Abstract
Objective
To investigate the concentration of the integrase strand inhibitor raltegravir (RAL) throughout gastrointestinal (GI) tissue, especially gutassociated lymphoid tissue (GALT), as an adjunct to current prevention and cure strategies.
Design
Open-label pharmacokinetic study
Methods
HIV-negative men received RAL 400 mg twice daily for 7 days. Seven blood plasma (BP) specimens were collected over 12-hr intervals; timed tissue specimens from terminal ileum, splenic flexure, and rectum were also obtained by colonoscopy following the first dose (FD) and on Day 7 [Multiple Dose (MD)]. RAL concentrations were measured by validated LC-MS assay with 1 ng/mL lower limit of detection. Data were analyzed by noncompartmental methods (WinNonlin 6). Tissue exposures are reported as composite medians and tissue density of 1.04 g/mL is assumed for comparisons.
Results
Fourteen men completed evaluations. Median (range) age was 24 (19–49) yrs and BMI 25 (19–31) kg/m2. After the FD, AUC-0-12h was highest in the terminal ileum (594 μg*h/mL). Exposures were 160, 68 and 39-fold greater than BP at the terminal ileum, splenic flexure and rectum, respectively. After multiple doses, exposure was highest at the splenic flexure (2240 μg*h/mL); exposure at the terminal ileum and rectum were equivalent (both 788 μg*h/mL). Following multiple doses, exposures were 160–650-fold greater than BP throughout the colon.
Conclusions
RAL rapidly disseminates into GI tissue and concentrations remain significantly higher than BP. RAL exposure in GI tissue remains higher than any ARV investigated to date. These data suggest that RAL should result in full suppression of viral replication in GI tissue and GALT.
Keywords: gut-associated lymphoid tissue, HIV cure, latency, pharmacokinetics, raltegravir
Background
Combination antiretroviral therapy (ART) results in significant reduction in morbidity and mortality in those individuals who achieve sustained virologic suppression [1–3]. Efforts are now focusing on eradication of the HIV epidemic, which require the prevention of new infections and the elimination of HIV from infected individuals. Two methods of ‘cure’ are being considered: the complete elimination of HIV from infected individuals or rendering the virus incapable of further replication (‘functional cure’). Complete eradication, however, is obstructed by pools of latently infected resting CD4+ T cells capable of viral replication [4,5] that are established early in infection [6], and are not protected by the rapid initiation of ART following infection [7].
Gut-associated lymphoid tissue (GALT) is the largest aggregate of lymphoid tissue within the body. GALT contains a high concentration of activated CD4+ T cells susceptible to HIV infection, the majority of which die quickly as a result of viral cytopathic effects or host responses [8–10]. However, a minority of infected CD4+ T cells survive, reverting to a latent resting state [6,11], and are capable of viral replication when activated [5,12]. These cells may be protected from the effects of potent antiretroviral therapy despite suppression of plasma viremia [4,13].
Numerous strategies aimed towards reversing latency or activating resting infected CD4+ T cells are currently being investigated [14–21]. The integrase strand transfer inhibitors such as raltegravir prevent the integration of reverse transcripts into newly infected CD4+ T cells, aborting ongoing rounds of viral replication. These drugs are well-tolerated with minimal drug-drug interactions [22]. However to be efficacious, these agents require rapid and high penetration into lymphoid tissue where latent CD4+ T cells reside. Our previous investigations demonstrated wide variability in the penetration of ARVs into rectal tissue [23,24]. However, all segments of gastrointestinal tissue may not be equally permissive to ARVs, nor representative of the entire colon. Identifying therapeutics achieving high penetration into viral reservoirs is a key component to the HIV cure initiative. The primary objective of the following investigation was to determine the penetration of raltegravir into three segments of the gastrointestinal tract, including GALT, after single and multiple dosing.
Methods
Study design and subject selection
Healthy HIV-negative male volunteers were enrolled in this 7-day, open-label, investigator-initiated, pharmacokinetic study at the University of North Carolina at Chapel Hill (UNC). The UNC Biomedical Review Board approved the study, which was registered with ClinicalTrials.gov (NCT01325051). All visits were conducted in the UNC Clinical and Translational Research Unit. All subjects provided written informed consent prior to study procedures. Subjects were enrolled from April and November 2011.
