Abstract
Purpose
The purpose of this article was to review our experience in the treatment of complicated mandibular fractures in children using resorbable plates.
Patients and Methods
Records of 14 patients who sustained and presented to our department with complicated fractures of the mandible, and were treated with resorbable plates were retrieved. Permission was sought from and granted by the institution ethical committee. Data extracted included patients’ gender, age, etiology of fracture, nature of fracture and site of the fracture.
Results
Of the 14 patients, there were 10 males and 4 females with a male to female (M:F) ratio of 2.5:1. Their ages ranged from 6 to 15 years, with a mean of 10.14 years. The etiology of the fractures included road traffic accidents (n = 11) and falls (n = 3). Most of the fractures were sustained on the body of the mandible. Majority of the patients had displacement of the fracture segments; 2 patients had comminuted fractures. All the fractures were treated using resorbable plates and healed uneventfully.
Conclusion
Whereas the number of patients in this case series was small, it is worth noting that children sometimes present with complicated fractures of the mandible, thereby necessitating open reduction and internal fixation. Resorbable plates when available and affordable, are an effective option for open reduction and internal fixation of such fractures.
Keywords: Resorbable plates, Mandibular fractures, Children
Introduction
In clinical practice, across all clinical specialities, children constitute a special group of patients. Indeed in oral and maxillofacial surgery too, the management of mandibular fractures in children has special considerations as compared to the management of similar fractures in adults.
The anatomical characteristics of the developing mandible and the presence of tooth buds in the jaws of children, makes the management of mandibular fractures in the pediatric group a challenge and therefore calls for application of different surgical techniques [1, 2].
A number of authors are in agreement that whenever possible, conservative approach be employed in the form of closed reduction [1, 3, 4]. This approach certainly will apply to greenstick, simple, non-displaced fractures. However, children sometimes present with severe fractures in which the closed approach may not be the choice of treatment. The fractures may present with displacement, severe malocclusion, multiple fractures, or comminuted. Under these circumstances, open reduction and internal fixation is the treatment of choice. The use of resorbable plates when available, is an alternative that is gradually getting into active use for fracture fixation in children [5].
The purpose of this article was to review our experience in the treatment of complicated mandibular fractures in children using resorbable plates.
Patients and Methods
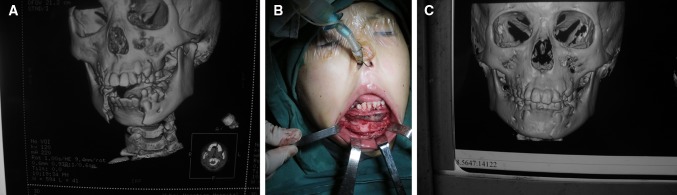
Records of 14 patients who sustained and presented to our department with complicated fractures of the mandible, and were treated with resorbable plates were retrieved. Permission was sought from and granted by the institution ethical committee. Data extracted included patients’ gender, age, etiology of fracture, nature of fracture, site of the fracture and surgical approach used. The surgical procedures were performed under general anesthesia; intraoral (vestibular) and extraoral (submandibular) surgical incisions were used to access the fracture sites. Majority of the incisions were intraoral, except for one subcondylar fracture and a comminuted fracture body of the mandible which were accessed through extraoral incisions (Figs. 2B, 3D). Regarding the operation procedure in brief; on accessing the fracture site, under clear visualization (Fig. 2B), interpositional tissues in the form of bony spicules and soft tissue were cleared off the site. Reduction of the fracture was then done, taking caution of proper alignment of the bone segments and checking the occlusion. A template, when necessary, was used to record the alignment/curvature of a particular site of the mandible; the resorbable plate was then molded according to the template. We used Lactosorb™ (poly-l-lactic acid/polyglycolic acid) plates and screws. Hot sterile saline was used to heat the plates in order to curve/mold them to the desired shape as per the template; exposure was about 15 s, with temperature not exceeding 85 °C according to the manufacturer’s recommendations. Drill holes were made through the outer cortex only, a screw thread hand tool used to in-print the threads. The resorbable plates (2.0 mm) were then fixed at the lower margin of the mandible (Fig. 1B) using monocortical screws. Special care was taken to avoid injury to the underlying tooth buds; in the canine region, a longer plate was used to ensure screw placement distant from this lowest position of tooth buds. Post-operatively, oral hygiene instructions including tooth brushing using a soft toothbrush and mouth rinsing with 0.1 % chlorhexidine 3 times a day, were emphasized. The patients were post-operatively advised to restrict themselves to a soft diet and avoid any activities that may transmit excessive loading forces to the mandible for a period of about 4 weeks. Restoration of premorbid (functional) occlusion was used to assess treatment results.
