Abstract
The authors of this study evaluated a structured 10-session psychosocial support group intervention for newly HIV-diagnosed pregnant South African women. Participants were expected to display increases in HIV disclosure, self-esteem, active coping and positive social support, and decreases in depression, avoidant coping, and negative social support. Three hundred sixty-one pregnant HIV-infected women were recruited from four antenatal clinics in Tshwane townships from April 2005 to September 2006. Using a quasi-experimental design, assessments were conducted at baseline and two and eight months post-intervention. A series of random effects regression analyses were conducted, with the three assessment points treated as a random effect of time. At both follow-ups, the rate of disclosure in the intervention group was significantly higher than that of the comparison group (p < 0.001). Compared to the comparison group at the first follow-up, the intervention group displayed higher levels of active coping (t = 2.68, p < 0.05) and lower levels of avoidant coping (t = −2.02, p < 0.05), and those who attended at least half of the intervention sessions exhibited improved self-esteem (t = 2.11, p < 0.05). Group interventions tailored for newly HIV positive pregnant women, implemented in resource-limited settings, may accelerate the process of adjusting to one's HIV status, but may not have sustainable benefits over time.
Keywords: HIV/AIDS, mental health, pregnancy, psychosocial, social support
Introduction
Sub-Saharan Africa continues to share a disproportionate percentage of global HIV infections, with an estimated 68% of all people living with HIV/AIDS located in the region (UNAIDS, 2010). South Africa, the country most severely affected by the epidemic, has approximately 5.6 million HIV-infected people (UNAIDS, 2010). Women account for an estimated 58% of all HIV infections in South Africa (UNAIDS, 2010), and the risk of infection for women between the ages of 20 and 29 years is almost six times that of males in the same age group (Rehle et al., 2007). Approximately 29% of all pregnant women in South Africa are HIV-infected (Department of Health, 2009).
The need to explore novel and culturally relevant support intervention strategies has become a growing necessity. South Africa has a significant and unmet need among HIV-infected women for adequate psychosocial support (Olley et al., 2003; Moultrie & Kleintjes, 2006). This need is exacerbated by the fact that people living with HIV, who experience a wide array of psychosocial stressors, now also have improved longevity, due to recent advances in treatment (Scott–Sheldon et al., 2008).
With the continual improvement of prevention of mother-to-child transmission (PMTCT) programs (Stringer et al., 2008), women in developing countries, such as South Africa, are increasingly discovering their HIV status during pregnancy. Pregnancy itself is a stressful and demanding life event (Geller, 2004), and the news of HIV-infection during this period can be devastating for a pregnant woman, potentially affecting her ability to cope (Blaney et al., 2004), the outcome of her pregnancy (Alder et al., 2007; Psaros, Geller, & Aaron, 2009) and her functioning as a parent. The increasing number of women who are discovering their HIV status during pregnancy, coupled with the related amplified need for support, makes pregnancy a logical entry point for psychosocial intervention.
The Psychosocial Needs of Pregnant HIV-Infected Women
Not enough emphasis has been placed in sub-Saharan Africa on the development of care and support interventions (Amon, 2002) and the provision of psychosocial support for those infected (Skinner & Mfecane, 2004), particularly for low-income HIV positive women (Ironson et al., 2005). In addition, research on the psychological aspects of having HIV during pregnancy has been limited (Sanders, 2008).
HIV presents a multitude of diverse stresses that can negatively affect pregnant women's mental well being (Plattner & Meiring, 2006; Amuyunzu–Nyamongo et al., 2007) but despite this, the psychosocial consequences of HIV have often been under-diagnosed and under-treated (Ironson et al., 2005). In a meta-analysis of 23 studies conducted in Africa, Brandt (2009) showed a significant association between HIV and mental illness, with depression the most frequently reported individual problem.
Depression has been shown to directly compromise the immune system, which may accelerate disease progression (Evans, Ten–Have, & Douglas, 2002; Chida & Vedhara, 2009) and have negative repercussions for a pregnancy, while positive affect (Moskowitz, 2003) and high self-esteem (Ironson et al., 2005) have been associated with decreased disease progression. A meta-analysis on depression during pregnancy (Ryan, Mills, & Misri, 2005) concluded that, left untreated, mental distress can negatively affect birth outcomes and neonatal health, and lead to post-partum depression, which can in turn affect mother-infant attachments, potentially resulting in negative consequences for child development.
In addition, a growing body of literature from developing countries has shown the close relationship that exists between maternal mental health and children's growth, development and morbidity (Patel, DeSouza, & Rodrigues, 2003; Rahman et al., 2004; Harpham et al., 2005; Rahman et al., 2007; Adewuya, Ola, Aloba, et al., 2008). Psychosocial intervention decreases mental distress during pregnancy (Spinelli, 1997) and reduces the risk of post-partum depression (Dennis & Creedy, 2004).
Coping with the Psychosocial Effects of HIV Infection
The psychosocial impact of HIV infection on women can be diminished through the effective utilization of various psychosocial resources, such as social support, optimism and adaptive coping strategies (Gurung et al., 2004; Chida & Vedhara, 2009). HIV-positive women often lack adequate social support (Morrow, Costello, & Boland, 2001) and difficulty in disclosing one's HIV status is frequently a barrier to seeking support. For a number of reasons, such as the fear of abandonment, stigma, and violence, disclosure continues to be a complicated task for women (Makin et al., 2008; Visser et al., 2008). However, knowing someone living with HIV can assist in the difficult process of disclosure (Makin et al., 2008). Despite this, there is presently little empirical support that support groups enhance disclosure for women.
Support Groups
A pressing need exists within sub-Saharan Africa for the development and assessment of support interventions (Simbayi et al., 2007). Three recent meta-analyses, which helped examine the effectiveness of psychosocial interventions for people living with HIV, have confirmed various effects associated with participation in such interventions, including significant reductions in anxiety, depression, psychological distress, stress and anger, and improvements in coping skills and quality of life (Himelhoch, Medoff, & Oyeniyi, 2007; Crepaz et al., 2008; Scott–Sheldon et al., 2008). People attending support groups are more likely to disclose their HIV status than those who do not attend support groups (Kalichman et al., 1996). Support groups provide HIV-positive people with a safe environment to talk about HIV, share their experiences, and listen to the stories of others who are in a similar position (Summers et al., 2000).