Subjects were screened within 42 days before study medication dosing. Screening procedures consisted of a complete medical history and physical examination, 12-lead electrocardiogram (ECG) with cardiology interpretation, comprehensive laboratory studies (complete blood count with differential, liver function tests, serum chemistries, urinalysis, and urine toxicology). Subjects were screened for active hepatitis B and hepatitis C, and HIV (ARCHITECT HIV Ab/Ag Combo Abbott Laboratories, Saint-Laurent, Quebec, Canada). All testing was performed in the UNC Health Care McClendon Laboratories. Testing for rectal sexual transmitted infections, including Neisseria gonorrhea, Chlamydia trachomatis was performed in the Microbiology Core Laboratory of the Southeastern Sexually Transmitted Infections Cooperative Research Center (Gen-Probe Aptima® San Diego, CA).
Subjects were eligible to participate if they were healthy males between 18–49 years of age, and had a body mass index (BMI) 18–30 kg/m2 with a total body weight >50 kg. Subjects were required to have a fully intact gastrointestinal tract. Subjects agreed to not participate in the conception process, abstain from all sexual intercourse and the use of intra-rectal products for 72 hours before study entry until study discharge. Subjects were excluded for any clinically significant abnormal laboratory tests, physical findings or clinical condition that would interfere with study procedures. Subjects were required to stop all prescription and nonprescription medications 7 days before and herbal supplements 14 days before study enrollment, and medications could not be restarted until study completion. Subjects were limited to consumption of less than 14 alcoholic beverages per week, and acetaminophen at doses of <1gm/day.
Study visits
Subjects received raltegravir 400 mg orally twice daily on days 1–6 and a single dose on day 7 for a total of 13 doses. Subjects participated in two intensive PK visits, coinciding with the first and last dose of study drug. No less than 24 hours prior to both PK visits, subjects began a clear liquid diet without solid food, milk, coffee, tea or any product containing red or purple dye. Subjects were admitted to the inpatient research unit 18 hours prior to each colonoscopy, during which time an observed full bowel preparation with a gallon of polyethylene glycol consumed in four hours or less was performed. At both PK visits, blood was collected within 30 minutes before observed dose followed by 1, 2, 3, 4, 6, 8, and 12 hours post-dose. Each subject was assigned to a colonoscopy procedure time coinciding with a post-dose time, which was identical for both first dose and steady state (multiple dose) procedures. Two subjects were assigned to one of seven potential times (1, 2, 3, 4, 6, 8, and 12 hr post-dose). All subjects were observed for at least six hours post-colonoscopy. Subjects recorded on a drug diary card the time of all outpatient doses on days 2–6, and were contacted by telephone each day to assess adverse events and compliance with study medication dosing. Subjects returned to the clinic for a follow-up safety visit 7–10 days after final dose.
Sample collections
Blood plasma
Whole blood was obtained using K2EDTA collection tubes (BD Diagnostics, Franklin Lakes, NJ) and centrifuged at 800 g at 4°C for 10 minutes. Aliquots of the resulting blood plasma were distributed into labeled cryovials and stored at −80°C until analysis.
Gastrointestinal tissue
Intestinal tissue samples were obtained during colonoscopy at one of two UNC Gastrointestinal (GI) Procedure Suites according to standard GI procedures. Monitored conscious sedation was provided for all subjects. Biopsy sites were identified and rinsed with sterile irrigation water containing simethicone 40 mg oral drops (40 mg/ 0.6 ml, Major Pharmaceuticals, Livonia, MI) before collection. Biopsies were taken from each of three locations: terminal ileum, splenic flexure, and rectum (approximately 15 cm from the anal verge). Five double biopsies were collected at each site using a Radial Jaw 4 Large Capacity Forceps with needle (Boston Scientific, Natick, MA). Biopsy specimens from each site were pooled into a single labeled cryovials, and immediately snap-frozen in liquid nitrogen. All specimens were stored at −80°C until analysis.
Sample analysis
Raltegravir concentrations in blood plasma and intestinal tissue were analyzed by a validated LC-MS assay with a 1ng/mL lower limit of detection.
Statistical analysis
Pharmacokinetic parameters were estimated using non-compartmental methods (Phoenix WinNonlin Pro 5.2; Certara, L.P., St. Louis MO). Maximum concentration (Cmax), time at maximum concentration (Tmax), and concentration 12 hours after dosing (C12h) were determined by visual inspection of the subject profiles, and used the log-linear trapezoidal method to calculate the area-under-the-time-concentration-curve over the 12-hour dosing interval (AUC0-12h). A tissue density of 1.04 g/mL was used to convert ng/g to ng/mL [25]. For tissue, composite concentration-time profiles were created using median concentrations for calculating and reporting pharmacokinetic parameters. Descriptive statistics using WinNonlin® were performed. Demographic data are presented as median (range). Pharmacokinetic data are presented as median (25th–75th percentile) for plasma, and as a single composite value from median tissue concentrations. Accumulation ratios were calculated utilizing the equation Multiple Dose AUC0-12h/First Dose AUC0-12h.
