Abstract
Neuroimaging has gained widespread use in neuropsychological research and practice. However, there are neither established guidelines on how neuropsychologists might become competent researchers or consumers of neuroimaging data, nor any published studies describing the state of neuroimaging training among neuropsychologists. We report the results of two online surveys, one of 13 expert neuropsychologist-neuroimagers, whose responses informed the formulation of a second, larger survey to neuropsychologists-at-large that were a random selection of a third of the members of the International Neuropsychological Society and American Academy of Clinical Neuropsychology. 237 doctoral-level neuropsychologists, or 15.3% of potential participants, provided complete responses. Most respondents (69.2%) received training in neuroimaging, mostly at the post-doctoral level, largely through independent study, clinical conferences, instruction by clinical supervisors, and individualized mentoring, on topics such as neuroimaging modalities in neurology, neuroanatomy, and the appropriate information to glean from neuroradiology reports. Of the remaining respondents who did not receive training in neuroimaging, 64.4% indicated that such training would be very or extremely beneficial to one’s career as a neuropsychologist. Both neuropsychologist-neuroimagers and neuropsychologists-at-large provided specific recommendations for training. Findings from this initial effort will guide trainees who seek to develop competence in neuroimaging, and inform future formulations of neuropsychological training.
Keywords: training, survey, neuroimaging, MRI, neuropsychology
INTRODUCTION
Since its first applications in the late 1970’s, neuroimaging has gained widespread use in clinical practice and research. A cursory search of the term “neuroimaging” in PubMed reveals its exponential growth as evidenced by the number of citations returned per decade: 122 from 1980-1989, 2,955 from 1990-1999, 11,996 from 2000-2009, and already 28,711 since 2010. Albeit not to the same scale, the field of neuropsychology has undergone similarly dramatic changes within the same decades. Certain tasks formerly designated within the expertise of neuropsychology, particularly lesion localization and laterality of function, have been almost entirely supplanted by neuroimaging. The changing landscape of the field is perhaps best highlighted in these statements:
“The historical methods of neuropsychological research have essentially reached their limit as to unraveling of the brain’s role in cognition and behavior. As a clinical and research discipline we need to rapidly incorporate the new technologies.” (Bigler, 1991)
“New imaging technologies have already made some traditional tests redundant, or greatly reduced the frequency with which they are relied upon.” (Baxendale & Thompson, 2010)
“Already structural, diffusion, and resting state functional brain image databases are being assembled on a large scale, enabling for example the use of probabilistic atlases that enable us to apply the same kinds of actuarial approaches to quantifying brain structure that are customary in our inspection of neuropsychological test scores.” (Bilder, 2011)
Nonetheless, the well-established knowledge base of clinical and actuarial inferences derived from neuropsychological approaches will likely thrive alongside the progress of neuroimaging, as implementation of ongoing advances in rehabilitation, forensics, and treatment planning remain important functions of a neuropsychologist. Thus, to optimize the relevance of neuropsychologists in contemporary practice and research settings, competency in neuroimaging should become part of comprehensive training in neuropsychology. Neuropsychologists are uniquely suited to capitalize on applications of neuroimaging, as well-established psychometric measures of cognitive functions are important benchmarks on which neuroimaging techniques and metrics are validated. Indeed, neuropsychologists have integral roles in national Alzheimer’s disease centers, epilepsy services, traumatic brain injury centers, and countless other clinical and research enterprises wherein the assessment or rehabilitation of cognitive function is of paramount interest.
Despite the extent to which the average neuropsychologist is exposed to neuroimaging through clinical or research activities, there are no training standards for the interpretation or application of these findings. There are no published studies on the level of competency neuropsychologists have or need to attain in neuroimaging, much less established curricula for how one might obtain competency, similar to those published for neurologists (Masdeu, 1997). This is likely challenged by ethical guidelines that discourage practicing outside the limits of one’s education and training, particularly since neuroimaging has historically been within the purview of radiology. However, with the availability of functional and structural magnetic resonance imaging (MRI) in clinical care, the trend of decreased reimbursement rates for neuropsychological services (Kanauss, Schatz, & Puente, 2005), and the need for neuropsychological expertise to translate imaging research findings into clinically meaningful concepts, the line between standard neuropsychological practice and proficiency in neuroimaging has blurred significantly. As yet, there have not been any published studies that address the extent to which neuropsychologists have been trained to meet these needs.
