Abstract
Background
There is an inherently difficult learning curve associated with minimally invasive surgical (MIS) approaches to spinal decompression and fusion. The association between complication rate and the learning curve remains unclear.
Questions/purposes
We performed a systematic review for articles that evaluated the learning curves of MIS procedures for the spine, defined as the change in frequency of complications and length of surgical time as case number increased, for five types of MIS for the spine.
Methods
We conducted a systematic review in the PubMed database using the terms “minimally invasive spine surgery AND complications AND learning curve” followed by a manual citation review of included manuscripts. Clinical outcome and learning curve metrics were categorized for analysis by surgical procedure (MIS lumbar decompression procedures, MIS transforaminal lumbar interbody fusion, percutaneous pedicle screw insertion, laparoscopic anterior lumbar interbody fusion, and MIS cervical procedures). As the most consistent parameters used to evaluate the learning curve were procedure time and complication rate as a function of chronologic case number, our analysis focused on these. The search strategy identified 15 original studies that included 966 minimally invasive procedures. Learning curve parameters were correlated to chronologic procedure number in 14 of these studies.
Results
The most common learning curve complication for decompressive procedures was durotomy. For fusion procedures, the most common complications were implant malposition, neural injury, and nonunion. The overall postoperative complication rate was 11% (109 of 966 cases). The learning curve was overcome for operative time and complications as a function of case numbers in 20 to 30 consecutive cases for most techniques discussed within this review.
Conclusions
The quantitative assessment of the procedural learning curve for MIS techniques for the spine remains challenging because the MIS techniques have different learning curves and because they have not been assessed in a consistent manner across studies. Complication rates may be underestimated by the studies we identified because surgeons tend to select patients carefully during the early learning curve period. The field of MIS would benefit from a standardization of study design and collected parameters in future learning curve investigations.
Introduction
The ability to treat conditions of the spine through minimally invasive surgical (MIS) techniques has garnered increased interest from spine surgeons and their patients over the past two decades [17]. MIS for the spine includes a wide variety of procedures designed to achieve decompression and stabilization of the cervical, thoracic, or lumbar spine while minimizing soft tissue damage. The principle of soft tissue preservation in MIS for the spine is largely accomplished by way of a carefully planned approach to the surgical target site. MIS fusion of the lumbar spine utilizes multiple paramedian incisions with tubular dilation to prevent crush injury or detachment of the stabilizing muscles of the spine. Important structures spared with this approach, as well as with lateral approaches to lumbar fusion, include the spinous process, the tendinous attachments of the multifidus muscle, and the supraspinous and interspinous ligaments [7, 9, 13]. Similarly, an anterior approach to MIS cervical decompression is utilized to prevent damage to the posterior cervical paraspinal musculature [5]. These techniques may result in less postoperative instability, less intraoperative blood loss, a shorter hospital stay, and a lower infection rate than traditional open procedures [5, 10, 14, 22]. Potential long-term benefits include less postoperative instability, which could lead to improved patient function.
A major challenge of MIS for the spine is the technical difficulty of working through a narrow surgical corridor with limited visualization of anatomic landmarks. A spine surgeon trained in traditional open methods must overcome a learning curve on the way to mastering MIS techniques for the spine [2, 9, 26, 28]. Specialized retraction systems, computer-assisted navigation technologies, and focused cadaveric training courses have been developed to decrease the MIS learning curve [28]. However, surgeons who adopt these techniques must be prepared for a higher complication rate and prolonged operative times during the initial experience with MIS procedures [20].
This systematic review evaluated the learning curves of MIS procedures for the spine, defined as the change in frequency of complications and length of surgical time as case number increased, for five types of MIS for the spine.
