Abstract
Background
The immediate placement of implants into fresh extraction socket has proven to be a safe and predictable procedure. However, there is lack of scientific evidence regarding the healing pattern and osseointegration associated with immediate implants especially with different grafting materials.
Methods
A total of 30 patients male or female, with a mean age of 23.1 years ± 6.0 in the age group of 18–38 years, each having at least one tooth indicated for extraction (either maxillary or mandibular anterior teeth) were selected and randomly divided in to two groups. 30 Implants (Xive® friadent, Germany) were placed into fresh extraction sockets during this study. Two types of graft materials namely Dembone® (freeze-dried bone allograft) for group A and G-Bone® (modified hydroxyapatite) for group B were used. After implant placement all implants were evaluated clinically and radiographically at baseline, 3 months, 6 months, 9 months and 12 months. All clinical and radiographic parameters were subjected to statistical analysis. Intragroup comparisons were made with paired ‘t’ test and intergroup comparisons with unpaired ‘t’ test (P > 0.05 NS, ≤0.05 S, ≤0.01 HS).
Result
During the 1-year interval, no implant was lost and the mean bone level at the implants was maintained or even improved.
Conclusion
Immediate restoration of single tooth implants placed in fresh extraction sockets could be considered a valuable option to replace a missing tooth. The graft materials used in both groups have been found to be equally effective.
Keywords: Immediate implant, DFDBA, HA
Introduction
The replacement of a tooth using an implant is derived from an evolution in concepts, technology, and clinical applications, following years of basic research and fundamental studies on the concept of osseointegration. The method of osseointegration, developed by many researchers, is well documented.1 Due to the advantages provided by implant supported prosthesis, like improved esthetics, improved function, improved hygiene accessibility, and osseous preservation, all at a comparable cost, the single tooth implant replacement is a more viable option for today's patient than teeth supported fixed partial denture that involves preparation of adjacent teeth.
In situations where a tooth requires extraction and replacement, original protocol (gold standard) suggested a 6–12 month waiting period before implant placement. The original protocol has been challenged within the last decade and new protocols have been developed in which implants are placed at the time of extraction of the tooth. This protocol wherein implants have been placed at the time of tooth extraction is known as immediate implants. Since, the first report of the placement of a Tubingen® dental implant into a fresh extraction socket, there has been increasing interest in this technique.2 Research and clinical studies on immediate implants in animals and humans have been encouraging.3,4 Immediate implant placement was shown to have a failure rate of <5%, which is comparable to delayed placement. There is enough scientific evidence to support the procedures of immediate implant placement in comparison to the conventional two stage delayed protocol.5
Inspite of advanced diagnostic facilities, it is a real challenge to place an implant matching the extracted tooth dimensions. The space between the implant and bone is required to be filled in three dimensions with a biocompatible material for enhanced osseointegration. A number of graft materials are used for this purpose and these include the use of expanded poly tetra fluoro ethylene (ePTFE) membranes, bioabsorbable membranes, demineralized freeze-dried bone allograft (DFDBA), freeze-dried bone allograft (FDBA), bone autograft, hard tissue replacement polymer, connective tissue barriers, hydroxyapatite (HA), xenografts, use of growth and differentiation factors, particulate and block grafting materials and guided bone regeneration (GBR). As per scientific evidence, none of these materials had shown any superior outcome when compared in-vivo.6,7 Therefore an ‘in-vivo’ study was undertaken to evaluate clinically and radiographically the success of immediate implant placement at the time of extraction with two commonly used graft materials i.e. Dembone® (Demineralized freeze-dried bone) and G-Bone® (modified hydroxyapatite granules). Even though these two materials are used extensively in regenerative procedures, there is no enough scientific literature to support their use in immediate implants.