One might argue that functional neuroanatomy courses sufficiently cover the information necessary to interpret the behavioral relevance of neuroimaging findings, so additional instruction on magnetic resonance physics, image acquisition, post-processing, and the like, is unnecessary. However, this may result in a tendency to overlook the inherent limitations of these comparatively new techniques (Jones, Knösche, & Turner, 2012; Logothetis, 2008; Poldrack, 2009), and to emphasize neuroimaging findings over inferences derived from decades of neuropsychological research. Neuropsychology is a field concerned with brain-behavior relationships, and it is incumbent upon the field to stay abreast of emerging approaches that characterize brain function and dysfunction. Thus, this study was conceived with two goals: first, to describe the current state of neuroimaging training among a representative sample of neuropsychologists; and second, to combine this information with recommendations from respondents to inform future proposals for the implementation of neuroimaging training.
We conducted two web-based, self-administered surveys. The first survey inquired about the extent of neuroimaging training obtained by neuropsychologists who have established expertise in neuroimaging (hereafter referred to as “neuropsychologist-neuroimagers”). The purpose of this semi-structured survey questionnaire was to ensure that the response options designed by the study investigators were relevant and appropriate, and to solicit opinions and advice from experts who have obtained neuroimaging training in the course of their careers. Based on their responses and input, a second survey was prepared and disseminated to a random sub-sample of members of the American Academy of Clinical Neuropsychology (AACN) and the International Neuropsychological Society (INS). The results herein summarize the extent of neuroimaging training among the respondents and list the specific training resources they recommend.
METHODS
The surveys were designed by the study investigators and were administered using REDCap (http://www.project-redcap.org/), an NIH-funded secure web application created to support secure data capture for research studies initiated by participating institutions. Study procedures were approved by the Medical University of South Carolina Institutional Review Board. The survey responses of the neuropsychologist-neuroimagers were collected from June 1 to 20, 2012, while the survey responses of neuropsychologists-at-large were collected from September 5 to 19, 2012.
Participants
For the survey of neuropsychologist-neuroimagers, the study investigators first independently generated a list of neuropsychologists with established expertise in applying neuroimaging to their clinical or research activities, then developed a final list following consensus agreement. Seventeen North American neuropsychologist-neuroimagers were contacted directly via email and provided with a link to the survey. Respondents were given the option to disclose their name and email address should they consent to be contacted again by the investigators for further questions or consultation.
For the survey of neuropsychologists-at-large, the authors obtained the e-mail addresses of North American members of the AACN and INS who possessed a doctoral degree (i.e., Ph.D., Psy.D., or Ed.D.), using the organizations’ online membership rosters that were accessible in August 2012. Figure 1 summarizes the process of respondent selection. Briefly, one-third of the members of both organizations were randomly selected, and this subset was reviewed to eliminate duplicate respondents due to being members of both AACN and INS (n=66) and to omit individuals who participated in the survey of neuropsychologist-neuroimagers (n=6). 1,772 individuals were contacted via REDCap and 222 emails returned as undeliverable, resulting in 1,550 viable respondents.
Figure 1.
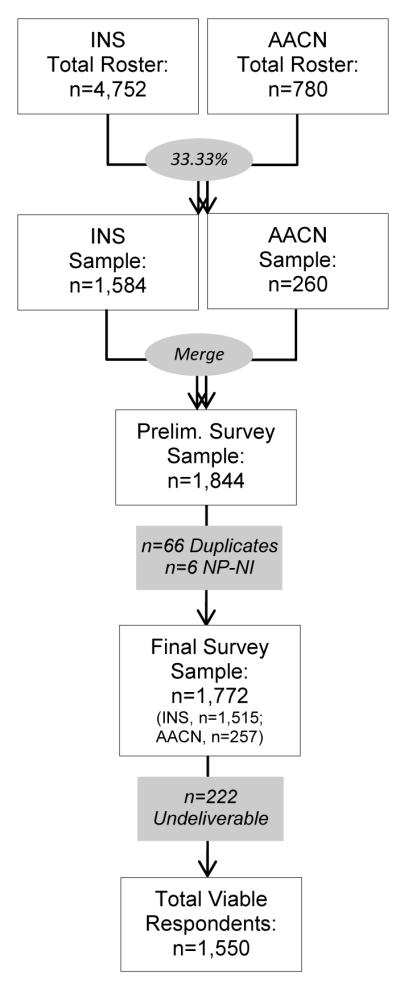
Flow diagram of the process of identifying the sample for the survey of neuropsychologists-at-large. Note: AACN=American Academy of Clinical Neuropsychology, INS=International Neuropsychological Society, NP-NI=Neuropsychologists-neuroimagers.
