Abstract
Background
Age, sex, and medical comorbidities may be associated with differences in patient-reported outcome scores after THA. Highest level of education may be a surrogate for socioeconomic status, but the degree to which this is associated with patient-reported outcomes after THA is not known.
Questions/purposes
We investigated the national Swedish Hip Arthroplasty Register for the association of education attainment on patient-reported outcomes 1 year after THA; specifically, we evaluated level of education attainment against health-related quality of life (HRQoL), pain reduction, and satisfaction with treatment 1 year after THA.
Methods
All THAs for osteoarthritis performed from 2005 through 2007 with complete patient-reported outcome measures (representing 49% of the THAs performed for this diagnosis) were selected from the Swedish Hip Arthroplasty Register. These cases were merged with national databases containing education attainment, marital status, and comorbidities (n = 11,464; mean age of patients, 64 years). The patient-reported outcome measure protocol included the HRQoL measure EuroQol five-dimension scale (EQ-5D), a VAS for pain, the Charnley classification survey, and a VAS addressing THA satisfaction. Linear regression analyses determined the association of preoperative patient factors with patient-reported outcomes.
Results
High education attainment was associated with higher HRQoL (EQ-5D index ßhigh = 0.03 ± 0.01; EQ VAS ßhigh = 2.6 ± 0.5) after THA, whereas those with low and medium education were at risk for lower HRQoL. High education was associated with less pain after treatment (ßhigh = −3.3 ± 0.05). Individuals with low or medium education were at risk for less satisfaction with THA (p < 0.001).
Conclusions
Our results suggest clinicians should support patients with low and medium education to a greater extent. Identification of patients who will benefit most from THA and educating those at risk for poorer outcomes, like patients with low and medium education, ultimately may improve patient satisfaction, HRQoL, pain, and the cost utility of THA.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3504-2) contains supplementary material, which is available to authorized users.
Introduction
Historically, THA success has been defined by implant survivorship and radiographic evaluation. However, neither of those assessments gives the clinician a sense of how the patient feels about the influence the treatment had on his or her life. Although the long-term surgical success of THA is well documented, clinicians now have additional tools for evaluation through patient-reported outcome measures. Patient-reported outcome measures provide a patient’s self-reported assessment of his or her condition. Implementation of patient-reported outcome measures in the clinic or by mail can provide information to improve treatment by THA. Patient-reported outcomes include health-related quality of life (HRQoL), pain assessment, and satisfaction with treatment. Understanding patient factors that influence THA outcomes can aid clinicians when assessing risk factors for poor results. Risk adjustment is important in statistical analysis because patient demographic data then can be correlated to patient-reported outcomes to gain a better understanding of how patient groups differ after THA and to identify groups at risk for poor outcomes allowing targeted care to reduce those risks. Age, sex, and comorbidities are common patient factors considered before primary and revision THAs [1, 21, 25]. Identification of additional risk factors such as socioeconomic or social support status may allow physicians to more accurately anticipate their patients’ results from treatment.
Socioeconomic status is determined by three factors: an individual’s occupation, his or her income, and the highest level of education attained. Education fundamentally influences occupation and income by determining the types of jobs available, the probability of unemployment, and therefore the individual’s income [23]. Particularly in health studies, education attainment may be used as a proxy for socioeconomic status [4, 10]. Education typically is complete early in life, whereas chronic conditions of aging, like osteoarthritis (OA), tend to present later in life [4]. Unlike income and occupation, education largely remains stable throughout an adult’s lifespan and thus represents a more constant measure of socioeconomic status. Individuals not part of the workforce such as homemakers, the unemployed, the retired, and those on disability are included when socioeconomic status determination considers education attainment rather than occupation or income. Finally, when investigating the effect of socioeconomic status on health, education is the least likely factor to be changed by disease [10]. Even so, there are differing accounts regarding whether an individual’s socioeconomic status is associated with outcomes like functional status, HRQoL, and satisfaction after surgery [2, 8, 16, 24]. For analyses of this sort, many of the groups studied have been relatively small with patient populations of 1000 or less.
In this study, we therefore explored how patient socioeconomic status was associated with patient-reported outcomes 1 year after THA in 11,464 patients from a nationwide cohort. The aim was to determine if higher educational attainment resulted in more favorable measures of HRQoL, pain reduction, and greater satisfaction with treatment 1 year after THA.