Material and methods
A total of 30 patients male or female, in the age group of 18–38 years, each having at least one tooth indicated for extraction (either maxillary or mandibular anterior teeth) were selected and 30 implants were placed into fresh extraction sockets during this study. The patients selected were non-smokers, free from any systemic disease, non-bruxers, with sufficient quality and quantity of bone and prepared to comply with the follow-up and maintenance programme. Indications for tooth extraction and immediate implant placement included root fractures, endodontic failures, caries, internal resorption, external resorption, tooth with open apex and over-retained deciduous tooth. After approval from the local ethical committee, all the patients signed an informed consent form before starting the clinical protocols. After the routine preoperative investigations and treatment planning, Implants were placed in the subsequent appointments by single operator following standardized clinical and laboratory protocols.
Xive S® implants (Friadent®, Dentsply, Mannheim, Germany) used in this study were of root form threaded and internal hex design. Patients were divided in to two groups based on the graft material used. For group A, demineralized freeze-dried bone allograft (Dembone® Pacific Coast Tissue Bank, 2500-19 S, Flower St. Los Angeles) was used and for group B, modified hydroxyapatite (G-Bone®, Surgiwear Limited, Belgium) was used (Fig. 1).
Fig. 1.

Dembone ® (DFDBA) & G-Bone® (modified hydroxyapatite).
Surgery was performed under local anesthesia (lignocaine 20 mg/ml with adrenaline 1:80,000). All the surgical procedures were carried under strict aseptic conditions. Teeth indicated for extractions were removed atraumatically. After evaluating the dimensions of the socket and findings of the CT scan, final decision regarding the dimensions of the implant was taken. Drilling of the osteotomy site was done according to the manufacturer instructions. Sequential drilling with copious irrigation was carried out till the desired dimensions were achieved depending on the selected implant. Implants of decided dimension were placed at a speed of 20–30 rpm using xive® implant driver. During implant placement care was taken that, angulation of placement was identical to that of the pre-existing tooth. Implants were placed 1 or 2 mm below the alveolar crest. Xive® implants are provided with an abutment for the option of immediate loading. In this study, since the implants were not immediately loaded they were separated from the abutment with hex driver and cover screw was placed. Discrepancies between the implant and walls of the prepared socket were measured and bone graft was placed (Figs. 2 and 3). 15 sockets received HA available in granule form and 15 sockets received DFDBA. The site was covered with snugly sutured flap. 5-0 silk sutures were used to achieve primary closure with the help of interrupted sutures. The oral hygiene instructions were given and the patients were followed up frequently. After Implant placement, all patients were recalled for evaluation of peri-implant soft tissue conditions, individual implant stability and radiographic marginal bone loss. All the implants were prosthetically loaded with porcelain fused to metal crowns after 6 months (Fig. 4).
Fig. 2.

Implant site showing horizontal defect dimensions (HDD).
Fig. 3.

HDD filled with bone graft.
Fig. 4.

Post rehabilitation view of implant retained porcelain fused to metal crown.
Evaluation of the treatment outcome
Patients were evaluated with the following clinical and radiological parameters at baseline (BL), 3 months (3M), 6 months (6M), 9 months (9M) and 12 months (12M). All these parameters were evaluated for the implant (IMP) site as well as full mouth (FM) for comparisons.
Soft tissue evaluation
Soft tissue evaluation was done using modified Plaque Index, Gingival Index and probing depth. For modified Plaque Index and Gingival Index the implants were evaluated at four sites (buccal, lingual, mesial, and distal). Probing depth was also evaluated at four sites around implant (mesial, buccal, distal and lingual) using a force-controlled calibrated periodontal probe (Florida Probe®, Florida probe corporation, Gainesville, FL, USA) with a constant probing force of 15 g.
