Abstract
Background
Reliable methods of fixation of soft tissue and bone are of utmost importance in reconstructive shoulder surgery and in many orthopaedic applications. Current methods of securing lesser tuberosity osteotomies performed during shoulder arthroplasty and tuberosity fixation performed during repair of proximal humeral fractures often rely on alternating half hitches or surgeon’s knots regardless of the suture configuration used passing through the tissue (eg, Mason-Allen, Krackow). The racking hitch knot in contrast to half hitches allows sequential tightening, even under tension, with minimal risk of knot slippage or premature locking. These knot characteristics allow the surgeon to stepwise improve their reduction before committing and locking a construct, preventing hanging knots or under-tensioned repairs. However, little data exist to support the use the racking hitch knot to guide decision making regarding how to back up the knot or to explain the effect of suture material on security and strength.
Questions/purposes
The objectives of our study were (1) to identify the optimal number of half hitches necessary to maintain knot security for a single knot; (2) to evaluate if a difference exists in the relative behavior of racking hitch knots when tied using different suture materials; and (3) to define the biomechanical differences between the racking hitch and two other knot configurations commonly used in shoulder surgery (Weston and square knots).
Methods
Using an Instron device we tested the effect of adding supplemental half hitches (from one to four) to the racking hitch. Additionally, a selection of commercially available braided nonabsorbable polyethylene sutures and different knot configurations (racking hitch, Weston knot, and square knot) also were tested. Data were compared using ANOVA.
Results
Increasing the number of half hitches improved knot performance in peak load testing and cyclic testing, revealing a significant difference between the racking hitch supplemented with one and four half hitches (199.2 N versus 428.8 N, p < 0.05). Force Fiber™ #2 (359.6 N) and FiberWire® #2 (302 N) showed increased loads to failure compared with Ethibond Excel™ #2 or Force Fiber™ #3/4, whereas Ethibond Excel™ had the least amount of slippage during cyclic testing (0.09 mm). The racking hitch knot had considerably higher loads to failure (359.6 N) than the Weston (145.2 N) or square (77 N) knots.
Conclusions
The racking hitch knot exhibited significantly higher loads to failure and comparable knot slippage (elongation during cyclic testing) when compared with other commonly used knots. According to the biomechanical data, the addition of four half hitches to supplement the racking hitch and the choice of FiberWire® #2 or Force Fiber™ #2 suture resulted in increased knot security.
Clinical Relevance
This knot adds a tool to the arsenal for surgeons best suited for repairs requiring a high degree of knot security and reliable tissue tensioning.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3478-0) contains supplementary material, which is available to authorized users.
Introduction
Anatomic restoration is of paramount importance in reconstructive shoulder surgery. The suture material chosen and the knot configuration used for repair varies among surgeons and situations. However, the most critical aspect of any repair is that the mechanical integrity of the construct must be able to withstand physiologic forces during the healing process [10]. Burkhart et al. [4] addressed the concept of knot effectiveness. Namely, knot security (resistance to loosening or breaking) and loop security (tightness of the initial loop) play a key role in maintaining the knot. The ideal knot configuration would maximize knot security and loop security with little to no variation in tying technique.
In light of this, surgeons at our institution have been using the racking hitch knot routinely during shoulder procedures. We believe that the intrinsic stability of the knot provides robust fixation and, in the process, confers sufficient stability to the construct for reliable healing. The racking hitch knot is a sliding, strangle knot whose tension can be readjusted even after one half hitch is thrown over the top of the initial knot (Fig. 1) (Video 1. Supplemental material is available with the online version of CORR). When multiple sutures are placed in series, the knots can be tightened sequentially. Each knot can be cinched and backed up with one half hitch minimizing backward sliding of the knot and allowing for tuning a reduction. This effect is similar to the sequential tensioning screws in a compression plate or the use of multiple cerclage wires. The ability to properly tension multiple sutures at different anchoring positions allows for even load sharing on each of the sutures.