Patients and Methods
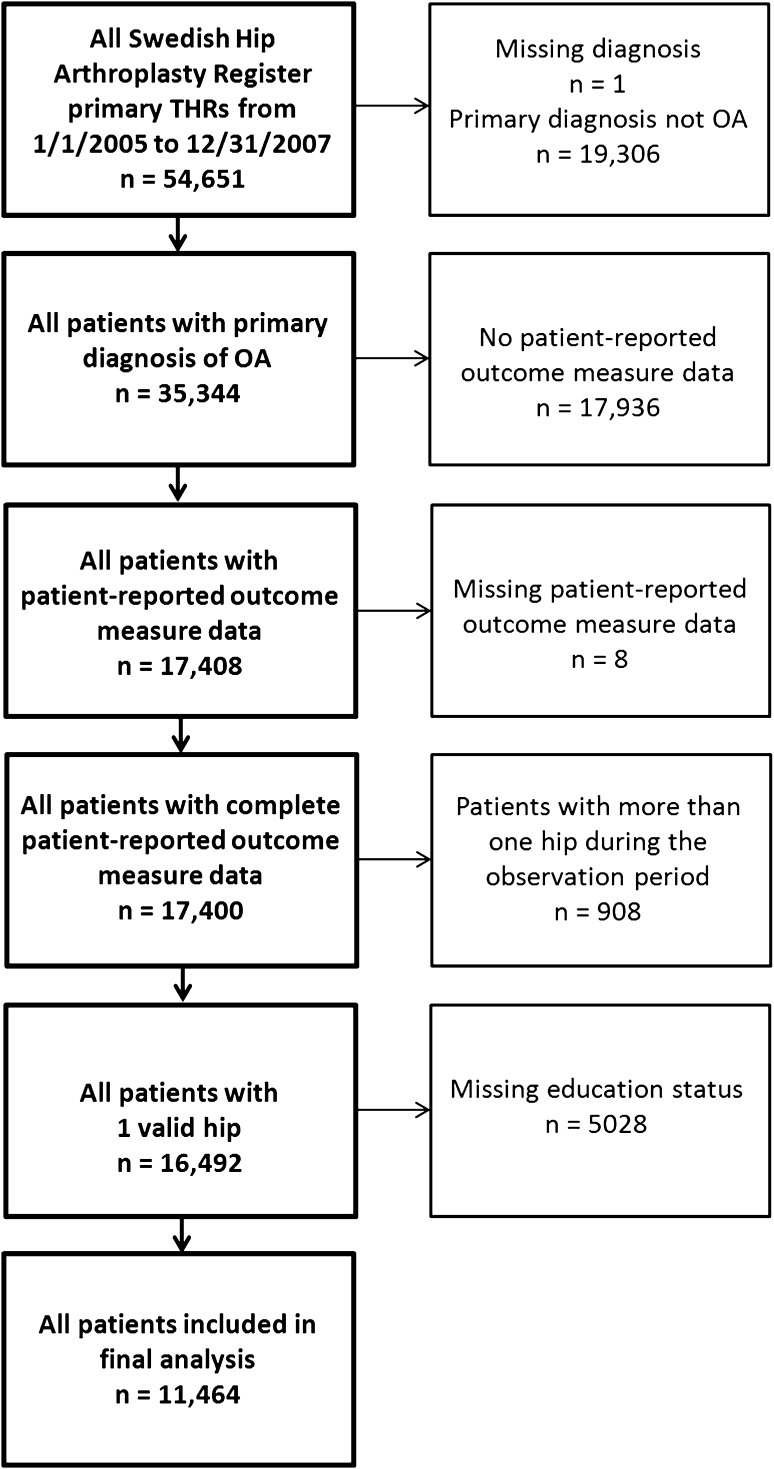
The population of this prospective, observational national registry study included all patients with OA having primary THA performed from January 2005 through December 2007 from the Swedish Hip Arthroplasty Register (n = 54,651). Complete preoperative and 1-year postoperative patient-reported outcome measures were required for inclusion. The patient-reported outcome measure protocol was implemented in the register in 2002. Three-quarters of hospitals were participating in 2005, and by 2007, 92% of hospitals were administering the surveys. The patient-reported outcome measure protocol includes the EuroQol group HRQoL measure EQ-5D, a VAS for pain (from 0 to 100, where 0 was no pain), the Charnley classification survey, and a VAS addressing satisfaction with the outcome of surgery at 1 year (from 0 to 100, where 0 was complete satisfaction with treatment) [3, 7]. Details of implementation of this ethically approved protocol and each patient-reported outcome measure have been reported [22]. For the purpose of homogeneity, patients who died or underwent reoperation within 1 year of surgery were excluded from the analysis. If an individual had bilateral primary THAs during the sample period, the first hip with complete preoperative and 1-year postoperative patient-reported outcome measures was included in the analysis. Whether the hip included in the analysis was the first or second in the selection period was noted. After ethical review board approval (328-08), these cases were merged with national statistics databases recording comorbid conditions (the National Patient Registry of the National Board of Health and Welfare) and the highest recorded level of education achieved according to the International Standard Classification of Education (ISCED) 97 standard and marital status from Statistics Sweden. Only individuals with educational attainment information were included in the final analysis, totaling 11,464 patients (Fig. 1).
Fig. 1.
A flow diagram shows patient selection from the Swedish Hip Arthroplasty Register for the final linear regression analyses.
Patients lacking education data tended to be older; however, there was no difference in preoperative or postoperative patient-reported outcome measure scores between the patients with and without educational status in the database (Appendix 1. Supplemental material is available with the online version of CORR). Charlson’s comorbidity index was calculated from all comorbid diagnoses 2 years before surgery. Classification of individuals was based on the presence or absence of comorbid conditions; 9863 individuals had no comorbidities. Education was divided into three levels: low (no education beyond primary school [up to 8 years]); medium (no education beyond secondary school [9–12 years]); and high (any postsecondary education). Marital status was defined as single, married, or widowed as a measure of social support (Table 1).
Table 1.
