Abstract
Background
Lumbar degenerative scoliosis is a common condition in the elderly. Open traditional surgical approaches are associated with high-morbidity complication rates. Less invasive options may carry fewer risks in this patient population. A minimally disruptive lateral transpsoas retroperitoneal technique to accomplish interbody fusion was developed to avoid the morbidity of traditional open surgery, but this approach as an anterior stand-alone construction has not been reported yet for the treatment of adult degenerative scoliosis.
Questions/purposes
We determined (1) the clinical outcomes (VAS scores for back and leg, Oswestry Disability Index), (2) the radiographic outcomes (Cobb angle, lumbar lordosis, sacral slope, high-grade subsidence, osseous fusion), and (3) the reoperation and complication rates in an older population undergoing this surgical approach.
Methods
Between 2004 and 2008, 62 patients were treated surgically for adult degenerative scoliosis, of whom 46 (74%) were treated with stand-alone lateral lumbar interbody fusion; 11 of these (24%) were lost to followup before 24 months, leaving the records of 35 patients (nine men, 26 women; mean ± SD age, 68 ± 10 years) available for this retrospective review. General indications for this approach included neurogenic claudication and radicular symptoms with history of chronic low-back pain. A total of 107 levels were treated (mean, three; range, one to seven). Clinical and radiographic outcomes were assessed at a followup of 24 months.
Results
Mean VAS back pain scores improved from 85 mm preoperatively to 27 mm at latest followup (p < 0.001). VAS leg pain scores improved from 91 mm to 24 mm (p < 0.001). Oswestry Disability Index scores improved from 51 to 29 (p < 0.001). Coronal alignment improved from Cobb angles of 21° to 12° (p < 0.001). Lumbar lordosis improved from 33° to 41° (p < 0.001). Sacral slope was enhanced from 28° to 35° (p < 0.001). Fusion rate was 84% at final evaluation. High-grade subsidence was seen in 10 patients (29%). Three patients (9%) needed further surgical intervention.
Conclusions
Use of the lateral approach achieved reasonable coronal and sagittal correction, as well as improvements in pain and function, in mild scoliotic deformities; however, subsidence was a concern, occurring in 29% of patients. Questions still remain regarding the need for additional supplementation or the use of wider cages to prevent subsidence.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Lumbar degenerative scoliosis is a common condition of the lumbar spine and its incidence is increasing as the aging population grows. Most patients with this condition are treated nonoperatively [9, 37], but when this treatment fails, surgery may be considered, mostly to achieve spinal canal decompression. Several surgical options are available depending on the patient’s symptoms and severity of the deformity. Several options are described in the literature, including decompression alone, decompression and instrumented arthrodesis, and posterior and circumferential fusion with the use of interbody fusion via an anterior, posterior, or lateral approach [5].
In large curves, structural anterior column support provides several benefits, including improved stability, decreased stress on screws, higher fusion rates, and better lumbar lordosis [16, 17, 26, 30, 31, 39]. Nevertheless, instrumented arthrodesis procedures are not free of complications, and considering all the comorbidities associated with an older population, surgical treatment of degenerative scoliosis should be carefully studied to avoid them. Transfeldt et al. [36] has shown that complications occur more frequently in larger and more complex procedures, such as long fusions (sacrum to curve apex). Overall major complication rates for these procedures, including neurologic deficit, infection, thromboembolism, and death, can exceed 30% [11, 36].
In recent years, a minimally disruptive lateral transpsoas retroperitoneal technique to accomplish interbody fusion has been developed as an alternative approach to avoid the morbidity of traditional open surgery [2, 29]; proof-of-concept has been established even in elderly and obese patients [32, 33]. This approach, also called lateral lumbar interbody fusion, is mostly utilized with posterior supplementation but can be used as a stand-alone anterior construction since it preserves the anterior longitudinal ligament [24], avoiding disruption of posterior stabilizing structures, permitting insertion of a large interbody graft, and restoring foraminal height with a larger surface area for arthrodesis [23, 24, 27]. A few articles reporting small case series of scoliosis treated with lateral lumbar interbody fusion have been published [3, 10, 18, 25], including a literature review [4], but none of them in a cohort consisting of only stand-alone cases for degenerative scoliosis only.