Fig. 1A–F.
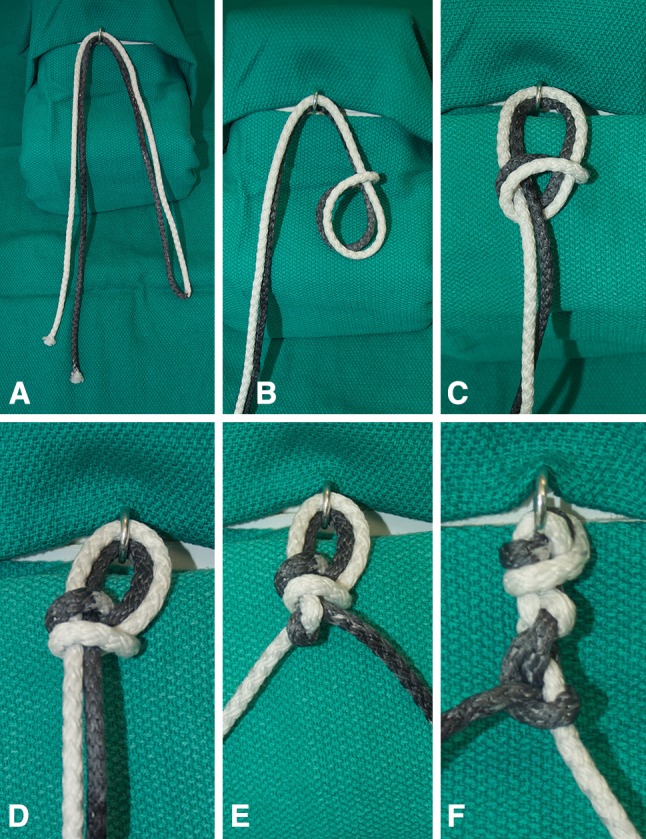
(A) The loop end of the rope is passed through one side of the knot tying station and the free ends are passed through the opposite end. (B) A loop is created through which the free ends of the rope will be passed to create the racking hitch. (C) The free ends of the rope have been passed through the loop. (D) The racking hitch is tightened to the tying station. (E) The racking hitch has been backed up by an initial half hitch. At this point, retensioning can be performed before supplementation with additional half hitches. (F) The racking hitch has now been reinforced with a total of four half hitches.
The objectives of the study were (1) to identify the optimal number of half hitches necessary to maintain knot security for a single knot; (2) to evaluate if a difference exists in the relative behavior of racking hitch knots when using different suture materials; and (3) to define the biomechanical differences between the racking hitch and other common sliding and static knots used in shoulder surgery.
Materials and Methods
All testing was done under ambient conditions and all sutures were wetted with normal saline before and during all testing to simulate in vivo conditions. Each knot was tied under 20-N load directly on the circular testing fixture (Fig. 2). The knots were tied with the use of an arthroscopic knot pusher to ensure accurate control of the tension applied to the knot. Furthermore, a tensiometer was used on the post limb of the knot to ensure 20-N load was applied and that each knot was consistently tensioned. The knots were tied in their respective, standard described techniques by a shoulder and elbow fellow (SV) under the guidance of the lead investigator (JDK).
Fig. 2.