Population demographic summary
| Patient demographics | Summary values |
|---|---|
| Mean age (years, SD) | 64 (7.9) |
| Patient count (female) | 11,464 (6226) |
| Charnley class count (%) | |
| A | 4952 (43) |
| B | 1591 (14) |
| C | 4921 (43) |
| Hip order count (%) | |
| First | 9146 (80) |
| Second | 2318 (20) |
| Marital status count (%) | |
| Single | 3105 (27) |
| Married | 7181 (63) |
| Widowed | 1178 (10) |
| Education level count (%) | |
| Low | 4257 (37) |
| Medium | 4916 (43) |
| High | 2291 (20) |
Statistical Methods
The outcomes at 1 year were dependent variables: EQ-5D index, EQ VAS, pain VAS, and satisfaction VAS. Bayesian model averaging identified the significant predictors of each outcome parameter [12]. Bayesian model averaging does not base inference on a single model, but on a combination of models; thus it avoids model selection bias and has good specificity without compromising sensitivity [9]. Decisions regarding the importance of a predictor in the model are based on the estimated posterior probability. The literature does not consider a variable supported by Bayesian model averaging if the posterior inclusion probability is less than 50% indicating that the variable does not contribute to or influence the outcome [20]. The independent variables tested by Bayesian model averaging were age, sex, Charnley classification, presence of comorbidities, whether the included hip was the first or second in the time interval, the preoperative EQ-5D index and EQ VAS, the preoperative pain VAS, marital status, and education level. The preoperative EQ-5D index and the EQ VAS were included when conducting Bayesian model averaging because these outcome scores represented slightly different elements of preoperative HRQoL. The index reflected a weighted population-based representation of the five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), and the EQ VAS was an overview of the patient’s impression of their HRQoL on that day. Significant variables (minimum of 0.50 posterior probability thresholds) were included in the final linear regression analyses to determine the effect of each preoperative patient factor on the outcome parameter in question [9, 15].
Of the independent variables tested, education attainment, preoperative HRQoL, and Charnley classification were associated with each of the outcome parameters and therefore were included in all linear regression models. The majority of variables selected through Bayesian model averaging had a posterior probability threshold of 1.00 indicating that they were definitive predictors and were included in the final linear regression models (Table 2). None of the predictors tested were excluded from all linear models.
Table 2.
Posterior probability threshold of each independent variable for the outcome parameters as determined by Bayesian model averaging*
| Predictors | Patient-reported outcomes | |||
|---|---|---|---|---|
| EQ-5D index | EQ VAS | Pain VAS | Satisfaction VAS | |
| Age | 0.00 | 0.06 | 1.00† | 1.00† |
| Sex | 1.00† | 0.00 | 0.13 | 1.00† |
| Comorbidity | 1.00† | 1.00† | 0.00 | 0.20 |
| Charnley classification | 1.00† | 1.00† | 1.00† | 1.00† |
| Preoperative EQ-5D index | 1.00† | 1.00† | 1.00† | 0.83† |
| Preoperative EQ VAS | 1.00† | 1.00† | 1.00† | 1.00† |
| Preoperative pain VAS | 0.00 | 0.00 | 0.80† | 0.00 |
| Hip order | 0.00 | 1.00† | 0.00 | 1.00† |
| Marital status | 0.13 | 0.00 | 1.00† | 0.07 |
| Education level | 1.00† | 1.00† | 1.00† | 1.00† |
* Any variable with a probability ≥ 0.50 was subsequently included in the linear regression model for that outcome parameter (indicated by †).
Variable regression coefficients were assessed (reported as ß with a subscript indicator) and standard deviations and CI were calculated to determine the influence of each significant variable on the outcomes. Regression coefficients from linear regression are an easy to interpret effect measure; for a unit increase in the exposure holding all other variables constant, the expected change in the outcome equals the regression coefficient (ß). For a continuous variable, this denotes a unit increase. For example, if the coefficient for the EQ VAS (ßEQ VAS) were 1, a score of 0 would increase to 1. However, if we are interested in only fractions of a unit increase, then the regression coefficient can be divided by the factor of the unit increase in which we are interested (eg, for a 0.1 unit increase divide the regression coefficient by 10). For a categorical exposure, the regression coefficient gives the expected difference of the outcome means between the two groups. Statistical analyses were performed using the R computing environment (Version i386 2.15.2) [19].