Results
Subject demographics, disposition, and safety
Nineteen men screened for this study: 15 were enrolled, and 14 completed the protocol. One subject was withdrawn from participation following the first pharmacokinetic visit due to significant findings on colonoscopy. This subject did not contribute demographic or pharmacokinetic data, and was referred for appropriate follow up. Median (range) age of the 14 evaluable participants was 24 (19–49) years, weight was 80.1 (56.5–104.9) kg, and body mass index was 25.3 (19.0–30.9) kg/ m2. Nine (64%) subjects were Caucasian, and five (36%) were African American. Subjects tolerated the study medication well. One subject had a mild increase in pre-existing intermittent elevated alanine aminotransferase (ALT), which returned to normal prior to study discharge. Two evaluable subjects had incidental findings of polyps on initial colonoscopy.
Pharmacokinetics
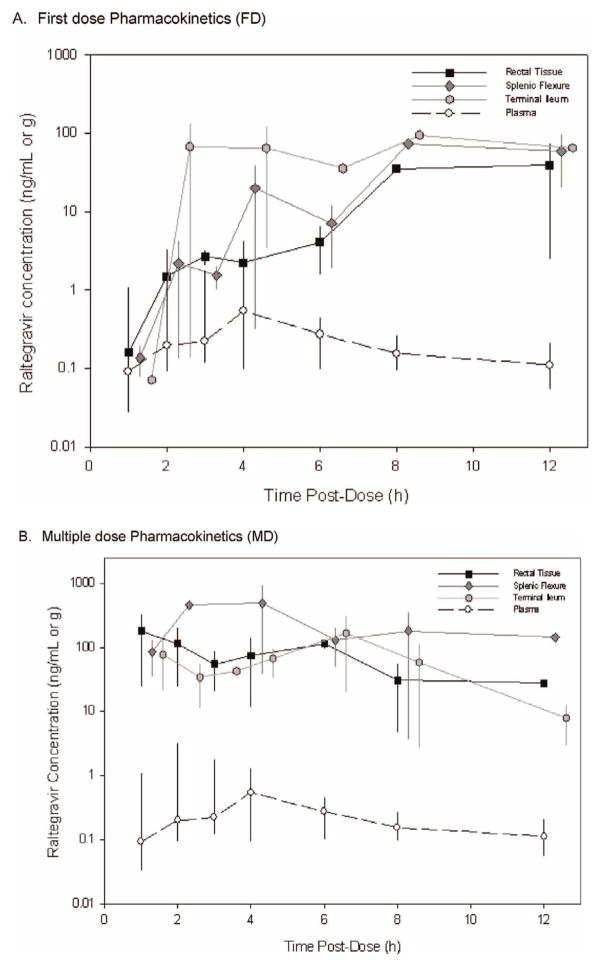
Table 1 summarizes the pharmacokinetic parameters, relative exposures compared to BP, and accumulation over time for each matrix. Figure 1a and 1b represent the pharmacokinetic profiles of all biological matrices following the 1st and 13th dose, respectively, over a 12-hour dosing period. Raltegravir concentrations throughout the GI tract were similar to blood plasma within one hour following the first dose, achieve steady-state concentrations within 12 hours after the first dose, and remain considerably higher than blood plasma.
Table 1.
Pharmacokinetic Parameters.
| Pharmacokinetic Parameters | Blood Plasma
|
Rectal Tissue
|
Splenic Flexure
|
Terminal Ileum
|
||||
|---|---|---|---|---|---|---|---|---|
| First Dose | Multiple Dose | First Dose | Multiple Dose | First Dose | Multiple Dose | First Dose | Multiple Dose | |
| Tmax (hr) | 4 (1.9–12.6) | 3.5 (1–8.9) | 12.2 | 3.4 | 10 | 3.4 | 9.9 | 8.6 |
| Cmax (μg/mL) | 0.8 (0.005–6.7) | 0.7 (0.3–5.7) | 39 | 114 | 73 | 291 | 95 | 58 |
| C12h (μg/mL)* | 0.1 (0.065–0.380) | 0.09 (0.040–0.35) | 39 | 28 | 59 | 144 | 64 | 7.8 |
| AUC0-12h (μg* hr/mL)* | 3.7 (1.5–9.5) | 3.4 (1.5–20.5) | 143 | 788 | 258 | 2240 | 594 | 788 |
| BP: Tissue Ratio** | ||||||||
| AUC0-12h (μg* hr/mL) | – | – | 39 | 231 | 68 | 659 | 160 | 156 |
| C12h (μg/mL) | – | – | 390 | 311 | 590 | 1600 | 640 | 87 |
| PK2: PK1 Accumulation Ratios*** | 0.9 (1.0–2.2) | 5.5 | 8.7 | 0.9 | ||||
Composite Profile.