Participants benefit most from interventions with ten sessions or more, as they then have the opportunity to reinforce the skills and knowledge that are acquired (Crepaz et al., 2008). In addition, interventions with sessions of 90 minutes in duration and with content specifically tailored to improve coping strategies and to improve social support, were the most successful for people living with HIV (Himelhoch et al., 2007).
In addition to outlining the major successes of support interventions, authors of recent meta-analyses have consistently identified two primary limitations of studies in this field of HIV research. First, very few studies have extended follow-up observations further than immediate post-intervention assessments, making it difficult to determine whether the effects of such interventions are sustainable over time (Himelhoch et al., 2007; Crepaz et al., 2008; Scott–Sheldon et al., 2008). Second, a limitation identified in previous research is that most of the studies have been conducted in the United States, primarily among the gay male population (Himelhoch et al., 2007; Crepaz et al., 2008), with very few studies conducted in developing countries and among women, where and in whom the need for such research is in fact the greatest (Scott–Sheldon et al., 2008).
Study Purpose
In this study, a structured psychosocial support group intervention, tailored to meet the specific needs of pregnant South African women recently diagnosed HIV positive, was evaluated. Using a quasi-experimental design, psychosocial variables were assessed at baseline and at two and eight months post-intervention. Compared to women who did not take part in the intervention, it was hypothesized that participation in the intervention would significantly increase levels of disclosure, self-esteem, active coping and positive social support, as well as decrease levels of depression, avoidant coping, and negative social support.
Methods
Participants
Over a period of 18 months (April 2005–September 2006), 361 pregnant HIV-infected women were recruited through the Serithi Project1 from four antenatal clinics in two townships in Tshwane (Pretoria), South Africa. Trained research assistants recruited eligible participants (i.e., pregnant HIV-positive women attending one of the four antenatal clinics) during their antenatal check-ups with assistance from clinic staff. Eligible women were given an information pamphlet about the Serithi Project, and invited to participate.
Both communities are predominantly black, Sepedi speaking and below average socio-economic status. These communities form part of a historically disadvantaged area and are representative of a large portion of the urban population in South Africa (Visser et al., 2009). During the time of the study, the prevalence rate of pregnant women testing HIV-positive in South Africa was 30.2% (Department of Health, 2005). From the 3,608 women screened at the four clinics during the study, 830 pregnant women (23%) were diagnosed HIV-positive, 40% of whom agreed to participate in the study.
Women were recruited at approximately 28 weeks into their pregnancy, with their gestational ages ranging from 6 to 41 weeks (SD = 6.7). After completion of the baseline assessment, the authors invited participants to take part in a structured 10-session weekly psychosocial support group intervention. Of the 361 women recruited for the study, 144 (40%) women chose to participate in this intervention. We conducted 15 structured support groups during the 18 months of the study (approximately 10 participants per group). The remaining 217 (60%) women declined the invitation to join the groups and formed the comparison group.
The authors conducted two follow-up assessments with all participants at two and eight months following completion of the intervention, which corresponded to approximately three months and nine months after the birth of their babies (Figure 1). Fifteen women (10%) who took part in the intervention and 67 women (31%) in the comparison group were lost to followup (not returning for either follow-up assessment). Thus, 129 intervention group participants and 150 comparison group participants were included in the analysis.
Figure 1.
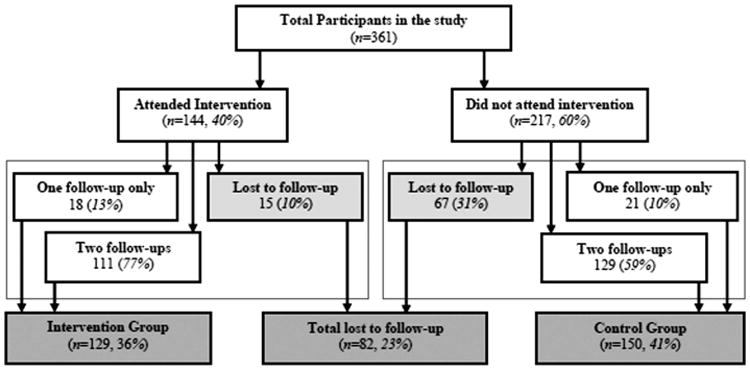
Schematic diagram of participant flow.
The women all provided informed, written, and signed consent prior to their involvement in the study. Institutional review board approval for the study protocol was obtained from the Faculty of Health Sciences Research Ethics Committee, University of Pretoria, South Africa and the Human Investigation Committee of Yale University School of Medicine, USA.
Intervention
An action research approach (Walker, 1998) was utilized in the development of the structured group intervention, with the intention of ensuring that the specific needs of the women would be incorporated into the intervention (Visser et al., 2005). This process involved: focus groups with community members and interviews with 317 HIV-infected women to gain better insight into the needs of pregnant HIV-infected women; two pilot support groups with HIV-infected women to refine the program; and last, three focus groups with participants and facilitators involved in piloting of the program, to finalize its development.
The intervention was developed from a systems theory perspective (Hanson, 1995), addressing first the personal level, with sessions focusing on HIV-related knowledge and the emotional impact of HIV infection. The intervention then moved to a focus on relational issues such as disclosure, and how to cope more effectively with HIV infection personally, in the home, the family, and within intimate relationships. Stress management was also addressed, with a strong emphasis placed on the relationship between stress and the immune system. Sessions then addressed issues of coping with stigma, discrimination and education on basic human rights. The intervention concluded with a session on life planning and goal setting, so as to leave participants with a sense of hope and a feeling of empowerment. The sessions were all structured so as to encourage group participation and experiential learning through games, role-plays, exercises, story-telling, case studies, and the sharing of experiences, feelings, and ideas (Visser et al., 2005).