Results
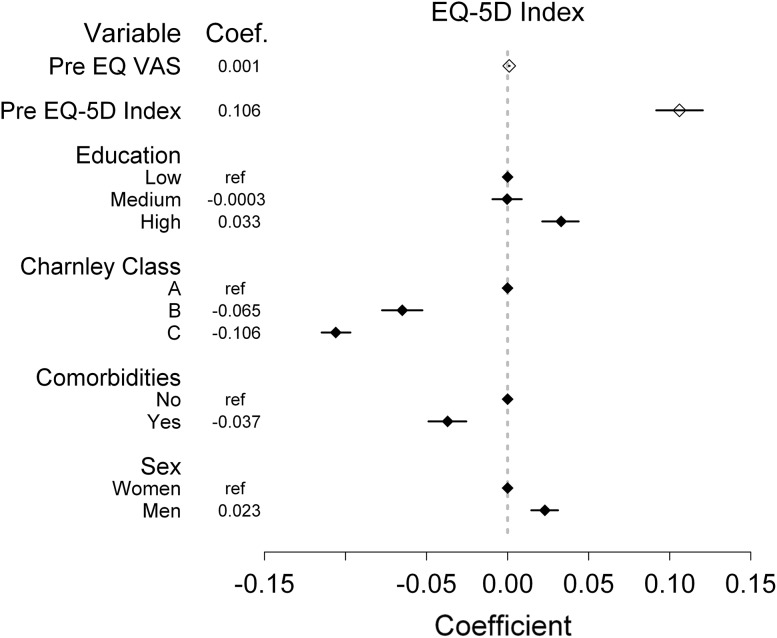
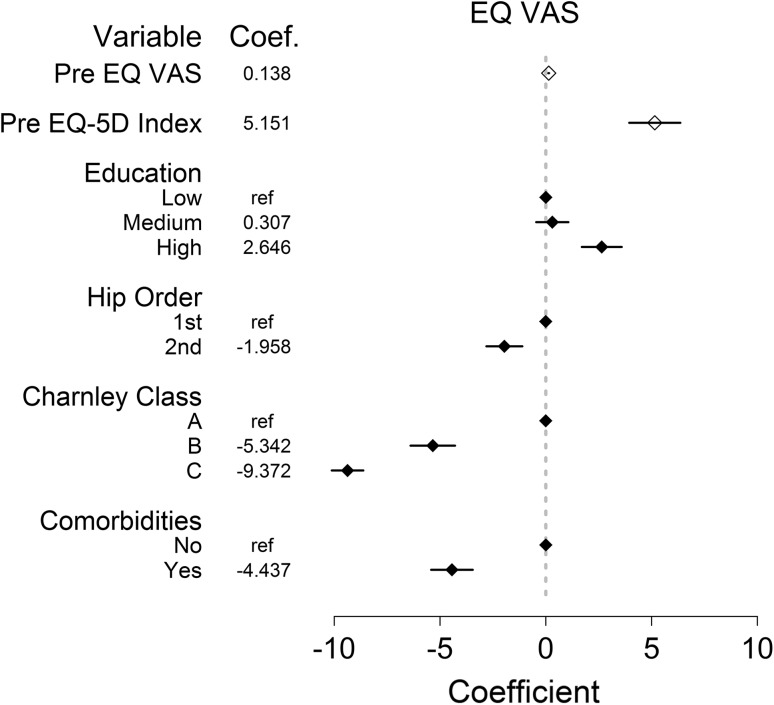
Regardless of education attainment, on average HRQoL improved and pain decreased in all groups after THA (Table 3), but postoperative HRQoL measured by the EQ-5D index (Fig. 2) and the EQ VAS (Fig. 3) were associated with preoperative HRQoL states and with education attainment, Charnley classification, and the presence of comorbidities. The better the preoperative HRQoL of the individual (EQ-5D index ßindex = 0.11 ± 0.01 and ßEQ VAS = 0.001 ± 0.0001; EQ VAS ßindex = 5.2 ± 0.6 and ßEQ VAS = 0.14 ± 0.01), the greater the chance was of a high postoperative HRQoL. High education attainment also was associated with higher HRQoL (EQ-5D index ßhigh = 0.03 ± 0.01; EQ VAS ßhigh = 2.6 ± 0.5) postoperatively. Individuals with Charnley classification B or C disease and those with comorbidities had a greater risk of poorer HRQoL postoperatively measured by the EQ-5D index (Fig. 2) and the EQ VAS (Fig. 3), (all p < 0.001). Men were associated with more favorable weighted EQ-5D index scores (ß = 0.02 ± 0.004) than women (reference) after surgery. However, when measuring HRQoL through the EQ VAS, the variable of sex was not associated with patient-reported scores.
Table 3.
Mean (SD) patient-reported outcome measure scores preoperatively, 1 year postoperatively, and the change during this period stratified by education level
| Patient-reported outcome measure | All patients | Low | Medium | High | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop erative score | Postoperative score | Score change | Preoperative score | Postoperative score | Score change | Preoperative score | Postoperative score | Score change | Preoperative score | Postoperative score | Score change | |
| EQ-5D index*+^ | 0.42 (0.31) | 0.79 (0.23) | 0.37 (0.34) | 0.42 (0.31) | 0.79 (0.24) | 0.36 (0.35) | 0.41 (0.31) | 0.79 (0.24) | 0.37 (0.34) | 0.43 (0.31) | 0.82 (0.22) | 0.39 (0.34) |
| EQ VAS*+^ | 54.2 (22.2) | 77.3 (19.8) | 23.1 (26.1) | 54.3 (21.8) | 76.5 (20.2) | 22.2 (26.5) | 53.5 (22.5) | 76.8 (20.0) | 23.4 (26.2) | 55.4 (22.4) | 79.8 (18.2) | 24.4 (25.0) |
| Pain VAS*+^ | 61 (17) | 14 (18) | −47 (23) | 61 (17) | 15 (17) | −46 (23) | 61 (16) | 14 (20) | −47 (23) | 60 (16) | 11 (20) | −49 (22) |
| Satisfaction+ | – | 16 (20) | – | – | 16 (20) | – | – | 16 (21) | – | – | 14 (20) | – |
* Preoperative scores; +postoperative scores; ^changes from preoperative to postoperative scores among the low, medium, and high education levels were significantly different at p ≤ 0.01.
Fig. 2.
Linear regression results are shown for the independent variables (preoperative [pre] EQ VAS, preoperative EQ-5D index, education attainment, Charnley classification, comorbidities, and sex) included in the model where the points represent the slope coefficient (coef.) with the 95% CI for the dependent postoperative EQ-5D index variable. Any variable without a CI was the reference variable (ref), and any variable whose CI did not include 0 represents a significant influence on the EQ-5D index. Continuous variables are represented by an open diamond and categorical variables are represented by a filled diamond.
Fig. 3.