Measures
The web-based surveys were composed of close-ended questions with dichotomous or polytomous response options. For certain questions, respondents were prompted to provide an estimated percent of time (up to 100) spent on a particular activity or in a specific setting. Branching logic for contingency questions were also included. For example, if a respondent endorsed not having received training in neuroimaging, associated questions were not administered to these respondents. After completing the structured survey questions, respondents were given the option to respond to open-ended questions. With the exception of open-ended questions and questions that were not prompted by branching logic, all forced-choice fields were programmed to require responses for the survey to be considered “complete,” thereby eliminating the possibility of missing data. The surveys had two general sections:
Informed consent and review of inclusion criteria
Informed consent was obtained through a detailed description of the study that preceded the survey questions, which included disclosure of minimal risks (e.g., loss of time) and measures to ensure confidentiality; potential participants were assured that no identifiers would be attached to their responses. Responses were downloaded directly from the survey website to a secure database, which prevented data entry errors. Respondents were informed of the inclusion criteria: primary location of residence/employment in North America and possession of a doctoral degree.
Survey proper
The survey included questions that were divided into three thematic sections: (a) Personal information and training history: Gender, race/ethnicity, age-range, percent of time dedicated to clinical and research activities in one’s training; (b) Workplace setting and activities: Current board certifications, nature of employment and departmental affiliation, and percent time dedicated to clinical and research activities in one’s training; (c) Neuroimaging training: Types of training received and when these occurred, content areas covered; and (d) Recommendations for how and at what point in training in neuropsychology should neuroimaging training occur. The complete surveys are provided as Supplementary Material.
Procedures
For both surveys, each potential participant was sent an email invitation via REDCap with a unique survey link to a brief 5-10 minute online survey on neuroimaging training as previously described. A reminder e-mail was sent to potential participants one week after the first invitation to enhance response rates and to thank those who have already responded. Respondents were given two weeks to complete the survey. At the conclusion of the surveys, respondents were offered the opportunity to obtain a summary of this study’s findings as compensation; no monetary incentive was offered. Confidentiality was ensured by specifying REDCap settings so that no identifiable information could be collected from respondents or their computers, and the e-mail list of society members and of potential participants in this study were securely deleted after the initial and reminder emails were sent. As the purpose of this study was to first provide an overview of neuroimaging training among neuropsychologists, only parametric and non-parametric descriptive statistics are reported here. All analyses were performed using IBM SPSS Statistics version 20 (Armonk, NY).
RESULTS
Survey of Neuropsychologist-Neuroimagers
Survey invitations were sent to 17 neuropsychologist-neuroimagers, 13 of whom provided complete responses. These respondents were mostly male (69.2%), white (92.3%), and had obtained their Ph.D. (92.3%) from an American Psychological Association (APA) accredited doctoral program (76.9%) in clinical neuropsychology (46.2%), clinical psychology (38.5%), or experimental psychology (15.3%). The respondents represented a broad range of years of experience, with approximately half (54.8%) endorsing 16 or more years since obtaining their doctorate. Six were board certified (5 through American Board of Professional Psychology-Clinical Neuropsychology [ABPP-CN], 1 through the American Board of Professional Neuropsychology [ABN]). All were employed in an academic medical center, with some reporting affiliations with university (30.8%) or a VA hospital (15.4%). All engage in research, at reportedly an average of 65.4% (SD=29.7%) of the time, while only seven of the 13 respondents endorsed having a clinical practice at an average time effort of 19.3% (SD=19.9%).
All neuropsychologist-neuroimagers endorsed using MRI in their professional activities (structural MRI, 100%; functional and diffusion MRI, 92.3%; arterial spin labeling (ASL), 53.8%), with fewer endorsing the use of magnetic resonance spectroscopy (38.5%), positron emission tomography (PET; 30.8%), and electroencephalography/event-related potentials (EEG/ERP; 15.4%). They obtained training through independent study (100%), individual mentoring (92.3%), attendance of brief workshops (69.2%) and clinical conferences (53.8%), formal coursework at the post-graduate level (38.5%), web tutorials (38.5%), lab assistantships (30.8%), and formal coursework in graduate school (7.7%). In this survey, the study investigators presented the neuropsychologist-neuroimager respondents with options representing the content areas covered during their training, and specific knowledge and skills they deemed necessary to become a competent researcher or consumer of neuroimaging data. Their selection of the provided survey options informed the design of the most appropriate and relevant item response options for the subsequent survey of neuropsychologists-at-large.
Survey of Neuropsychologists-at-Large
An invitation to participate in the survey was emailed to 1,550 potential participants. Surveys completed within two weeks of the initial email invitation were included in the analyses. 237 respondents completed the survey, representing a 15.3% response rate. While modest, this survey’s response rate is comparable to the proportion of respondents in a previously published survey of neuropsychological practices and perspectives regarding the assessment of judgment ability (17%; Rabin, Borgos, & Saykin, 2008) which also did not offer direct compensation to its respondents.
