Abstract
Background
Although minimally invasive surgical (MIS) approaches to the lumbar spine for posterior fusion are increasingly being utilized, the comparative outcomes of MIS and open posterior lumbar fusion remain unclear.
Questions/purposes
In this systematic review, we compared MIS and open transforaminal or posterior lumbar interbody fusion (TLIF/PLIF), specifically with respect to (1) surgical end points (including blood loss, surgical time, and fluoroscopy time), (2) clinical outcomes (Oswestry Disability Index [ODI] and VAS pain scores), and (3) adverse events.
Methods
We performed a systematic review of MEDLINE®, Embase, Web of Science, and Cochrane Library. Reference lists were manually searched. We included studies with 10 or more patients undergoing MIS compared to open TLIF/PLIF for degenerative lumbar disorders and reporting on surgical end points, clinical outcomes, or adverse events. Twenty-six studies of low- or very low-quality (GRADE protocol) met our inclusion criteria. No significant differences in patient demographics were identified between the cohorts (MIS: n = 856; open: n = 806).
Results
Equivalent operative times were observed between the cohorts, although patients undergoing MIS fusion tended to lose less blood, be exposed to more fluoroscopy, and leave the hospital sooner than their open counterparts. Patient-reported outcomes, including VAS pain scores and ODI values, were clinically equivalent between the MIS and open cohorts at 12 to 36 months postoperatively. Trends toward lower rates of surgical and medical adverse events were also identified in patients undergoing MIS procedures. However, in the absence of randomization, selection bias may have influenced these results in favor of MIS fusion.
Conclusions
Current evidence examining MIS versus open TLIF/PLIF is of low to very low quality and therefore highly biased. Results of this systematic review suggest equipoise in surgical and clinical outcomes with equivalent rates of intraoperative surgical complications and perhaps a slight decrease in perioperative medical complications. However, the quality of the current literature precludes firm conclusions regarding the comparative effectiveness of MIS versus open posterior lumbar fusion from being drawn and further higher-quality studies are critically required.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3465-5) contains supplementary material, which is available to authorized users.
Introduction
Lumbar spinal fusion is an accepted method of treatment for a variety of spinal pathologies [46]. As the proportion of adults older than 65 years continues to rise [21], the demand for spinal fusion procedures, particularly for degenerative disorders, continues to increase. Unfortunately, the substantial blood loss [6], high complication rates [5], and prolonged hospital stay [37] associated with traditional open midline techniques of spinal fusion may expose this patient population to an undesirable level of surgical morbidity [9]. Minimally invasive surgical (MIS) procedures have demonstrated improved clinical outcomes and decreased perioperative morbidity in the fields of general surgery, gynecology, and urology [13, 26, 38]. These results, coupled with advances in development of surgical instrumentation, magnification, and illumination, have led to the application of MIS techniques to spinal fusion. However, before widespread adoption of these novel procedures, their relative worth and clinical efficacy must be compared to standard open spinal fusion.
The Institute of Medicine has highlighted the need for studies examining the outcomes of alternative treatment methods, termed comparative effectiveness research (CER). According to the Institute of Medicine: “comparative effectiveness research is the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat and monitor or improve the delivery of care” [25]. Traditionally carried out by healthcare providers, CER of spinal fusion has historically focused on outcome measures of primary importance to surgeons, including surgical time, estimated blood loss (EBL), and fusion rates. Over the last decade, the importance of inclusion of patient-reported outcome measures in CER has been emphasized [7, 8]. Furthermore, CER is meant to assist not only patients and clinicians but also all stakeholders, including purchasers and policy makers, in making informed decisions that will improve health care for the individual or population. Unfortunately, physicians and surgeons often lack the perspective and language of purchasers and policy makers, who ultimately must consider the relative value of different healthcare interventions. The value of a healthcare intervention is defined as the quality or outcome of an intervention relative to its cost over time [32]. Consequently, cost reduction without regard to relative outcome is shortsighted and potentially leads to ineffective care [30].
We therefore compared MIS and open transforaminal or posterior lumbar interbody fusion (TLIF/PLIF) specifically with respect to (1) surgical end points (including EBL, surgical time, and fluoroscopy time), (2) clinical outcomes (Oswestry Disability Index [ODI] and VAS pain scores), and (3) adverse events.