Linear regression results are shown for the independent variables (preoperative [Pre] EQ VAS, preoperative EQ-5D index, education attainment, hip order, Charnley classification, and comorbidities) included in the model where the points represent the slope coefficient (coef.) with the 95% CI for the dependent EQ VAS variable. Any variable without a CI was the reference variable (ref), and any variable whose CI did not include 0 represents a significant influence on the EQ VAS. Continuous variables are represented by an open diamond and categorical variables are represented by a filled diamond.
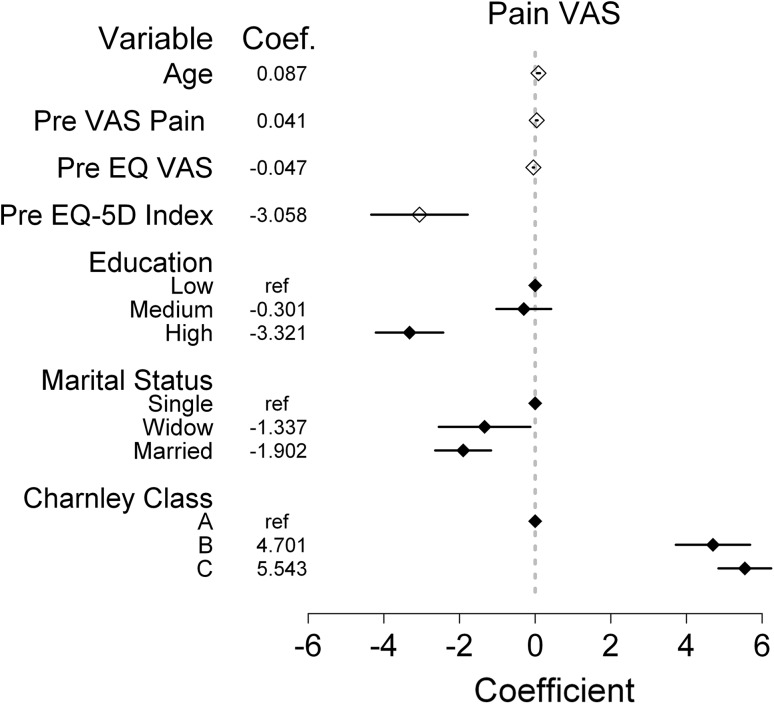
Age and preoperative VAS pain were not associated with HRQoL after THA; however, they were important predictors of postoperative pain (ßage = 0.1 ± 0.02; ßpain = 0.04 ± 0.01) as were both preoperative measures of HRQoL (ßindex = −3.1 ± 0.7; ßEQ VAS = −0.05 ± 0.01). Older individuals, patients with greater preoperative pain, and those with worse HRQoL before surgery were at greater risk of higher levels of postoperative pain, which was reflected in the regression coefficients (p < 0.001). As seen with the postoperative EQ-5D index and EQ VAS, a high level of education was associated with lower pain after THA (ßhigh = −3.3 ± 0.5), whereas low and medium levels of education failed to have a significant association with pain reduction after surgery (Fig. 4). That is not to say that patients with low or medium education levels did not have improvements in pain, just that their education was not associated with their pain reduction. Once again having a Charnley classification of B (ß = 4.7 ± 0.5) or C (ß = 5.5 ± 0.4) increased the risk of more pain after THA. Single individuals (reference) were at greater risk of pain after surgery when compared with married (ß = −1.9 ± 0.4) or widowed (ß = −1.3 ± 0.6) individuals (Fig. 4).
Fig. 4.
Linear regression results of the independent variables (age at surgery, preoperative [Pre] pain VAS, preoperative EQ VAS, preoperative EQ-5D index, education attainment, marital status, and Charnley classification) included in the model where the points represent the slope coefficient (coef.) with the 95% CI for the dependent pain VAS variable. Any variable without a CI was the reference variable (ref), and any variable whose CI did not include 0 represents a significant influence on the pain VAS. Continuous variables are represented by an open diamond and categorical variables are represented by a filled diamond.
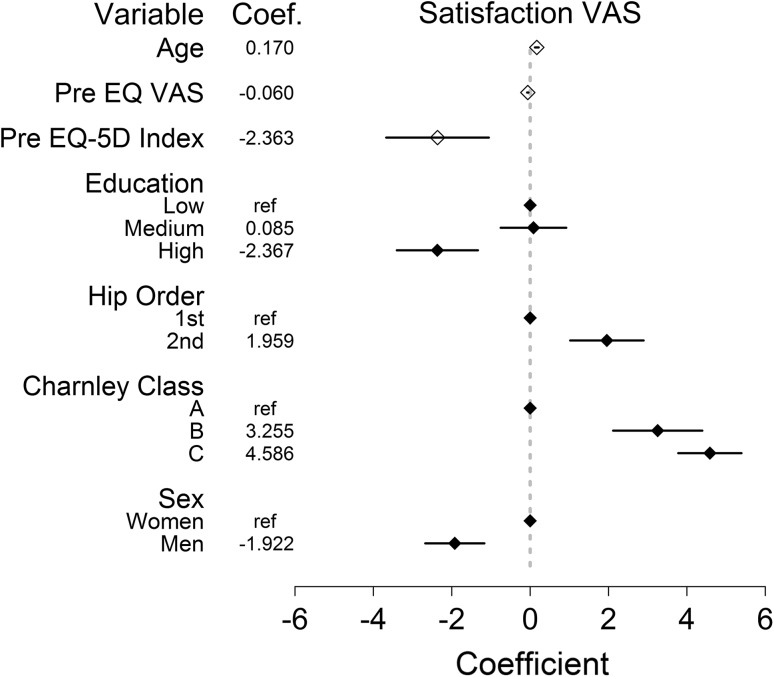
Most of the tested predictors, with the exception of marital status and comorbidities, were associated with patient satisfaction with their THA 1 year after surgery. Women, individuals with Charnley classification B or C, older people, and those with low or medium education levels were associated with less satisfaction (Fig. 5) (all p < 0.001).