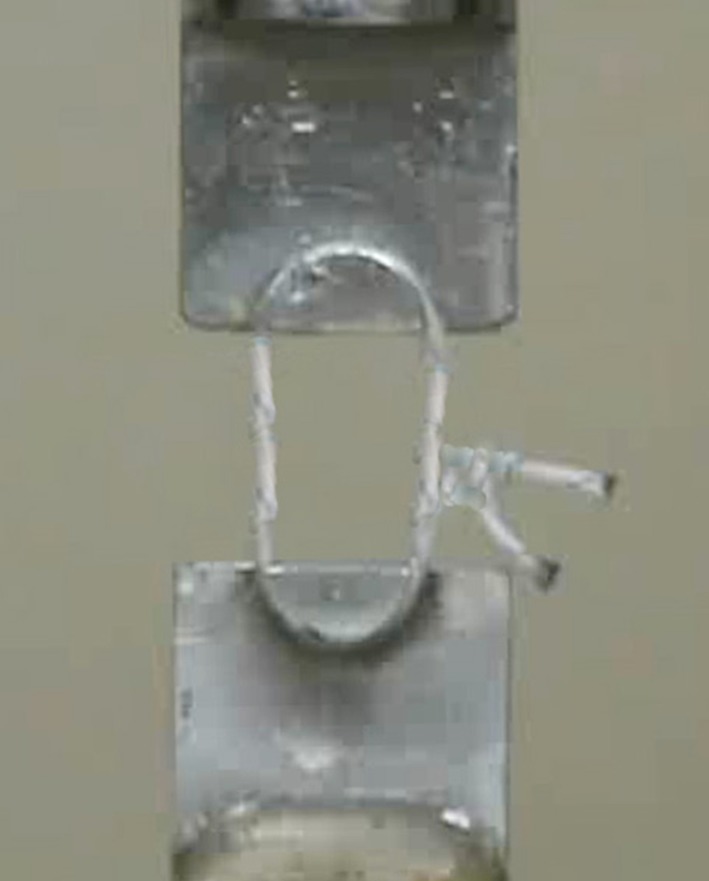
Each knot was tied directly on the circular testing fixture shown in the figure. The knots were tied with the use of an arthroscopic knot pusher to ensure accurate control of the tension applied to the knot and a tensiometer was used on the post limb of the knot to ensure 20-N load was applied consistently.
Before mechanical testing, a 10-N preload was placed on each sample until no additional displacement was observed and then testing began. Subsequently, each knot underwent biomechanical testing with an Instron testing device (Instron, Norwood, MA, USA). To evaluate cyclic displacement and ultimate load to failure, cyclic loading 10 to 30 N for 200 cycles at 1 Hz was applied to each knot. We designated the distance of 3 mm as clinically relevant failure. This was defined by prior biomechanical testing [1, 3]. Each test condition was repeated three times. The number of cycles to 3 mm of elongation was recorded and load and displacement curves were generated from the data. Mean and standard deviations were calculated on peak elongations.
Load to failure testing also was conducted on each knot with a crosshead speed of 0.5 mm/second (speed at which the suture grips separate). Each test condition was repeated five times. The load at which 3-mm suture elongation or breakage occurred was measured and recorded among the groups. Means and standard deviations were collected on peak load and load at 3 mm of elongation. Photographs and video recording of all knot failures were obtained at the time of testing to report mode of knot failure.
For the first part of the study, racking hitch knots (Fig. 1) with one, two, three, or four half hitches were tied with Force Fiber™ #2 (Tornier, Edina, MN, USA) to determine the mechanical differences between the configurations.
Next, we used four commercially available sutures to compare the strength and security of the racking hitch across different suture types. Force Fiber™ #2 (Tornier), Force Fiber™ #3–4 (Tornier), FiberWire® #2 (Arthrex, Naples, FL, USA), and Ethibond Excel™ #2 (Ethicon, Somerville, NJ, USA) were used in this phase of the study. Racking hitch knots were tied with each suture material and were backed up with three half hitches with alternating posts.
Finally, using Force Fiber™ #2, we conducted a comparison between the racking hitch backed up with three half hitches, Weston, and square knots. The Weston and square knots also were backed up with three half hitches. They were selected because they have been used by other authors in biomechanical testing and are example of a common sliding knots and a common static knot [1, 3, 8].
Statistical analysis was performed on the data gathered. An ANOVA was performed to compare peak load at failure with the number of half hitches used to back up the racking hitch, suture type, and knot configuration (square versus Weston versus racking hitch).