Composite Profile Ratios are calculated using the parameter values for individual tissue type and the median of blood plasma.
Accumulation Ratios are calculated by utilizing the equation: Multiple Dose AUC 0–12 h/First Dose AUC 0–12 h.
Fig. 1.
(a). First dose Pharmacokinetics (FD). (b). Multiple dose Pharmacokinetics (MD)
Blood Plasma
Following the first dose, the AUC0-12h of raltegravir in blood plasma was 3.7 (1.5–9.5) μg*hr/mL, and 3.4 (1.5–20.5) μg*hr/mL after multiple doses. Raltegravir did not accumulate in blood plasma over the study period (MD to FD ratio: 0.9). Overall, the pharmacokinetic profiles in blood plasma following the first dose and multiple doses were consistent with previous results in HIV-negative [26] and HIV-positive [27] women.
Terminal ileum
After the first dose, raltegravir readily penetrated the terminal ileum with concentrations equivalent to blood plasma 1-hour post dose and exceeding blood plasma within 2 hours. Peak concentrations were reached by 4 hours post-dose and remained higher than other segments of the colon for the duration of the first 12-hour dosing period (Fig. 1). Pharmacokinetic parameters are listed in Table 1. The concentration 12 hours after the first dose (C12h) was 64 μg/mL. AUC0-12h was 160-fold higher than blood plasma [594 vs. 3.7 (IQR 1.5–9.5) μg*hr/mL]. With repeated doses, tissue exposure increased by 30% (788 μg*hr/mL), while plasma exposure remained stable (3.7 vs. 3.4 μg*hr/mL). C12h concentrations were lower after multiple doses versus the first dose (7.8 vs. 64 μg/mL). However, all C12h concentrations were >80-fold higher than blood plasma concentrations across all doses. Cumulative tissue exposure was essentially unchanged (MD: FD ratio of 0.9) and was 156-fold higher than blood plasma.
Splenic flexure
The maximum concentration at the splenic flexure was reached 10 hours after the first dose and was 49-fold higher than blood plasma. C12h was similar to concentration in the terminal ileum (59 vs. 64 μg/mL). Following multiple doses, the AUC0-12h increased from 258 to 2240 μg*hr/mL, which was approximately 650-fold higher than blood plasma. Raltegravir accumulated in the area of the splenic flexure more than any other area within the gastrointestinal tract following multiple doses (accumulation ratio = 8.7).
Rectum
Following the initial dose, the AUC0-12h was lower in the rectum (143 μg*hr/mL) than in other segments of the colon, but accumulated 5-fold with repeated dosing (first dose AUC0-12 143 μg*hr/mL; multiple dose AUC0-12h 788 μg*hr/mL). C12h were 40% lower compared to the terminal ileum (64 μg/mL) after the first dose, but remained >200-fold higher than blood plasma concentrations across the multiple dosing period.
Discussion
Within the terminal ileum, raltegravir rapidly penetrates and surpasses plasma exposure by 160-fold after a single dose. Blood plasma concentrations following 7 days of dosing are achieved in gastrointestinal tissue within 10 hours of dosing. Raltegravir accumulates throughout the GI tissue with exposures 150–600 fold greater than blood plasma following repeated dosing. These concentrations are the highest reported for any orally-dosed antiretroviral in gastrointestinal tissue to date [28].
Previous investigations by our group and others have shown wide variability in colorectal tissue penetration and assumptions between specific antiretroviral agents or classes cannot be made. In HIV-negative men, darunavir exposure in rectal tissue is 2.7 fold higher than blood plasma [24]. The CCR5 antagonist maraviroc exposure in rectal tissue is even higher: 9-fold following a single dose and 27-fold higher than blood plasma following multiple doses [23]. Following multiple doses, etravirine exposure is 2-fold higher than blood plasma [24]. The wide variability in exposure between drugs with similar mechanisms of action and within the same tissue is exemplified in the NRTIs tenofovir and emtricitabine. In rectal tissue, tenofovir exposures are 46-fold higher while emtricitabine exposures are 2.6-fold higher than blood plasma following a single dose [29].