Fig. 5.
Linear regression results of the independent variables (age at surgery, preoperative [Pre] EQ VAS, preoperative EQ-5D index, education attainment, hip order, Charnley classification, and sex) included in the model where the points represent the slope coefficient (coef.) with the 95% CI for the dependent satisfaction variables. Any variable without a CI was the reference variable (ref), and any variable whose CI did not include 0 represents a significant influence on the satisfaction. Continuous variables are represented by an open diamond and categorical variables are represented by a filled diamond.
Discussion
Identification of patient factors, in addition to sex, age, and comorbidity status that are associated with patient-reported outcomes after THA, is vital for accurate risk adjustment and patient education before surgery. We investigated how level of education attainment as a surrogate for socioeconomic status was associated with differences in patient-reported outcomes 1 year after THA. Controlling for sex, age, Charnley class, comorbidities, and preoperative health states, our analyses found that higher education attainment, representing higher socioeconomic status, was associated with more favorable patient-reported outcomes. A positive association was found with HRQoL, less postoperative pain, and satisfaction in individuals with any postsecondary education.
Exclusion of occupation and income in this investigation of socioeconomic status may have distorted our results. However, groups incorporating these factors found that education was an independent predictor of OA and surgical outcomes [2, 4, 10, 13, 18]. Biases may be introduced if considering the excluded determinants because there may be reverse causation between OA and occupation and/or income. Low-income jobs tend to be more labor intensive increasing the chances of OA just as severe OA may result in decreased earnings or job loss [4, 18]. Of the determinants of socioeconomic status, education occurs earliest in life and is the most constant regardless of disease [4, 10]. In patients with OA, education is a useful measure of socioeconomic status because it likely would be complete before the onset of OA. However, we cannot confirm this because income and occupation were not collected nor incorporated in our analyses.
Generalizability of our findings to non-Swedish populations may be limited by the use of education attainment. National education systems can vary substantially. We did our best to mitigate this by categorizing education attainment. The use of education as a continuous variable could be misleading when comparing nations because the minimum number of required years of childhood education varies. This inconsistency could influence how education attainment is interpreted with respect to health outcome studies among nations. Another possible limitation of this study is the use of patient-reported outcome measures with bounded scores; however, these limitations hold true for all patient-reported outcome investigations. Whenever a score has an upper or lower bound such as the EQ-5D index or VAS scores, there is the chance for ceiling or floor effects. Individuals who start near the top on these scales with the best health states leave little room to measure improvement after treatment. Therefore, some sensitivity of the scales or statistical power might be lost owing to patients with high preoperative scores. Our population size was such that sufficient statistical power or skewed data were not a concern.
Differences in the postoperative scores between the different education groups may appear small at the population level (0.03 for the EQ-5D index, 2.2 on the EQ VAS, 4 on the pain VAS, and 2 on the satisfaction VAS), and some might argue that they are too small to find clinically relevant. However, variations among the groups exist such that linear regression analyses were able to identify differences in patient-reported outcomes among groups of patients with low, medium, and high levels of education after controlling for other patient factors. Several methods exist to calculate the minimal important difference (MID) between groups, but these calculations differ greatly and consensus regarding which to use does not exist [17]. The significance of a MID is dependent on the population used to calculate the value. MIDs calculated from individual responses may not translate to changes measured on the population level. Walters and Brazier [27] aimed to identify a MID for the EQ-5D index from eight longitudinal studies and identified MID values ranging from −0.011 to 0.140, and while their solution was to average these values for a MID of 0.074, their CIs were large indicating uncertainty in this calculation. Universal MID values for patient-reported outcome measures theoretically are appealing, but without a strong understanding of the implications of the MID on the patient versus the population level or without a criterion standard, which is impossible in preference-based measures, they can be misleading. No such standardized MID scores exist for the EQ-5D or pain VAS in a Swedish population with OA. Subgroups in our population show significant differences in the extent of benefits of treatment with THA. Such is the nature of averages, not all patients with a low education level had poorer outcomes; however, enough of these patients did not improve in HRQoL or have as much pain reduction as those with a high education level to have as high a population average in their postoperative outcome scores. This indicates that some portion of the patients with low and medium education should receive more targeted care.
A better understanding of the mechanism with which patients of varying education recover after THA is important for presurgical evaluation. Twenty percent of postoperative physical activity variance after THA is associated with education, age, and family status [26]. Education teaches individuals how to seek and process information on a progressively higher level, enabling greater self-sufficiency and a feeling of control of one’s well-being [23]. Patients with higher education in our population may have had greater medical knowledge, increased ability to apply practical knowledge, and more realistic expectations for their surgery. In addition, their higher HRQoL scores preoperatively and postoperatively suggest that they were more prone to seek medical advice and may have been more motivated during their rehabilitation. Patients at risk for less postoperative activity such as those with lower education need to be informed of this risk and encouraged to increase postoperative activity. Perhaps if patients with low and medium education received individualized preoperative instruction outlining practical expectations and the importance of postoperative activity, they may have more realistic expectations and greater success after surgery.