Results
Half Hitch Comparison
The average peak load to failure increased after the addition of a second half hitch (from 199.2 N to 273.2 N) and a third half hitch 359.6 N (Table 1). However, the addition of a fourth half hitch had the highest average peak loads 428.8. An ANOVA was performed to compare peak load at failure with the number of half hitches used to back up the racking hitch. According to the data, backing up the racking hitch with only one half hitch was statistically weaker than adding two, three, or four half hitches (p = 0.012). A trend toward increasing peak loads was observed comparing a racking hitch backed up with two versus three half hitches but this was not statistically significant (p = 0.10). A trend toward increased peak loads also was observed across all cases but no statistical difference was seen in the comparison between the peak loads with two, three, or four half hitches added to the construct. Cyclic data showed that the addition of half hitches to the racking hitch showed little improvement in knot slippage (Table 2). However, there was a general trend of decreased slippage distance relative to the number of half hitches.
Table 1.
Peak load data
| Knot type | Variable | Average peak load (N) | SD | Average load at 3 mm of elongation (N) | SD |
|---|---|---|---|---|---|
| Racking hitch knot (n = 5) (Force Fiber™ #2) |
Number of hitches | ||||
| 1 | 199.2 | 43.9 | 168.2 | 35.9 | |
| 2 | 273.2 | 91.5 | 234.6 | 60.5 | |
| 3 | 359.6 | 101.1 | 277.1 | 71 | |
| 4 | 428.8 | 137.9 | 311 | 72.8 | |
| Suture type | |||||
| Racking hitch with 3 half hitches (n = 5) | Force Fiber™ #2 | 359.6 | 101.1 | 277.1 | 71 |
| Ethibond Excel™ #2 | 270.4 | 13.2 | 174.5 | 6.7 | |
| FiberWire® #2 | 302.0 | 9.7 | 190.1 | 64.2 | |
| Force Fiber™ #3–4 | 278.9 | 64.6 | 245.5 | 33.8 | |
| Knots with three half hitches (Force Fiber™ #2) |
Racking hitch | 359.6 | 101.1 | 277.1 | 71 |
| Square knot (n = 6) | 77.4 | 45.6 | 69.4 | 39.9 | |
| Weston knot (n = 5) | 145.2 | 63.2 | 122.2 | 48.9 | |
Force Fiber™ #2 (Tornier, Edina, MN, USA); FiberWire® #2 (Arthrex, Naples, FL, USA); Ethibond Excel™ #2 (Ethicon, Somerville, NJ, USA).
Comparison of the average peak load to failure and load to 3 mm of elongation of a racking hitch knot backed up with three half hitches compared with square knots and Weston knots.
Table 2.
Cyclic data*
| Variable | Average peak elongation (mm) | SD peak |
|---|---|---|
| Number of hitches† (n = 5) | ||
| 1 half hitch | 0.52 | 0.07 |
| 2 half hitches | 0.36 | 0.14 |
| 3 half hitches | 0.23 | 0.13 |
| 4 half hitches | 0.05 | 0.03 |
| Suture type (n = 5)≠ | ||
| Force Fiber™ #2 | 0.23 | 0.13 |
| Ethibond Excel™ | 0.09 | 0.01 |
| FiberWire® | 0.16 | 0.05 |
| Force Fiber™ #3–4 | 0.19 | 0.07 |
| Knot type† | ||
| Racking hitch three half hitches (n = 5) | 0.23 | 0.13 |
| Square three half hitches (n = 6) | 1.1 | 2 |
| Weston three half hitches (n = 5) | 0.18 | 0.02 |
* 10–30 N for 200 cycles; †tied with Force Fiber™ #2; ≠tied with a racking hitch, backed up with three half hitches; Force Fiber™ #2 (Tornier, Edina, MN, USA); FiberWire® #2 (Arthrex, Naples, FL, USA); Ethibond Excel™ #2 (Ethicon, Somerville, NJ, USA).