Radiographic evaluation
IOPA radiographs were taken using the long cone paralleling technique and assessed at the time of implant placement, at 3 months, 6 months, 9 months and 12 months (Fig. 5). Exposures, developing and fixing were done by the same operator under standardized protocols. It was ensured that each radiograph showed an undistorted view of the featured implant in their entirety plus at least 5 mm of bone apical to the apex of the implant. A computer loaded with Corel Draw® software was used to analyze the radiographs. The IOPA radiographs were transferred to the computer, enlarged to actual size (known actual implant dimensions) and amount of bone resorption was measured from the crestal bone level to the implant crest module at mesial and distal sites.
Fig. 5.
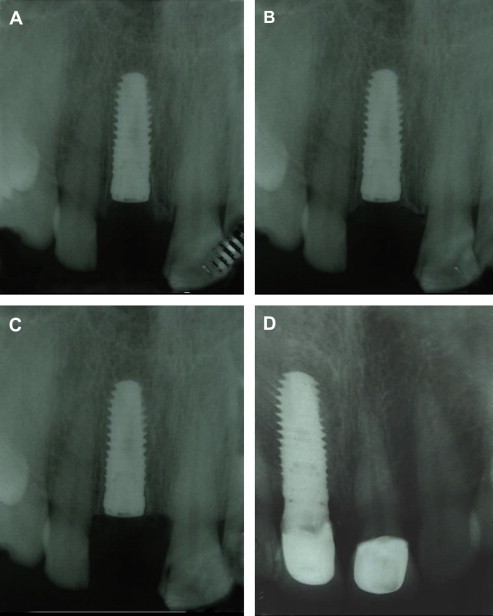
IOPA X-rays: Baseline, 3 months, 6 months and 12 months.
Measurement of implant stability
Periotest (PeriotestS3218®, Medizntechnik, Gulden) was used for measurement of implant stability at 6, 9 and 12 months. The data collected by clinical and radiographic evaluation were subjected to statistical analysis. Intragroup comparisons were made with paired ‘t’ test and intergroup comparison with unpaired ‘t’ test (P > 0.05 NS, ≤0.05 S, ≤0.01 HS).
Results
The Plaque Index and Gingival Index for full mouth as well as the implant sites reduced over a period of 12 months for both the groups indicating a sound healthy mucosa and positive tissue integration around dental implants. Comparison between mean Plaque Index values between group A & group B for different periods and different sites is reflected in Table 1. Comparison between group A and group B with respect to implant was not significant for any period. However with respect to 6 month period the differences between groups were significant (t = 2.01, P = 0.054). Table 2 shows the comparison between mean Gingival Index values between group A & group B for different sites (FM & IMP) from baseline to 12 months. Since all within group comparisons (except one between Implant baseline vs Implant 12M in group B) were not statistically significant, between groups comparisons were made only for 12M period. With respect to FM as well as IMP, the mean Gingival Indices of the two groups were not statistically significant for 12M period. The Mean Gingival Index for group A was 0.901 and for group B 0.845 at the end of 12M period.
Table 1.
Statistical analysis of Plaque Index (group A vs group B).
| Time | Groups | Full mouth (FM) |
Implant (IMP) |
||
|---|---|---|---|---|---|
| Mean PI ± SD | t∗∗P | Mean PI ± SD | t∗∗P | ||
| Baseline | Group A | 0.9133 ± 0.0903 | 0.07 0.943 NS |
0.925 ± 0.103 | 0.71 0.484 NS |
| Group B | 0.911 ± 0.110 | 0.957 ± 0.136 | |||
| 3 Months | Group A | 0.937 ± 0.121 | 1.03 0.312 NS |
0.957 ± 0.130 | 0.91 0.372 NS |
| Group B | 0.892 ± 0.121 | 0.9207 ± 0.0866 | |||
| 6 Months | Group A | 0.936 ± 0.141 | 1.91 0.066 NS |
0.852 ± 0.127 | 2.01 0.054 |
| Group B | 0.8600 ± 0.0627 | 0.937 ± 0.103 | |||
| 9 Months | Group A | 0.8727 ± 0.0949 | 0.43 0.670 NS |
0.8387 ± 0.0955 | 1.02 0.316 NS |
| Group B | 0.855 ± 0.131 | 0.8700 ± 0.0707 | |||
| 12 Months | Group A | 0.8787 ± 0.0954 | 0.13 0.898 NS |
0.846 ± 0.106 | 0.04 0.971 NS |
| Group B | 0.874 ± 0.102 | 0.8473 ± 0.0952 | |||
P > 0.05 NS, ≤0.05 S, ≤0.01 HS.