We therefore determined (1) the clinical outcomes (VAS scores for back and leg, Oswestry Disability Index [ODI]), (2) the radiographic outcomes (Cobb angle, correction of lumbar lordosis, sacral slope, frequency of high-grade subsidence and osseous fusion), and (3) the reoperation and complications rates in a group of patients with adult degenerative scoliosis undergoing lateral lumbar interbody fusion.
Patients and Methods
Study Cohort
This was a retrospective, institutional review board-approved study. Inclusion criteria were age greater than 65 years at time of surgery, adult degenerative scoliosis with radicular or central compromise with or without back pain, preoperative coronal Cobb angle of at least 10°, failed extensive nonoperative therapy, surgical treatment with stand-alone lateral lumbar interbody fusion, and at least 2 years of followup. Exclusion criteria were posterior instrumentation, prior lumbar fusion surgery, and other comorbidities, such as neoplasia, trauma, infection, or spondylolisthesis of greater than Grade II.
In a private spine center, between 2004 and 2008, 62 patients were treated surgically for adult degenerative scoliosis, of whom 46 (74%) were treated with lateral lumbar interbody fusion using a stand-alone anterior construction by a single senior spine surgeon (LP); 11 of these (24%) were lost to followup before 24 months, leaving the records of 35 patients (nine men, 26 women; mean ± SD age, 68 ± 10 years; range, 65–87 years) available for review (Table 1). Mean followup was 24 months. All eligible patients gave informed consent to participate in the study.
Table 1.
Demographic data
| Variable | Value |
|---|---|
| Number of patients | 35 |
| Number of levels | 107 |
| Number of levels per case* | 3.15 (1–7) |
| Age (years)† | 68.2 ± 9.8 |
| Sex (number of female patients) | 26 (74%) |
| BMI (m/kg2) | 26.4 ± 4.6 |
* Values are expressed as mean, with range in parentheses; †values are expressed as mean ± SD.
Surgery Indications and Techniques
The primary indication for surgical treatment was neurogenic claudication in patients with degenerative scoliosis with lumbar stenosis and no response to nonoperative treatment for at least 6 months before surgery. Typical symptoms were lumbar and/or leg pain in standing and walking. Relative indications proposed for surgery included curve progression, sagittal and/or coronal imbalance with unremitting back pain, documented history of progressive curve, radiculopathy on the side of the concavity of the curve (as a result of pedicle-on-pedicle stenosis), and loss of lumbar lordosis in patients with a history of flat-back syndrome or back pain. Contraindications to indirect decompression by the stand-alone lateral lumbar interbody fusion procedure were severe facet hypertrophy, significant facet joint space widening, congenital small pedicles, severe osteoporosis, and/or indication of L5-S1 arthrodesis.
The patients underwent lateral lumbar interbody fusion using an 18-mm (AP dimension) polyetheretherketone (PEEK) cage (CoRoent®; NuVasive, Inc, San Diego, CA, USA) at the spine level that presented central and/or lateral stenosis (commonly concomitant with spondylolisthesis, laterolisthesis, and/or rotator subluxation). Levels at the apex were also accessed. Intraoperatively neuromonitoring was performed with real-time, automated, dynamically stimulated EMG guidance with discrete threshold identification (NeuroVision®; NuVasive, Inc). In degenerative scoliosis, the side selected for access to the disc space was the concave side of the scoliotic curve, dictated by the ease of access and coronal and rotational corrections achieved. Careful attention was paid to releasing the disc and annulus all the way to the opposite side to get maximal coronal correction at the index segment. After appropriate endplate preparation, PEEK spacers augmented with synthetic bone graft were inserted. One milliliter of corticoid was used on top of the lumbar plexus to minimize the consequences of neural distraction. After insertion, the incision was closed in a standard fashion. Patients were encouraged to ambulate as soon as they could, and bracing was not routinely prescribed.
A total of 107 levels were treated (mean, three; range, one to seven). The most common apical disc level was L3 (66%), followed by L2 (27%). Surgeries were performed in a mean of 137 minutes (range, 80–240 minutes), with a mean estimated blood loss of 54 mL. The mean hospital stay was 34 hours (range, 24–96 hours).