Materials and Methods
Systematic Review and Study Inclusion
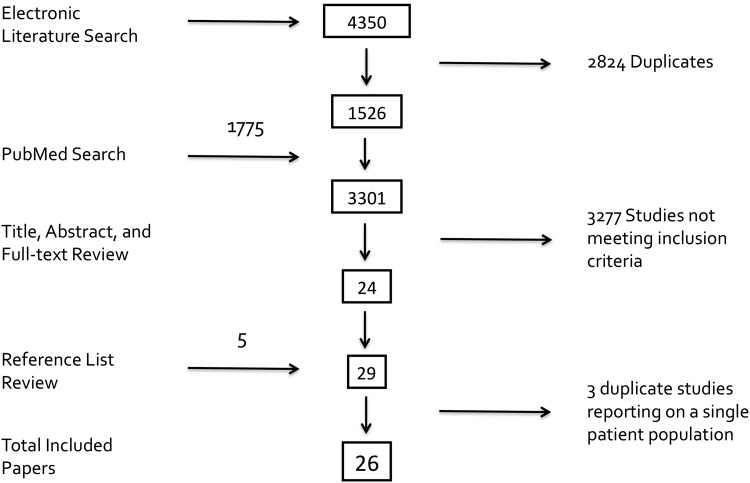
Our systematic review was performed following guidelines proposed by the Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group [36] and the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [23]. Identification of relevant studies began with an electronic search of MEDLINE®, Embase, Web of Science, and Cochrane Library from database inception to May 2012 inclusive. Our research coordinator (OP) with training related to the conduct of systematic reviews performed the searches. Medical Subject Heading (MeSH) search terms used included derivatives of “minimally invasive”/”minimal access” and “lumbar spine”/”lumbar vertebrae” or “fusion”/”surgical procedures”. Citations were limited to those published in English. The exact details of each database search are presented in Appendix 1 (supplemental materials are available with the online version of CORR®). Potential articles were then imported into the online reference management program RefWorks (RefWorks-COS, ProQuest, LLC, Bethesda, MD, USA) to remove duplicate citations and organize the studies before review for study inclusion (Fig. 1).
Fig. 1.
A flowchart shows the results of systematic review of the literature with methods of study identification and exclusion.
Two independent reviewers (CLG, KM) then screened study titles, abstracts, and full-text articles to identify randomized controlled trials or comparative studies comparing open and MIS fusion from a posterior approach in a unique sample of patients with degenerative lumbar pathology. Included in our study were articles with 10 or more patients per study arm and reporting at least one of the following: (1) surgical end point(s), (2) clinical outcome (ODI or VAS pain scores), or (3) adverse events. To ensure capture of articles not identified by our electronic search, each reviewer also performed a PubMed search using the phrase “minimally invasive spine surgery” and a manual search of reference lists of included articles. Study authors and field experts were not consulted as part of our search strategy. In cases of disagreement, the senior author (YRR) was consulted to obtain consensus regarding suitability for study inclusion. From the potential studies identified by our electronic database search and manual searching of reference lists, 26 citations remained for study inclusion [1, 3, 10–12, 15, 16, 18–20, 22, 24, 27–29, 31, 33–35, 39–45] (Table 1).
Table 1.
Patient demographics and outcomes of included cohort studies
| Study | Study design, enrollment dates, GRADE rating | Number of patients (MIS/open) | Male:female (number of patients) | Mean age (years) | Diagnosis | Followup (months) | % followup | Variables studied (MIS/open)* | Total complication rate (%) (MIS/open) |
|---|---|---|---|---|---|---|---|---|---|
| Adogwa et al. [1] | Retrospective 2007–2008 Low | 15/15 | MIS: 7:8 Open: 5:10 |
MIS: 50.8 Open: 49.7 |
DS | 24 (final) | 100 | OR time: 300/210†
EBL: 200/295† LOS: 3/5† VAS back: 5.5/4.6 VAS leg: 5.5/3.5 ODI: 15.7/17.1 |
0/6.7 |
| Bagan et al. [3] | Retrospective 2002–2005 Very low | 28/19 | NA | MIS: 52.9 Open: 59.3 |
DS, IS, LDH, DDD | 1 (final) | 100 | LOS: 5/7 | 18/37 |
| Dhall et al. [10] | Retrospective 2003–2006 Very low | 53/53 | NA | MIS: 53 Open: 53 |
DDD (n = 24) DS (n =18) |
MIS/open: 24/34 (mean) | 100 | OR time: 199/237 EBL: 194/505 |
5.7/3.8 |
| Fan et al. [11] | Prospective 2005–2006 Very low | 28/31 | MIS: 18:10 Open: 16:15 |
MIS: 51.4 Open: 52 |
IS (n = 13) DS (n = 27) LDH (n = 5) Stenosis (n = 14) |
MIS/open: 14.4/13.5 (mean) | MIS: 91 Open: 93 |
OR time: 203.6/194.5 EBL: 496.4/887.7 Transfusion (units): 0.43/1.16 Time to ambulation (days): 3.8/13.4 LOS: 9.5/15.2 ODI: 10.7/21.2 VAS back: 1.8/3.4 |