The reported concentrations are dependent on the methods in which the antiretroviral agents are being measured. For example, low or sub-therapeutic concentrations of atazanavir, tenofovir and emtricitabine were found in isolated mononuclear cells from the colorectal tissue of 5 HIV-infected men [30,31]. In contrast our previous [23,24,29,32] and current work quantifies the drug of interest in homogenized tissue. Others have measured intracellular concentrations of raltegravir from peripheral blood mononuclear cells using methods similar to intracellular reverse transcriptase inhibitors [33,34]. However, underestimation of drug concentrations may result from analyzing specific cells from colonic tissue due to the difficulty in obtaining sufficient quantities of in vivo tissue required to accurately identify and isolate enough cells. In contrast, the use of tissue homogenates may result in an overestimation in drug exposure, as both intracellular and extracellular concentrations are being measured. These studies emphasize the importance in developing standard methods for measuring drug concentrations in specific matrices in order to expedite research priorities such that results across investigations can be compared and target concentrations based on specific objections (eg eradication, treatment, or prevention) can be determined.
Eradication priorities have been recently outlined [35]. Embedded within these priorities are strategies aimed towards disrupting proviral quiescence in latently infected CD4+ T cells and using a multi-dimensional approach to block production of infectious virions. The viral decay kinetics of raltegravir [36–38] suggests that as resting CD4+ T cells are activated, these virions could be quickly rendered non-infectious. Our findings demonstrate that raltegravir achieves maximum concentrations in GALT within 12 hours after a single dose, and suggests that an extended dosing period would not be required before interventions aimed at activating the latent reservoir were initiated. Although it could be theorized that the high tissue concentrations quantifiable within 1 hour of dosing are due to rapid gastrointestinal absorption following a complete bowel preparation, plasma concentrations are similar to those in our previous investigations [26,27] suggesting that absorption is not significantly altered by the bowel preparation. Additionally, we have noted rapid drug delivery to colorectal tissue with maraviroc, darunavir, and etravirine in subjects where bowel preparation was not performed [23,24].
Furthermore, a mechanism by which efficacy of potential strategies is easily quantified and reflective of all lymphoid tissue is essential. Rigorous investigations following antiretroviral intensification with raltegravir demonstrate the lack of effect on low-level plasma viremia [39–42], which may not reflect alterations elsewhere in the body. For example, seven HIV-infected individuals were noted to have a reduction in proviral DNA in GALT following raltegravir intensification [43]. In acutely infected individuals in which there is rapid depletion of active CD4+ T cells, the prompt initiation of ‘megaART’ –—including raltegravir and the CCR5-receptor agonist maraviroc to standard ART–—results in a reduction in HIV DNA from rectal tissue [44]. Similarly, the marked reduction of rectal tissue HIV DNA in rhesus macaques with chronic simian immunodeficiency virus is also seen with the addition of raltegravir and maraviroc to standard antiretroviral therapy [45]. Depending on the application, as this investigation found, targeting different areas of the colon (eg. GALT vs. colorectal tissue) may be necessary to make precise measures of drug exposure and determine subsequent pharmacokinetic predictors of drug efficacy.
This study reinforces that tissue pharmacokinetics can be unpredictable, and need to be evaluated in the relevant tissues for the appropriate clinical application. We have demonstrated that precisely timed tissue specimens across the gastrointestinal tract can be obtained and data quantified for informative pharmacokinetic information. In this study, we demonstrate that raltegravir can rapidly and efficiently penetrate GALT and colorectal tissue. Identifying antiretrovirals that can enter these viral reservoirs at highly active concentrations can facilitate the selection of optimal therapy for investigations in the prevention and cure of HIV infection.
Acknowledgments
Supported in part by National Institutes of Health grants R37 DK49381 (MS Cohen), R34 AI087065 (ADM Kashuba), K23 AI773355 (KB Patterson), U01 AI095031 (ADM Kashuba), P30 AI50410 (UNC Center for AIDS Research), and UL1 RR025747 (UNC TraCS Clinical Translational Research Center). Supported in part by the Merck Investigator Initiated Research Program. Rectal sexually transmitted disease screening was performed in the Microbiology Core Laboratory of the Southeastern Sexually Transmitted Infections Cooperative Research Center under the direction of Dr. Marcia Hobbs and supported by NIH grant U19 AI31496. The authors appreciate the efforts of the UNC Gastrointestinal Procedure nurses in coordinating the precise timing of colonoscopies.
This investigation was supported in part by National Institutes of Health grants K23 AI77355 (KB Patterson), R34 AI087065 (ADM Kashuba). U01 AI095031 (ADM Kashuba), P30 AI50410 (UNC Center for AIDS Research), UL1 RR025747 (UNC TraCS Clinical Translational Research Center) and U19 AI31496 (Microbiology Core Laboratory of the Southeastern Sexually Transmitted Infections Cooperative Research Center). Supported also in part by the Merck Investigator Initiated Research Program.
Footnotes
Conflicts of interest
KB Patterson and ADM Kashuba have received investigator initiated research grants from Merck and GlaxoSmithKline. The remaining authors have no competing interests.