Search Strategy and Criteria
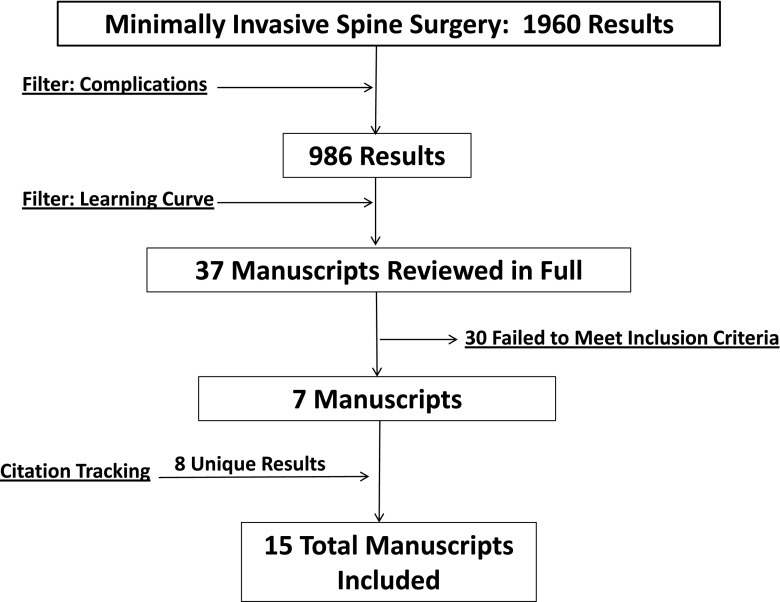
We used the Cochrane methodology [4] to perform a systematic review of PubMed for the learning curve of five categories of MIS procedures for the spine: MIS lumbar decompression procedures, MIS transforaminal lumbar interbody fusion (TLIF), percutaneous pedicle screw insertion, laparoscopic anterior lumbar interbody fusion (ALIF), and MIS cervical procedures. We used three successive searches: “minimally invasive spine surgery” (1960 results), “AND complications” (reduced to 986 articles), “AND learning curve” (reduced to 37 articles) (Fig. 1).
Fig. 1.
A flow diagram illustrates the search and selection process.
All manuscripts returned from this search strategy were reviewed in full for inclusion. Additionally, a manual review of the citation sections within included articles was performed. All case reports, case series, and clinical learning curve studies that pertained to decompression or fusion procedures of the cervical, thoracic, or lumbar spine were included. Studies that focused on revision procedures, corpectomy, or treatment of traumatic fracture or malignancy were excluded. The search strategy identified 37 total manuscripts that were reviewed in full. Twenty of these articles were excluded for not discussing complications during the learning curve period. An additional eight publications were excluded because they focused on treatment for fracture, malignancy, revision surgery, corpectomy, or cervical disc replacement. Two articles were excluded for only presenting cadaveric data. Manual review of the reference sections of included studies yielded eight additional publications that met inclusion criteria and were included in this review. Thus, a total of 15 articles were included in our systematic review, none of which were case reports [1, 3, 6, 8, 11, 12, 15, 16, 18, 19, 21, 23–25, 27] (Table 1).
Table 1.
Characteristics of included studies
| Study | Intervention | Study design | Sample size | Level of evidence | Learning curve findings |
|---|---|---|---|---|---|
| Nowitzke [16] (2005) | Microendoscopic discectomy | Prospective | 35 | IV | Procedure time: asymptote reached at Case 30 |
| Jhala and Mistry [6] (2010) | Microendoscopic discectomy | Retrospective | 100 | IV | Complications: all occurred in initial 10 cases (n = 4): nerve root injury with conversion (Case 1), discitis (Case 4), unintended removal of facet joint (Case 5), dural tear (Case 7) |
| Rong et al. [23] (2008) | Microendoscopic discectomy | Prospective | 60 | IV | Conversion to open: 1 in the initial 10 procedures; none thereafter |
| Complications: all occurred in the initial 20 procedures (n = 5) | |||||
| Procedure time: asymptote reached at Case 20 | |||||
| EBL: asymptote reached at Case 20 | |||||
| Reoperations: none | |||||
| McLoughlin and Fourney [15] (2008) | Tubular microdiscectomy | Prospective | 52 | IV | Complications: all occurred in the initial 30 procedures (n = 3); dural tears (Cases 2, 8, 26) |
| Procedure time: asymptote reached at Case 15 | |||||
| Parikh et al. [18] (2008) | Microdiscectomy and MIS laminectomy | Prospective | 230 | III | Procedure time: 55% decrease in procedure time from initial case to Case 230 |
| Lee and Lee [12] (2008) | Pecutaneous endoscopic lumbar discectomy | Prospective | 51 | IV | Complications: all occurred in the initial 25 procedures (n = 2) |
| Procedure time: asymptote reached at Case 35 | |||||
| Clinical outcome: trend toward better clinical outcome with more experience | |||||
| Foley and Gupta [3] (2002) | Percutaneous pedicle screw | Prospective | 52 (screws) | IV | Complications: single reoperation for hardware loosening (Case 1) |
| Procedure time: decreased chronologically | |||||