Fig. 2.
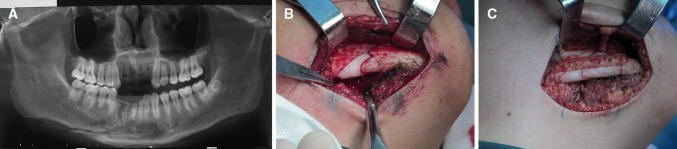
A Panoramic radiograph showing a comminuted fracture of the right body of mandible in a 15-year old boy; also crown fractures of teeth 31,41, and avulsion of 42,43. B Intraoperative photograph showing the comminuted fracture exposed through extraoral approach. C Fracture reduced and fixed with 2.0 mm resorbable plates and screws; the mental nerve was preserved
Fig. 3.
A Panoramic radiograph showing right subcondylar fracture in a 14-year old boy. B Medially displaced condylar segment. C Intraoperative photograph showing the condyle clamped and drawn inferiorly; resorbable plate being screwed in place before re-positioning it. D Resorbable plate and screws in place after reduction and fixation of the fracture
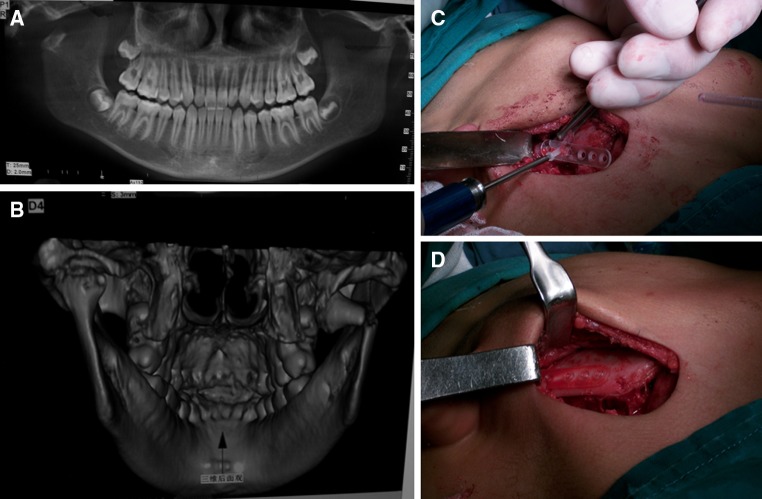
Fig. 1.
A Bilateral mandibular fracture in a 9-year old girl, with displacement of the segment and malocclusion. B Intraoperative photograph showing the fracture reduced and fixed with resorbable plates and screws. C Post-operative result showing satisfactory healing and restoration of occlusion and mandibular countour
Results
Details of data collected from the 14 patients is shown in Table 1; there were 10 males and 4 females; male to female (M:F) ratio was 2.5:1. Their ages ranged from 6 to 15 years, with a mean of 10.14 years. The etiology of the fractures included road traffic accidents (n = 11) and falls (n = 3). Most of the fractures were sustained on the body of the mandible. Majority of the patients had displacement of the fracture segments; 2 patients had comminuted fractures. Post-operative assessment was by the results of the final review as outpatient after 3 months. The consolidation of the fractures was assessed by physical examination, alongside radiography (Fig. 1C). The main focus was on satisfactory occlusion, function and restored alignment/contour of the mandible. All the patients healed uneventfully post-operatively; complications such as infection, non-union, mal-union, mandibular deviation, deviation on mouth-opening were not encountered. The patients achieved satisfactory preinjury occlusion and mandibular contour, thus good function and esthetics.