Author Contributions: KBP, MSC and ADMK conceived and designed the experiments. HAP and TS coordinated the specimen collections. NJS, ESD, RDM performed the colonoscopies and obtained the biopsy specimens. SJ analyzed the specimens. KBP and ADMK analyzed the data. KBP and ADMK created the presentation of some of the data for the 13th International Workshop on Clinical Pharmacology of HIV Therapy April 16–18, 2012 Barcelona, Spain. KBP and ADMK wrote the paper. All authors reviewed the paper.
References
- 1.Palella FJ, Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338 (13):853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 2.Walensky RP, Paltiel AD, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194 (1):11–19. doi: 10.1086/505147. [DOI] [PubMed] [Google Scholar]
- 3.Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finzi D, Hermankova M, Pierson T, Carruth LM, Buck C, Chaisson RE, et al. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science. 1997;278 (5341):1295–1300. doi: 10.1126/science.278.5341.1295. [DOI] [PubMed] [Google Scholar]
- 5.Wong JK, Hezareh M, Gunthard HF, Havlir DV, Ignacio CC, Spina CA, et al. Recovery of replication-competent HIV despite prolonged suppression of plasma viremia. Science. 1997;278 (5341):1291–1295. doi: 10.1126/science.278.5341.1291. [DOI] [PubMed] [Google Scholar]
- 6.Chun TW, Engel D, Berrey MM, Shea T, Corey L, Fauci AS. Early establishment of a pool of latently infected, resting CD4(+) T cells during primary HIV-1 infection. PNAS. 1998;95 (15):8869–8873. doi: 10.1073/pnas.95.15.8869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hicks CB, Gay C, Ferrari G. Acute HIV infection: the impact of anti-retroviral treatment on cellular immune responses. Clin Exp Immunol. 2007;149 (2):211–216. doi: 10.1111/j.1365-2249.2007.03437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J Exp Med. 2004;200 (6):749–759. doi: 10.1084/jem.20040874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei X, Ghosh SK, Taylor ME, Johnson VA, Emini EA, Deutsch P, et al. Viral dynamics in human immunodeficiency virus type 1 infection. Nature. 1995;373 (6510):117–122. doi: 10.1038/373117a0. [DOI] [PubMed] [Google Scholar]
- 10.Chun TW, Finzi D, Margolick J, Chadwick K, Schwartz D, Siliciano RF. In vivo fate of HIV-1-infected T cells: quantitative analysis of the transition to stable latency. Nature Medicine. 1995;1 (12):1284–1290. doi: 10.1038/nm1295-1284. [DOI] [PubMed] [Google Scholar]
- 11.Finzi D, Blankson J, Siliciano JD, Margolick JB, Chadwick K, Pierson T, et al. Latent infection of CD4+ T cells provides a mechanism for lifelong persistence of HIV-1, even in patients on effective combination therapy. Nature Medicine. 1999;5 (5):512–517. doi: 10.1038/8394. [DOI] [PubMed] [Google Scholar]
- 12.Joos B, Fischer M, Kuster H, Pillai SK, Wong JK, Boni J, et al. HIV rebounds from latently infected cells, rather than from continuing low-level replication. PNAS. 2008;105 (43):16725–16730. doi: 10.1073/pnas.0804192105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gulick RM, Mellors JW, Havlir D, Eron JJ, Gonzalez C, McMahon D, et al. Treatment with indinavir, zidovudine, and lamivudine in adults with human immunodeficiency virus infection and prior antiretroviral therapy. N Engl J Med. 1997;337 (11):734–739. doi: 10.1056/NEJM199709113371102. [DOI] [PubMed] [Google Scholar]
- 14.Davey RT, Jr, Chaitt DG, Albert JM, Piscitelli SC, Kovacs JA, Walker RE, et al. A randomized trial of high- versus low-dose subcutaneous interleukin-2 outpatient therapy for early human immunodeficiency virus type 1 infection. J Infect Dis. 1999;179 (4):849–858. doi: 10.1086/314678. [DOI] [PubMed] [Google Scholar]
- 15.Brooks DG, Arlen PA, Gao L, Kitchen CM, Zack JA. Identification of T cell-signaling pathways that stimulate latent HIV in primary cells. PNAS. 2003;100 (22):12955–12960. doi: 10.1073/pnas.2233345100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han Y, Wind-Rotolo M, Yang HC, Siliciano JD, Siliciano RF. Experimental approaches to the study of HIV-1 latency. Nat Rev Microbiol. 2007;5 (2):95–106. doi: 10.1038/nrmicro1580. [DOI] [PubMed] [Google Scholar]