| Lau et al. [11] (2011) | MIS TLIF | Retrospective | 10 | III | Complications: in initial 10 cases (n = 4); cardiopulmonary event and deep wound infection (n = 1), superficial wound infection (n = 1), pseudarthrosis (n = 1), instrumentation malposition requiring reoperation (n = 1) |
| Park and Ha [19] (2007) | MIS TLIF | Prospective | 32 | II | Complications: 13% rate in the initial 32 cases (n = 4); screw malposition (n = 1), spacer migration (n = 1), deep wound infection (n = 1), nonunion (n = 1) |
| Schizas et al. [25] (2009) | MIS TLIF | Prospective | 18 | II | Complications: no pattern of increased complications during initial MIS cases compared to open group |
| Procedure time: asymptote reached at Case 15 (30% decrease from initial case) | |||||
| EBL: lower EBL in initial series of MIS group compared to open group | |||||
| Dhall et al. [1] (2008) | MIS TLIF | Retrospective | 21 | III | Complications: 14% rate in the initial 20 cases (n = 3); spacer migration (n = 1), malpositioned screw (n = 1), pseudarthrosis (n = 1) |
| Procedure time: asymptote reached at Case 20 (50% decrease from initial case) | |||||
| EBL: lower EBL in initial series of MIS patients compared to open patients | |||||
| Kim et al. [8] (2008) | MIS TLIF-imaging technology | Prospective/retrospective | 10/8 | III | Complications: none in initial series |
| Procedure time: navigation reduces fluoroscopy time and radiation exposure without increasing overall operative time | |||||
| Regan et al. [21] (1999) | Laparoscopic ALIF | Prospective | 240 | IV | Procedure time: 23% decrease in operative time for all learning surgeons (first five cases vs last five cases) |
| Tan et al. [27] (2008) | Endoscopic anterior cervical discectomy | Prospective | 36 | IV | Procedure time: asymptote reached at Case 20 |
| Conversion to open: none reported | |||||
| Fusion rate: 100% fusion rate | |||||
| Scheufler and Kirsch [24] (2007) | Percutaneous posterior cervical decompression | Prospective | 11 | IV | Procedure time: decreased 41% over initial series |
MIS = minimally invasive surgery; TLIF = transforaminal lumbar interbody fusion; ALIF = anterior lumbar interbody fusion; EBL = estimated blood loss.
The mean publication year was 2007 (median 2008). We included three microendoscopic decompression studies, two tubular microdiscectomy studies, one percutaneous endoscopic lumbar discectomy study, one percutaneous pedicle screw study, four MIS TLIF studies, one laparoscopic ALIF study, one endoscopic anterior cervical decompression study, one MIS posterior cervical decompression study, and one imaging technology study in this review.
Of 966 MIS procedures for the spine included in this review, data were collected prospectively on 827 cases and retrospectively on 139 cases. We included nine publications with Level IV evidence (case series without comparison group) [3, 6, 12, 15, 16, 21, 23, 24, 27], four with Level III evidence (retrospective comparative study) [1, 8, 11, 18], and two with Level II evidence (prospective comparative study) [19, 25].
MIS learning curve parameters that were assessed relative to chronologic case number were operative time (n = 11), complication type/frequency (n = 10), and estimated blood loss (n = 2). The overall postoperative complication rate was 11% (109 of 966 cases).
All findings were summarized qualitatively without statistical pooling or performing meta-analysis. Statistical findings from relevant studies are listed individually (Table 1).
Results
Decompression Procedures
Results from 528 decompression procedures (428 prospective, 100 retrospective) were included from six publications [6, 12, 15, 16, 18, 23] (Table 1). Five studies had Level IV evidence [6, 12, 15, 16, 23] and one had Level III evidence [18]. There were 195 microendoscopic discectomy cases, 282 tubular microdiscectomy cases, and 51 percutaneous endoscopic lumbar discectomy cases included in this review [6, 12, 15, 16, 18, 23].