Suture Comparison
In the pull to failure testing, slight differences were noted across all the suture types. Notably, Force Fiber™ #2 had the highest peak loads at 359.6 N, whereas Ethibond Excel™ showed the lowest peak loads at 270.4 N. In the cyclic testing, Ethibond Excel™ showed the least slippage (0.09 mm) while Force Fiber™ #2 showed the greatest slippage (0.23 mm).
Knot Configuration Comparison
The racking hitch tied with three half hitches (Force Fiber™ #2) had the highest average peak load to failure (359.6 N), whereas square knots tied with Force Fiber™ #2 had the lowest average peak loads (77.4 N). A one-way ANOVA of these data showed that the peak load to failure was significantly greater for the racking hitch than either the square or Weston knots (p < 0.001).
However, cyclic data across the three-knot configurations showed little to no difference in elongation distances between Weston and racking hitch knots, whereas square knots showed nearly 500% greater elongation at 200 cycles (1.1 mm versus 0.23 mm) (Table 2).
Discussion
Bone and tissue fixation are critical elements to success in reconstructive shoulder surgery and many other orthopaedic fields. The racking hitch knot has practical advantages over other common sliding and locking knots as it has high load to failure when backed up with half hitches and sufficient knot security to prevent slippage even when only tied with one half hitch. These properties allow a surgeon the ability to stepwise improve a reduction before further securing a knot with additional half hitches. This knot characteristic, allowing for further sliding while still having security prevents hanging knots, avoids slack after additional knots have been thrown and under-tensioned repairs. In this study we sought define the number of half hitches necessary to back up a racking hitch knot, to explore the effect of suture material on knot performance, and to compare the racking hitch with two other common knot configurations. Four half hitches showed the greatest load to failure and the least slippage. Although all of the nonabsorbable braided polyethylene sutures performed well, Force Fiber™ #2 showed the greatest strength while Ethibond Excel™ showed the least slippage. Finally, the racking hitch performed better in load to failure and cyclic loading than the square or Weston knots.
Although our study provides proof of a concept for use of the racking hitch knot, it is not without significant limitations. This is a biomechanical study and tests only knot security and load to failure in an in vitro set up. Alternative study designs using a cadaveric repair of the lesser tuberosity or clinical trials comparing alternative fixation techniques would provide useful data. Failure of fixation in osteotomy repair and fracture fixation is not infrequently a biological problem (patient age, smoking, medical comorbidities), not just a failure of fixation [6, 12]. From our study we do not have the ability to know if the additional strength gained from using a racking hitch knot results in a clinically significant difference in healing. Nevertheless, this study does answer a few critical questions regarding the racking hitch knot and proves its strength in repair.
Some other studies have looked at the effect of adding additional throws to knot configurations. Ilahi et al. [9] explored the effect of additional throws tied on square knots. They showed that by increasing from three to five throws the ultimate load to failure increased from 122.6 to 152.8 N. We too saw incremental gains in strength with the addition of more throws. However, the knot tested in their design was not a racking hitch. In a study using a knot more similar to ours, Chokshi et al. [5] compared a modified racking hitch with modified Roeder knots and square knots using Ethibond Excel™ #2. In their study, only one underhand throw was applied to the initial racking hitch and no testing was performed of additional hitches. The peak load to failure values averaged 122 N ± 20.70 N [5], whereas our results with just one half hitch (using Force Fiber™ #2) yielded peak load values of 199.2 N. These data were obtained using a different suture and without the additional security of more half hitches making further comparisons difficult to interpret.1
Numerous authors have analyzed the effect of suture choice on knot performance. Although there are no universal conclusions regarding the suture with the best repair characteristics, braided polyester sutures often have shown higher load to failure than alternative choices [2, 9, 10]. Abbi et al. [1] reported that knots tied with FiberWire® had the highest load to failure values, averaging 275.97 N. Swan et al. [11] also looked at the effect of suture type on load to failure using Force Fiber™, FiberWire®, and Ethibond Excel™. Swan et al. [11] observed the highest load to failure using Force Fiber™ suture across all three knots tested in their trial. They observed a similar magnitude load to failure for their surgeon’s knot tied with Force Fiber™ (230.1 N) as we observed for a racking hitch with one half hitch (273.2 N). In addition, they observed a similar increased load to failure across many knot configurations when Force Fiber™ was used compared with FiberWire®.