Data Collection
We collected demographic and intraoperative data and data from physical examination, neurologic assessment, and clinical and radiographic evaluations, which were performed preoperatively as part of a prospectively maintained database, and during the followup visits at 1 and 6 weeks and 3, 6, 12, and 24 months. Operative data collection included operative time, estimated blood loss, length of hospital stay, level(s) treated, complications, and adverse events.
Clinical evaluations were obtained through self-assessed questionnaires including a 100-mm VAS for back and leg pain and the ODI for function assessment. Postoperative neurologic status was recorded evaluating psoas muscle and sensitivity on the side of the approach.
The radiographic analysis consisted of Cobb angle measurements, lumbar lordosis (L1-S1), sacral slope, subsidence, and fusion. Coronal alignment was measured by means of the Cobb angle. Sagittal alignment was measured by means of global lordosis and sacral slope. Subsidence was classified as described previously [22, 23] in radiographs in the AP and lateral views and CT scans, based on the amount of cage subsidence into the vertebral endplates: absent or low-grade = 0% to 49%; and high-grade = 50% to 100% collapse of the level. Fusion status was determined oriented as described previously [6, 14, 15] in plain neutral and flexion-extension radiographs and eventually CT scans in cases with no clear conclusion on the radiographs. Fusion was defined as bridging bone connecting the adjacent vertebral bodies either through the implants or around the implants, less than 5° of angular motion, 3 mm or less of translation, and absence of radiolucent lines around more than 50% of either of the implant surfaces.
Physical evaluations and recording of complications were performed by the operating spine surgeon. Other clinical data and outcomes were recorded independently of the operating spine surgeon. Radiographic evaluations were performed by a surgeon committee of three observers. Intra- and interobserver variability was not assessed.
Statistical Analysis
Statistical analyses were performed using SPSS® software (Version 10; SPSS Inc, Chicago, IL, USA). A one-tailed paired t-test was used for comparison between variables, with p values of less than 0.05 considered significant.
Results
Clinical Outcomes
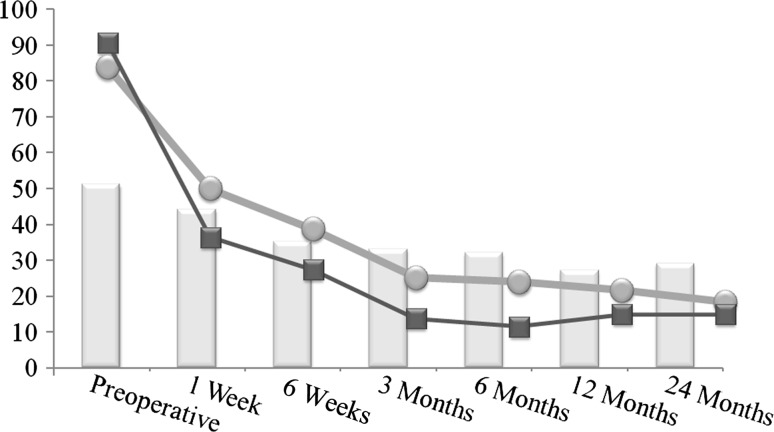
Clinical results obtained through self-assessed questionnaires improved at the postoperative visits (Fig. 1). Low-back pain as assessed by VAS score showed a 30% improvement (p < 0.001) at the first postoperative visit and 43% improvement (p < 0.001) at final followup compared to preoperatively. Resolution of pain caused by stenosis was assessed by VAS of the lower extremity. The mean baseline VAS score for leg pain was 91 mm and decreased 57% (p < 0.001) soon after surgery (1-week visit) and remained low at final followup, with 74% of symptom resolution (p < 0.001). ODI scores decreased and remained lower than the preoperative baseline at latest followup, with a 56% improvement observed (p < 0.001).
Fig. 1.
A graph shows mean scores for the ODI (bars), VAS back pain (light gray lines and dots), and VAS leg pain (dark gray lines and dots). Postoperative ODI values since the 6-week visit are significantly lower compared to baseline (p < 0.04). All postoperative VAS scores are significantly lower compared to baseline (p < 0.01).