All cases of durotomy, neurologic injury, and conversion to open procedures in these publications occurred within the initial 30 cases. When adverse events were recorded relative to sequential case number, there were combined complication rates of 11% (31 of 283) during the initial 30 decompression cases performed and 0% (0 of 117) after the 30th consecutive case by the learning surgeon. An overall complication rate of 6% (37 of 580) was reported in this collection of studies. The most frequently reported complications were durotomy (n = 25), nerve root compromise (n = 3), and incorrect level operation (n = 2). There was a combined reoperation rate of 3% (19 of 580) and a rate of conversion to open technique of 2% (five of 247).
Procedure length was also reported as a function of chronologic case number in four publications [15, 16, 18, 23]. The operative time was observed to decrease throughout these case series and approached an asymptote between the 15th and 30th procedure.
Percutaneous Pedicle Screw Insertion
A single percutaneous pedicle screw insertion learning curve study (Level IV evidence) met the inclusion criteria [3] (Table 1). That prospective study reported data on 52 successive percutaneous pedicle screw insertions in 12 patients. The authors of that study discovered loosening of the fixation construct after the first chronologic case that required revision surgery. There were no subsequent complications in that study.
MIS TLIF
Results from 99 MIS TLIF procedures (60 prospective, 39 retrospective) were included from five publications [1, 8, 11, 19, 25] (Table 1). The evidence was classified as Level II in two of these studies [19, 25] and as Level III in three studies [1, 8, 11].
For these studies, there was an overall complication rate of 20% (20 of 99), which included instrumentation malposition/migration (n = 6), perioperative infection (n = 4), nonunions (n = 5), durotomy (n = 1), and postoperative contralateral stenosis (n = 1). There were no reported conversions from MIS to open TLIF procedures. There was a cumulative complication rate of 33% (10 of 30) in three separate studies that evaluated complication rate relative to chronologic case number within the initial 10 cases performed by the learning surgeon [1, 11, 25].
There were two MIS TLIF studies that reported procedure time as a function of chronologic case number and they demonstrated mean decreases in operative time of 33% (360 minutes to 240 minutes) and 50% (250 minutes to 125 minutes) over the initial 20 MIS TLIF cases [1, 25]. These results suggest that the MIS TLIF learning curve in terms of operative time is approximately 20 cases.
ALIF
A single prospective collection of 240 laparoscopic ALIF procedures (Level IV evidence) met inclusion criteria and was included in the review [21] (Table 1). A total of 19 surgeons participated in this study. Collectively, there was a rate of intraoperative conversion to a traditional ALIF of 10% (25 of 240) and a reoperation rate of 5% (10 of 215). Complication rate was not assessed relative to chronologic procedure number. There was a mean decrease in operative time of 23% (215 minutes to 165 minutes) between the first five and last five procedures performed by each participating surgeon.
MIS Cervical Procedures
The search strategy captured prospectively collected data for 36 endoscopic anterior cervical decompression [27] and 11 percutaneous posterior cervical decompression procedures [24] (Table 1). The evidence in both studies was categorized as Level IV.
There was a complication rate of 3% (one of 36) (wound dehiscence) reported in the endoscopic anterior cervical decompression learning curve study [27] and no perioperative complications reported in a series of 11 percutaneous posterior cervical decompression and fusion procedures [24]. All cases were successfully completed without conversion to open techniques.
Operative time decreased 41% (243 minutes to 143 minutes) over the initial 10 cases of the posterior cervical decompression and fusion series [24]. Similarly, procedure length decreased 50% (140 minutes to 70 minutes) as the endoscopic anterior cervical decompression learning curve was overcome and an operative time asymptote was approached by the 20th procedure [27].
Discussion
There is an inherently difficult learning curve associated with MIS approaches to spinal decompression and fusion procedures. Since the association between important surgical parameters such as complication rate and operative time and the learning curve remains unclear, we conducted a review to characterize complication rate and operative time as a function of surgeon experience with MIS techniques for the spine. All studies that met the inclusion criteria of this review presented complication rate or operative time in terms of chronologic case number for the learning surgeon. The learning curve was overcome for both parameters after 30 chronologic cases in this collection of studies representing several MIS techniques.
This systematic review had a number of limitations. First, the learning surgeon may preferentially choose straightforward cases early in their experience with a new MIS technique, which could result in misleading complication rate and procedure time data. This selection bias would be reduced in an unselected series or properly designed randomized controlled study. Second, procedure time and complication rate were measured inconsistently in the included studies. In many cases, the operating surgeon was responsible for detecting these end points, which could greatly affect the frequency and severity of reported adverse events. Given these limitations, data presented in this review should be interpreted as merely an estimation of surgeon progression through the MIS learning curve.