The respondents were mostly white (94.9%), female (51.5%), and recipients of a Ph.D. (87.3%) from an APA/CPA-accredited doctoral program (86.9%). Slightly more than half of the respondents received their degree in clinical psychology (51.9%), while the rest received their degrees in clinical neuropsychology (28.3%), counseling psychology (7.6%), experimental psychology (3.0%), neuroscience/physiological psychology (2.5%), educational psychology (1.3%), school psychology (1.3%), or other (4.2%). The respondents represent a wide range of years of professional experience since obtaining their doctorate: 0-5 years (17.3%), 6-10 years (24.5%), 11-15 years (14.8%), 16-20 years (13.1%), 21-25 years (13.5%), and 25 and more years (16.9%). Several respondents (41.8%) were board certified by ABPP, mostly in Clinical Neuropsychology (n=87). Expectedly, most respondents endorsed membership in INS (88.6%) and AACN (43.5%), but also endorsed being members of APA Division 40 (66.2%), National Academy of Neuropsychology (56.1%), and other neuropsychological organizations (13.1%).
The majority of respondents endorsed completing training that was consistent with Houston Conference guidelines including specialized training in clinical neuropsychology in the scientist-practitioner model at some level in their training (doctoral [76.9%], internship [83.1%], post-doctoral [81.0%]), with many having been trained in an academic medical center (Table 1). Table 2 summarizes the activities and the settings in which the respondents were currently employed. The respondents mostly reported their departmental affiliations to be in psychiatry/mental health/behavioral sciences, psychology, or neurology. Respondents reported a wide range of ages on which they focus their clinical and research endeavors, but most respondents endorsed primarily working with adults. A relatively large proportion of respondents endorsed working in an academic medical center or a VA Hospital. Almost all respondents reported engaging in clinical practice, and the majority of professional effort reported (in % of weekly time in hours) was dedicated to clinical activities.
Table 1.
Settings in which respondents received their training (N=237).
| Doctoral Program |
Internship Program |
Post-doctoral Fellowship |
|
|---|---|---|---|
|
|
|||
| n (%) | n (%) | n (%) | |
| Training Setting | |||
| Academic medical center | 141 (59.5) | 141 (59.5) | 159 (67.1) |
| Private practice | 57 (24.1) | 4 (1.7) | 22 (9.3) |
| Rehabilitation facility | 62 (26.2) | 31 (13.1) | 33 (13.9) |
| University setting (psychology department clinic) |
181 (76.4) | 25 (10.5) | 22 (9.3) |
| Veterans Administration Hospital | 66 (27.8) | 75 (31.6) | 35 (14.8) |
| Other | 39 (16.5) | 34 (14.3) | 15 (6.3) |
| Not applicable | -- | -- | 19 (8.0) |
Table 2.
Characteristics of respondents’ workplace and activities (N=237).
| n (%) | |
|---|---|
| Board Certification | |
| ABPP-Clinical Neuropsychology | 87 (36.7) |
| ABPP-Clinical Psychology | 4 (1.7) |
| ABPP-Rehabilitation Psychology | 6 (2.5) |
| ABN | 8 (3.4) |
| ABPP-Other | 2 (0.8) |
| AAPN | 1 (0.4) |
| Other | 11 (4.6) |
| Department of Current Appointment | |
| Psychiatry/Mental Health/Behavioral Sciences | 91 (38.4) |
| Psychology | 65 (27.4) |
| Neurology | 49 (20.7) |
| Rehabilitation | 30 (12.7) |
| Neurosciences | 19 (8.0) |
| Pediatrics/Child Development/Child Studies | 12 (5.1) |
| Geriatrics/Gerontology | 5 (2.1) |
| Education | 2 (0.8) |
| Oncology | 2 (0.8) |
| Radiology | 1 (0.4) |
| Other | 22 (9.3) |
| Developmental Period of Patients of Interest | |
| Adult | 202 (85.2) |
| Geriatric | 161 (67.9) |
| Adolescent | 112 (47.3) |
| Pediatric | 82 (34.6) |
| Current Work Setting (Mean and SD of % time effort) | |
| Academic medical center (M=77.48%, SD=34.62; range 1-100) | 104 (43.9) |
| Private practice (M=75.60%, SD=31.94; range 5-100) | 73 (30.8) |
| VA hospital (M=88.62%, SD=17.28; range 50-100) | 29 (12.2) |
| University setting (e.g. psychology department) (M=70.16%, SD=36.48; range 5-100) |
25 (10.5) |
| Rehabilitation facility (M=73.65%, SD=35.30; range 1-100) | 23 (9.7) |
| Other (M=76.78%, SD=33.51; range 0-100) | 45 (19.0) |
| Weekly Activities (Mean and SD of % time) | |
| Clinical practice (M=65.44%, SD=29.05; range 5-100) | 215 (90.7) |
| Supervision or training (M=12.53%, SD=8.46; range 2-45) | 161 (67.9) |
| Research (M=29.28%, SD=27.23; range 5-100) | 140 (59.1) |
| Administrative (M=16.04%, SD=16.00; range 2-100) | 140 (59.1) |
| Teaching in a classroom/lecture (M=12.69%, SD=14.17; range 1-70) |
62 (26.2) |
Note: ABPP=American Board of Professional Psychology; ABN=American Board of Professional Neuropsychology; AAPN=American Academy of Pediatric Neuropsychology.