Six Masters-level psychology students from the University of Pretoria facilitated the groups, with the assistance of four HIV-positive women (two from each community). All facilitators took part in a comprehensive training workshop, dealing with HIV and AIDS knowledge, counseling and group facilitation skills, training on how to implement the sessions, and the ethics involved in working with HIV-positive women in a group setting. They also practiced group facilitation in role-play group sessions. The authors held supervision and debriefing sessions after each support group session, for reporting on and dealing with issues from the session and discussing the following weeks' session material. An intervention manual comprehensively guided the facilitators throughout the process and included detailed descriptions and background information on each session. Each group was allocated two co-facilitators, with the Masters student focusing primarily on the facilitation process, and the HIV-positive co-facilitator assisting with language and cultural issues, and also providing a “role-model” for the group members.
Measures
All participants completed the baseline assessment. We conducted follow-up interviews approximately two and eight months after completion of the intervention, which corresponds to approximately three and nine months after the birth of the infant.
A trained research assistant conducted the interviews in each woman's mother tongue. The interviews lasted between one and two hours, and included questions on the woman's health, demographics, financial status, reaction to receiving her HIV-positive result, serostatus disclosure, and various psychosocial measures. The study utilized the following measures to assess the impact of the intervention:
Serostatus disclosure
Participants were asked if they had disclosed their HIV status to anyone and to whom they had disclosed. Follow-up interviews questioned respondents on whether or not they had disclosed to anyone since the previous interview. The authors informed respondents who were in the support groups that this question referred only to disclosure outside of the support group.
Center for Epidemiologic Studies Depression scale (CES-D, Radloff, 1977)
The CES-D has four separate factors: depressive affect, somatic symptoms, positive affect, and interpersonal feelings. A modified 15-item scale was used in this study because of the possible overlap of somatic items between symptoms of HIV and pregnancy (Kalichman et al., 2000). In the present study, a reliability coefficient of 0.88 was found.
Rosenberg Self-Esteem Scale (RSE, Rosenberg, 1979)
The RSE is a 10-item scale with four response choices, ranging from “strongly agree” to “strongly disagree.” The scores range from 10 to 40, with 40 indicating high self-esteem (alpha = 0.75).
Modified version of the Brief COPE (Carver, 1997)
The modified Brief COPE included 15 of the original items, with nine items added to make the measure more HIV-specific. We conducted an exploratory factor analysis which identified two factors, for which the authors then created two separate scales, namely “active” and “avoidant coping.” Results for the active coping scale showed an adequate internal consistency (alpha = 0.75). The avoidant coping scale had poor internal consistency (alpha D 0.54).
Multidimensional Social Support Inventory (Bauman & Weiss, 1995)
The MSSI was adapted to assess women's perceptions of the support they receive. The instrument was originally developed to assess the five domains of social support among minority women with HIV/AIDS in the USA. For this study, the authors combined practical, emotional, and affirmational support into a category termed “positive support.” This was done to differentiate from items assessing “negative support,” such as receiving unwanted help and advice, being dominated, and not having one's wishes respected. In each domain the respondent indicates the availability and adequacy of support they receive in three specific situations. Answers are coded on a four-point scale (“as much as I need,” “quite a lot,” “only a little,” and “no support”). In this study a reliability score of 0.9 was found for positive support and 0.6 for negative support.
Data Analysis
The authors conducted the analyses with intervention participation as the primary independent variable. To assess the effectiveness of the intervention, we conducted a series of random effects regression analyses (Raudenbush, Yang, & Yosef, 2000), thus allowing for the use of all available data, rather than excluding or imputing missing data. For each regression analysis, the authors treated the three assessment points as a random effect of time. Because the authors were interested in assessing both short- and long-term effects, a series of planned comparisons were modeled that looked at differences at the two and eight month follow-up periods.
The authors conducted two planned comparisons within the random effects regression for each outcome variable to take into account the level of attendance. First the authors compared the intervention group (IG) with the comparison group (CG). Next, the authors explored possible dose response effects by looking at members of the IG who had above average intervention exposure. The authors created a subgroup of IG, the High Attendance Group (HAG), including intervention participants who attended at least half of the sessions. The authors conducted a secondary contrast assessing differences between the HAG and the CG. This second contrast allowed us to examine the potential effect of group attendance. For the categorical variable (Disclosure), the authors conducted a series of logistic regression analyses (i.e. one at the two month follow-up and one at the eight month follow-up), using baseline disclosure as a covariate. For continuous outcomes (such as self-esteem and depression scores), the authors employed random effect regressions using general linear mixed models with SPSS® Version 15 for Windows, while controlling for baseline scores. Each contrast is distributed as a t-score.
Given the quasi-experimental design of this study, the authors controlled for a number of covariates using a backward stepwise procedure, in which covariates were eliminated until all had an associated p-value of < .25. Variables were removed one at a time and the effect was assessed by the significance of the change in the −2 log likelihood value. If this was > 0.05, the independent variable was removed. The most appropriate covariance structure was established using the same procedure. Once the final model was obtained, a plot of residuals was performed to assess normality. With regard to the logistic regression analyses, the likelihood ratio test was used to determine which variables to eliminate from the model. Model fit was then assessed by means of the Pseudo R2 statistic and the Hosmer Lemeshow test.
The authors controlled for the following potential covariates: age, marital status, number of dependents, CD4 count, time since diagnosis, HIV-related knowledge, level of education, having a regular income, per capita income, housing score,2 whether the participant's partner had a regular income, power score,3 and receiving financial support from the partner.
Results
Socio-Demographics of Participants
Significant differences at baseline between the intervention and comparison groups included employment (p < 0.05), with significantly fewer women from the intervention group working at the time of the initial interview (Table 1). The intervention group also had significantly lower per capita income compared to the comparison group (p < 0.05). In addition, a higher proportion of the intervention group had had already disclosed their HIV status (p < 0.05). A comparison of the baseline psychosocial data (Table 2) revealed significantly higher depression scores (p < 0.05) in the intervention group. The authors controlled for these variables in subsequent analyses.
