be zygomatic complex fractures (125 cases; 62.5 %) mostly in the age group of 21–30 years. This was followed by Lefort II fractures (46 cases; 23 %), multiple fractures (20 cases; 10 %) and Lefort I fractures (12 cases; 6 %), Lefort III fractures (9 cases; 4.5 %) and naso-ethmoidal fractures (cases; 4 %) in descending order.
Table 3.
Age range distribution of subjects as per the type of mid face fracture
| Age group | Zygomatic complex fracture | Le Fort I fracture | Le Fort II fracture | Le Fort III fracture | Naso-ethmoidal fracture | Multiple | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | M | F | M | F | M | F | |
| 0–10 | 4 | 2 | 00 | 0 | 00 | 0 | 0 | 00 | 0 | 0 | 00 | 00 |
| 11–20 | 16 | 5 | 00 | 2 | 05 | 1 | 1 | 02 | 1 | 1 | 03 | 01 |
| 21–30 | 44 | 11 | 04 | 2 | 24 | 4 | 0 | 01 | 1 | 1 | 05 | 01 |
| 31–40 | 15 | 6 | 00 | 0 | 05 | 2 | 0 | 01 | 0 | 0 | 03 | 01 |
| 41–50 | 08 | 4 | 02 | 1 | 03 | 2 | 0 | 01 | 0 | 0 | 03 | 01 |
| 51–60 | 05 | 1 | 01 | 0 | 01 | 0 | 0 | 0 | 0 | 0 | 01 | 00 |
| 61–70 | 02 | 2 | 00 | 0 | 00 | 0 | 0 | 0 | 1 | 1 | 00 | 01 |
| Total | 94 | 31 | 07 | 05 | 38 | 08 | 08 | 01 | 05 | 03 | 15 | 05 |
Ocular injuries were present in 169 cases (84.5 %). Sub-conjunctival haemorrhage was present mostly in 167 cases (83.5 %) followed by corneal injury (30 cases; 15 %), reduced acuity (23 cases; 11.5 %), diplopia (21 cases; 10.5), enophthalmos (17 cases; 8.5 %), telecanthus (10 cases; 5 %), hyphema (7 cases; 3.5), blindness (6 cases; 3 %) and proptosis (1 cases; 0.5 %). Other ocular findings such as angle recession, retinal tear, choroid rupture and traumatic mydriasis were not present in this group of patients (Table 4).
Table 4.
Distribution of patients according to type of ocular injuries
| Ocular involvement | Male | Female | Total |
|---|---|---|---|
| Diplopia | 17 | 04 | 21 |
| Enophthalmos | 14 | 03 | 17 |
| Proptosis | 01 | 00 | 01 |
| Reduced acuity | 18 | 05 | 23 |
| Telecanthus | 07 | 03 | 10 |
| Retinal tear | 00 | 00 | 00 |
| Corneal injury | 25 | 05 | 30 |
| Blindness | 04 | 02 | 06 |
| Subconjunctival hemorrhage | 130 | 37 | 167 |
| Hyphema | 06 | 01 | 07 |
| Traumatic mydriasis | 00 | 00 | 00 |
| Angle recession | 00 | 00 | 00 |
| Choroid rupture | 00 | 00 | 00 |
The total number of ocular involvement in the mid-face fractures was significantly higher in the subjects with zygomatic complex fractures (104; 61 %) followed by Lefort II fractures in 44 (26.1 %), multiple fractures (multiple fractures involve a combination of two or more fractures) in 20 (11.9 %), Lefort III fractures in 9 (5.3 %), naso-ethmoidal fractures in 8 (4.7 %) and Lefort I fractures in 2 (1 %) patients.
Discussion
Different studies have shown that there are epidemiological differences in the etiology, type, and site of fracture and in patient characteristics [8, 9, 20, 22, 23].
The higher frequency of maxillofacial injuries among males compared to females is a universal finding in all previous studies [2, 7–9, 11, 22]. The male:female ratio (3.16:1) in our sample was lower than what has been reported by Cavalcanti et al. [8], Cheema and Amin [9] and Ugboko et al. [23] and this finding is in accordance with previous studies from India [13, 22] as well as from other parts of the world [7, 14]. This may be due to the active participation of females in society and consequently they are more susceptible to road traffic accidents and assault.