Prior training in neuroimaging
A minority of respondents (n=73, 30.8%) reported that they never received any formal or informal training in neuroimaging. Of these respondents, most deemed that neuroimaging training would be (marginally [32.9%], very [46.6%], extremely [17.8%]) beneficial to one’s career as a neuropsychologist, whereas two respondents endorsed that such training would not at all be beneficial. The remaining 164 respondents mostly endorsed receiving their neuroimaging training at the post-doctoral level (80.5%), followed by the pre-doctoral level (53.0%), post-training level (49.4%), and internship level (40.2%).
Table 3 summarizes the type of formal and informal neuroimaging training received, and the content areas covered during these experiences. The majority of respondents obtained their training through independent reading and study, clinical conferences, instructions by clinical supervisors, and individual mentoring or training. The respondents received their training through options that were unique to the institutions in which they obtained their training, such as grand rounds (neurology, psychiatry, neuroradiology, neuroscience), case conferences, medical school courses, specific lectures such as neuropathology brain dissection, involvement in a research project, supervision by a neuropsychologist-neuroimager, close interactions with a colleague with expertise in neuroimaging, and review of patient scans through electronic medical records. The most frequently endorsed topics covered during neuroimaging training experiences included: neuroimaging modalities used in clinical neurology settings, neuroanatomy, and knowing what information to glean from neuroradiology reports.
Table 3.
Types of training and content areas covered during neuroimaging training experiences (n=164).
| n (%) | |
|---|---|
| Types of neuroimaging training received | |
| Independent reading and study | 132 (80.5) |
| Clinical conferences, discussion of patient neuroimaging data | 131 (80.0) |
| Instruction by a clinical supervisors on including information from neuroradiology reports in clinical neuropsychology reports |
113 (68.9) |
| Individual mentoring/training by expert | 110 (67.1) |
| Intensive, brief workshop/training | 65 (39.6) |
| Lab-based (assistantship) | 50 (30.5) |
| Formal coursework (grad school) | 42 (25.6) |
| Formal coursework (post-grad) | 36 (22.0) |
| Web-based tutorials | 22 (13.4) |
| Other | 16 (9.8) |
| Content areas covered during neuroimaging training experiences | |
| Basic knowledge of neuroimaging modalities used in neurology | 150 (91.5) |
| Neuroanatomy | 146 (89.0) |
| Specific types of information to glean from neuroradiology reports | 136 (82.9) |
| Magnetic resonance physics | 104 (63.4) |
| Experimental design (for fMRI, PET) | 89 (54.3) |
| Image acquisition | 75 (45.7) |
| Stimulus presentation software | 66 (40.2) |
| Preprocessing and analysis | 60 (36.6) |
| Hemodynamics | 58 (35.4) |
| Biochemistry | 51 (31.1) |
| Contrast agents | 49 (29.9) |
| Ethical use of neuroimaging | 41 (25.0) |
| Other | 3 (1.8) |
Note: fMRI=Functional Magnetic Resonance Imaging; PET=Positron Emission Tomography.
Current use of neuroimaging in professional activities
Of the respondents surveyed, 90 (38.3%) reported using neuroimaging in their professional activities, although it must be noted that a definition of the term “use” was not provided in the survey. These respondents were not significantly different from the other respondents in terms of race, degree type, degree specialization, or years of experience following receipt of one’s degree, except they were more likely to be male, χ2(1, 238)=5.19, p<0.05, similar to the neuropsychologist-neuroimagers surveyed. Of this sub-sample, 41.1% use neuroimaging for both clinical and research purposes, while 31.1% and 27.8% use neuroimaging for clinical or research purposes, respectively. Thus, out of the 90 respondents who reported using neuroimaging in professional activities, as many as 72.2% report using neuroimaging for clinical purposes. The modalities used in descending order of endorsement frequency were: structural MRI (92.2%), functional MRI (53.3%), diffusion MRI (51.1%), PET (47.8%), EEG/ERP (38.9%), single-photon emission computed tomography (SPECT; 25.6%), ASL (15.6%), neurostimulation (14.4%), magnetic resonance spectroscopy (10.0%), magnetoencephalography (5.6%), optical imaging (4.4%), or other (6.7%). Interestingly, of these 90 respondents, 12.2% indicated that they had not received any formal or informal instruction in neuroimaging in their training.