Table 1. Demographic Factors at Baseline by Condition.
| Intervention group | Comparison group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Demographic variable | N | M | SD | % in condition | N | M | SD | % in condition | t score | χ2a | P |
| Age | 129 | 27.35 | 5.49 | 150 | 26.89 | 5.34 | 0.71 | .48 | |||
| Time since HIV diagnosisi | 127 | 14.20 | 46.84 | 146 | 13.73 | 45.19 | 0.08 | .93 | |||
| Per capita incomeii | 121 | 326.35 | 260.20 | 137 | 435.60 | 372.43 | −2.70 | .01 | |||
| SE Scoreiii | 129 | 1.48 | 1.10 | 150 | 1.56 | 1.06 | −0.61 | .54 | |||
| Power Scoreiv | 129 | 4.22 | 1.36 | 148 | 4.24 | 1.44 | −0.12 | .91 | |||
| Home language | 1.49 | .69 | |||||||||
| Sepedi | 54 | 41.9 | 71 | 47.3 | |||||||
| Zulu | 23 | 17.8 | 27 | 18 | |||||||
| Setswana | 13 | 10.1 | 16 | 10.7 | |||||||
| Otherv | 39 | 30.2 | 36 | 24 | |||||||
| Highest level of education: | 1.77 | .62 | |||||||||
| None | 3 | 2.3 | 2 | 1.3 | |||||||
| Primary | 12 | 9.3 | 12 | 8 | |||||||
| Secondary | 97 | 75.2 | 122 | 81.3 | |||||||
| Tertiary | 17 | 13.2 | 14 | 9.3 | |||||||
| Marital status: | 2.44 | .30 | |||||||||
| Married | 21 | 16.3 | 18 | 12 | |||||||
| Single with partner | 91 | 70.5 | 118 | 78.7 | |||||||
| Single without partner | 17 | 13.2 | 14 | 9.3 | |||||||
| Employment: | 7.32 | .01 | |||||||||
| Regular income | 22 | 17.1 | 46 | 31.1 | |||||||
| No regular income | 107 | 82.9 | 102 | 68.9 | |||||||
| Know someone with HIV | 1.65 | .20 | |||||||||
| Yes | 71 | 55 | 71 | 47.3 | |||||||
| No | 58 | 45 | 79 | 52.7 | |||||||
| Disclosed HIV status | 3.92 | .05 | |||||||||
| Yes | 92 | 71.3 | 90 | 60 | |||||||
| No | 37 | 28.7 | 60 | 40 | |||||||
Time since HIV diagnosis measured in weeks;
Per capita income measured in South African Rand (ZAR);
Socio-economic score measuring standard of living;
Power score measured the level of power the subject holds within her home, to make decisions related to sex, finances, food, health, and children;
Other languages included English, Afrikaans, Xhosa, Sotho, Venda, Tsonga, Ndebele, Seswati, and Shona.
Table 2. Psychosocial Factors.
| Baseline | 2 month follow-up | 8 month follow-up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Condition | N | Mean (SD) | N | Mean (SD) | Random effects regression planned contrast (t) | p | N | Mean (SD) | Random effects regression planned contrast (t) | p | |
| Active coping | 2.68 | .01 | 1.22 | .22 | |||||||
| (039) | Comparison | 146 | 31.48(3.96) | 143 | 32.77 (4.29) | 134 | 33.32 (3.93) | ||||
| Intervention | 128 | 32.07 (3.78) | 125 | 34.75 (3.35) | 115 | 34.67 (3.56) | |||||
| Avoidant coping | −2.02 | .04 | −0.35 | .73 | |||||||
| (024) | Comparison | 146 | 16.42 (2.51) | 143 | 16.35 (2.42) | 134 | 13.99 (2.48) | ||||
| Intervention | 129 | 16.73 (2.67) | 125 | 15.94 (2.78) | 115 | 14.24 (2.29) | |||||
| Self-Esteem | 1.92 | .06 | 1.27 | .21 | |||||||
| (040) | Comparison | 147 | 33.07 (4.06) | 143 | 33.81 (3.83) | 134 | 34.18(4.31) | ||||
| Intervention | 129 | 32.91 (4.14) | 125 | 34.44 (3.97) | 115 | 34.63 (3.37) | |||||
| Depression | 1.12 | .27 | −1.46 | .15 | |||||||
| (060) | Comparison | 146 | 16.04 (11.80) | 143 | 12.84 (12.53) | 134 | 14.32 (14.19) | ||||
| Intervention | 128 | 19.36 (14.42) | 124 | 16.59 (14.26) | 115 | 14.90(12.71) | |||||
| Positive support | 0.82 | .41 | −0.42 | .67 | |||||||
| (027) | Comparison | 149 | 19.93 (4.70) | 143 | 18.96 (4.58) | 134 | 19.27 (4.75) | ||||
| Intervention | 128 | 18.91 (5.87) | 123 | 19.63 (4.72) | 115 | 18.90 (5.04) | |||||
| Negative support | 0.68 | .47 | −1.28 | .20 | |||||||
| (09) | Comparison | 149 | 2.19 (2.51) | 143 | 3.73 (3.19) | 134 | 2.94 (2.58) | ||||
| Intervention | 129 | 2.47 (2.51) | 125 | 4.25 (3.46) | 115 | 2.71 (2.84) | |||||
Note. All analyses controlled for age, marital status, number of dependents, CD4 count, time since diagnosis, HIV-related knowledge, level of education, whether the participant had a regular income, per capita income, housing score, whether the participant's partner had a regular income, power score, or whether the participant received financial support from her partner.
Lost to Follow-Up
Comparison group participants were significantly more likely to be lost to follow-up (i.e., only attend the baseline interview) than participants who took part in the intervention (p < 0.001). The women who were lost to follow-up (67 women from the comparison group and 15 women from the intervention group) differed significantly at baseline from those who remained in the study. Women who were lost to follow-up were more likely to be living with a partner (p < 0.001), have a lower socio-economic status (p < 0.001), a lower level of HIV-related knowledge (p < 0.05), a lower level of self-esteem (p < 0.05) and a lower level of active coping (p < 0.05).
Attendance
On average, women attended slightly more than half of the sessions (Mean = 5.3 sessions, SD = 3.1). For this reason, the analysis included a second contrast, comparing the women in the HAG (the high attendance group– 78 women who attended at least five of the ten sessions) with those in the CG (the comparison group), so as to account for the possible impact of session attendance. Comparing the baseline scores of the HAG with those of the women who had not attended at least half of the sessions (LAG; low attendance group), significantly more women in the LAG had depressive symptoms (p < 0.05), lower active coping (p < 0.05) and a partner (p < 0.05) than women who had attended at least five sessions (HAG).