20.7/17.9 |
| Gahreman et al. [12] | Prospective 2004–2007 Very low | 25/27 | MIS: 12:13 Open: 13:14 |
MIS: 53 Open: 60 |
IS or DS | 12 (final) | 100 | OR time: 220/203†
Transfusion (units): 1/5† Time to ambulation (days): 2/4† LOS: 4/7† VAS back: 2/2† VAS leg: 5/7† |
NA |
| Harris et al. [15] | Retrospective NA Very low | 30/21 | MIS: 10:20 Open: 9:12 |
MIS: 69 Open: 66 |
DS | 12 (final) | NA | OR time: 150/156 EBL: 208/335 LOS: 2.5/3.2 VAS leg: 2.32/2.38 ODI: 13.9/6.4 |
13.3/14.3 |
| Isaacs et al. [16] | Retrospective 2001–2002 Very low | 20/24 | MIS: 7:13 Open: 16:8 |
MIS 58 Open: 51 |
Spondylolisthesis | NA | 100 | OR time: 300/276 EBL: 226/1147 Transfusion rate (%): 0/17 LOS: 3.4/5.1 |
5/25 |
| Kotani et al. [18] | Prospective 2005–? Very low | 43/37 | 27:53 | 65 | Spondylolisthesis | 24 (minimum) | NA | OR time: 172/176 EBL: 181/453 ODI: 13.2/32.1‡ |
2.3/0 |
| Lau et al. [19] | Retrospective 2005–2008 Very low | 10/12 | MIS: 40:60 Open: 42:58 |
MIS: 47 Open: 47 |
DDD (n = 11) Spondylolisthesis (n = 10) Pars defect (n = 1) |
MIS/open: 15.2/12.6 (mean) | 100 | OR time: 389.7/365.3 EBL: 466.7/464.6 Transfusion (mL): 200/428.6 Time to ambulation (days): 1.8/3.6 LOS: 5/6.2 |
40/8.3 |
| Lee et al. [20] | Prospective 2002–2008 Low | 72/72 | MIS: 20:52 Open: 22:50 |
MIS: 52.2 Open: 56.6 |
LDH, stenosis, spondylolisthesis | 24 (final) | MIS: 96 Open: 92 |
OR time: 166.4/181.8 EBL: 50.6/447.4 XR time: 49.0/17.6 Time to ambulation (days): 1.2/3.4 LOS: 3.2/6.8 VAS back: 2.3/2.4 VAS leg: 1.6/2.0 ODI: 21.4/10.7 |
12.5/9.7 |
| Mobbs et al. [22] | Prospective 2006–2010 Very low | 37/30 | MIS: 19:18 Open: 16:14 |
MIS: 69 Open: 67 |
DS (n = 27) IS (n = 13) Stenosis (n = 22) Scoliosis (n = 5) |
MIS/open: 11.5/18.7 (mean) | MIS: 90 Open: 73 |
Time to ambulation (days): 0.9/1.3 LOS: 5.9/9.7 ODI: 23.0/28.1 |
5.4/33.3 |
| Ntoukas and Muller [24] | Retrospective 2006–2008 Very low | 20/20 | MIS: 13:7 Open: 11:9 |
MIS: 57 Open: 59 |
DS | 12 (final) | 100 | OR time: 275/152 EBL: 135/432 XR time: 297/123 LOS: 5/10 ODI: 15/18 |
0/ 5.0 |
| Park and Ha [27] | Prospective 2003–2004 Very low | 32/29 | MIS: 8:24 Open: 13:16 |
MIS: 62 Open: 59 |
LDH, stenosis, spondylolisthesis | 12 (final) | 100 | OR time: 191.7/148.8 EBL: 432.8/737.9 Transfusion (units): 0.22/0.97 Time to ambulation (days): 1.22/2.97 LOS: 5.3/10.8 VAS back: 2.1/3.8 |
12.5/13.8 |
| Pelton et al. [28] | Retrospective 2008–2010Very low | 33/33 | MIS: 23:10 Open: 21:12 |
MIS: 52 Open: 50 |
DDD, stenosis with spondylolisthesis | 6 (final) | 100 | WC:OR time: 116/184 EBL: 127/338 LOS: 2/3VAS back: 4.1/5.9 Non-WC: OR time: 110/185 EBL: 224/288 LOS: 2/3 VAS back: 3.8/5.3 |
NA |
| Peng et al. [29] | Retrospective 2004–2006 Very low | 29/29 | MIS: 5:24 Open: 5:24 |
MIS: 54.1 Open: 52.5 |
DS | 24 (final) | NA | OR time: 216.4/170.5 EBL: 150/681 XR time: 105.5/35.2 Transfusions (units): 0/2 Time to ambulation (days): 2.3/4.1 LOS: 4.0/6.7 ODI: 16.2/17.5 |
6.9/13.8 |
| Rampersaud et al. [31] | Retrospective 2005–2008 Low | 37/41 | MIS: 18:19 Open: 21:20 |
MIS: 55 Open: 57 |
DS (n = 42) IS (n = 36) |
12 (final) | 100 | OR time: 222/227.4 EBL: 200.4/797.8 Transfusion rate (%): 0/17 LOS: 6.1/8.4 ODI: 18.9/33.7 |
10.8/29.3 |
| Scheufler et al. [33] | Retrospective 2003 Low | 53/67 | MIS: 23:28 Open: 33:29 |
MIS: 54.7 Open: 55.7 |
DS (n = 73) DDD (n = 47) |
16 (final) | 100 | 1-level: OR time: 104/132 EBL: 55/125 2-level: OR time: 175/192 EBL: 124/351 |
NA |
| Schizas et al. [34] | Prospective NA Very low | 18/18 | NA | MIS: 46 Open: 58 |
IS (n = 21) DDD or stenosis (n = 14) Iatrogenic spondylolisthesis (n = 1) |
22 (mean) | NA | OR time: 348/312 EBL: 456/961 LOS: 6.1/8.2 ODI: 33/26 |
16.7/11.1 |
| Starkweather et al. [35] | Prospective NA Very low | 17/18 | MIS: 10:7 Open: 8:10 |
MIS: 52 Open: 51 |