Recommendations for neuroimaging training
The majority of respondents (60.8%) indicated that it is very important that neuropsychologists receive training in neuroimaging, while 32.5% endorsed it as somewhat important, and a minority endorsed that it was neither unimportant nor important (3.4%) or somewhat unimportant (3.4%). In terms of when this training should occur, the respondents recommended all levels of training: post-doctoral (76.8%), pre-doctoral (60.3%), internship (59.1%), and post-training (38.8%). Respondents were given the option to volunteer courses, workshops, and other resources that they found helpful in educating themselves in neuroimaging. Ninety respondents provided responses to this open-ended query, which we reviewed and summarized in a table that lists widely available resources (Table 4).
Table 4.
Recommended training resources.
|
Online Resources and Textbooks Harvard University Whole Brain Atlas (http://www.med.harvard.edu/aanlib/home.html) Wayne State University Radiologic Anatomy (http://www.med.wayne.edu/diagradiology/anatomy_modules/brain/brain.html) Neuroanatomy Through Clinical Cases (Blumenfeld, 2010) Clinical Magnetic Resonance Spectroscopy: Techniques and Applications (Barker, 2010) Workshops BRAINS Camp, University of Iowa Functional Magnetic Resonance Imaging (fMRI) workshop, University of Michigan (http://sitemaker.umich.edu/fmri.training.course/home) Functional Magnetic Resonance Imaging (fMRI) workshop, Medical College of Wisconsin Harvard-Massachusetts General Hospital Martinos Center (http://www.nmr.mgh.harvard.edu/martinos/training/index.php) Neuroimaging software workshops (Analysis of Functional NeuroImages [AFNI], Analyze, FMRIB Software Library [FSL], FreeSurfer, Statistical Parametric Mapping [SPM]) National Institute of Mental Health (NIMH) Summer Institute in Cognitive Neuroscience Workshops in conferences (National Academy of Neuropsychology, International Neuropsychological Society, American Society for Functional Neuroradiology, Organization for Human Brain Mapping, International Society for Magnetic Resonance in Medicine) |
DISCUSSION
The purpose of this study was to describe the current state of neuroimaging training among neuropsychologists, and to provide recommendations for training through a survey of members of two large neuropsychological organizations (N=237). Over two-thirds of the respondents endorsed receiving formal or informal neuroimaging training, mostly at the post-doctoral level, largely through independent reading and study, clinical conferences, instruction by clinical supervisors, and individualized mentoring or training, with instruction more frequently focused on topics such as neuroimaging modalities in clinical neurology settings, neuroanatomy, and the appropriate information to glean from neuroradiology reports. These results indicate that most neuropsychologists receive some form of instruction in neuroimaging for what appears to be most pertinent to clinical applications. This likely reflects that most of the respondents endorsed engaging in clinical practice, at the highest average proportion of effort compared to other activities. However, several respondents also endorsed receiving more detailed instruction in neuroimaging, suggesting that direct clinical application is not the only purpose for which training in neuroimaging is obtained.
A noteworthy finding is that a considerable sub-sample of respondents (38.3%) endorsed using neuroimaging, predominantly structural MRI, in their professional activities. This may reflect the increasing trend for neuroimaging to be part of neuropsychological practice and research, and perhaps the growing interest in obtaining skills in this area among people in the field, even among those who had not received any formal or informal instruction in neuroimaging during their training. Indeed, while a minority of respondents (30.8%) endorsed not having received any formal or informal training in neuroimaging, two-thirds of these respondents indicated that such training would be very or extremely beneficial to one’s career as a neuropsychologist. Thus, obtaining training in neuroimaging for potential application to one’s clinical or research endeavors may be a significant need that training programs may have to address.
Although the majority of respondents endorsed that neuroimaging training is important and useful, no established guidelines exist for neuroimaging training among neuropsychologists. Findings from the present study suggest that such instruction should perhaps occur at multiple levels of training, including during both pre-doctoral and post-doctoral training, and also possibly after formal training has been completed. The respondents provided a variety of existing resources including websites, textbooks, and formal workshops that may be particularly useful components of neuroimaging training (see Table 4). In addition, a recent special issue of the journal NeuroRehabilitation focused on neuroimaging applications that may be particularly relevant to those with interest in rehabilitation settings. This special issue also includes a primer on neuroimaging and, although some of the content is focused on applications to rehabilitation settings, it may be a useful primer for neuropsychologists more broadly, including those working in other settings (Wilde, Hunter, & Bigler, 2012).