NS: non significant.
S: significant.
HS: highly significant.
∗ Paired ‘t’ test (intragroup comparisons).
∗∗ Unpaired ‘t’ test (intergroup comparison).
Table 2.
Statistical analysis of Gingival Index (group A vs group B).
| Time | Groups | Full mouth (FM) |
Implant (IMP) |
||
|---|---|---|---|---|---|
| Mean GI ± SD | t∗∗P | Mean GI ± SD | t∗∗P | ||
| 12 Months | Group A | 0.901 ± 0.1671 | 0.91 0.372 NS |
0.825 ± 0.105 | 1.49 0.148 NS |
| Group B | 0.845 ± 0.175 | 0.91 0.372 NS |
0.901 ± 0.167 | 1.49 0.148 NS |
|
P > 0.05 NS, ≤0.05 S, ≤0.01 HS.
NS: non significant.
S: significant.
HS: highly significant.
∗ Paired ‘t’ test (intragroup comparisons).
∗∗ Unpaired ‘t’ test (intergroup comparison).
Comparison between peri-implant sulcular depth values between group A & group B for Implant at different sites and periods of evaluation (6M, 9M & 12M) is shown in Table 3. The table also shows the results of between group comparisons for each site for different periods. Probing depth was also stable throughout the evaluation period and the observations were not statistically significant (P > 0.05 NS). Evaluation of intraoral periapical radiograph of the implant with Corel Draw® software at mesial and distal sites revealed significant decrease in bone height indicating bone remodeling around the implant. Comparison of radiographic evaluation data between group A & group B for different periods is reflected in Table 4. Evaluation of intraoral periapical radiograph of the implant with Corel Draw® software at mesial and distal sites revealed significant decrease in bone height for both the groups indicating bone remodeling around the Implant.
Table 3.
Statistical analysis of peri-Implant sulcular depth values (group A vs group B).
| Groups | Time | Mesial |
Midbuccal |
Distal |
Lingual |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean PD ± SD | t∗∗P | Mean PD ± SD | t∗∗P | Mean PD ± SD | t∗∗P | Mean PD ± SD | t∗∗P | ||
| Group A | 6M | 2.200 ± 0.775 | 0.21 0.836 NS |
1.867 ± 0.834 | 0.21 0.833 NS |
1.400 ± 0.507 | 1.17 0.254 NS |
1.600 ± 0.632 | 0.55 0.590 NS |
| Group B | 2.267 ± 0.961 | 1.933 ± 0.884 | 1.667 ± 0.724 | 1.733 ± 0.704 | |||||
| Group A | 9M | 2.400 ± 0.737 | 0.80 0.432 NS |
2.333 ± 0.816 | 0.44 0.662 NS |
1.933 ± 0.458 | 0.84 0.410 NS |
1.733 ± 0.884 | 0.45 0.657 NS |
| Group B | 2.600 ± 0.632 | 2.467 ± 0.834 | 1.800 ± 0.414 | 1.600 ± 0.737 | |||||
| Group A | 12M | 2.800 ± 0.941 | 0.76 0.456 NS |
2.067 ± 0.961 | 0.55 0.587 NS |
2.067 ± 0.799 | 0.40 0.696 |
2.333 ± 0.816 | 0.44 0.662 NS |
| Group B | 2.533 ± 0.990 | 2.27 ± 1.03 | 1.93 ± 1.03 | 2.467 ± 0.834 | |||||
P > 0.05 NS, ≤0.05 S, ≤0.01 HS.
