Introduction
Golf as an activity appeared early in the world of sport. It is reported to have originated in Scotland and is now a popular recreational sport worldwide. As the population ages; golf is likely to become an increasingly popular leisure time activity because it allows a variety of individuals, regardless of skill, gender, or age, to play simultaneously.
Injury as with all other sports can also occur while playing golf. The low back followed by the elbow are the most common sites of injury sustained whilst playing golf and can either be due to overuse or traumatic in nature.1
Golf-related ocular injuries have been reported since the early 1900s.2 Though this type of injury is fortunately rare, however the effects are usually devastating and often of such a severity that it usually necessitates the removal of the eye.3,4
Most of the golf-related eye injuries mentioned in literature have occurred either due to golf balls (more commonly) or due to the clubs used.3,4 In the past there have been incidents reported of ocular trauma occurring from the explosive rupture of the golf balls,5 however nowadays with the quality of golf balls improving, such incidents are practically unheard of. The available literature also mentions of a couple of rare cases of ocular injuries caused by golf tees,6 however ocular injury caused by a splinter ricocheting back into the eye of the player himself, while taking a golf swing, is unheard of. To the best of our knowledge it has never been ever reported in literature earlier.
Case report
A 42 year old patient was brought, early in the morning, with a history of injury to his left eye while playing golf. The patient, a right handed golfer, had unluckily managed to land his golf ball right behind a tree in the previous shot. In order to get his ball back onto the fairway the patient had to take his next shot at a difficult angle for which he adopted a very awkward stance and took a full swing trying to gain as much distance as possible, in the relatively right direction. Though the patient did successfully manage to extricate his ball, however while taking this difficult shot, his club also struck a hard unknown object, most probably a stone or a piece of wood lying on the ground next to the ball, camouflaged by the leaves. The patient is still not sure what exactly did he hit, but this object flew off, struck the tree trunk and ricocheted back, striking him on his left eye. This was followed by severe pain and loss of vision. The game was immediately abandoned and he was brought to this centre.
On presentation, the patient had severe pain on even trying to open his eye. His vision was reduced to just hand movements close to face. Slit lamp examination revealed the eye to be severely contaminated with dirt and dust particles. There was circumcorneal congestion and the cornea was very hazy. Fluorescein staining revealed a large corneal epithelial defect in the temporal half of the cornea. The anterior chamber too was hazy due to hyphaema and there was traumatic mydriasis with a mid dilated fixed pupil [Fig. 1]. The fundus details could not be evaluated due the media being extremely hazy. The intraocular pressure (IOP) was raised to 54 mm of Hg as measured by a non-contact tonometer (NCT).
Fig. 1.
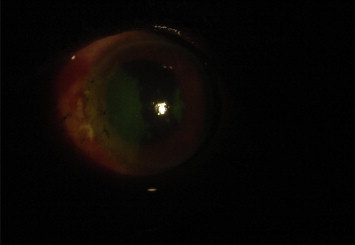
Fluorescein stain revealing corneal epithelial defect in the temporal half of the cornea.
Initially the eye was washed thoroughly with sterile normal saline to remove the dirt particles. Then a USG B Scan was done which revealed a vitreous haemorrhage but luckily no retinal detachment [Fig. 2]. The patient was admitted given an eye shield and advised activity restriction (quiet ambulation). He was started on IV Mannitol 350 ml stat followed by tablet acetazolamide 250 mg 2 TDS. Topically, broad spectrum antibiotic eye drops were started, initially at 2 hourly intervals for the first 48 h and then tapered off to QID dosage for the next 5 days. He was also put on topical antiglaucoma medication i.e. Timolol 0.5% + dorzolamide TDS + brimonidine 0.2% BD along with mydriatics i.e. eye drop homatropine 2% QID. He was also put on systemic steroids i.e. tab prednisolone 60 mg OD in tapering doses.
Fig. 2.
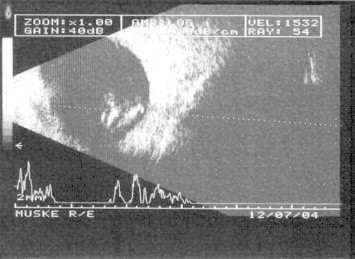
USG B Scan showing the vitreous haemorrhage.
The patient responded well to the above treatment and within 72 h the corneal epithelial defect had reduced and the hyphaema had settled down inferiorly [Fig. 3]. The IOP was 36 mm of Hg NCT and the patient's vision improved to counting fingers close to face.
Fig. 3.

Three days post injury – The corneal epithelial defect has reduced and the hyphaema has settled down inferiorly.
By end of first week the corneal epithelial defect had healed, though some corneal haze still persisted. The hyphaema too reduced to a small clot on the nasal aspect of the anterior chamber and the patients vision improved to 6/36 [Fig. 4]. The IOP reduced to 18 mm of Hg NCT. Tablet acetazolamide was stopped, though the topical antiglaucoma medication was continued. USG B Scan done at this stage revealed a resolving vitreous haemorrhage.
Fig. 4.