Neuropsychologists, due to their unique combination of training that covers many aspects of clinical psychology, psychometrics, neuroscience, and cognitive psychology, among others, are in an excellent position to inform task design in functional neuroimaging studies such as fMRI. Many classic fMRI tasks including N-back and Stroop were not necessarily designed with clinical populations in mind and were not intended to detect treatment effects or disease-related decline. Indeed, knowledge of brain-behavior relationships and brain disorders are essential for design of tasks intended to elicit a brain response (Amaro & Barker, 2006). Translation of a behavioral task that is well known to clinical neuropsychologists, say the Trailmaking test, may not be practical for functional imaging paradigms. At this level, neuropsychology training could play a critical role in deconstructing this task into basic components of visual processing, attention, and psychomotor skills to develop an fMRI-appropriate task that adequately reflects these core cognitive processes. In addition, neuropsychologists have specialized knowledge of cognitive strengths and weaknesses of clinical populations that could inform task design to make an efficient and statistically powerful task that maximizes detection of effects of interest while minimizing participant burden. This is an example of how instruction or training in neuroimaging might prepare neuropsychologists to provide a unique contribution to the development of meaningful functional paradigms.
This study also introduces several questions for future consideration, as extensions of this initial effort or as a formalized discourse among neuropsychologists at a national or international level. For instance, although neuroimaging is listed as a topic under the requirement of education on brain-behavior relationships, to what extent should the current or future Houston Conference guidelines accommodate competence in neuroimaging? Should an appropriate level of competence in neuroimaging be required in preparation for board certification? And what would constitute an “appropriate” level of competence befitting a neuropsychologist? Although these questions are beyond the scope of this manuscript, we encourage individuals at all levels pre- and post-training to consider the possibilities introduced here, given the undeniable ubiquity of neuroimaging in neuropsychological practice and research. In the meantime, it is hoped that these recommendations will be helpful to current trainees interested in obtaining competence as a consumer of clinical or research neuroimaging data, and also contribute to current conceptualizations of neuroimaging training that can be implemented across different training programs and settings.
This study has the following limitations. First, as with any survey study, the conclusions from this study are limited to the sample from which the results are derived, and only reflect the experiences and opinions of the particular respondents to this survey. However, we provided an ample description of the survey sample to provide a framework for evaluating our study results. Furthermore, we have reason to believe that the survey respondents are reasonably representative of neuropsychologists-at-large. In the recent “salary survey” of neuropsychologists that had a large response rate (56%; Sweet, Meyer, Nelson, & Moberg, 2011), the proportion of their respondents mostly endorsed having a Ph.D. (82.5%), were female (52.8%), white (89.9%), and board certified by ABPP (35.1%), not unlike the survey respondents in this study (i.e., 87.3% Ph.D., 51.5% female, 94.9% white, and board certified 41.8%), one difference being that the 74.0% respondents in the salary survey obtained their degree in the field of clinical psychology in contrast to just 51.9% in our study. As previously mentioned, the relatively modest response rate in this study is at least comparable to the number of respondents in a previously published survey which also did not offer direct compensation to its respondents (Rabin et al., 2008).
Second, using the results from a survey of largely academic neuropsychologistneuroimagers to inform the response options for the survey of the neuropsychologists-at-large may have biased the survey construction towards more academically-oriented pursuits and content areas. But since potential neuroimaging training will most likely have to be obtained in academic medical centers, we believe these response options are representative of the options available to trainees, many of whom already obtain at least part of their training in these contexts. Third, some survey questions were ambiguously worded and may have been interpreted differently by respondents. For instance, the “use” of neuroimaging in one’s clinical activities may or may not have been deemed as encompassing a relatively routine practice of reviewing and incorporating neuroradiology results in one’s report. Thus, such terms should be operationally defined in future efforts to fully characterize the extent neuroimaging modalities and the data these provide are adopted in neuropsychological research and practice. Lastly, this study is descriptive and does not report inferential statistics that can identify possible bias in respondent background, training, preferences, etc. that may modify our conclusions, as we were not privy to any data from non-respondents with which comparisons could be made. Future work with a larger sample could build on the work described here, specifically including queries and response options with which direct hypotheses can be tested.