NS: non significant.
S: significant.
HS: highly significant.
∗ Paired ‘t’ test (intragroup comparisons).
∗∗ Unpaired ‘t’ test (Intergroup comparison).
Table 4.
Radiographic analysis data using Corel Draw® image analysis software on mesial and distal sites.
| Radiographic analysis (mesial) |
Radiographic analysis (distal) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BL | 3M | 6M | 9M | 12M | BL | 3M | 6M | 9M | 12M | |
| Group A | ||||||||||
| 1 | 5.4 | 4.9 | 4.3 | 3.8 | 3.3 | 2.2 | 2 | 1.8 | 1.5 | 1.1 |
| 2 | 4.1 | 3.9 | 3.35 | 2.9 | 2.4 | 3.6 | 3.1 | 2.7 | 2.5 | 2.1 |
| 3 | 4.2 | 4.0 | 3.36 | 3 | 2.5 | 3.9 | 3.7 | 2.8 | 2.4 | 2.2 |
| 4 | 5.8 | 4.2 | 3.9 | 2.9 | 2.4 | 2.9 | 2.4 | 2 | 1.7 | 1.4 |
| 5 | 4.96 | 4.8 | 4.9 | 4.8 | 3.9 | 3.5 | 2.4 | 2.1 | 1.9 | 1.6 |
| 6 | 5.3 | 4.8 | 4.2 | 3.7 | 3.3 | 2.2 | 2 | 1.8 | 1.5 | 1.1 |
| 7 | 4.5 | 3.9 | 3.35 | 2.9 | 2.4 | 3.6 | 3.1 | 2.7 | 2.5 | 2.1 |
| 8 | 4.9 | 4.0 | 3.36 | 3 | 2.5 | 3.9 | 3.7 | 2.8 | 2.4 | 2.2 |
| 9 | 4.7 | 4.4 | 3.7 | 3.3 | 3.2 | 3.2 | 3.4 | 2.6 | 2 | 1.8 |
| 10 | 4.9 | 4.8 | 4.6 | 4.3 | 4.1 | 3 | 2.5 | 2.1 | 1.9 | 1.4 |
| 11 | 4.7 | 4.6 | 4.4 | 4.2 | 4 | 3.2 | 2.8 | 2.4 | 2 | 1.5 |
| 12 | 5 | 4.9 | 4.7 | 4.4 | 4.2 | 3.3 | 2.5 | 2.2 | 1.8 | 1.4 |
| 13 | 9.63 | 9.2 | 6.12 | 5.9 | 5 | 5.6 | 2.1 | 1.9 | 1.1 | 0.91 |
| 14 | 5.5 | 5 | 4.8 | 4.6 | 4.5 | 1.9 | 1.4 | 1 | 0.6 | 0.4 |
| 15 | 7.3 | 6.8 | 6.4 | 5.6 | 5.2 | 4.3 | 3.9 | 3.4 | 3.1 | 2.7 |
| Group B | ||||||||||
| 1 | 4.6 | 3.9 | 3.5 | 3.5 | 3.4 | 2.3 | 2.1 | 2 | 2 | 1.3 |
| 2 | 6.63 | 5.6 | 4.3 | 3.7 | 3.4 | 6.4 | 5.6 | 4.9 | 4.2 | 3.5 |
| 3 | 4.9 | 4.4 | 3.7 | 3.3 | 3.2 | 3.2 | 3.4 | 2.6 | 2 | 1.8 |
| 4 | 5.3 | 4.8 | 4.2 | 3.7 | 3.2 | 2.1 | 1.9 | 1.7 | 1.4 | 1.1 |
| 5 | 4 | 3.8 | 3.25 | 2.8 | 2.3 | 3.4 | 3 | 2.6 | 2.4 | 2 |
| 6 | 4.1 | 3.9 | 3.32 | 3 | 2.4 | 3.8 | 3.6 | 2.7 | 2.3 | 2.1 |
| 7 | 5.7 | 4.1 | 3.8 | 2.8 | 2.3 | 2.8 | 2.3 | 2 | 1.6 | 1.3 |
| 8 | 4.9 | 4.7 | 4.5 | 4.2 | 3.9 | 3.5 | 2.4 | 2.1 | 1.9 | 1.6 |
| 9 | 5.2 | 4.7 | 4.3 | 3.7 | 3.3 | 2.2 | 2 | 1.8 | 1.5 | 1.1 |
| 10 | 4.8 | 3.9 | 3.45 | 2.8 | 2.4 | 3.6 | 3.1 | 2.7 | 2.5 | 2.1 |
| 11 | 5.2 | 4.9 | 4 | 3.7 | 3 | 3.9 | 3.7 | 2.8 | 2.4 | 2.2 |
| 12 | 4.6 | 4.3 | 3.6 | 3.3 | 3.1 | 3 | 3.2 | 2.5 | 2 | 1.8 |
| 13 | 4.9 | 4.8 | 4.6 | 4.3 | 4.1 | 3 | 2.5 | 2.1 | 1.9 | 1.4 |
| 14 | 4.7 | 4.6 | 4.4 | 4.2 | 4 | 3.2 | 2.8 | 2.4 | 2 | 1.5 |
| 15 | 5 | 4.9 | 4.7 | 4.4 | 4.2 | 3.3 | 2.5 | 2.2 | 1.8 | 1.4 |
Comparison of Periotest values between group A & group B for implant sites for 6M, 9M and 12M periods was not statistically significant. The mean Periotest value and Standard Deviation for implant at, 6 months, 9 months and 12 months were −2.13 ± 1.19 (group A), −2.20 ± 1.57(group B); −2.27 ± 1.71 (group A), −0.47 ± 2.26 (group B); 2.20 ± 1.42 (group A), −2.87 ± 1.41 (group B). The t value and P value of group A vs group B for 6M, 9M and 12M period were 0.13, 0.897; 0.64, 0.113; 1.29, 0.208 respectively.
Discussion