Lumbar instability | 1.5 (final) | 100 | OR time: 110/298 EBL: 96/427 LOS: 1.8/5 |
0/0 |
| Tsutsumimoto et al. [39] | Retrospective 2004–2006 Very low | 10/10 | MIS: 2:8 Open: 3:7 |
MIS: 61 Open: 64 |
DS | 24 (final) | 100 | OR time: 148.3/155.8 EBL: 282.0/352.6 |
NA |
| Villavicencio et al. [40] | Retrospective 2002–2004 Low | 76/63 | MIS: 34:42 Open: 24:39 |
MIS: 51 Open: 59 |
DDD ± spondylolisthesis, stenosis, or LDH | 37.5 (mean) | 100 | OR time: 214.9/222.5 EBL: 163.0/366.8 LOS: 3.0/4.2 |
Minor: 22.2/13.2Major: 0/9.5 |
| Wang et al. [41] | Prospective RCT 2006–2008 Low | 42/38 | MIS: 24:17 Open: 23:15 |
MIS: 51 Open: 57 |
DS (n = 25) LDH (n = 12) Stenosis (n = 42) |
32.7 (mean) | 100 | OR time: 168.7/145.0 EBL: 207.7/258.9 XR time: 92.7/43.9 LOS: 6.4/8.7 |
7.1/13.2 |
| Wang et al. [42] | Prospective 2006–2009 Very low | 42/39 | MIS: 13:29 Open: 12:27 |
MIS: 56 Open: 54 |
Spondylolisthesis (n = 29) Stenosis (n = 43) Iatrogenic instability (n = 9) |
36.1 (mean) | NA | OR time: 127/168 EBL: 274/645 XR time: 46/24 VAS back: 1.3/1.5 ODI: 18.2/17.4 |
9.5/17.5 |
| Wang et al. [43] | Prospective 2006–2008 Low | 42/43 | MIS: 13:29 Open: 16:27 |
MIS: 50 Open: 53 |
DS (n = 46) IS (n = 39) |
26.3 (mean) | 100 | OR time: 156/142 EBL: 264/673 XR time: 84/37 Transfusion (units): 0.12/1.47 LOS: 10.6/14.6 VAS back: 1.3/2.5 ODI: 10.8/12.1 |
9.5/7.0 |
| Wang et al. [44] | Prospective 2006–2008 Very low | 25/27 | MIS: 13:12 Open: 15:17 |
MIS: 55 Open: 56 |
Spondylolisthesis (n = 6) LDH (n = 15) Stenosis (n = 19) Instability (n = 12) |
27.5 (mean) | NA | OR time: 139/143 EBL: 291/652 XR time: 73/39 VAS back: 1.3/1.3 VAS leg: 1.0/1.0 ODI: 12.4/11.5 |
16.0/29.6 |
| Wang et al. [45] | Retrospective NA Very low | 52/22 | NA | MIS: 55 Open: 56 |
Spondylolisthesis, stenosis, or DDD | NA | 100 | 1-level: EBL: 145/400 LOS: 3.9/4.8 2-level:EBL: 187/493 LOS: 5.1/7.1 |
7.7/31.8 |
* Values are expressed as the median at final followup unless specified otherwise; †value are expressed as the mean; ‡represents outcome at 3 months; MIS = minimally invasive surgery; NA = not available; RCT = randomized controlled trial; DS = degenerative spondylolisthesis; IS = isthmic spondylolisthesis; LDH = lumbar disc herniation; DDD = degenerative disc disease; NA = not available; OR time = operative time (minutes); EBL = estimated blood loss (mL); LOS = length of stay (days); VAS = visual analog scale score for pain (points); ODI = Oswestry Disability Index (points); XR time = fluoroscopy time (seconds); WC = Workman’s Compensation Board.
Data Extraction
Relevant study data were extracted independently and in duplicate by the two study reviewers and entered into a custom electronic data extraction form (Appendix 2). Data elements of interest included a verification of study eligibility, study design, patient population demographics, interventions performed, study outcomes, statistical methods, and study results. Outcomes included operative time, fluoroscopy time, intraoperative EBL, length of hospital stay (LOS), VAS scores for back and leg pain, and ODI. Extracted data were then entered into a spreadsheet (Microsoft® Excel® 97-2004; Microsoft Corp, Redmond, WA, USA) by one reviewer (KM) with confirmation of accuracy being performed by a second reviewer (CLG).
Assessment of Study Quality
Two independent reviewers (CLG, YRR) assessed the methodologic quality of each included study. Information regarding study design, study quality, consistency of results, directness of evidence, and study precision was extracted from each paper. Based on this information, the overall quality of each study was rated as high, moderate, low, or very low according to the GRADE protocol [4]. Consensus regarding the final GRADE rating was arrived at through discussion by the two reviewers when necessary.