Disclosure
The authors conducted logistic regression analyses, controlling for baseline disclosure and covariates (p < 0.25), to determine whether participation in the intervention was significantly related to disclosure. Covariates included marital status, whether the woman had a regular income, per capita income, the power score, depression, negative coping, and self-esteem.
At baseline, 71% of the women in the intervention group had disclosed their status compared to 60% in the comparison group (p < 0.05). At the two month follow-up, the rate of disclosure in the intervention group was 94%, compared to 78% in the comparison group (AOR = 3.7, 95% CI = 1.5– 9.2, p < 0.001). By the eight month follow-up, 97% of the intervention group and 82% of the comparison group had disclosed (AOR = 8.3, 95% CI = 2.1– 32.9, p < 0.001). Therefore, even after controlling for baseline disclosure, the intervention group had significantly more disclosure at the two-month and eight-month follow ups.
Psychosocial Impact
Using a series of random effects regressions with planned contrasts, significant differences were found between the IG and the CG at the two-month follow-up both in terms of active coping and avoidant coping (Table 2). After adjusting for baseline differences, random effects regression contrasts showed that the intervention group displayed significantly higher levels of active coping compared to the comparison group at the two-month follow-up (t = 2.68, p < 0.05). Similarly, the IG had significantly lower levels of avoidant coping compared to the CG at the two-month follow-up (t = −2.02, p < 0.05). These improved levels of coping were maintained to the eight-month follow-up, although at this stage the CG coping scores had also improved considerably, and did not differ significantly from those of the IG.
Results also showed a marginally significant difference in self-esteem at the two-month follow up (t = 1.92, p = 0.057), with the IG self-esteem improving from slightly below that of the CG at baseline (IG = 32.91; CG = 33.07) to above the CG scores at the two-month follow-up (IG = 34.44; CG = 33.81). Similar to the pattern of the coping scores, these improved levels of self-esteem were maintained at the eight-month follow-up (34.63), at which stage the CG self-esteem scores had also improved (34.18). No significant differences were found between the groups in terms of depressive symptoms and support (positive and negative).
Secondary Contrast: Comparison of HAG and CG
To assess whether effects were existent/stronger for those in the intervention with adequate levels of intervention exposure, the authors conducted a secondary contrast that compared the HAG with the CG. The results from this contrast revealed that the women in the HAG were 14 times more likely to have disclosed at the eight-month follow-up than those in the comparison group (p < 0.001).
In addition, the self-esteem scores of the HAG differed significantly from those of the CG (t = 2.11, p < 0.05), with the HAG showing a considerable increase in self-esteem from baseline (32.98) to the two-month follow-up (35.02), whereas the CG remained relatively unchanged from baseline (33.07) to the two month follow-up (33.80). Similar to the self-esteem scores in the primary analysis, the HAG's improved self-esteem scores were maintained to the eight month follow-up, at which stage the CG's self-esteem scores had increased to comparable levels, eliminating the significant difference between them.
The secondary contrast also revealed that although levels of positive support remained relatively stable across all three sub-groups (IG, HAG, and CG) at all three time points, the HAG experienced a significant decrease in negative support at the eight-month follow-up, compared to the comparison group which experienced an increase in negative support (t = −2.41, p < 0.05).
Discussion
The aim of this study was to evaluate whether structured support groups are an effective intervention for pregnant South African women recently diagnosed HIV positive; and whether the effects of these interventions are sustainable over time. Results showed that such an intervention can improve adaptive coping strategies, self-esteem and HIV disclosure. Intervention participants experienced accelerated increases in coping and self-esteem from baseline to the first follow-up, but while these scores were maintained at the final follow-up, the associated scores of the comparison group had reached similar levels. This suggests that, in addition to its impact on disclosure, the structured support intervention accelerated the women's ability to cope during pregnancy, birth and early motherhood. The improvements in the coping strategies of the women who participated in the intervention may be attributed to their involvement and experience in the groups, as well as the content of the sessions, which was focused on developing their coping skills. A recent meta-analysis supports this result, because it showed that supportive interventions developed to assist people living with HIV can have a positive effect on participant's coping skills (Crepaz et al., 2008).
The accelerated increase in the use of active coping strategies and reduction in the use of avoidant coping strategies following participation suggests that the intervention was successful in supporting women in coping with their HIV infection during the time of their pregnancy and for the first few months after giving birth. This acceleration in adjusting to their HIV infection has the potential to affect positively not just the woman herself, but also her child and the development of their relationship in the future.
While the improvement in adaptive coping through follow-up may suggest sustainability of intervention outcomes, differences between the intervention group and the comparison group diminished over time. The task of ensuring the sustainability of such outcomes is challenging, however, because most HIV-positive women living in low socio-economic conditions are exposed to a range of psychological stressors that also have a strong influence on their psychosocial well-being (Gurung et al., 2004), and focused short-term interventions may not result in wide-ranging sustainable outcomes.
While the improvements in coping were not accompanied by decreases in the depressive symptom scores, participation in the intervention was positively related to the self-esteem of the women who had attended at least half of the sessions at short term follow-up, compared to the comparison group. This suggests that structured interventions have the potential to significantly improve psychological well-being, but indicates that the level of attendance plays an important role. More attention should therefore be placed on methods to maximize attendance rates in similar interventions.
While levels of positive support did not differ between the groups over time, women who attended at least half of the group sessions displayed significant decreases in negative support at the two month follow-up, compared to the comparison group. This suggests that women who attended more sessions felt more empowered and in control, and did not experience others to be overprotective or providing unwanted support.
Increased levels of disclosure of HIV status to friends and family were also observed among intervention participants, confirming previous research that has shown that people attending support groups are more likely to disclose their HIV status (Kalichman et al., 1996). Disclosure is an active coping strategy and may be an important step in HIV-related support seeking (Huber, 1996) and psychosocial adjustment, and also closely related to a woman's willingness to seek health care services (Nuwagaba–Biribonwoha et al., 2007). Kimberley and Serovich (1996) described disclosure in terms of six stages, and the first of these involves adjustment to the diagnosis. This suggests that individuals who have disclosed may be better adjusted to their HIV infection than those who have not, and this can subsequently contribute to increased support.