The advent of osseointegration and advances in biomaterials and techniques has contributed to increased application of dental implants in the restoration of partial and completely edentulous patients. Immediate implant placement after extraction has become a favored treatment protocol with many clinicians worldwide. Placement of an implant directly into a prepared extraction socket at the time of extraction has several advantages that have the potential to improve patient acceptance of the procedure. The advantages are elimination of the waiting period for socket ossification, fewer surgical sessions required, shortened edentulous time period, reduced overall cost, preservation of alveolar bone height and width, decreased operatory time with less trauma to the tissues and less discomfort to the patient. By using the extraction site that follows the natural long axis of the tooth, easier implant orientation and better prosthodontic rehabilitation can be achieved. Several authors have reported placement of implants into extraction sockets.8–11
Although the immediate implant placement is very a reliable and predictable procedure, it is very difficult to select an implant exactly matching the dimensions of the extracted socket. Inspite of advances in the design technologies and clinical expertise the horizontal defect dimensions (HDD) or so called ‘jumping distance’ needs to be filled with a graft material for primary stability and better osseointegration. A bone graft is a tissue or material used to repair a defect or deficiency in contour and/or volume. There is a diversity of opinion regarding what graft materials should be used for typical clinical applications, the rationale for their use, the rationale for using combinations of materials, and the percentages of each material used in combination. Various types of biocompatible graft materials have been widely used in bone regeneration procedures prior to implant placement. The autograft, allograft, alloplast, and xenograft materials all have reported success, alone or in combination for bone augmentation.5,6
As a result of the advancement in biotechnology, cell biology, and molecular biology, the conventional method of harvesting a large amount of autogenous bone graft with potential clinical hazards has already been challenged and replaced by more scientific methods such as the DFDBA, HA, concentrated plasma derived growth factor (PDGF), recombinant osteogenic growth factor, BMP or ‘in- vitro’ cultured pluripotential osteogenic cells. Among the materials listed before DFDBA12,13 and HA14,15 have been extensively used in implant dentistry. A matter of controversy in implant dentistry concerns what is the most appropriate bone substitute for ridge preservation and to manage the so called ‘jumping distance’ in immediate extraction and implant placement. A number of graft materials have been reported in the literature for bone augmentation. Since little has been reported to date to give any insight as to whether such grafts can support functioning dental implants, this study was undertaken to evaluate the success of immediate implants in fresh extraction sites and to compare two graft materials (modified hydroxyapatite vs Demineralized freeze-dried bone) in such procedures.