Based on the GRADE protocol, all of the studies, except for the single prospective randomized controlled trial by Wang et al. [41], which was rated initially as high quality, started with a low quality rating (Appendix 3). All included studies suffered from methodologic flaws resulting in downgrading of their quality. The single prospective randomized controlled trial [41] was given a low quality rating. Of the prospective comparative cohort studies, two retained their low-quality rating [20, 43] and nine were downgraded to very low quality [11, 12, 18, 22, 27, 34, 35, 42, 44]. Four of the retrospective comparative cohort studies stayed at a rating of low quality [1, 31, 33, 40] and 10 were downgraded to very low quality [3, 10, 15, 16, 19, 24, 28, 29, 39, 45].
Comparison of Patient Demographics in the MIS and Open Cohorts
The MIS and open cohorts in the 26 studies included 856 and 806 patients, respectively. Mean values for age, sex (% male), number of surgical levels, and preoperative diagnoses were calculated for those studies reporting on patient demographics. Between-group comparisons were performed using a two-sample t-test for continuous variables, a two-proportion z-test for number of surgical levels, and a chi-square test of independence for preoperative diagnosis. A p value of less than 0.05 was considered statistically significant. No significant differences were identified between the open and MIS cohorts with respect to age, sex, number of spinal levels treated, or preoperative diagnosis, although not all of the studies included the data required to be included in this between-cohort comparison (Table 2).
Table 2.
Comparison of patient demographic data in the MIS and open cohorts
| Variable | Number of studies | MIS cohort | Open cohort | p value |
|---|---|---|---|---|
| Number of patients | 26 | 856 | 806 | |
| Mean age (years) | 15 | 55.32 | 56.71 | 0.07† |
| Sex (% male) | 22 | 41 | 44 | 0.12‡ |
| Surgical level (%)* | 24 | 0.44§ | ||
| 1-level | 92 | 90 | ||
| 2-level | 8 | 9 | ||
| Diagnosis (%) | 14 | 0.25§ | ||
| Spinal stenosis | 20 | 17 | ||
| Degenerative spondylolisthesis | 40 | 42 | ||
| Isthmic spondylolisthesis | 17 | 17 | ||
| Degenerative disc disease | 15 | 13 | ||
| Other | 7 | 11 |
* One study had a separate category for 3+ level surgeries; this subsample was omitted; †independent two-sample t-test; ‡two-proportion z-test; §chi-square test of independence; MIS = minimally invasive surgery.
Results
Surgical End Points
Surgical time tended to be equivalent between the MIS and open cohorts (n = 23 studies [1, 10–12, 15, 16, 18–20, 24, 27–29, 31, 33–35, 39–44]), with surgery taking 104 to 390 minutes and 132 to 365 minutes in the MIS and open cohorts, respectively. EBL was generally lower in the MIS study arms (n = 23 studies [1, 10, 11, 15, 16, 18–20, 24, 27–29, 31, 33–35, 39–45]), with reported mean EBL ranging from 51 to 496 mL in the MIS groups and 125 to 1147 mL in the open groups. Fluoroscopy time was consistently higher in the MIS groups (n = 7 studies [20, 24, 29, 41–44]), with MIS patients being exposed to 49 to 297 seconds of fluoroscopy compared to 24 to 123 seconds in the open cohorts. LOS was shorter for the MIS cohorts (n = 21 studies [1, 3, 11, 12, 15, 16, 18–20, 22, 24, 27–29, 31, 34, 35, 40, 41, 43, 45]), with MIS patients experiencing a 1.8- to 11-day hospitalization compared to 3 to 15 days for the open patients. However, lack of randomization may have led to selection bias regarding case complexity and a trend toward lower EBL and shorter hospital LOS in MIS patients.
Patient-reported Outcomes
Postoperative pain was found to be equivalent at a variety of followup intervals in the 15 studies in which VAS was included [1, 11, 12, 15, 20, 22, 24, 27–29, 34, 40, 42–44]. ODI values were reported in 13 studies between 12 and 36 months postoperatively [1, 11, 15, 18, 20, 22, 24, 29, 31, 34, 42–44] and, based on the threshold for a minimal clinically important difference [32], were generally equivalent between the MIS and open cohorts (range: 10.7–33 for MIS versus 6.4–33.7 for open).
Adverse Events
Adverse events, including transfusion, were reported in all but three of the included studies [28, 33, 39] (Table 3). Trends toward fewer surgical complications, including dural tear, superficial infection, graft malposition, neurologic deficit or nerve injury, and hematoma, were observed in the MIS cohorts. There also seemed to be fewer adverse medical events, including urinary tract infection, respiratory complications, cardiac complications, and transfusions, in the MIS groups. However, the degree to which selection bias may have influenced these results cannot easily be quantified.
Table 3.