Perhaps the most clinically relevant parameter used to assess surgeon progression through the procedural learning curve is complication rate. All complications, adverse events, and conversions to open techniques occurred within the initial 30 procedures when these parameters were reported as a function of chronologic case number. The lack of clear anatomic landmarks appears to be a significant limitation in the MIS approach to the spine. Jhala and Mistry [14] attributed complications during the microendoscopic discectomy learning curve period to unfamiliarity with endoscopic image orientation and suboptimal approach to the surgical target. This resulted in injury to neurologic structures, multiple durotomies, wrong-level procedures, and unintended removal of facet joint structures in the initial series of patients. Multiple authors argue the key step in overcoming the MIS learning curve is an ideal entry point and trajectory during the surgical approach [1, 19, 23]. Dhall et al. [1] and Park and Ha [19] both assert that a correct initial placement of the tubular dilator during the MIS TLIF approach prevents intraoperative readjustments, which can lead to a high rate of neurologic injury and inadequate decompression.
Procedure time is a frequently used parameter to assess surgeon progression through the learning curve. Several studies plotted operative time as a function of chronologic case number and correlated surgeon comfort and technical efficiency to a decrease in procedure length [1, 12, 15, 16, 21, 23–25, 27]. These studies demonstrated procedure time rapidly decreased 23% to 58% during the initial series of cases and approached an asymptote between the 10th and 30th case [1, 15, 16, 21, 23–25, 27].
In summary, we found that studies evaluated the learning curve very inconsistently. Most studies utilized procedure time versus chronologic case number as the main parameter to assess competence. Complication rate as a function of chronologic case number, a key parameter, was not always discussed. Standardization of studies on this important topic would allow better assessment of strategies to decrease learning curve problems, such as the use of advanced intraoperative imaging technologies or specialized training programs. Future studies should standardize learning curve assessment to include both procedure time and complication rate as a function of case number. Additional parameters such as health-related quality-of-life outcomes, estimated blood loss, reoperation rate, and conversion to open techniques should also be evaluated in relation to sequential procedure performed within the learning curve period.
Footnotes
One of the authors (JAS) certifies that he, or a member of his immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article. One of the authors certifies that he (CWK), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount less than USD 10,000 from Globus Medical (Audubon, PA, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
References
- 1.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up: clinical article. J Neurosurg Spine. 2008;9:560–565. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 2.Eck JC, Hodges S, Humphreys SC. Minimally invasive lumbar spinal fusion. J Am Acad Orthop Surg. 2007;15:321–329. doi: 10.5435/00124635-200706000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002;97(1 suppl):7–12. doi: 10.3171/spi.2002.97.1.0007. [DOI] [PubMed] [Google Scholar]
- 4.Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929–1941. [DOI] [PubMed]
- 5.Jaikumar S, Kim DH, Kam AC. History of minimally invasive spine surgery. Neurosurgery. 2002;51:S1–S14. doi: 10.1097/00006123-200211002-00003. [DOI] [PubMed] [Google Scholar]
- 6.Jhala A, Mistry M. Endoscopic lumbar discectomy: experience of first 100 cases. Indian J Orthop. 2010;44:184–190. doi: 10.4103/0019-5413.62051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim CW. Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine (Phila Pa 1976). 2010;35:S281–S286. doi: 10.1097/BRS.0b013e3182022d32. [DOI] [PubMed] [Google Scholar]
- 8.Kim CW, Lee YP, Taylor W, Oygar A, Kim WK. Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J. 2008;8:584–590. doi: 10.1016/j.spinee.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Kim CW, Siemionow K, Anderson DG, Phillips FM. The current state of minimally invasive spine surgery. Instr Course Lect. 2011;60:353–370. [PubMed] [Google Scholar]