Radiographic Outcomes
The mean Cobb angle decreased (p < 0.001) from a preoperative value of 21° to 12° at latest followup. The mean lumbar lordosis significantly increased (p < 0.001) from a preoperative value of 32° (SD, 7°) to 41° (SD, 6°) at final followup, while mean sacral slope increased (p < 0.001) from 28° to 35° (Table 2). An example of the coronal alignment achieved by the lateral approach in a standard construction is shown (Fig. 2), while another example shows the sagittal alignment after the procedure, with evidence of enhancement in lumbar lordosis and sacral slope (Fig. 3). Bone ingrowth and fusion were confirmed in 90 of the 107 levels at 24-month evaluation (Fig. 4).
Table 2.
Spinopelvic parameters
| Parameter | Preoperative | 2 years | p value |
|---|---|---|---|
| Lumbar lordosis (°)* | 32.6 (10.8) | 41.46 (11.3) | < 0.001 |
| Sacral slope (°)* | 27.6 (8.4) | 35.4 (8.7) | < 0.001 |
| Cobb angle (°)* | 21.3 (6.7) | 11.5 (4.7) | < 0.001 |
| Bone fusion (number of levels) | 90/107 (84%) |
* Values are expressed as mean, with SD in parentheses.
Fig. 2A–B.
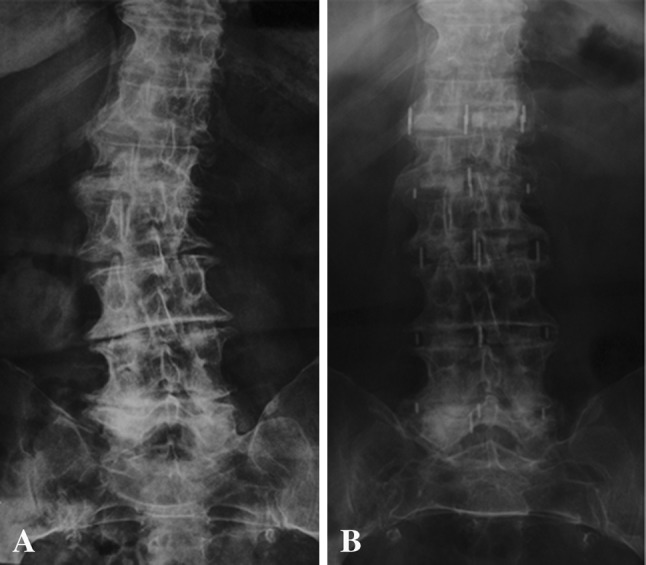
(A) Preoperative and (B) 24-month AP radiographs demonstrate coronal correction after stand-alone lateral lumbar interbody fusion. Note the rotational and curve correction without the need for pedicle screws.
Fig. 3A–B.

(A) Preoperative and (B) 24-month lateral radiographs demonstrate sagittal correction after stand-alone lateral lumbar interbody fusion. Note that, by positioning the cages anteriorly in the disc space, it is possible to increase lordosis, while a posterior positioning of the cage generates a prokyphotic construction.
Fig. 4A–G.
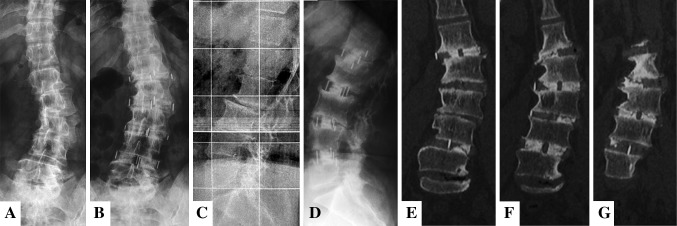
(A) Preoperative and (B) 24-month AP radiographs; (C) preoperative and (D) 24-month lateral radiographs; and (E–G) 24-month coronal CT reconstructions demonstrate sagittal and coronal correction and interbody fusion in (E) L1-L2, (F) L2-L3 and L4-L5, and (G) L3-L4. Note also laterolisthesis correction and vertebral derotation.