Higher levels of disclosure are important from an individual point of view, but also have implications for prevention, testing and treatment. Research has shown that when disclosure does occur, testing and the use of contraception increases. (King et al., 2008; Wong et al., 2009), as well as improved adherence to PMTCT (Matji et al., 2008).
Given the above findings, it is clear that delays in disclosing can have far-reaching detrimental effects. In a study conducted in South Africa, 79% of women participants had disclosed to their partners, but 15% of these had delayed more than a year before disclosing (Skogmar et al., 2006). The implementation of support groups, such as the one assessed in this research, may therefore offer important benefits not only for the individuals that participate, but for the community at large.
The authors controlled for discrepancies in levels of disclosure between conditions displayed during the baseline assessment during the analyses of follow-up data. Disclosure of one's HIV status is inevitable in an HIV support group, and individuals who are not ready to disclose may fear participation in a support group for this reason. This is especially true in a close-knit community such as the communities from which these women came. It may seem daunting to an individual still coming to terms with their infection to join a support group. Individuals may also fear the consequences of their disclosure, for fear of their family, friends and the community in general finding out, and for fear of the possible consequent discrimination. Several members of the comparison group in this study mentioned these reasons for not participating in the intervention (Mundell et al., in press). The risks involved in support groups are a limitation of the intervention.
Limitations
Limitations of the present study included: (1) the quasi-experimental nature of the study, which promoted baseline differences between the two conditions due to non-randomization and thus self-selection for participation in the intervention; (2) the potential influence of pregnancy and childbirth on intervention attendance, because the findings suggested that participants who did not attend at least half of the sessions did not fully benefit from their involvement;4 (3) related to the previous point, the low participation rate, which may have resulted in participation bias; and (4) the relatively small sample size, which may have resulted in insufficient statistical power to determine meaningful differences, particularly when controlling for confounding factors.
Conclusion
Study findings suggest that an intervention developed to meet the specific needs of pregnant South African women recently diagnosed HIV positive can accelerate these women's abilities to cope more effectively with their HIV infection and improve levels of HIV status disclosure. The results also suggest that such an intervention can have a positive effect on self-esteem. Improvements in the use of active coping skills, self-esteem and disclosure rates support our hypothesis that an intervention of this kind can assist pregnant women in their attempts to cope with their newly discovered HIV positive status.
The overall impact of intervention would seem to be relatively short-term, and thus the sustainability of the benefits of the intervention is uncertain. Only disclosure was found to be a significant outcome of participation at the second follow-up, since the psychosocial improvements of the comparison group over time diminished the differences between the groups at the final follow-up. This implies that interventions of this kind, implemented in resource-limited settings, may accelerate the process of adjusting to one's HIV status, but may not have sustainable benefits over time. While this accelerated adjustment is important, considering the time at which it occurs (i.e., during pregnancy and the first few months of motherhood), the result suggests that the intervention may only significantly affect participants during and directly following their involvement. This may in part be due to the broad range of other psychological stressors experienced by women living in these kinds of environments (Gurung et al., 2004).
Future research should include strategies to maximize intervention exposure for participants and consider integration of an on-going support program (such as a member-run support group) to follow-on from the more structured intervention. In addition, as was the case in this study, interventions should be developed to not only meet the specific HIV-related needs of the target group, but also assist them in managing general life stressors, as these may have a significant impact on the women's adjustment to HIV infection. Finally, to address the methodologic limitations of this study, it is recommended that future research should use a randomized controlled trial to verify these results in a larger sample in which selection and participation biases are minimized.
Although the results of this study outline some key challenges in successfully implementing structured support groups, it is clear that developing countries such as South Africa could certainly benefit from their implementation. This is especially considering the current lack of psychosocial support for people living with HIV and AIDS, and the relatively low cost implications of implementing support groups. It will be important, however, that these interventions are developed to meet the specific needs of the participants, and to integrate mechanisms for more on-going support.
Footnotes
The Serithi Project (NIH R24HD43558) is a longitudinal study aimed at developing an understanding of the experiences of women who test HIV-positive at antenatal clinics in townships in Tshwane, South Africa.
The housing score included five items, namely whether the house was built from bricks or cement, whether there was running water within the home, whether there was a flushing toilet, whether the dwelling had electricity and whether a refrigerator was owned A score of 1 was assigned for affirmative answers. The total score was out of 5.
A power score was calculated, which estimates the level of power the woman holds within her home, to make decisions related to sex, finances, food, health decisions, and children. A score of 1 was assigned if the women made the decision, or it was made jointly with her and someone else. The total score was out of 6.
The authors examined correlations between stage of pregnancy and the various psychosocial scores for the women participating in the groups, but found no significant differences.
Contributor Information
Jonathan P. Mundell, MRC Unit for Maternal and Infant Health Care Strategies, University of Pretoria, Pretoria, South Africa.
Maretha J. Visser, Department of Psychology, University of Pretoria, Pretoria, South Africa.
Jennifer D. Makin, MRC Unit for Maternal and Infant Health Care Strategies, University of Pretoria, Pretoria, South Africa.
Trace S. Kershaw, School of Public Health, Yale University, New Haven, Connecticut, USA.
Brian W. C. Forsyth, Department of Pediatrics, Yale University, New Haven, Connecticut, USA.
Bridget Jeffery, MRC Unit for Maternal and Infant Health Care Strategies, University of Pretoria, Pretoria, South Africa.
Kathleen J. Sikkema, Department of Psychology and Neuroscience, Duke University, Durham, North Carolina, USA.