Table 1.
Summary of patients′ data
| Patient | Sex | Age | Etiology | Nature of fracture | Site of fracture | Surgical approach |
|---|---|---|---|---|---|---|
| 1 | M | 14 | Fall | Displaced | Subcondyle | Extraoral |
| 2 | M | 6 | Fall | Displaced | Symphysis | Intraoral |
| 3 | F | 9 | RTA | Bilateral/displaced | Parasymphysis/body | Intraoral |
| 4 | M | 15 | RTA | Comminuted | Body | Extraoral |
| 5 | F | 12 | RTA | Displaced | Symphysis | Intraoral |
| 6 | M | 8 | RTA | Bilateral/displaced | Parasymphysis/body | Intraoral |
| 7 | M | 14 | RTA | Comminuted | Body | Extraoral |
| 8 | M | 9 | RTA | Displaced | Body | Intraoral |
| 9 | M | 14 | RTA | Displaced | Symphysis | Intraoral |
| 10 | F | 7 | Fall | Displaced | Symphysis | Intraoral |
| 11 | M | 11 | RTA | Bilateral/displaced | Body | Intraoral |
| 12 | M | 7 | RTA | Displaced | Body | Intraoral |
| 13 | M | 13 | RTA | Displaced | Body | Intraoral |
| 14 | F | 10 | RTA | Displaced | Body | Intraoral |
RTA road traffic accidents
Discussion
Maxillofacial fractures are not common in children because children have many fat pads around the upper and lower jaws, which are thought to cushion any impact [6–8]. However, when they occur they usually affect the mandible [6, 9–11]. Fractures of the mandible result in esthetic and functional disturbances to the patient. Biodegradable osteofixation devices are being increasingly used in cases of trauma to avoid problems associated with conventional metal osteofixation [12–14]. The avoidance of these problems is even more paramount in children.
For the purpose of this case series, complicated mandibular fractures were considered as those with severe displacement, malocclusion, multiple fractures or comminuted. One of the most important goals of treatment of mandibular fractures is to restore form and function; loss of function has nutritional and dietary implications to the patient, and ultimately on the general health.
Most of the cases were males, with a male to female ratio of 2.5:1. This was in agreement with studies that have reported males as being the predominantly affected sex [1, 15–20]. An explanation of greater and more dangerous activities among boys is common to a number of studies [21–23].
The major etiological factors were road traffic accidents and falls. Of the 14 patients, 11 had road traffic accidents as the cause of injury resulting in fracture of the mandible, 3 had their fractures having resulted from falls. These findings are similar to a number of studies that have documented road traffic accidents as a major cause of maxillofacial fractures [1, 15, 20].
Because of the functional, and sometimes esthetic difficulties encountered by patients with mandibular fractures, treatment of the fractures is paramount. In oral and maxillofacial surgery, the two main treatment approaches are: closed reduction, and open reduction and internal fixation with titanium plates and screws. It is important to note that the majority of simple and non-displaced fractures in children should be managed by a conservative and non-invasive approach; this can range from observation under soft diet to closed reduction by maxillomandibular fixation with elastics for short periods of time [3, 4]. This indeed, is the old and classic approach with its own advocates [19]. Immobilzation by maxillomandibular fixation in itself can be a challenge in children compared to the cooperation exhibited by adult patients [18, 19]. However, in the daily practice of oral and maxillofacial surgery, situations occur when children and young adolescents present with complicated fractures with displacement (Fig. 3B), malocclusion (Fig. 1A), comminuted (Fig. 2A), and multiple fractures. Under such circumstances, the surgeon’s treatment plan may round-up to open reduction and internal fixation [18]. For decades, this approach has also been anchored on the use of metal plates and screws. Without completely over-looking the documented advantages of metal plate fixation of maxillofacial fractures, their use for fixation of mandibular fractures in children can be complicated by the state of mixed dentition; risk of intrabony embedment of metal screws affecting jaw/teeth growth [2, 5, 17, 18, 24], palpability or visibility of plates through the chin, damage to tooth buds [19], need for secondary surgery to remove the plates.