Reoperations and Complications
Intraoperative complications included three instances of anterior longitudinal ligament rupture, which resulted in a more anterior placement of the device. Ten patients (29%) experienced cage subsidence by 6-week followup and no progression was seen up to 3-month evaluation. After the subsidence, patients experienced a sudden increase in low-back pain, some with just discomfort and others with more significant symptoms (persisting some months). In two (6%) of them, radiculopathy arose, requiring a foraminotomy and pedicle screw supplementation 12 months after surgery. One patient (3%) with subsidence had persistent back pain due to cage micromotion and was reoperated on with pedicle screw supplementation. No long-lasting (more than 6 months) neural deficits related to the lumbar plexus were recorded.
Discussion
Spine surgery for the elderly population is increasing as the population ages. Thus, as incidence of medical comorbidities increases, so does that of spinal deformity [9, 12, 13, 35]. Morbidity reduction in adult scoliosis surgical treatment is an end point that may be achieved with less invasive techniques. The extreme lateral interbody fusion technique has become an increasingly popular approach for achieving interbody fusion, and promising results have been reported. Stand-alone interbody construction comprises a less disruptive lateral-only procedure and has also been used by some surgeons, and it may also be beneficial in the treatment of elderly patients. A few articles reporting small case series of scoliosis treated with lateral lumbar interbody fusion have been published [10, 18, 25], but none of them in a cohort consisting of only stand-alone cases for degenerative scoliosis only. We therefore determined (1) the clinical outcomes (VAS scores for back and leg, ODI), (2) the radiographic outcomes (Cobb angle, correction of lumbar lordosis, sacral slope, frequency of high-grade subsidence and osseous fusion), and (3) the reoperation and complications rates in a group of patients with adult degenerative scoliosis undergoing lateral lumbar interbody fusion.
This study had a number of limitations. First, it is a retrospective study, which raises a concern about selection bias and loss to followup, although this was somewhat mitigated by the use of consistent selection criteria during the study period. Second, full-length radiographs were not available to address global coronal or sagittal alignment; therefore, we could only analyze local deformity correction, and reciprocal changes are yet to be determined after this surgical approach. Third, to minimize patients’ exposure to radiation, not all patients had CT scans, only those whose fusion status was not possible to determine on radiographs. Moreover, plain films have shown strong evidence of fusion or pseudarthrosis; thus, helical CT is unlikely to provide useful new information [6, 14, 15]. Fourth, radiographic assessment was not performed by multiple observers so it was not possible to test interobserver agreement; rather, it was performed by experienced examiners in a unique committee as frequently performed in reports of other small case series. Fifth, our study was neither a large case series nor a comparative study, and some analyses were not possible (for example, analysis of the subset of patients with subsidence); nevertheless, our study is the largest case series of stand-alone treatment of degenerative scoliosis at the time of this report. Sixth, subsidence was evaluated only up to 3 months and some authors claim that later evaluation may give different results; however, our subsidence evaluation was based on a study [22] suggesting that 3-month subsidence has no significant progression with lateral placed cages. Finally, we did not report side effects related to the psoas entry and the lumbar plexus in detail because at the time of data collection we did not have a standardized method to record this variable such as that published by Le et al. [21]; nevertheless, we observed no permanent deficit 6 months after surgery.
The clinical outcomes evaluated at 24 months in this series showed improvements in VAS and ODI scores. VAS leg pain is not the most suitable criterion to assess the treatment of stenosis and all its related symptoms but is an indirect measure of claudication, when patients experience pain and/or extreme discomfort during walking. Dakwar et al. [10] operated on 25 patients with adult scoliosis using the lateral approach along with pedicle screws. They found improved preoperative symptoms, with 70.4% decrease in VAS score, 44% decrease in ODI, and solid fusion in 100% of patients. Anand et al. [3] found 57% reduction in VAS and 82% reduction in ODI at an average of 22 months after surgery in adult degenerative scoliosis treated with the lateral approach along with posterior instrumentation. The data suggest that indirect neural decompression can be achieved in select patients using lateral interbody fusion with disc space distraction and stabilization of the involved motion segment, both in instrumented and stand-alone lateral interbody constructions.