- 17.Archin NM, Cheema M, Parker D, Wiegand A, Bosch RJ, Coffin JM, et al. Antiretroviral intensification and valproic acid lack sustained effect on residual HIV-1 viremia or resting CD4+ cell infection. PLoS One. 2010;5 (2):e9390. doi: 10.1371/journal.pone.0009390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Archin NM, Eron JJ, Palmer S, Hartmann-Duff A, Martinson JA, Wiegand A, et al. Valproic acid without intensified antiviral therapy has limited impact on persistent HIV infection of resting CD4+ T cells. AIDS. 2008;22 (10):1131–1135. doi: 10.1097/QAD.0b013e3282fd6df4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Archin NM, Liberty AL, Kashuba AD, Choudhary SK, Kuruc JD, Crooks AM, et al. Administration of vorinostat disrupts HIV-1 latency in patients on antiretroviral therapy. Nature. 2012;487 (7408):482–485. doi: 10.1038/nature11286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lehrman G, Hogue IB, Palmer S, Jennings C, Spina CA, Wiegand A, et al. Depletion of latent HIV-1 infection in vivo: a proof-of-concept study. Lancet. 2005;366 (9485):549–555. doi: 10.1016/S0140-6736(05)67098-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xing S, Bullen CK, Shroff NS, Shan L, Yang HC, Manucci JL, et al. Disulfiram reactivates latent HIV-1 in a Bcl-2-transduced primary CD4+ T cell model without inducing global T cell activation. J Virology. 2011;85 (12):6060–6064. doi: 10.1128/JVI.02033-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Havlir DV. HIV integrase inhibitors–out of the pipeline and into the clinic. N Engl J Med. 2008;359 (4):416–418. doi: 10.1056/NEJMe0804289. [DOI] [PubMed] [Google Scholar]
- 23.Brown KC, Patterson KB, Malone SA, Shaheen NJ, Prince HM, Dumond JB, et al. Single and multiple dose pharmacokinetics of maraviroc in saliva, semen, and rectal tissue of healthy HIV-negative men. J Infect Dis. 2011;203 (10):1484–1490. doi: 10.1093/infdis/jir059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown KC, Patterson KB, Jennings SH, Malone SA, Shaheen NJ, Asher Prince HM, et al. Single and Multiple Dose Pharmaco-kinetics of Darunavir plus Ritonavir and Etravirine in Semen and Rectal Tissue of HIV-Negative Men. J Acquir Immune Defic Syndr. 2012;61 (2):138–144. doi: 10.1097/QAI.0b013e31825cb645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mardirossian G, Tagesson M, Blanco P, Bouchet LG, Stabin M, Yoriyaz H, et al. A new rectal model for dosimetry applications. J Nucl Med. 1999;40 (9):1524–1531. [PubMed] [Google Scholar]
- 26.Jones A, Talameh J, Patterson K, Rezk N, Prince H, Kashuba ADM. First-Dose and Steady-State Pharmacokinetics of Raltegravir in the Genital Tract of HIV Uninfected Women. 10th International Workshop on Clinical Pharmacology of HIV Therapy; 2009 April 15–17; Amsterdam, The Netherlands. 2009. [Google Scholar]
- 27.Patterson KB, Prince HA, White N, Wang R, Jones A, Kashuba ADM. Pharmacokinetics of Raltegravir in the Blood Plasma and Genital Tract of HIV-positive and HIV-negative Women. XVIII International AIDS Conference; 2010 July 18–23; Vienna, Austria. 2010. [Google Scholar]
- 28.Nicol MR, Kashuba AD. Pharmacologic Opportunities for HIV Prevention. Clin Pharmacol Ther. 2010;88 (5):598–609. doi: 10.1038/clpt.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patterson KB, Prince HA, Kraft E, Jenkins AJ, Shaheen NJ, Rooney JF, et al. Penetration of Tenofovir and Emtricitabine in Mucosal Tissues: Implications for Prevention of HIV-1 Transmission. Science Transl Med. 2011;3 (112):112re4. doi: 10.1126/scitranslmed.3003174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fletcher C, editor. Pharmacologic Analysis of Lymphatic Reservoirs of HIV Infection; Fifth International Conference on HIV Persistence During Therapy; 2011 December 6–9; St. Maarten, West Indies. 2011. [Google Scholar]
- 31.Cohen J HIV/AIDS research. Tissue says blood is misleading, confusing HIV cure efforts. Science. 2011;334 (6063):1614. doi: 10.1126/science.334.6063.1614. [DOI] [PubMed] [Google Scholar]