THA is commonly an elective procedure performed to improve HRQoL through increased activity and decreased pain, and the majority of patients experience improvement in these areas, particularly those with high education. Failure to alleviate pain however is associated with dissatisfaction after surgery [1]. Patients with low and medium education were associated with more pain and less satisfaction. If their function did not improve to desired levels, this and unalleviated pain may have resulted in less satisfaction with the treatment at 1 year. Individuals undergoing THA for their second hip were also associated with less treatment satisfaction at 1 year. More evidence is necessary to establish the cause of this trend. Patient satisfaction will continue to be an important outcome for elective joint arthroplasty, and dissatisfaction needs to be better understood. Although the differences identified in our study sometimes were small in magnitude at the population level, we believe they are important. Each of the significant factors identified is associated with how the patients do after THA. Our goal is to identify as many patient factors as possible, with the goal of eventually creating a decision-making tool for patients with OA before surgery. No one patient factor will explain all of the changes seen after surgery, but it is important to recognize that patient-reported outcomes may be influenced by a large number of variables, each exacting a small but detectable, and potentially important, influence on the overall clinical picture.
In the literature, associations between education and surgical outcomes have been explored using numerous patient-reported outcome measures [2, 8, 16, 24]. When investigating postoperative function, an American study found that lack of a college education was associated with poorer function after THA [2]. In a German population, positive associations were found with increases in the WOMAC in patients who completed their education after 12 years as compared with those with only 8 years of education; however, it is not clear whether these improvements were in all three WOMAC subscales [24]. Similar to what we report, Fortin et al. [8] found that greater education attainment was associated with lower pain and better function 6 months after arthroplasty independent of preoperative pain or functional status. Conversely, Keurentjes et al. [16] found no association with THA outcomes and education. However, their study population was small with a long followup interval bringing into question whether statistical associations were reliable.
The severity of physical OA symptoms is more associated with patients with low education, who currently have a greater unmet need for arthroplasty [4, 10]. Their willingness to undergo surgery however is equal to their more educated peers; therefore, patient willingness does not account for the treatment discrepancy [11]. The disparity between patients with OA with low socioeconomic status and access to total joint surgery exists even in countries with equal access to health care [5, 6, 11]. Although these individuals are at risk for lower patient-reported outcomes than more educated patients, they still have marked improvements and benefit from the treatment.
The strength of this investigation stems from the 96% nationwide completeness of procedures in the Swedish Hip Arthroplasty Register and the increase to 92% of hospitals participating in the patient-reported outcome measure program by 2007 [14]. Also enhancing this work was the ability to merge THA data with demographic and socioeconomic variables allowing rigorous statistical analysis of the association of patient factors with patient-reported outcomes 1 year after THA. Our results suggest clinicians should support patients with low and medium education to a greater extent. Identification of these patients is easy, inexpensive, and does not require special diagnostic tests. They may require more information or additional explanation to guide their postoperative expectations. The goal of elective THA is to eliminate pain, return the patient to full (or close to full) function, and in turn, improve HRQoL. Identification or confirmation of new and existing factors associated with patient-reported outcomes is an important step in improving care with THA. Referring clinicians and surgeons need to educate patients about their risks and set realistic expectations for outcomes after THA. Because no one patient factor will explain all of the changes seen after surgery, it is critical for studies like this to identify as many influential patient factors as possible, even if the influence of each factor considered in isolation is small, as was the case for some end points we studied. Identification of patients who will benefit most from THA and providing additional information to patients at risk for poorer outcomes, like those with low and medium education attainment, ultimately may improve patient satisfaction HRQoL, pain, and the cost utility of THA.
Electronic supplementary material
Acknowledgments
We thank Thomas Eisler MD, for help in initiating this important work investigating the influence of socioeconomic status on patient-reported outcomes and for his role in obtaining local ethical approval.
Footnotes
This study was funded by the Swedish Hip Arthroplasty Register, Gothenburg, Sweden (GG), the Harris Orthopaedic Laboratory, Boston, MA, USA (HM), and research grants from Dr Felix Neuberghs Foundation, Gothenburg, Sweden (OR).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Data from this project were provided from the Swedish Hip Arthroplasty Register in Gothenburg, Sweden, and the data analyses took place in Gothenburg, Sweden, and Boston, MA, USA.