One week post injury – Mild corneal haze still persists and the hyphaema has reduced to a small clot on the nasal aspect of the anterior chamber.
By the end of 4 weeks the patient's vision had improved to 6/6 (P), and his cornea had cleared completely, however mild traumatic mydriasis still persisted [Fig. 5]. USG B Scan too revealed a completely resolved vitreous haemorrhage. Gonioscopy done at this stage revealed no evidence of angle recession. The patient was subsequently sent on 4 weeks sick leave. Gonioscopy was repeated again after the patient returned back after the sick leave and was normal. He is now being regularly followed up on an OPD basis.
Fig. 5.

Four weeks post injury – A clear cornea with a completely resolved hyphaema: however mild traumatic mydriasis persisting.
Discussion
Sports induced injuries are indeed very common with more than 600,000 sports and recreation related eye injuries occurring every year.7 Though golf-related eye injuries are quite uncommon, however when they do occur, they are so severe, that often enucleation is the only course available.3,4 Most injuries occur with golf balls and less commonly with golf clubs. However golf club injuries are commoner in children and usually occur while at play away from the golf course.8
In our case the eye injury had occurred with a splinter ricocheting into the eye while the patient himself was taking a golf swing. Fortunately the patient reported immediately, so that appropriate management could be started early. Luckily too it was a closed globe injury; as injuries associated with a ruptured globe usually have a worse visual prognosis.9
Since on presentation the eye appeared to be severely contaminated, the patient was prophylactically started on systemic as well as topical broad spectrum antibiotics. We also started the patient on antiglaucoma drugs as the injury was associated with hyphaema and a raised intraocular pressure. Topical mydriatics were used to relieve ciliary spasm and pain.10 General measures like hospitalization, eye shield application and avoidance of strenuous activity were the same as supported by most literature.11
Conclusion
In conclusion, golf related ocular injuries, though uncommon, are frequently associated with severe ocular trauma and a poor visual outcome. Most of the injuries occur either due to the golf balls or the golf clubs. However eye injury caused by an object, other than the golf ball, ricocheting back into the eye of the player himself, while taking a golf swing, was until now, absolutely unheard of.
Conflicts of interest
All authors have none to declare.
References
- 1.McHardy A., Pollard H., Luo K. Golf injuries: a review of the literature. Sports Med. 2006;36(2):171–187. doi: 10.2165/00007256-200636020-00006. [DOI] [PubMed] [Google Scholar]
- 2.Pollack J.S., Mieler W.F., Mittra R.A. Golf-related ocular injuries. Curr Opin Ophthalmol. 1997 Jun;8(3):15–18. doi: 10.1097/00055735-199706000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Townley D., Kirwan C., O'Keefe M. Golf–recognising the risk of severe eye injury. Ir Med J. 2008 Jun;101(6):167–169. [PubMed] [Google Scholar]
- 4.Jayasundera T., Vote B., Joondeph B. Golf-related ocular injuries. Clin Exp Ophthalmol. 2003 Apr;31(2):110–113. doi: 10.1046/j.1442-9071.2003.00615.x. [DOI] [PubMed] [Google Scholar]
- 5.Farley K.G. Ocular trauma resulting from the explosive rupture of a liquid center golf ball. J Am Optom Assoc. 1985 Apr;56(4):310–314. [PubMed] [Google Scholar]
- 6.Specht C.S., Varga J.H., Jalali M.M., Edelstein J.P. Orbitocranial wooden foreign body diagnosed by magnetic resonance imaging. Dry wood can be isodense with air and orbital fat by computed tomography. Surv Ophthalmol. 1992 Mar–Apr;36(5):341–344. doi: 10.1016/0039-6257(92)90110-f. [DOI] [PubMed] [Google Scholar]
- 7.Mishra A., Verma A.K. Sports related ocular injuries. MJAFI. 2012;68:260–266. doi: 10.1016/j.mjafi.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hink E.M., Oliver S.C., Drack A.V. Pediatric golf-related ophthalmic injuries. Arch Ophthalmol. 2008 Sep;126(9):1252–1256. doi: 10.1001/archopht.126.9.1252. [DOI] [PubMed] [Google Scholar]
- 9.Weitgasser U., Wackernagel W., Oetsch K. Visual outcome and ocular survival after sports related ocular trauma in playing golf. J Trauma. 2004 Mar;56(3):648–650. doi: 10.1097/01.ta.0000062970.91139.05. [DOI] [PubMed] [Google Scholar]
- 10.Papaconstantinou D., Georgalas I., Kourtis N., Karmiris E., Chrysanthi K., Ladas L. Contemporary aspects in the prognosis of traumatic hyphemas. Clin Ophthalmol. 2009;3:287–290. doi: 10.2147/opth.s5399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carlzada J.I., Kerr N.C. Traumatic hyphaemas in children secondary to corporal punishment with a belt. Am J Ophthalmol. 2003;135(5):719–720. doi: 10.1016/s0002-9394(02)01890-1. [DOI] [PubMed] [Google Scholar]