- 10.Kotani Y, Abumi K, Ito M, Sudo H, Abe Y, Minami A. Mid-term clinical results of minimally invasive decompression and posterolateral fusion with percutaneous pedicle screws versus conventional approach for degenerative spondylolisthesis with spinal stenosis. Eur Spine J. 2012;21:1171–1177. doi: 10.1007/s00586-011-2114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF) J Clin Neurosci. 2011;18:624–627. doi: 10.1016/j.jocn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo). 2008;48:383–389. doi: 10.2176/nmc.48.383. [DOI] [PubMed] [Google Scholar]
- 13.Mathews HH, Long BH. Minimally invasive techniques for the treatment of intervertebral disk herniation. J Am Acad Orthop Surg. 2002;10:80–85. doi: 10.5435/00124635-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 14.McAfee PC, Phillips FM, Andersson G, Buvenenadran A, Kim CW, Lauryssen C, Isaacs RE, Youssef JA, Brodke DS, Cappuccino A, Akbarnia BA, Mundis GM, Smith WD, Uribe JS, Garfin S, Allen RT, Rodgers WB, Pimenta L, Taylor W. Minimally invasive spine surgery. Spine (Phila Pa 1976). 2010;35:S271–S273. doi: 10.1097/BRS.0b013e31820250a2. [DOI] [PubMed] [Google Scholar]
- 15.McLoughlin GS, Fourney DR. The learning curve of minimally-invasive lumbar microdiscectomy. Can J Neurol Sci. 2008;35:75–78. doi: 10.1017/s0317167100007599. [DOI] [PubMed] [Google Scholar]
- 16.Nowitzke AM. Assessment of the learning curve for lumbar microendoscopic discectomy. Neurosurgery. 2005;56:755–762. doi: 10.1227/01.NEU.0000156470.79032.7B. [DOI] [PubMed] [Google Scholar]
- 17.Oppenheimer JH, DeCastro I, McDonnell DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus. 2009;27:E9. doi: 10.3171/2009.7.FOCUS09121. [DOI] [PubMed] [Google Scholar]
- 18.Parikh K, Tomasino A, Knopman J, Boockvar J, Härtl R. Operative results and learning curve: microscope-assisted tubular microsurgery for 1-and 2-level discectomies and laminectomies. Neurosurg Focus. 2008;25:E14. doi: 10.3171/FOC/2008/25/8/E14. [DOI] [PubMed] [Google Scholar]
- 19.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine (Phila Pa 1976). 2007;32:537–543. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 20.Perez-Cruet MJ, Fessler RG, Perin NI. Review: complications of minimally invasive spinal surgery. Neurosurgery. 2002;51:S26–S36. [PubMed] [Google Scholar]
- 21.Regan JJ, Yuan H, McAfee PC. Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery: a prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine (Phila Pa 1976). 1999;24:402–411. doi: 10.1097/00007632-199902150-00023. [DOI] [PubMed] [Google Scholar]
- 22.Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976). 2011;36:26–32. doi: 10.1097/BRS.0b013e3181e1040a. [DOI] [PubMed] [Google Scholar]
- 23.Rong LM, Xie PG, Shi DH, Dong JW, Lin B, Feng F, Cai DZ. Spinal surgeons’ learning curve for lumbar microendoscopic discectomy: a prospective study of our first 50 and latest 10 cases. Chin Med J (Engl). 2008;121:2148–2151. [PubMed] [Google Scholar]
- 24.Scheufler KM, Kirsch E. Percutaneous multilevel decompressive laminectomy, foraminotomy, and instrumented fusion for cervical spondylotic radiculopathy and myelopathy: assessment of feasibility and surgical technique. J Neurosurg Spine. 2007;7:514–520. doi: 10.3171/SPI-07/11/514. [DOI] [PubMed] [Google Scholar]
- 25.Schizas C, Tzinieris N, Tsiridis E, Kosmopoulos V. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009;33:1683–1688. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sclafani JA, Regev GJ, Webb J, Garfin SR, Kim CW. Use of a quantitative pedicle screw accuracy system to assess new technology: initial studies on O-arm navigation and its effect on the learning curve of percutaneous pedicle screw insertion. SAS J. 2011;5:57–62. doi: 10.1016/j.esas.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan J, Zheng Y, Gong L, Liu X, Li J, Du W. Anterior cervical discectomy and interbody fusion by endoscopic approach: a preliminary report. J Neurosurg Spine. 2008;8:17–21. doi: 10.3171/SPI-08/01/017. [DOI] [PubMed] [Google Scholar]
- 28.Voyadzis JM. The learning curve in minimally invasive spine surgery. Semin Spine Surg. 2011;23:9–13. doi: 10.1053/j.semss.2010.11.003. [DOI] [Google Scholar]