References
- Adewuya AO, Ola BO, Aloba OO, Mapayi BM, Okeniyi JA. Impact of postnatal depression on infants' growth in Nigeria. J Affect Disorders. 2008;108:191–93. doi: 10.1016/j.jad.2007.09.013. [DOI] [PubMed] [Google Scholar]
- Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: A risk factor for obstetric fetal and neonatal outcome? A critical review of the literature. J Matern-Fetal Neo M. 2007;20:189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- Amon JJ. Preventing HIV infections in children and adolescents in sub-Saharan Africa through integrated care and support activities: A review of the literature. Afr J AIDS Res. 2002;1:143–9. doi: 10.2989/16085906.2002.9626553. [DOI] [PubMed] [Google Scholar]
- Amuyunzu–Nyamongo M, Okeng'o L, Wagura A, Mwenzwa E. Putting on a brave face: The experiences of women living with HIV and AIDS in informal settlements of Nairobi, Kenya. AIDS Care. 2007;19(Supplement 1):s25–s34. doi: 10.1080/09540120601114618. [DOI] [PubMed] [Google Scholar]
- Bauman LJ, Weiss E. Multidimensional Social Support Inventory: Revised. Bronx, New York: Albert Einstein College of Medicine; 1995. [Google Scholar]
- Blaney N, Fernandez M, Etier K, Wilson T, Walter E, Koenig L. Psychosocial correlates of depression among HIV-infected pregnant women. AIDS Patient Care ST. 2004;18:405–15. doi: 10.1089/1087291041518201. [DOI] [PubMed] [Google Scholar]
- Brandt R. Putting mental health on the agenda for HIV+ women: A review of evidence from Sub-Saharan Africa. Women Health. 2009;49:215–28. doi: 10.1080/03630240902915044. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chida Y, Vedhara K. Adverse psychosocial factors predict poorer prognosis in HIV disease: A meta-analytic review of prospective investigations. Brain Behav Immun. 2009;23:434–45. doi: 10.1016/j.bbi.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Passin WF, Herbst JH, Rama SM, Malow RM, Purcell DW, et al. Meta-analysis of cognitive-behavioral interventions on HIV-positive persons' mental health and immune functioning. Health Psychol. 2008;27:4–14. doi: 10.1037/0278-6133.27.1.4. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane DB Syst Rev. 2004;4:CD001134. doi: 10.1002/14651858.CD001134.pub2. [DOI] [PubMed] [Google Scholar]
- Department of Health. National HIV and syphilis antenatal sero-prevalence survey in South Africa 2005. Pretoria: Department of Health; 2005. [Google Scholar]
- Department of Health. 2008 national antenatal sentinel HIV and syphilis prevalence survey, South Africa. Pretoria: Department of Health; 2009. [Google Scholar]
- Evans DL, Ten–Have TR, Douglas SD. Association of depression with viral load, CD9 T lymphocytes, and natural killer cells in women with HIV infection. Am J Psychiat. 2002;159:1752–59. doi: 10.1176/appi.ajp.159.10.1752. [DOI] [PubMed] [Google Scholar]
- Geller PA. Pregnancy as a stressful life event. CNS Spectr. 2004;9:188–97. doi: 10.1017/s1092852900008981. [DOI] [PubMed] [Google Scholar]
- Gurung RA, Taylor SE, Kemeny M, Myres H. HIV is not my biggest problem: The impact of HIV and chronic burden on depression in women at risk for AIDS. J Soc Clin Psychol. 2004;23:490–511. [Google Scholar]
- Hanson BG. General systems theory beginning with wholes. Toronto: Taylor & Francis; 1995. [Google Scholar]
- Harpham T, Huttly S, DeSilva MJ, Abramsky T. Maternal mental health and child nutritional status in four developing countries. J Epidemiol Commun H. 2005;59:1060–4. doi: 10.1136/jech.2005.039180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelhoch S, Medoff DR, Oyeniyi G. Efficacy of group psychotherapy to reduce depressive symptoms among HIV-infected individuals: A systematic review and meta-analysis. AIDS Patient Care ST. 2007;21:732–39. doi: 10.1089/apc.2007.0012. [DOI] [PubMed] [Google Scholar]
- Huber CH. Facilitating disclosure of HIV-positive status to family members. Fam J Couns Ther. 1996;4:53–55. [Google Scholar]
- Ironson G, Weiss S, Lydston D, Ishii M, Jones D, Asthana D, et al. The impact of improved self-efficacy on HIV viral load and distress in culturally diverse women living with AIDS: The SMART/EST Women's Project. AIDS Care. 2005;17:222–36. doi: 10.1080/09540120512331326365. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188:662–70. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Sikkema KJ, Somlai A. People living with HIV infection who attend and do not attend support groups: A pilot study of needs, characteristics and experiences. AIDS Care. 1996;8:589–99. doi: 10.1080/09540129650125542. [DOI] [PubMed] [Google Scholar]
- Kimberly JA, Serovich JM. Perceived social support among people living with HIV/AIDS. Am J Fam Ther. 1996;24:41–53. [Google Scholar]
- King R, Katuntu D, Lifshay J, Packel L, Batamwita R, Nakayiwa S, et al. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS Behav. 2008;12:232–43. doi: 10.1007/s10461-007-9307-7. [DOI] [PubMed] [Google Scholar]
- Makin JD, Forsyth BWC, Visser MJ, Sikkema KJ, Neufeld S, Jeffery B. Factors affecting disclosure in South African HIV-positive pregnant women. AIDS Patient Care ST. 2008;22:907–16. doi: 10.1089/apc.2007.0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matji JN, Wittenberg DF, Makin JD, Jeffery B, MacIntyre UE, Forsyth BWC. Psychosocial and economic determinants of infant-feeding intent by pregnant women in Tshwane/Pretoria. S Afr J Child Health. 2008;2:114–18. [Google Scholar]
- Morrow K, Costello T, Boland R. Understanding the psychosocial needs of HIV-positive women: A qualitative study. Psychosomatics: J of Consult Liais Psychiat. 2001;42:497–503. doi: 10.1176/appi.psy.42.6.497. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT. Positive affect predicts lower risk of AIDS mortality. Psychosomatic Medicine. 2003;65:620–26. doi: 10.1097/01.psy.0000073873.74829.23. [DOI] [PubMed] [Google Scholar]