- 32.Dumond JB, Patterson KB, Pecha AL, Werner RE, Andrews E, Damle B, et al. Maraviroc Concentrates in the Cervicovaginal Fluid and Vaginal Tissue of HIV-Negative Women. J Acquir Immune Defic Syndr. 2009;51 (5):546–553. doi: 10.1097/QAI.0b013e3181ae69c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robbins BL, Nelson SR, Fletcher CV. A novel ultrasensitive LC-MS/MS assay for quantification of intracellular raltegravir in human cell extracts. J Pharm Biomed Anal. 2012;70:378–387. doi: 10.1016/j.jpba.2012.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King T, Bushman L, Kiser J, Anderson PL, Ray M, Delahunty T, et al. Liquid chromatography-tandem mass spectrometric determination of tenofovir-diphosphate in human peripheral blood mononuclear cells. J Chromat B. 2006;843 (2):147–156. doi: 10.1016/j.jchromb.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 35.Deeks SG. HIV: Shock and kill. Nature. 2012;487 (7408):439–440. doi: 10.1038/487439a. [DOI] [PubMed] [Google Scholar]
- 36.Grinsztejn B, Nguyen BY, Katlama C, Gatell JM, Lazzarin A, Vittecoq D, et al. Safety and efficacy of the HIV-1 integrase inhibitor raltegravir (MK-0518) in treatment-experienced patients with multidrug-resistant virus: a phase II randomised controlled trial. Lancet. 2007;369 (9569):1261–1269. doi: 10.1016/S0140-6736(07)60597-2. [DOI] [PubMed] [Google Scholar]
- 37.Markowitz M, Morales-Ramirez JO, Nguyen BY, Kovacs CM, Steigbigel RT, Cooper DA, et al. Antiretroviral activity, pharmacokinetics, and tolerability of MK-0518, a novel inhibitor of HIV-1 integrase, dosed as monotherapy for 10 days in treatment-naive HIV-1-infected individuals. J Acquir Immune Defic Syndr. 2006;43 (5):509–515. doi: 10.1097/QAI.0b013e31802b4956. [DOI] [PubMed] [Google Scholar]
- 38.Murray JM, Emery S, Kelleher AD, Law M, Chen J, Hazuda DJ, et al. Antiretroviral therapy with the integrase inhibitor raltegravir alters decay kinetics of HIV, significantly reducing the second phase. AIDS. 2007;21 (17):2315–2321. doi: 10.1097/QAD.0b013e3282f12377. [DOI] [PubMed] [Google Scholar]
- 39.Gandhi RT, Zheng L, Bosch RJ, Chan ES, Margolis DM, Read S, et al. The effect of raltegravir intensification on low-level residual viremia in HIV-infected patients on antiretroviral therapy: a randomized controlled trial. PLoS Med. 2010;7 (8):e1000321. doi: 10.1371/journal.pmed.1000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hatano H, Hayes TL, Dahl V, Sinclair E, Lee TH, Hoh R, et al. A randomized, controlled trial of raltegravir intensification in antiretroviral-treated, HIV-infected patients with a suboptimal CD4+ T cell response. J Infect Dis. 2011;203 (7):960–968. doi: 10.1093/infdis/jiq138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dinoso JB, Kim SY, Wiegand AM, Palmer SE, Gange SJ, Cranmer L, et al. Treatment intensification does not reduce residual HIV-1 viremia in patients on highly active antiretroviral therapy. PNAS. 2009;106 (23):9403–9408. doi: 10.1073/pnas.0903107106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McMahon D, Jones J, Wiegand A, Gange SJ, Kearney M, Palmer S, et al. Short-course raltegravir intensification does not reduce persistent low-level viremia in patients with HIV-1 suppression during receipt of combination antiretroviral therapy. Clin Infect Dis. 2010;50 (6):912–919. doi: 10.1086/650749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yukl SA, Gianella S, Sinclair E, Epling L, Li Q, Duan L, et al. Differences in HIV burden and immune activation within the gut of HIV-positive patients receiving suppressive antiretroviral therapy. J Infect Dis. 2010;202 (10):1553–1561. doi: 10.1086/656722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ananworanich J, Schuetz A, Vandergeeten C, Sereti I, de Souza M, Rerknimitr R, et al. Impact of multi-targeted antiretroviral treatment on gut T cell depletion and HIV reservoir seeding during acute HIV infection. PLoS One. 2012;7 (3):e33948. doi: 10.1371/journal.pone.0033948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shytaj IL, Norelli S, Chirullo B, Della Corte A, Collins M, Yalley-Ogunro J, et al. A highly intensified ART regimen induces long-term viral suppression and restriction of the viral reservoir in a simian AIDS model. PLoS Pathog. 2012;8 (6):e1002774. doi: 10.1371/journal.ppat.1002774. [DOI] [PMC free article] [PubMed] [Google Scholar]