Cultural and socioeconomic characteristics have significant influence in gender distribution of maxillofacial injuries. In countries such as Austria [12], Japan [14] and Jordan [7] where females participate widely in social activities, the male-to-female ratios for the occurrence of maxillofacial trauma were reduced to 2:1. Conversely, Ahmed et al. [2] reported higher ratio of men to women than other studies (11:1), mostly due to cultural features of the United Arab Emirates, where men usually do outdoor work and few women drive.
This study revealed that the peak incidence of maxillofacial fractures occurred in the 21–30 year age group, with mean age of 29.6 years. Many surveys of maxillofacial fractures reported the same results concerning age [2, 5, 7, 8, 20]. The possible explanation for this was that younger persons involved in intense social interaction and higher rate of mobility, drive motor vehicles carelessly making them more susceptible to road transport accident and interpersonal assault.
Road traffic accidents remain the most frequent cause in the many developing countries, including India [8, 9, 20–24]. The present study supports the findings of these earlier studies, showing that road traffic accidents represents 64 % of all etiological factors. Within the category of road traffic accidents, motorcycle accidents, bicycles accidents and collisions of light and heavy vehicles are important etiological factors. Motorcycles are important means of transport in our region and they accounted for significant number of cases (55.4 %) of traffic accidents in this study. Similar studies have shown that the incidence of motorcycle crashes in other developing countries is about 19–62 % [8, 22].
Eventhough traffic rules and regulations have been enforced, the reasons for this high frequency are difficult to postulate but may be due to inadequate road safety awareness, unsuitable road conditions, violation of the speed limit, old and poorly maintained vehicles without safety features such as anti-lock braking system and energy absorbing materials, large number of overloaded buses, failure to wear seatbelt or helmets, entry into opposite traffic lane, violation of the highway code, abuse of alcohol or other intoxicating agents, inexperienced young drivers, behavioral disorders and socio-cultural insufficiencies of some drivers.
Consumption of alcohol is strongly associated with maxillofacial injuries. Alcohol impairs judgment, brings out aggression, often leads to inter-personal violence and road traffic accident [16, 18]. In the study, 33.5 % of patients were under alcohol influence and males accounted for 99 % of this group. Thus, there should be strong pressure by governments through advertisement and television to outlaw drunk drivers and enforce regulation.
The most common fractures were the zygomatic complex fractures (62.5 %) followed by the Lefort II fractures in 23 % patients which is comparable to previous studies [2, 7, 11].
The reported incidence of ocular injuries in patients with midfacial fractures ranges from 2.7 to 90.6 % [3, 4, 17, 19]. In our study the overall incidence of ocular injuries was found to be 84.5 %, in accordance with the above studies. This large variation from 2.7 to 90.6 % in previous studies depends on the specialty of the examiner, and whether minor injuries were included in addition to major ones.
Sub-conjunctival haemorrhage was present in 83.5 % patients followed by corneal injury in 15 %, reduced acuity in 11.5 %, enophthalmos in 10.5 %, diplopia in 11.5 %, telecanthus in 5 %, hyphema in 3.5 % and blindness in 3 %. Other ocular findings such as angle recession, retinal tear, choroid rupture, proptosis and traumatic mydriasis were not found in this study.
In our study sub-conjunctival haemorrhage was the most common ocular injury and was present in 83.5 % of patients. This compared favorably with previous studies [1, 3, 4] where it was present in 60–74 % of cases [3, 19]. In our series, symptomatic diplopia occurred in 11.5 % of the patients. This is in approximate agreement with a study by Al-Qurainy et al. [1], who found that 19.8 % of patients with midfacial fractures had diplopia and other studies [6, 19].
Enophthalmos following facial trauma should always raise suspicion of an orbital wall fracture and a CT scan is advisable when plain X-rays are negative [1]. Our figures (8.5 %) are closely in accordance with those of Al-Qurainy et al. [1]. Patient’s visual acuity and pupil examination are the “vital signs” of the eye. Al-Qurainy et al. [1] found visual acuity to be impaired in 15.4 %. We found that 11.5 % (23) of patients had reduced visual acuity at the time of injury and out of this three patients had permanent loss in vision. So study shares similar views with the existing studies.