References
- 1.Anakwe RE, Jenkins PJ, Moran M. Predicting dissatisfaction after total hip arthroplasty: a study of 850 patients. J Arthroplasty. 2011;26:209–213. doi: 10.1016/j.arth.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Bischoff-Ferrari HA, Lingard EA, Losina E, Baron JA, Roos EM, Phillips CB, Mahomed NN, Barrett J, Katz JN. Psychosocial and geriatric correlates of functional status after total hip replacement. Arthritis Rheum. 2004;51:829–835. doi: 10.1002/art.20691. [DOI] [PubMed] [Google Scholar]
- 3.Callaghan JJ, Dysart SH, Savory CF, Hopkinson WJ. Assessing the results of hip replacement: a comparison of five different rating systems. J Bone Joint Surg Br. 1990;72:1008–1009. doi: 10.1302/0301-620X.72B6.2246281. [DOI] [PubMed] [Google Scholar]
- 4.Cleveland RJ, Schwartz TA, Prizer LP, Randolph R, Schoster B, Renner JB, Jordan JM, Callahan LF. Associations of educational attainment, occupation and community poverty with hip osteoarthritis. Arthritis Care Res (Hoboken). 2013;65:954–961. doi: 10.1002/acr.21920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dixon T, Shaw M, Ebrahim S, Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63:825–830. doi: 10.1136/ard.2003.012724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dixon T, Urquhart DM, Berry P, Bhatia K, Wang Y, Graves S, Cicuttini FM. Variation in rates of hip and knee joint replacement in Australia based on socio-economic status, geographical locality, birthplace and indigenous status. ANZ J Surg. 2011;81:26–31. doi: 10.1111/j.1445-2197.2010.05485.x. [DOI] [PubMed] [Google Scholar]
- 7.EuroQolGroup. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. [DOI] [PubMed]
- 8.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, Phillips C, Partridge AJ, Belisle P, Fossel AH, Mahomed N, Sledge CB, Katz JN. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–1728. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 9.Genell A, Nemes S, Steineck G, Dickman PW. Model selection in medical research: a simulation study comparing Bayesian model averaging and stepwise regression. BMC Med Res Methodol. 2010;10:108. doi: 10.1186/1471-2288-10-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hannan MT, Anderson JJ, Pincus T, Felson DT. Educational attainment and osteoarthritis: differential associations with radiographic changes and symptom reporting. J Clin Epidemiol. 1992;45:139–147. doi: 10.1016/0895-4356(92)90006-9. [DOI] [PubMed] [Google Scholar]
- 11.Hawker GA, Wright JG, Glazier RH, Coyte PC, Harvey B, Williams JI, Badley EM. The effect of education and income on need and willingness to undergo total joint arthroplasty. Arthritis Rheum. 2002;46:3331–3339. doi: 10.1002/art.10682. [DOI] [PubMed] [Google Scholar]
- 12.Hoeting JA, Madigan D, Raftery AE, Volinsky CT. Bayesian model averaging: a utorial. Statistical Science. 1999;14:382–417. doi: 10.1214/ss/1009212519. [DOI] [Google Scholar]
- 13.Juhakoski R, Malmivaara A, Lakka TA, Tenhonen S, Hannila ML, Arokoski JP. Determinants of pain and functioning in hip osteoarthritis: a two-year prospective study. Clin Rehabil. 2013;27:281–287. doi: 10.1177/0269215512453060. [DOI] [PubMed] [Google Scholar]
- 14.Karrholm J, Garellick G, Rogmark C, Herberts P. Swedish Hip Arthroplasty Register: Annual Report 2007. Gothenburg, Sweden: Swedish Hip Arthroplasty Register; 2008. [Google Scholar]
- 15.Kass RE, Raftery AE. Bayes factors. J Am Statist Assoc. 1995;90:773–795. doi: 10.1080/01621459.1995.10476572. [DOI] [Google Scholar]
- 16.Keurentjes JC, Blane D, Bartley M, Keurentjes JJ, Fiocco M, Nelissen RG. Socio-economic position has no effect on improvement in health-related quality of life and patient satisfaction in total hip and knee replacement: a cohort study. PLoS One. 2013;8:e56785. doi: 10.1371/journal.pone.0056785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King MT. A point of minimal important difference (MID): a critique of terminology and methods. Expert Rev Pharmacoecon Outcomes Res. 2011;11:171–184. doi: 10.1586/erp.11.9. [DOI] [PubMed] [Google Scholar]
- 18.Leigh JP, Fries JF. Occupation, income, and education as independent covariates of arthritis in four national probability samples. Arthritis Rheum. 1991;34:984–995. doi: 10.1002/art.1780340808. [DOI] [PubMed] [Google Scholar]
- 19.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. Available at: http://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006. Accessed January 16, 2014.
- 20.Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111–163. doi: 10.2307/271063. [DOI] [Google Scholar]
- 21.Rolfson O, Dahlberg LE, Nilsson JA, Malchau H, Garellick G. Variables determining outcome in total hip replacement surgery. J Bone Joint Surg Br. 2009;91:157–161. doi: 10.1302/0301-620X.91B2.20765. [DOI] [PubMed] [Google Scholar]
- 22.Rolfson O, Karrholm J, Dahlberg LE, Garellick G. Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J Bone Joint Surg Br. 2011;93:867–875. doi: 10.1302/0301-620X.93B7.25737. [DOI] [PubMed] [Google Scholar]
- 23.Ross CE, Wu C-L. The links between education and health. Am Sociol Rev. 1995;60:719–745. doi: 10.2307/2096319. [DOI] [Google Scholar]
- 24.Schafer T, Krummenauer F, Mettelsiefen J, Kirschner S, Gunther KP. Social, educational, and occupational predictors of total hip replacement outcome. Osteoarthritis Cartilage. 2010;18:1036–1042. doi: 10.1016/j.joca.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Singh JA, Lewallen D. Age, gender, obesity, and depression are associated with patient-related pain and function outcome after revision total hip arthroplasty. Clin Rheumatol. 2009;28:1419–1430. doi: 10.1007/s10067-009-1267-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevens M, Wagenmakers R, Groothoff JW, Bulstra SK, van den Akker-Scheek I, Zijlstra W. Physical activity behavior after total hip arthroplasty (THA): a prediction based on patient characteristics. Patient Educ Couns. 2007;69:196–199. doi: 10.1016/j.pec.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 27.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14:1523–1532. doi: 10.1007/s11136-004-7713-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.