Radiographic results showed good overall correction in this case series. The lateral access provides a route to perform ipsilateral/contralateral annulus release and wide discectomy and allows a large graft to enter into the interbody space and distraction of the adjacent vertebrae symmetrically. Sharma et al. [34] found, in a retrospective review of 43 consecutive patients with adult scoliosis treated using the lateral approach, a mean correction of 3.7° (p ≤ 0.001) at each accessed level in the coronal plane, in a total of 87 instrumented levels. Similarly, there was a mean gain of 2.8° (p ≤ 0.001) of lordosis at each level. Anand et al. [3] found a mean preoperative Cobb angle of 22° was corrected to 7° (68% reduction), while Wang and Mummaneni [38] found a 63% reduction. We found similar results. The spinopelvic parameters were analyzed postoperatively, and difficulty in obtaining lateral radiographs that included the femur head prevented us from having all the needed information; thus, we measured only the sacral slope and lumbar lordosis as predictors of sagittal balance. Acosta et al. [1] found an increase in lumbar lordosis of only 9%, while we found a 27% gain in global lordosis. This may be explained by a more anterior positioning of the cages in our series, which is an important determinant factor of postoperative alignment and increment of lumbar lordosis [19].
The frequency of complications was almost restricted to the onset of cage subsidence. The incidence of reoperations as a consequence of surgical complications tends to increase with complexity of the surgical procedures. Carreon et al. [8] studied short-term complications in elderly patients with degenerative disease (spinal stenosis, spondylolisthesis, and/or scoliosis) treated with decompression and instrumentation. The study revealed an incidence of 21% of at least one major complication, 70% of at least one minor complication, 50% of more than one complication, and 2% of deaths. Isaacs et al. [19] stratified their case series into patients undergoing extreme lateral interbody fusion as a stand-alone procedure or with percutaneous instrumentation and patients undergoing the procedure with posterior instrumentation. The results pointed to a higher major complication rate in patients undergoing the procedure with posterior instrumentation (20.7% versus 9%); nevertheless, the authors concluded that the overall adverse events compared favorably to those cited in other case series of degenerative deformity. In the lateral access literature for the treatment of degenerative scoliosis, the most commonly observed complications are hip flexor weakness, anterior thigh pain, and numbness [4]. Although these clinical presentations can intimidate unaware surgeons and patients, they have been consistently reported to be transient conditions, with resolution in 6 weeks. It should be noted that none of our patients required immediate reoperation. It was necessary to reoperate on four of our patients (at 2-year followup) due to persistent back pain either because of incomplete decompression or loosening of the achieved decompression as a consequence of cage subsidence. No infections were observed. In our series, major medical complications were not seen and none of patients needed postoperative intensive care, being transferred to regular hospital rooms within an hour after surgery.
In some patients with high-grade facet joint arthrosis, decompression is not completely feasible because the facet joint is not able to slide and allow the opening of the foramen [28]. Loosening of the disc due to significant subsidence is another reason for insufficient decompression and reoperation [20] and was found in our study. In addition, osteoporosis may be a significant contributor to deformity and degenerative scoliosis. This may be a limitation in the treatment of patients older than 65 years for lumbar degenerative scoliosis because of an increased incidence of subsidence in this population. To biomechanically evaluate stand-alone extreme lateral interbody fusion, Cappuccino et al. [7] showed that using a larger cage generates the largest stand-alone reduction in ROM compared with literature-reported anterior and transforaminal lumbar interbody fusion constructs, diminishing the incidence of subsidence, but in some cases, it is not sufficient to prevent subsidence [23]. It has been shown that the incidence of subsidence can be reduced using wider cages, with better clinical and radiographic results [23]. In the present series, only cases with 18-mm cages were analyzed, which may justify our subsidence rate.