Knot Type
Elkousy et al. [7] also tested load to failure characteristics with different knot configurations. In their study, the highest load to failure values were seen with the Weston knot (168 N) [7]. Our testing setup using a Weston knot also tied with Force Fiber™ resulted in a similar load to failure of 145.2 N. However, in our study, the load to failure values for the racking hitch with three half hitches averaged 359.6 N. This is more than twice the force reported by Elkousy et al. [7]. Although a portion of the improved performance may be attributed to the knot configuration, a possible explanation of these observed differences is that a racking hitch knot is tied with a doubled suture. This doubling of the suture effectively doubles the number of strands crossing the testing apparatus or in vivo, holding a repair. While this doubling of the suture does result in more suture in the knot and more suture crossing the tissue, it may allow the surgeon to safely use a smaller USP size suture to adjust for the increased knot volume (substituting a #5 for a #2) and appears to also increase the strength of a repair.
Our standard fixation of a lesser tuberosity osteotomy involves the use of a series of racking hitch knots (Fig. 3). Typically we use three or four knots. Once the initial racking hitches are placed and cinched, each is backed up with one half hitch (Fig. 3) (Video 2. Supplemental material is available with the online version of CORR). Because the knot can slide with little slippage with just one half hitch, the knots can be tightened sequentially which creates slack in the other sutures. This residual slack can be eliminated by retensioning the racking hitch (sliding and cinching the knot again). Once physiologic tension has been restored the knots are further secured by adding the three or four half hitches. This unique capability of easy sliding with little risk of slippage is the fundamental reason we choose to use the racking hitch for bony and soft tissue fixation.
Fig. 3A–D.
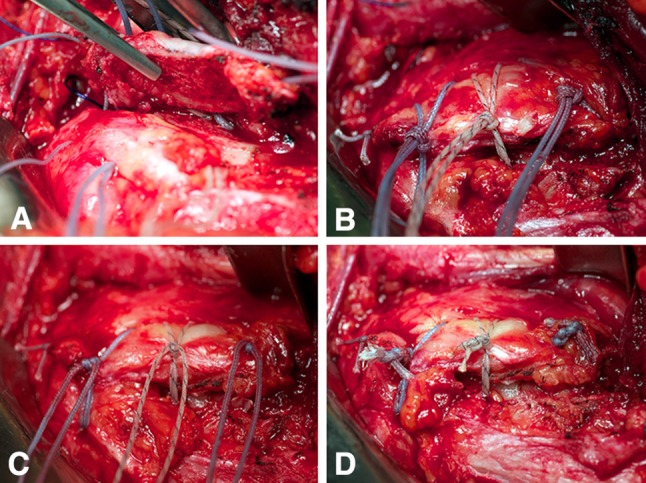
(A) The loops of the racking hitch are placed laterally and the free ends of the doubled suture are passed at the bone-tendon interface medially. The lesser tuberosity acts as a bony “washer,” thus providing secure fixation. (B) Racking hitches are thrown in sequence and backed up by one half hitch and then sequentially tightened reducing the tuberosity. (C) Additional half hitches are added to the construct to provide additional knot security (“backing up” the initial half hitch). A total of four additional half hitches are added. (D) The final racking hitch knot construct shows robust fixation with compression of the lesser tuberosity fragment to the osteotomy site.
Future directions for this project could include biomechanical testing in a cadaveric model, testing load to failure and cyclic testing of a repaired lesser tuberosity osteotomy, and determining the compression achieved at the osteotomy interface. Additionally, clinical data regarding the outcomes of repairs using this construct in comparison to other fixation strategies would be helpful. However, these questions are beyond the scope of our study.