In this case series, we used resorbable plates to treat 14 children who presented with complicated mandibular fractures, as defined earlier, in whom open reduction and internal fixation was the most appropriate option. The fractures were located at the symphysis, parasymphysis, body and subcondyle (n = 1). With exception of two comminuted body fractures and one subcondylar fracture, the rest of the fracture sites were accessed through intraoral incisions. Resorbable plates and screws are known to less likely disturb skeletal growth; however, depending on the application technique, they may still damage unerupted teeth and tooth buds. In our experience, the following measures were effectively used to prevent damage to inferior dental/mental nerves, teeth/tooth buds: the mental foramen/nerve were identified and preserved (Fig. 2C), the plates were fixed at the lower margin of the mandible, drill holes were made through the outer cortex only. In the canine region, which is the lowest position of tooth buds in the mandible, longer plates were used to ensure screw placement distant from the canine bud area. The mandible is known to be subjected to functional/loading forces; therefore, placement of only one plate at the inferior border may be inadequate to withstand the multiple forces. In order to improve on the strength of the plates and stability of the fixation, an interdental wire (0.4 mm) splint was used in some cases. Some of the intraoperative difficulties and limitations encountered included: small mouth in children leading to limitation in the degree of mouth-opening and retraction, difficulty in skin flap retraction while accessing a high subcondylar fracture (Fig. 3C), inadequate strength of the plates to withstand forces on the mandible in some cases; thus necessitating an additional wire splint. Literature has documented the advantages of resorbable plates that include avoidance of secondary surgery to remove the plates, gradual transfer of load to the healing bone during resorption, elimination or reduction in the period of maxillomandibular fixation [17, 18, 24, 25]. However, resorbable plates application are not completely complication-free; some of the associated complications include: breaking of the devices due to excessive forces, loosening and migration of the devices, damage to tooth buds, neurovascular injury, post-operative infection, foreign-body tissue reaction to the plates. However, in these series of patients, all the patients healed uneventifully; this was in agreement with other studies [18]. On a socio-economic view, resorbable plates and screws have a cost-related limitation in that they are very expensive.
Conclusion
Whereas the number of patients in this case series was small, it is worth noting that children sometimes present with complicated fractures of the mandible, thereby necessitating open reduction and internal fixation. Resorbable plates when available and affordable, are an effective option for open reduction and internal fixation of such fractures.
References
- 1.Glazer M, Joshua BZ, Woldenberg Y, Bodner L (2011) Mandibular fractures in children: analysis of 61 cases and review of the literature. Int J Pediatr Otorhinolaryngol 75:62–64 [DOI] [PubMed]
- 2.Bayat M, Ghorbani K, Motamedi MHK (2010) Treatment of mandibular angle fractures using a single bioresorbable miniplate. J Oral Maxillofac Surg 68:1573–1577 [DOI] [PubMed]
- 3.do Egito Vasconcelos BC, Augusto C, Lago P, Nogueira RVB, de Alencar Gondim DG, Filho AB (2009) Mandibular fracture in a premature infant: a case report and review of the literature. J Oral Maxillofac Surg 67:218–222 [DOI] [PubMed]
- 4.Kushner GM, Tiwana PS (2009) Fractures of the growing mandible. Atlas Oral Maxillofac Surg Clin 17:81–91 [DOI] [PubMed]
- 5.Senel FC, Tekin US, Imamoglu M (2006) Treatment of a mandibular fracture with biodegradable plate in an infant: report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:448–450 [DOI] [PubMed]