In conclusion, using the lateral approach, we were able to treat mild adult lumbar scoliosis in a less invasive way; the goals were reduction in pain after surgery and correction of deformity, without the risks and morbidity associated with larger approaches. We found satisfactory coronal and sagittal correction, as well as clinical improvements in pain and function; however, the frequency of clinically important subsidence was a concern. Questions still remain regarding additional posterior screw supplementation or the use of wider cages to prevent subsidence in the treatment of adult degenerative scoliosis. Stand-alone lateral lumbar interbody fusion can be applied as a less complex surgery to treat degenerative scoliosis, but for some cases, a staged approach for supplementation may be required.
Acknowledgments
The authors thank Thabata Bueno MS for her assistance with paper review.
Footnotes
One of the authors certifies that he (LP), or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of USD (USD 100,001 to USD 1,000,000), from NuVasive, Inc, CA, USA.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Instituto de Patologia da Coluna, São Paulo, Brazil.
References
- 1.Acosta FL, Liu J, Slimack N, Moller D, Fessler R, Koski T. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine. 2011;15:92–96. doi: 10.3171/2011.3.SPINE10425. [DOI] [PubMed] [Google Scholar]
- 2.Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech. 2008;21:459–467. doi: 10.1097/BSD.0b013e318167b06b. [DOI] [PubMed] [Google Scholar]
- 3.Anand N, Rosemann R, Khalsa B, Baron EM. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 2010;28:E6. doi: 10.3171/2010.1.FOCUS09272. [DOI] [PubMed] [Google Scholar]
- 4.Arnold PM, Anderson KK, McGuire RA., Jr The lateral transpsoas approach to the lumbar and thoracic spine: a review. Surg Neurol Int. 2012;3:S198–S215. doi: 10.4103/2152-7806.98583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bridwell KH. Selection of instrumentation and fusion levels for scoliosis: where to start and where to stop. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:1–8. doi: 10.3171/spi.2004.1.1.0001. [DOI] [PubMed] [Google Scholar]
- 6.Burkus JK, Foley K, Haid RW, LeHuec JC. Surgical Interbody Research Group—radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus. 2001;10:E11. doi: 10.3171/foc.2001.10.4.12. [DOI] [PubMed] [Google Scholar]
- 7.Cappuccino A, Cornwall GB, Turner AW, Fogel GR, Duong HT, Kim KD, Brodke DS. Biomechanical analysis and review of lateral lumbar fusion constructs. Spine (Phila Pa 1976). 2010;35(26 suppl):S361–S367. [DOI] [PubMed]
- 8.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop (Belle Mead NJ). 2003;32:77–82. [PubMed] [Google Scholar]
- 10.Dakwar E, Cardona RF, Smith DA, Uribe JS. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010;28:E8. doi: 10.3171/2010.1.FOCUS09282. [DOI] [PubMed] [Google Scholar]
- 11.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007;32:2238–2244. [DOI] [PubMed]
- 12.Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine: the influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 13.Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–146. doi: 10.1097/01.blo.0000198726.62514.75. [DOI] [PubMed] [Google Scholar]
- 14.Fogel GR, Toohey JS, Neidre A, Brantigan JW. Fusion assessment of posterior lumbar interbody fusion using radiolucent cages: x-ray films and helical computed tomography scans compared with surgical exploration of fusion. Spine J. 2008;8:570–577. doi: 10.1016/j.spinee.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein C, Drew B. When is a spine fused? Injury. 2011;42:306–313. doi: 10.1016/j.injury.2010.11.041. [DOI] [PubMed] [Google Scholar]
- 16.Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J. 2005;14:551–558. doi: 10.1007/s00586-004-0830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007;7:379–386. doi: 10.3171/SPI-07/10/379. [DOI] [PubMed] [Google Scholar]
- 18.Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM. A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976). 2010;35(26 suppl):S322–S330. [DOI] [PubMed]