In spite of these limitations, to our knowledge this is the first focused study of this issue that identifies the contexts and content areas in which neuropsychologists receive their neuroimaging training, the prevalence of the use of neuroimaging in professional neuropsychological practice and research, and the perception of the value of neuroimaging training, even among neuropsychologists with minimal or no experience with neuroimaging. Overall, the survey results indicate that while most neuropsychologists have at least some exposure to neuroimaging training, a not inconsequential proportion of respondents endorsed having no formal or informal instruction in neuroimaging, even among neuropsychologists who use neuroimaging in their professional activities. Nonetheless, the vast majority of those surveyed considers such training as essential to competently function as neuropsychologists in the current research and clinical climate in which neuroimaging is increasingly gaining importance. We hope that the information reported here will provide those involved in neuropsychology at all levels of training with useful options should they decide to pursue additional training in neuroimaging, and help define the appropriate training necessary to meet the changing landscape of neuropsychological research and clinical care.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank Drs. Erin Bigler and Robert Bilder for their assistance and encouragement in the early stages this project, and our Reviewers who provided insightful suggestions to enhance our paper’s impact and relevance. We would also like to thank Adam Spandorfer for his assistance in the survey preparation during his summer research experience at MUSC in 2012.
This project was conducted using REDCap (NIH/NCATS UL1TR000062). The authors were supported by the National Institutes of Health (Dr. Benitez SCTR UL1 TR000062 & KL2 TR000060; Dr. Hassenstab K23 DK094982; Dr. Bangen T32 MH1993417).
Footnotes
Preliminary analyses of some of these data were presented at the 41st Annual Meeting of the International Neuropsychological Society, February 6-9, 2013; Waikoloa, HI.
REFERENCES
- Amaro E, Jr, Barker GJ. Study design in fMRI: basic principles. Brain and cognition. 2006;60(3):220–232. doi: 10.1016/j.bandc.2005.11.009. doi:10.1016/j.bandc.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Barker PB. Clinical MR spectroscopy: techniques and applications. Cambridge University Press; Cambridge: 2010. [Google Scholar]
- Baxendale S, Thompson P. Beyond localization: the role of traditional neuropsychological tests in an age of imaging. Epilepsia. 2010;51(11):2225–2230. doi: 10.1111/j.1528-1167.2010.02710.x. doi:10.1111/j.1528-1167.2010.02710.x. [DOI] [PubMed] [Google Scholar]
- Bigler ED. Neuropsychological assessment, neuroimaging, and clinical neuropsychology: a synthesis. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists. 1991;6(3):113–132. [PubMed] [Google Scholar]
- Bilder RM. Neuropsychology 3.0: evidence-based science and practice. Journal of the International Neuropsychological Society: JINS. 2011;17(1):7–13. doi: 10.1017/S1355617710001396. doi:10.1017/S1355617710001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenfeld H. Neuroanatomy through clinical cases. 2nd ed Sinauer Associates, Inc; Sunderland, MA: 2010. [Google Scholar]
- Jones DK, Knösche TR, Turner R. White matter integrity, fiber count, and other fallacies: The do’s and don’ts of diffusion MRI. NeuroImage. 2012 doi: 10.1016/j.neuroimage.2012.06.081. doi:10.1016/j.neuroimage.2012.06.081. [DOI] [PubMed] [Google Scholar]
- Kanauss K, Schatz P, Puente AE. Current trends in the reimbursement of professional neuropsychological services. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists. 2005;20(3):341–353. doi: 10.1016/j.acn.2004.09.002. doi:10.1016/j.acn.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Logothetis NK. What we can do and what we cannot do with fMRI. Nature. 2008;453(7197):869–878. doi: 10.1038/nature06976. doi:10.1038/nature06976. [DOI] [PubMed] [Google Scholar]
- Masdeu JC. American Academy of Neurology neuroimaging training guidelines. The AAN Workshop on Neuroimaging Training. Neurology. 1997;49(6):1738–1740. doi: 10.1212/wnl.49.6.1738. [DOI] [PubMed] [Google Scholar]
- Poldrack RA. [Retrieved March 22, 2013];Neuroimaging: Separating the Promise from the Pipe Dreams - Dana Foundation. 2009 May 27; from http://www.dana.org/news/cerebrum/detail.aspx?id=22220.
- Rabin LA, Borgos MJ, Saykin AJ. A survey of neuropsychologists’ practices and perspectives regarding the assessment of judgment ability. Applied neuropsychology. 2008;15(4):264–273. doi: 10.1080/09084280802325090. doi:10.1080/09084280802325090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet JJ, Meyer DG, Nelson NW, Moberg PJ. The TCN/AACN 2010 “salary survey”: professional practices, beliefs, and incomes of U.S. neuropsychologists. The Clinical neuropsychologist. 2011;25(1):12–61. doi: 10.1080/13854046.2010.544165. doi:10.1080/13854046.2010.544165. [DOI] [PubMed] [Google Scholar]
- Wilde EA, Hunter JV, Bigler ED. A primer of neuroimaging analysis in neurorehabilitation outcome research. NeuroRehabilitation. 2012;31(3):227–242. doi: 10.3233/NRE-2012-0793. doi:10.3233/NRE-2012-0793. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