Modified Plaque Index and modified Gingival Index are recommended for the evaluation of oral hygiene practices and the status of the peri-implant mucosa.16 According to our results, the mean Plaque Index for full mouth and implant, for both groups decreased from baseline, to 3 months, 6 months, 9 months and 12 months (Table 1). This can be attributed to the plaque control by the patient and the repeated reinforcements of oral hygiene measures given to the patient by the clinician. However the reduction was not statistically significant for most of the comparisons (P > 0.05). The reductions in Plaque Indices were comparable for both implant and full mouth in both groups. This is in similarity to the earlier conducted studies17,18 where, there have been reductions in the plaque indices. As far as Gingival Index is concerned, since all within group comparisons (except one between implant baseline vs Implant 12M in group B) were not statistically significant, between groups comparisons were made only for 12M period. With respect to full mouth as well as implant, the mean Gingival Indices of the two groups were not statistically significant for 12M period. The Mean Gingival Index for group A was 0.901 and for group B 0.845 at the end of 12M period. Overall when we analyzed the data in group A as well as group B, the mean Gingival Indices have shown intermittent fluctuations without any statistical significance (P > 0.05) (Table 2). This may be due to the fact the patient oral hygiene maintenance measures differed between different periods. That reflects patient's neglect toward oral hygiene protocols. Similar findings were found in other studies.17,18
Peri-implant probing is a crucial procedure in diagnosis of the periodontium and therefore evaluation of maintenance phase of periodontal therapy. In our study peri-implant sulcular depths at mesial, buccal, distal and lingual sites for both group A and group B increased from 6 months to 9 months and then to 12 months (Table 3). However none of these increases were suggestive of inflammation. Similar observations were made by researchers in the earlier study17,18 wherein probing depths have increased, due to the fact that implants have been placed 1 or 2 mm below the level of the alveolar crest.
After subjecting the results of radiographic evaluation to statistical analysis, it was found that statistically highly significant bone resorption occurred on both mesial and distal sites. This is in similarity to the studies conducted by other researchers.19,20 But when comparisons were made between the groups, the results were not statistically significant (P > 0.05). Based on these findings, either or both of them may be considered for immediate extraction and implant procedures. The use of Periotest for evaluation of implant stability was recommended by many authors21,22 and our study also proved that it can be a valuable diagnostic tool. The results of our study also indicated negative values and the implants were well osseointegrated in both the groups (Fig. 6).
Fig. 6.

Results of periotest evaluation.
According to our study immediate implant survival rate is 100% during 1 year follow-up. Same results were found with respect to immediate implants in extracted socket during 1st year of study.23–26 However, other study reported 95% success rates with 5% failures in the 1st year of their study.20 Thus, with regard to implant survival, there seems to be no reason to refrain from immediate placement of implants into extraction sockets. In our study both DFDBA and HA produced equally good results. This is in agreement with other study conducted by Boëck-Neto et al.27 The results of their study indicated that both DFDBA and HA associated with an autogenous bone graft were biocompatible and promoted osteoconduction, acting as a matrix for bone formation. Although there are a great number of scientific investigations behind delayed placement and loading, a high proportion of the hardware and software preferences are based on empirical data only. We have simply learned to follow a certain protocol. It is indeed reasonable to challenge the osseointegrated protocol provided this is done in a scientifically controlled manner. Obviously, more basic science is needed to learn more about optimal timing of placement of implants into extraction sockets and their loading. Immediate placement of single tooth implants into fresh extraction sockets could be considered a valuable option to replace a hopeless tooth.