- 19.Kepler CK, Huang RC, Sharma AK, Meredith DS, Metitiri O, Sama AA, Girardi FP, Cammisa FP. Factors influencing segmental lumbar lordosis after lateral transpsoas interbody fusion. Orthop Surg. 2012;4:71–75. doi: 10.1111/j.1757-7861.2012.00175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le TV, Baaj AA, Dakwar E, Burkett CJ, Murray G, Smith DA, Uribe JS. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine(Phila Pa 1976). 2012;37:1268–1273. [DOI] [PubMed]
- 21.Le TV, Burkett CJ, Deukmedjian AR, Uribe JS. Postoperative lumbar plexus injury following lumbar retroperitoneal transpsoas minimally invasive lateral interbody fusion. Spine (Phila Pa 1976). 2013;38:E13–E20. [DOI] [PubMed]
- 22.Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013;19:110–118. doi: 10.3171/2013.4.SPINE12319. [DOI] [PubMed] [Google Scholar]
- 23.Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. ScienceWorldJournal. 2012;2012:456346. doi: 10.1100/2012/456346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marchi L, Oliveira L, Coutinho E, Pimenta L. The importance of the anterior longitudinal ligament in lumbar disc arthroplasty: 36-month follow-up experience in extreme lateral total disc replacement. Int J Spine Surg. 2012;6:18–23. doi: 10.1016/j.ijsp.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mundis GM, Akbarnia BA, Phillips FM. Adult deformity correction through minimally invasive lateral approach techniques. Spine (Phila Pa 1976). 2010;35(26 suppl):S312–S321. [DOI] [PubMed]
- 26.Niemeyer TK, Koriller M, Claes L, Kettler A, Werner K, Wilke HJ. In vitro study of biomechanical behavior of anterior and transforaminal lumbar interbody instrumentation techniques. Neurosurgery. 2006;59:1271–1276. doi: 10.1227/01.NEU.0000245609.01732.E4. [DOI] [PubMed] [Google Scholar]
- 27.Oliveira L, Marchi L, Coutinho E, Abdala N, Pimenta L. The use of rh-BMP2 in standalone eXtreme Lateral Interbody Fusion (XLIF®): clinical and radiological results after 24 months follow-up. World Spinal Column J. 2010;1:19–25. [Google Scholar]
- 28.Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976). 2010;35(26 suppl):S331–S337. [DOI] [PubMed]
- 29.Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435–443. doi: 10.1016/j.spinee.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 30.Ploumis A, Wu C, Fischer G, Mehbod AA, Wu W, Faundez A, Transfeldt EE. Biomechanical comparison of anterior lumbar interbody fusion and transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2008;21:120–125. doi: 10.1097/BSD.0b013e318060092f. [DOI] [PubMed] [Google Scholar]
- 31.Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW, Jr, Kuklo TR. Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech. 2005;18:337–346. doi: 10.1097/01.bsd.0000166642.69189.45. [DOI] [PubMed] [Google Scholar]
- 32.Rodgers WB, Cox CS, Gerber EJ. Early Complications of extreme lateral interbody fusion in the obese. J Spinal Disord Tech. 2010;23:393–397. doi: 10.1097/BSD.0b013e3181b31729. [DOI] [PubMed] [Google Scholar]
- 33.Rodgers WB, Gerber EJ, Rodgers JA. Lumbar fusion in octogenarians: the promise of minimally invasive surgery. Spine (Phila Pa 1976). 2010;35(26 suppl):S355–S360. [DOI] [PubMed]
- 34.Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 2011;24:242–250. doi: 10.1097/BSD.0b013e3181ecf995. [DOI] [PubMed] [Google Scholar]
- 35.Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28:E1. doi: 10.3171/2010.1.FOCUS09271. [DOI] [PubMed] [Google Scholar]
- 36.Transfeldt EE, Topp R, Mehbod AA, Winter RB. Surgical outcomes of decompression, decompression with limited fusion, and decompression with full curve fusion for degenerative scoliosis with radiculopathy. Spine (Phila Pa 1976). 2010;35:1872–1875. [DOI] [PubMed]
- 37.Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11:174–183. doi: 10.5435/00124635-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Wang MY, Mummaneni PV. Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus. 2010;28:1–8. doi: 10.3171/2010.1.FOCUS09286. [DOI] [PubMed] [Google Scholar]
- 39.Wu CH, Wong CB, Chen LH, Niu CC, Tsai TT, Chen WJ. Instrumented posterior lumbar interbody fusion for patients with degenerative lumbar scoliosis. J Spinal Disord Tech. 2008;21:310–315. doi: 10.1097/BSD.0b013e318148b256. [DOI] [PubMed] [Google Scholar]