- Moultrie A, Kleintjes S. Women's mental health in South Africa. In: Ijumba P, Padrarath A, editors. South African Health Review 2006. Durban: Health Systems Trust; 2006. pp. 347–373. [Google Scholar]
- Mundell JP, Visser MJ, Makin JD, Forsyth BW, Sikkema KJ. Support group processes: Perspectives from HIV-infected women in South Africa. Qual Res Psychol. doi: 10.1080/14780887.2010.500350. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuwagaba-Biribonwoha H, Mayon-White RT, Okong P, Carpenter LM. Challenges faced by health workers in implementing the prevention of mother-to-child HIV transmission (PMTCT) programme in Uganda. Oxford J Public Health. 2007;29:269–74. doi: 10.1093/pubmed/fdm025. [DOI] [PubMed] [Google Scholar]
- Olley BO, Gxamza F, Seedat S, Theron H, Taljaard J, Reid E, et al. Psychopathology and coping in recently diagnosed HIV/AIDS patients—the role of gender. S Afr Med J. 2003;93:928–31. [PubMed] [Google Scholar]
- Patel V, DeSouza N, Rodrigues M. Postnatal depression and infant growth and development in low income countries a cohort study from God, India. Arch Dis Child. 2003;88:34–37. doi: 10.1136/adc.88.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plattner IE, Meiring N. Living with HIV: The psychological relevance of meaning making. AIDS Care. 2006;18:241–45. doi: 10.1080/09540120500456227. [DOI] [PubMed] [Google Scholar]
- Psaros C, Geller PA, Aaron E. The importance of identifying and treating depression in HIV infected, pregnant women: A review. J Psychosom Obst Gyn. 2009;30:275–81. doi: 10.3109/01674820903254740. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psych Meas. 1977;1:385–401. [Google Scholar]
- Rahman A, Lovel H, Bunn J, Iqbal Z, Harrington R. Mother's mental health and infant growth: A case-control study from Rawalpindi. Child Care Hlth Dev. 2004;30:21–7. doi: 10.1111/j.1365-2214.2004.00382.x. [DOI] [PubMed] [Google Scholar]
- Rahman A, Bunn J, Lovel H, Creed F. Maternal depression increases infant risk of diarrheal illness: A cohort study. Arch Dis Child. 2007;92:24–8. doi: 10.1136/adc.2005.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S, Yang M, Yosef M. Maximum likelihood for hierarchical models via high-order, multivariate LaPlace approximation. J Comput Graph Stat. 2000;9:141–57. [Google Scholar]
- Rehle T, Shisana O, Pillay V, Zuma K, Puren A, Parker W, et al. National incidence measure—new insights into the South African epidemic. S Afri Med J. 2007;97:194–9. [PubMed] [Google Scholar]
- Rosenberg M. Conceiving the self. New York: Basic Books, Inc; 1979. [Google Scholar]
- Ryan D, Mills L, Misri N. Depression during pregnancy. Can Fam Physician. 2005;5:1087–93. [PMC free article] [PubMed] [Google Scholar]
- Sanders LB. Women's voices: The lived experience of pregnancy and motherhood after diagnosis with HIV. Journal of the Assoc of Nurses in AIDS Care. 2008;19:47–57. doi: 10.1016/j.jana.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Scott–Sheldon LAJ, Kalichman SC, Carey MP, Fielder R. Stress management improves mental health and quality of life in adults with HIV: A meta-analysis of randomized controlled trials, 1990 to 2006. Health Psychol. 2008;27:129–39. doi: 10.1037/0278-6133.27.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64:1823–31. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner D, Mfecane S. Stigma, discrimination and the implications for people living with HIV/AIDS in South Africa. SAHARA J. 2004;1:157–64. doi: 10.1080/17290376.2004.9724838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skogmar S, Shakely D, Lans M, Danell J, Andersson R, Tshandu N, et al. Effect of antiretroviral treatment and counselling on disclosure of HIV-serostatus in Johannesburg, South Africa. AIDS Care. 2006;18:725–30. doi: 10.1080/09540120500307248. [DOI] [PubMed] [Google Scholar]
- Spinelli MG. Interpersonal psychotherapy for depressed antepartum women: A pilot study. Am J Psychiatry. 1997;154:1028–30. doi: 10.1176/ajp.154.7.1028. [DOI] [PubMed] [Google Scholar]
- Stringer EM, Chi BH, Chintu N, Creek TL, Ekouevi DK, Coetzee D, et al. Monitoring effectiveness of programmes to prevent mother-to-child HIV transmission in lower-income countries. Bull World Health Organ. 2008;86:57–62. doi: 10.2471/BLT.07.043117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers J, Robinson R, Capps L, Zisook S, Atkinson JH, McCutchan E, et al. The influence of HIV-related support groups on survival in women who lived with HIV. Psychosomatics. 2000;41:262–66. doi: 10.1176/appi.psy.41.3.262. [DOI] [PubMed] [Google Scholar]
- UNAIDS. UNAIDS report on the global AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS; 2010. [Google Scholar]
- Visser MJ, Mundell JP, De Villiers AE, Sikkema K, Jeffery B. Development of structured support groups for HIV-positive women in South Africa. SAHARA J. 2005;2:333–43. doi: 10.1080/17290376.2005.9724858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser MJ, Makin JD, Vandormael A, Sikkema KJ, Forsyth BWC. HIV/AIDS stigma in a South African community. AIDS Care. 2009;21:197–206. doi: 10.1080/09540120801932157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser MJ, Neufeld S, De Villiers AE, Makin JD, Forsyth BWC. To tell or not to tell: South African women's disclosure of HIV status during pregnancy. AIDS Care. 2008;20:1138–45. doi: 10.1080/09540120701842779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker M. Action research and participatory research in South Africa. In: Mouton Johann, Muller Johan, Franks Peter, Sono Themba., editors. Theory and method in South African human sciences research: Advances and innovations. Pretoria: Human Sciences Research Council; 1998. pp. 239–53. [Google Scholar]
- Wong LH, Van Rooyen H, Modiba P, Richter L, Gray G, McIntyre JA, et al. Test and tell: Correlates and consequences of testing and disclosure of HIV status in South Africa. J Acq Immun Def Synd. 2009;50:215–22. doi: 10.1097/QAI.0b013e3181900172. [DOI] [PMC free article] [PubMed] [Google Scholar]