Visual loss or blindness is an uncommon complication of midfacial fractures, occurring in between 0.3 and 3.5 % of cases in reported series [3, 17, 19] and is usually caused by injuries directly to the globe, the optic nerve, or the visual pathway.
In this study blindness was present in 6 (3 %) patients. In four patients it was due to direct injury to globe and in the other two due to traumatic optic neuropathy.
Hyphema or bleeding in the anterior chamber is mostly caused due to tearing of blood vessels at the root of the iris. In this study hyphema was present in 3.5 % patients which is in approximate agreement with a study by Al-Qurainy et al. [1] and other studies [6, 19].
Disruption of the medial canthal ligament results in traumatic telecanthus. In this study traumatic telecanthus present in 5 % of cases.
Al-Qurainy et al. [1], Ansari [5] and Wood [24] noted that zygomatic complex fractures had a significantly higher incidence of visual sequellae (41 %) than other forms of midfacial injury (15 %). As per results in this study patients with ocular injuries were common and more with zygomatic fractures (61 %).
Road traffic accidents is the most common cause of a severe ocular injury in association with a midfacial fracture. Our data suggest that road traffic accidents is the most common cause of ocular injury in a patient with mid facial fractures.
Summary and Conclusion
According to this study, continuous long-term collection of data regarding the epidemiology of maxillofacial fractures is important because it may assist healthcare providers to provide necessary information for the development and evaluation of preventive measures for reducing the incidence of facial injuries, such as the introduction of the seat belt legislation, wearing of helmet, strict adherence of traffic rule and national prevention programmes for alcohol or drug abuse and addiction. This will also help in establishment of clinical and research protocol for effective management of maxillofacial trauma patients.
All patients sustaining midfacial fractures associated with ocular injuries should have an early ophthalmological examination at the time of trauma to detect any kind of ocular dysfunction. This will help maxillofacial surgeons to take necessary action if required before implementing their treatment plan. Many patients sustaining facial injury make recourse to legal or insurance claims. The results of detailed ophthalmic assessment often adds weight to such cases and affect levels of compensation paid.
References
- 1.Al-Qurainy IA, Stassen LF, Dutton GN, Moos KF, el-Attar A. Diplopia following midfacial fractures. Br J Oral Maxillofac Surg. 1991;29(5):291–301. doi: 10.1016/0266-4356(91)90114-K. [DOI] [PubMed] [Google Scholar]
- 2.Al Ahmed HE, Jaber MA, Salem H, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(2):166–170. doi: 10.1016/j.tripleo.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 3.Al-Qurainy IA, Stassen LF, Dutton GN, et al. The characteristics of midfacial fractures and the association with ocular injury: a prospective study. Br J Oral Maxillofac Surg. 1991;29:291. doi: 10.1016/0266-4356(91)90114-K. [DOI] [PubMed] [Google Scholar]
- 4.Amrith S, Saw SM, Lim TC, Lee TK. Ophthalmic involvement in cranio-facial trauma. J Carniomaxillofac Surg. 2000;28(3):140–147. doi: 10.1054/jcms.2000.0138. [DOI] [PubMed] [Google Scholar]
- 5.Ansari MH (2005) Blindness after facial fractures: a 19-year retrospective study. J Oral Maxillofac Surg 63:229–237 [DOI] [PubMed]