Complication rates in the MIS and open cohorts
| Outcome | Number of studies | Number of patients | Number of patients with complication/number of patients | |
|---|---|---|---|---|
| MIS cohort | Open cohort | |||
| Dural tear | 16 | 979 | 20/520 (3.8%) | 25/459 (5.4%) |
| Infection | 13 | 852 | 11/441 (2.5%) | 19/411 (4.6%) |
| Superficial | 6 | 354 | 4/178 (2.2%) | 11/176 (6.3%) |
| Deep | 5 | 332 | 5/176 (2.8%) | 4/156 (2.6%) |
| Surgical complications | 15 | 991 | 25/521 (4.8%) | 31/470 (6.6%) |
| Graft malposition | 5 | 422 | 6/219 (2.7%) | 9/203 (4.4%) |
| Screw malposition | 7 | 552 | 8/281 (2.8%) | 7/271 (2.6%) |
| Neurologic deficit/nerve injury | 9 | 633 | 8/343 (2.3%) | 11/290 (3.8%) |
| Hematoma | 4 | 282 | 3/156 (1.9%) | 4/126 (3.2%) |
| Medical complications | 13 | 854 | 18/441 (4.1%) | 49/413 (11.9%) |
| Urinary tract infection | 4 | 249 | 6/131 (4.6%) | 12/118 (10.2%) |
| Respiratory (pneumonia/atelectasis) | 4 | 296 | 2/150 (1.3%) | 5/146 (3.4%) |
| Cardiac (arrhythmia/myocardial infarction) | 3 | 206 | 1/108 (0.9%) | 4/98 (4.1%) |
| Transfusion required | 4 | 196 | 3/92 (3.3%) | 19/104 (18.3%) |
| Other | 5 | 359 | 6/191 (3.1) | 9/168 (5.4%) |
| Nonunion | 8 | 455 | 7/240 (2.9%) | 7/215 (3.3%) |
| Reoperation | 9 | 640 | 11/335 (3.3%) | 12/305 (3.9%) |
| For infection | 3 | 256 | 1/134 (0.7%) | 3/122 (2.5%) |
| For graft malposition | 3 | 242 | 2/129 (1.6%) | 2/113 (1.8%) |
| For hematoma | 1 | 30 | 0/15 (0%) | 1/15 (0.7%) |
| For screw malposition | 5 | 408 | 4/211 (1.9%) | 3/197 (1.5%) |
| For other reason | 3 | 188 | 4/95 (4.2%) | 1/93 (1.1%) |
| All complications* | 23 | 1420 | 81/743 (10.9%) | 131/677 (19.4%) |
* Not including reoperations; MIS = minimally invasive surgery.
Discussion
In many specialties, the introduction of MIS techniques has resulted in dramatic reduction of surgical morbidity and improved clinical outcomes resulting in near-universal adoption [13, 26, 38]. However, widespread application of MIS techniques to spine surgery remains controversial. In general, there has been a perceived lack of consistent evidence supporting clinical superiority of MIS compared to open fusion. Thus, uncertainty remains regarding the benefits required to offset the increased equipment cost and learning curve associated with adopting MIS lumbar fusion. Our systematic review, including more than 1600 patients from 26 studies, showed lower EBL, generally shorter hospital LOS, equivalent patient-reported outcomes, and a trend toward lower surgical and medical complications in patients undergoing MIS compared to open posterior lumbar fusion.
Limitations in study design significantly affect the quality of current CER pertaining to open versus MIS lumbar spinal fusion. The patient samples are small, ranging from 10 to 76 patients per treatment arm, and are often limited to nonconsecutive patients from a single institution, treated by a single surgeon. Furthermore, the decision to carry out open or MIS fusion is often dependent on a general shift in practice patterns of the enrolling surgeon who is likely biased in favor of MIS techniques [39], patient symptomatology [45] or diagnosis [34], patient preference [11, 12, 18, 19], or payment status [22, 27]. The resulting selection bias introduces the probability that observed differences in outcomes may be due to temporal shifts in practice, systematic differences in patient care, severity of disease, and/or patient expectations.
Despite these limitations, our comprehensive systematic review has identified differences in surgical end points that may favor MIS fusion. Patients in the MIS cohorts tended to lose less blood than their open counterparts with equivalent operative times, although selection bias related to underlying diagnosis and disease severity may have impacted these results. The tradeoff for this was higher fluoroscopy exposure in the MIS cohorts. Patients undergoing MIS fusion also showed a tendency for being discharged sooner from the hospital, although differences in postoperative care pathways, surgeon beliefs, and patient expectations may have influenced these results in favor of MIS fusion.
We have further identified that patient-reported outcomes, including VAS pain scores and ODI values, demonstrated equivalent intermediate-term clinical outcomes in patients undergoing MIS and open posterior lumbar fusion. However, the diagnostic heterogeneity in many of the studies [3, 10, 11, 19, 20, 22, 27, 28, 33–35, 40, 42, 44, 45] limits our ability to apply the results to any specific patient population. While diagnostic heterogeneity is less likely to influence surgical outcomes (ie, operative time and EBL) due to similarities in surgical technique across diagnostic categories, this is not the case with patient-reported outcomes, as clinical outcome of lumbar fusion is known to be dependent on primary diagnosis [14]. Given the low to very low quality of the existing literature and seemingly small differences in the effect sizes of MIS versus open fusion, the diagnostic heterogeneity of the patient populations intrinsic to each study likely creates a bias toward the null hypothesis.