- 6.Shaikh ZS, Worrall SF. Epidemiology of facial trauma in a sample of patients aged 1–18 years. Injury. 2002;33:669–671. doi: 10.1016/S0020-1383(01)00201-7. [DOI] [PubMed] [Google Scholar]
- 7.Holland AJA, Broome C, Steinberg A, Cass DT. Facial fractures in children. Pediatric Emerg Care. 2001;17:157–160. doi: 10.1097/00006565-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Managlia AJ, Kline ST. Maxillofacial trauma in the pediatric age group. Otolaryngol Clin North Am. 1983;16:717–730. [PubMed] [Google Scholar]
- 9.Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:126–134. doi: 10.1067/moe.2000.107974. [DOI] [PubMed] [Google Scholar]
- 10.Sherick DG, Buchman SR, Patel PP. Pediatric facial fractures: analysis of differences in sub-speciality care. Plast Reconstr Surg. 1998;102:28–31. doi: 10.1097/00006534-199807000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Kaban LB, Mulliken JB, Murry JE. Facial fractures in children: analysis of 122 fractures in 109 patients. Plast Reconstr Surg. 1977;59:15–20. doi: 10.1097/00006534-197701000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Ylikontiola L, Sundqvuist K, George KBS, Tormala P, Ashammakhi N (2004) Self-reinforced bioresorbable poly-L/DL-Lactide [SR-P(L/DL)LA] 70/30 miniplates and miniscrews are reliable for fixation of anterior mandibular fractures: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:312–317 [DOI] [PubMed]
- 13.Imola MJ, Hamlar DD, Shao W, Chowdhury K, Tatum S. Resorbable plate fixation in pediatric craniofacial surgery: long-term outcome. Arch Fac Plast Surg. 2001;3:79–90. doi: 10.1001/archfaci.3.2.79. [DOI] [PubMed] [Google Scholar]
- 14.Yerit KC, Enislidis G, Schopper C, et al. Fixation of mandible fractures with biodegradable plates and screws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:294–300. doi: 10.1067/moe.2002.122833. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira P, Marques M, Pinho C, Rodrigues J, Reis J, Amarante J (2004) Midfacial fractures in children and adolescents: a review of 492 cases. Br J Oral Maxillofac Surg 42:501–505 [DOI] [PubMed]
- 16.Mistretta MC (2005) Use of bioresorbable plating system in pediatric mandible fractures. J Oral and Maxillofac Surg 63:101
- 17.Yerit KC, Hainich S, Enislidis G, Turhani D, Klug C, Wittwer G, Ockher M, Undt G, Kermer C, Watzinger F, Ewers R. Biodegradable fixation of mandibular fractures in children: stability and early results. Oral Surg Oral Med Oral Radiol Endod. 2005;100(1):17–24. doi: 10.1016/j.tripleo.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Iatrou I, Theologie-lygidakis N, Tzerbos F. Surgical protocols and outcome for the treatment of maxillofacial fractures in children: 9 years experience. J Cranio Maxillofac Surg. 2010;38:511–516. doi: 10.1016/j.jcms.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2005;34(8):823–833. doi: 10.1016/j.ijom.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 20.Posnick JC, Wells M, Pron GE (1993) Pediatric facial fractures: evolving patterns of treatment. J Oral Maxillofac Surg 51:836–844 [DOI] [PubMed]
- 21.Berthouze E, Sagne D, Momege B, Achard R. Treatment of mandibular fractures in children: our therapeutic approach. Rev Stomatol Chir Maxillofac. 1980;81:285–288. [PubMed] [Google Scholar]
- 22.Powell EC, Tanz RR. Cycling injuries treated in emergency departments: need for bicycle helmets among preschoolers. Arch Pediatr Adolesc Med. 2000;154:1096–1100. doi: 10.1001/archpedi.154.11.1096. [DOI] [PubMed] [Google Scholar]
- 23.Powell EC, Tanz RR, Discala C. Bicycle-related injuries among preschool children. Ann Emerg Med. 1997;30:260–265. doi: 10.1016/S0196-0644(97)70159-8. [DOI] [PubMed] [Google Scholar]
- 24.Bell RB, Kindsfater CS (2006) The use of biodegradable plates and screws to stabilize facial fractures. J Oral Maxillofac Surg 64:31–39 [DOI] [PubMed]
- 25.Turvey TA, Proffit WP, Phillips C. Biodegradable fixation for craniomaxillofacial surgery: a 10 year experience involving 761 operations and 745 patients. Int J Oral Maxillofac Surg. 2011;40(3):244–249. doi: 10.1016/j.ijom.2010.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]