- 6.Barry C, Coyle M, Idress Z. Ocular finding in patients with orbitozygomatic complex fractures: a retrospective study. J Oral Maxillofac Surg. 2008;66:888–892. doi: 10.1016/j.joms.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Bataineh AB. Etiology and incidence of maxillofacial fractures in the north of Jordan Oral Surgery. Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31–35. doi: 10.1016/S1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 8.Cavalcanti AL, Bezerra PKM, D. Moraes de Oliveira DM, Granville-Garcia AF (2010) Maxillofacial injuries and dental trauma in patients aged 19–80 years, Recife, Brazil, Rev Esp Cir Oral Maxilofac 32:11–16
- 9.Cheema SA, Amin F. Incidence and causes of maxillofacial skeletal injuries at the Mayo Hospital in Lahore, Pakistan. Br J Oral Maxillofac Surg. 2006;44:232–234. doi: 10.1016/j.bjoms.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 10.Eggensperger N, Smolka K, Scheidegger B, Zimmermann B, Iizuka T (2007) A 3-year survey of assault-related maxillofacial fractures in central Switzerland. J Craniomaxillofac Surg 35:161–167 [DOI] [PubMed]
- 11.Erol B, Tanrikulu R, Görgün B. Analysis of demographic distribution and treatment in 2,901 patients (25-year experience) J Craniomaxillofac Surg. 2004;32:308–313. doi: 10.1016/j.jcms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Gassner R, Tuli T, Moreira R, H€achl O, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004;62:399–407. doi: 10.1016/j.joms.2003.05.013. [DOI] [PubMed] [Google Scholar]
- 13.Gupta AK, Garg R, Gupta A, Bajaj K (2009) A retrospective analysis of 189 patients of maxillofacial injuries presenting to a tertiary care hospital in Punjab, India. J Maxillofac Oral Surg 8:241–245 [DOI] [PMC free article] [PubMed]
- 14.Iida S, Kogo M, Sugiura T, Mima T, Matsuya T. Retrospective analysis of 1,502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001;30:286–290. doi: 10.1054/ijom.2001.0056. [DOI] [PubMed] [Google Scholar]
- 15.Kieser J, Stephenson S, Liston PN, Tong DC, Langley JD. Serious facial fractures in New Zealand from 1979 to 1998. Int J Oral Maxillofac Surg. 2002;31:206–209. doi: 10.1054/ijom.2002.0208. [DOI] [PubMed] [Google Scholar]
- 16.Laverick S, Patel N, Jones DC. Maxillofacial trauma and the role of alcohol. Br J Oral Maxillofac Surg. 2008;46(7):542–546. doi: 10.1016/j.bjoms.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Lim LH, Lam LK, Moore MH, et al. Associated injuries in facial fractures: review of 839 patients. Br J Plast Surg. 1993;46:635. doi: 10.1016/0007-1226(93)90191-D. [DOI] [PubMed] [Google Scholar]
- 18.Maaytah M, Smith SF, Jerjes W, Upile T. The effect of the new 24 h alcohol licensing law on the incidence of facial trauma in London. Br J Oral Maxillofac Surg. 2008;46:28. doi: 10.1016/j.bjoms.2008.07.172. [DOI] [PubMed] [Google Scholar]
- 19.Marin MI, Tejero TR, Dominguez FM, et al. Ocular injuries in midfacial fractures. Orbit. 1998;17:41. doi: 10.1076/orbi.17.1.41.7950. [DOI] [PubMed] [Google Scholar]
- 20.Ravindran V, Nair KSR. Metaanalysis of maxillofacial trauma in the northern districts of Kerala: one year prospective study. J Maxillofac Oral Surg. 2011;10:321–327. doi: 10.1007/s12663-011-0264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sawhney CP, Ahuja RB. Faciomaxillary fractures in North India: a statistical analysis and review of management. Br J Oral Maxillofac Surg. 1988;26:430–434. doi: 10.1016/0266-4356(88)90097-6. [DOI] [PubMed] [Google Scholar]
- 22.Subhashraj K, Ramkumar S, Ravindran C. Pattern of mandibular fractures in Chennai, India. Br J Oral Maxillofac Surg. 2008;46:126–127. doi: 10.1016/j.bjoms.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Ugboko VIC, Udoye C, Olateju SO, Amole AOD. Blindness and visual impairment from severe midface trauma in Nigerians. Int J Oral Maxillofac Surg. 2006;35:127–131. doi: 10.1016/j.ijom.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Wood GD. Blindness following fracture of the zygomatic bone. Br J Oral Maxillofac Surg. 1986;24:12–16. doi: 10.1016/0266-4356(86)90033-1. [DOI] [PubMed] [Google Scholar]