Finally, our examination of adverse events related to posterior lumbar fusion suggests that MIS techniques may decrease both surgical and medical complications, including transfusion, without compromising the surgeon’s ability to obtain successful union. Our ability to draw definitive conclusions regarding complications is limited, however, by the significant variability in complication definitions, methods of complication diagnosis, and lack of blinded assessment of complications. The bias introduced by these study design flaws almost certainly impacts on the absolute rates of complications reported, and selection bias pertaining to disease severity may have influenced the results in favor of MIS fusion. However, transfusion of a single unit of blood costs USD 1200 [2] and each in-hospital complication experienced by a spine patient is estimated to cost USD 10,000 [17]. Although not the focus of our systematic review, three of the included studies did perform some form of economic analysis [28, 31, 45]. The economic analyses were also highly biased and further limited to the perspective of hospital cost only. These studies demonstrated potential direct cost savings ranging from 11% to 24% in favor of MIS procedures. Therefore, while further well-designed studies with a priori definitions of complications and prospective blinded assessment are required to accurately determine complication rates in MIS versus open lumbar fusion, decreases in complications, and secondarily cost, may be reasons for surgeons to consider adopting MIS techniques in light of the clinical equipoise and start-up costs associated with MIS spinal procedures.
In conclusion, while current evidence reporting on the comparative clinical effectiveness of MIS and open posterior lumbar fusion for degenerative pathology is of low quality and associated with substantial bias, the findings of our systematic review suggest equivalent clinical patient-reported outcomes and the possibility of improved surgical outcomes and lower complication rates for patients undergoing MIS compared to open posterior lumbar fusion. Further well-designed prospective observational studies or randomized trials are required to definitively determine the comparative effectiveness of MIS TLIF/PLIF for degenerative disorders.
Electronic supplementary material
Acknowledgments
We thank Dr. Dorin Rabin and Dr. Sooyong Chua for their assistance with a preliminary review of the literature and Ms. Oma Persaud MSc for her assistance with the electronic literature search.
Footnotes
One of the authors (YRR) certifies that he or she, or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000, US from Medtronic, Inc (Memphis, TN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability and quality of life. J Spinal Disord Tech. 2011;24:479–484. doi: 10.1097/BSD.0b013e3182055cac. [DOI] [PubMed] [Google Scholar]
- 2.Allen RT, Garfin SR. The economics of minimally invasive spine surgery. Spine (Phila Pa 1976). 2010;35(26 suppl):S373–S382. [DOI] [PubMed]
- 3.Bagan B, Patel N, Deutsch H, Harrop J, Sharan A, Vaccaro AR, Ratliff JK. Perioperative complications of minimally invasive surgery (MIS): comparison of MIS and open interbody fusion techniques. Surg Technol Int. 2008;17:281–286. [PubMed] [Google Scholar]
- 4.Brozek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW, Phillips B, Lelgemann M, Lethaby A, Bousquet J, Guyatt GH, Schunemann HJ, GRADE Working Group Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64:669–677. doi: 10.1111/j.1398-9995.2009.01973.x. [DOI] [PubMed] [Google Scholar]
- 5.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi SK, Lee KY, Lee SR. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007;32:2232–2237. [DOI] [PubMed]
- 7.Chow A, Mayer EK, Dari AW, Athanasiou T. Patient-reported outcome measures: the importance of patient satisfaction in surgery. Surgery. 2009;146:435–443. doi: 10.1016/j.surg.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 8.Deshpande PR, Rajan S, Sudeepthi BL, Abdul Nazir CP. Patient-reported outcomes: a new era in clinical research. Perspect Clin Res. 2011;2:137–144. doi: 10.4103/2229-3485.86879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhall SS, Wang MY, Mummanenni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9:560–565. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 11.Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J. 2010;19:316–324. doi: 10.1007/s00586-009-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gahreman A, Ferch RD, Rao PJ, Bogduk N. Minimal access versus open posterior lumbar interbody fusion in the treatment of spondylolisthesis. Neurosurgery. 2010;66:296–304. doi: 10.1227/01.NEU.0000363600.24074.D0. [DOI] [PubMed] [Google Scholar]
- 13.Garry R, Fountain J, Mason S, Napp V, Brown J, Hawe J, Clayton R, Abbott J, Phillips G, Whittaker M, Lilford R, Bridgman S. The eVALuate study: two parallel randomized trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ. 2004;328:129–135. doi: 10.1136/bmj.37984.623889.F6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glassman SD, Carreon LY, Djurasovic M, Dimar JR, Johnson JR, Puno RM, Campbell MJ. Lumbar fusion outcomes stratified by specific diagnostic indication. Spine J. 2009;9:13–21. doi: 10.1016/j.spinee.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 15.Harris EB, Sayadipour A, Massey P, Duplantier NL, Anderson DG. Mini-open versus open decompression and fusion for lumbar degenerative spondylolisthesis with stenosis. Am J Orthop. 2011;40:E257–E261. [PubMed] [Google Scholar]