We showed that the racking hitch knot backed up with three half hitches is a biomechanically robust construct. Its ability to be retensioned and provide secure fixation are advantages of the racking hitch knot in procedures requiring reduction of bone or soft tissue.
Electronic supplementary material
Supplementary material 2 (M4 V 14802 kb)
Acknowledgments
We thank Ryan Schlotterback, Austin Allen, and Huong Do for assistance with the statistical analysis on this project.
Footnotes
We believe our data underscores the importance of using more than one half hitch on top of the racking hitch
One or more of the authors certifies that he (JDK), or a member of his immediate family has received or may receive payment or benefits, during the study period of 10,000 to 100,000 USD, from Tornier, Edina, MN, USA.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
References
- 1.Abbi G, Espinoza L, Odell T, Mahar A, Pedowitz R. Evaluation of 5 knots and 2 suture materials for arthroscopic rotator cuff repair: very strong sutures can still slip. Arthroscopy. 2006;22:38–43. doi: 10.1016/j.arthro.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Barber FA, Herbert MA, Beavis RC. Cyclic load and failure behavior of arthroscopic knots and high strength sutures. Arthroscopy. 2009;25:192–199. doi: 10.1016/j.arthro.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Baumgarten KM, Brodt MD, Silva MJ, Wright RW. An in vitro analysis of the mechanical properties of 16 arthroscopic knots. Knee Surg Sports Traumatol Arthrosc. 2008;16:957–966. doi: 10.1007/s00167-008-0595-x. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart SS, Wirth MA, Simonich M, Salem D, Lanctot D, Athanasiou K. Knot security in simple sliding knots and its relationship to rotator cuff repair: how secure must the knot be? Arthroscopy. 2000;16:202–207. doi: 10.1016/S0749-8063(00)90037-9. [DOI] [PubMed] [Google Scholar]
- 5.Chokshi BV, Ishak C, Iesaka K, Jazrawi LM, Kummer FJ, Rosen JE. The modified racking hitch (MRH) knot: a new sliding knot for arthroscopic surgery. Bull NYU Hosp Jt Dis. 2007;65:306–307. [PubMed] [Google Scholar]
- 6.Duckworth AD, Bennet SJ, Aderinto J, Keating JF. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. 2011;93:811–816. doi: 10.1302/0301-620X.93B6.26432. [DOI] [PubMed] [Google Scholar]
- 7.Elkousy HA, Sekiya JK, Stabile KJ, McMahon PJ. A biomechanical comparison of arthroscopic sliding and sliding-locking knots. Arthroscopy. 2005;21:204–210. doi: 10.1016/j.arthro.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Ilahi OA, Younas SA, Alexander J, Noble PC. Cyclic testing of arthroscopic knot security. Arthroscopy. 2004;20:62–68. doi: 10.1016/j.arthro.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Ilahi OA, Younas SA, Ho DM, Noble PC. Security of knots tied with ethibond, fiberwire, orthocord, or ultrabraid. Am J Sports Med. 2008;36:2407–2414. doi: 10.1177/0363546508323745. [DOI] [PubMed] [Google Scholar]
- 10.Lo IK, Ochoa E, Jr, Burkhart SS. A comparison of knot security and loop security in arthroscopic knots tied with newer high-strength suture materials. Arthroscopy. 2010;26(9 suppl):S120–S126. doi: 10.1016/j.arthro.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Swan KG, Jr, Baldini T, McCarty EC. Arthroscopic suture material and knot type: an updated biomechanical analysis. Am J Sports Med. 2009;37:1578–1585. doi: 10.1177/0363546509332816. [DOI] [PubMed] [Google Scholar]
- 12.Wieser K, Zingg P, Dora C. Trochanteric osteotomy in primary and revision total hip arthroplasty: risk factors for non-union. Arch Orthop Trauma Surg. 2012;132:711–717. doi: 10.1007/s00402-011-1457-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 2 (M4 V 14802 kb)