- 16.Isaacs RE, Podichetty VK, Santiago P, Sandhu FA, Spears J, Kelly K, Rice L, Fessler RG. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 17.Kalanithi PS, Patil CG, Boakye M. National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976). 2009;34:1963–1969. [DOI] [PubMed]
- 18.Kotani Y, Abumi K, Ito M, Sudo H, Abe Y, Minami A. Mid-term clinical results of minimally invasive decompression and posterolateral fusion with percutaneous pedicle screws versus conventional approach for degenerative spondylolisthesis with spinal stenosis. Eur Spine J. 2012;21:1171–1177. doi: 10.1007/s00586-011-2114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF) J Clin Neurosci. 2011;18:624–627. doi: 10.1016/j.jocn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21:2265–2270. doi: 10.1007/s00586-012-2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, Sullivan SD. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299:656–664. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 22.Mobbs RJ, Sivabalan P, Li J. Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci. 2012;19:829–835. doi: 10.1016/j.jocn.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Methods of systematic reviews and meta-analysis. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 24.Ntoukas V, Muller A. Minimally invasive approach versus traditional open approach for one level posterior lumbar interbody fusion. Minim Invasive Neurosurg. 2010;53:21–24. doi: 10.1055/s-0030-1247560. [DOI] [PubMed] [Google Scholar]
- 25.O’Leary TJ, Slutsky JR, Bernard MA. Comparative effectiveness research priorities at federal agencies: the view from the Department of Veterans Affairs, National Institute on Aging, and Agency for Healthcare Research and Quality. J Am Geriatr Soc. 2010;58:1187–1192. doi: 10.1111/j.1532-5415.2010.02939.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pace KT, Dyer SJ, Stewart RJ, Honey RJ, Poulin EC, Schiachta CM, Mamazza J. Health-related quality of life after laparoscopic and open nephrectomy. Surg Endoscopy. 2003;17:143–152. doi: 10.1007/s00464-002-8902-y. [DOI] [PubMed] [Google Scholar]
- 27.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine (Phila Pa 1976). 2007;32:537–543. [DOI] [PubMed]
- 28.Pelton MA, Phillips FM, Singh K. A comparison of perioperative costs and outcomes in patients with and without Workers’ compensation claims treated with MIS or open TLIF. Spine (Phila Pa 1976). 2012;37:1914–1919. [DOI] [PubMed]
- 29.Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2009;34:1385–1389. [DOI] [PubMed]
- 30.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 31.Rampersaud YR, Gray R, Lewis SJ, Massicotte EM, Fehlings MG. Cost-utility analysis of posterior minimally invasive fusion compared with conventional open fusion for lumbar spondylolisthesis. SAS J. 2011;5:29–35. doi: 10.1016/j.esas.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rihn JA, Berven S, Allen T, Phillips FM, Currier BL, Glassman SD, Nash DB, Mick C, Crockard A, Albert TJ. Defining value in spine care. Am J Med Qual. 2009;24(6 suppl):4S–14S. doi: 10.1177/1062860609349214. [DOI] [PubMed] [Google Scholar]
- 33.Scheufler K, Dohmen H, Vougiokas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007;60(4 suppl 2):203–212. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]
- 34.Schizas C, Tzinieris N, Tsiridis E, Kosmopoulos V. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009;33:1683–1688. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Starkweather AR, Witek-Janusek L, Nockels RP, Peterson J, Mathews HL. The multiple benefits of minimally invasive spinal surgery: results comparing transforaminal lumbar interbody fusion and posterior lumbar fusion. J Neurosci Nurs. 2008;40:32–39. doi: 10.1097/01376517-200802000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 37.Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE. 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine (Phila Pa 1976). 1997;22:2813–2822. [DOI] [PubMed]
- 38.Topcu O, Karakayali F, Kuzu MA, Ozdemir S, Erverdi N, Eihan A, Aras N. Comparison of long-term quality of life after laparoscopic and open cholecystectomy. Surg Endoscopy. 2003;17:291–295. doi: 10.1007/s00464-001-9231-2. [DOI] [PubMed] [Google Scholar]
- 39.Tsutsumimoto T, Shimogata M, Ohta H, Misawa H. Mini-open versus conventional open posterior lumbar interbody fusion for the treatment of lumbar degenerative spondylolisthesis. Spine (Phila Pa 1976). 2009;34:1923–1928. [DOI] [PubMed]
- 40.Villavicencio AT, Burneikiene S, Roeca CM, Nelson EL, Mason A. Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int. 2010;1:12. doi: 10.4103/2152-7806.63905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang H, Lu F, Jiang J, Ma X, Xiz X, Wang L. Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: a prospective randomized clinical trial. Chin Med J. 2011;124:3868–3874. [PubMed] [Google Scholar]
- 42.Wang J, Zhou Y, Feng Zhang Z, Qing Li C, Jie Zheng W, Liu J. Comparison of clinical outcome in overweight or obese patients after minimally invasive versus open transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2012 May 17 [Epub ahead of print]. [DOI] [PubMed]
- 43.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19:1780–1784. doi: 10.1007/s00586-010-1404-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011;20:623–628. doi: 10.1007/s00586-010-1578-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang MY, Cummock MD, Yu Y, Trivedi RA. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J Neurosurg Spine. 2010;12:694–699. doi: 10.3171/2009.12.SPINE09621. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson ANA, Birkmeyer N, Herkowitz H, Longley M, Lenke L, Emery S, Hu S. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91:1295–1304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.