Many different techniques exist for effective bone augmentation during implant placement. The approach is largely dependent on the extent of the defect and specific procedures to be performed for the implant reconstruction. It is most appropriate to use an evidenced-based approach when a treatment plan is being developed for bone augmentation cases. However, further clinical and histologic studies are needed to better understand the healing pattern of these biomaterials in relationship with dental implants positioned in grafted sites with bone substitutes.
Funding
This study has been funded by research grants from O/o DGAFMS, New Delhi.
Conflicts of interest
All authors have none to declare.
References
- 1.Adell R., Ericsson B., Lekholm U., Branemark P.I., Jemt T. A long-term follow up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5:347–359. [PubMed] [Google Scholar]
- 2.Schulte W. The intraosseous Al2O3 (Frialit) Tubingen implant. Developmental status after eight years (I–III) Quintessence Int. 1984;15:19–35. [Google Scholar]
- 3.Annerroth G., Hedstrom K., Kjellman O., Kondell P.A., Nordenram A. Endosseous titanium implants in extraction sockets. An experimental study in monkeys. Int J Oral Surg. 1985;14(1):50–54. doi: 10.1016/s0300-9785(85)80010-7. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz-Arad D., Chaushu G. Immediate implant placement: a procedure without incisions. J Periodontol. 1998;69(7):743–750. doi: 10.1902/jop.1998.69.7.743. [DOI] [PubMed] [Google Scholar]
- 5.Schropp L., Kostopoulos L., Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: a prospective clinical study. Int J Oral Maxillofac Implants. 2003;18(2):189–199. [PubMed] [Google Scholar]
- 6.Block M.S., Kent J.N. Placement of endosseous implants into tooth extraction sites. J Oral Maxillofac Surg. 1991;49(12):1269–1276. doi: 10.1016/0278-2391(91)90302-3. [DOI] [PubMed] [Google Scholar]
- 7.Paolantonio M., Dolci M., Scarano A. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontol. 2001;72(11):1560–1571. doi: 10.1902/jop.2001.72.11.1560. [DOI] [PubMed] [Google Scholar]
- 8.Barone A., Cornelini R., Ciaglia R., Covani U. Implant placement in fresh extraction sockets and simultaneous osteotome sinus floor elevation: a case series. Int J Periodontics Restorative Dent. 2008;28(3):283–289. [PubMed] [Google Scholar]
- 9.Tolman D.E., Keller E.E. Endosseous implant placement immediately following dental extraction and alveoloplasty: preliminary report with 6-year follow up. Int J Oral Maxillofac Implants. 1991;6(1):24–28. [PubMed] [Google Scholar]
- 10.Lang N.P., Bragger U., Hammerle C.H., Sutter F. Immediate transmucosal implants using the principle of guided tissue regeneration. I. Rationale, clinical procedures and 30-month results. Clin Oral Implants Res. 1994;5(3):154–163. doi: 10.1034/j.1600-0501.1994.050306.x. [DOI] [PubMed] [Google Scholar]
- 11.Bragger U., Hammerle C.H., Lang N.P. Immediate transmucosal implants using the principle of guided tissue regeneration (II). A cross-sectional study comparing the clinical outcome 1 year after immediate to standard implant placement. Clin Oral Implants Res. 1996;7(3):268–276. doi: 10.1034/j.1600-0501.1996.070309.x. [DOI] [PubMed] [Google Scholar]
- 12.Becker W., Urist M.R., Tucker L.M., Becker B.E., Ochsenbein C. Human demineralized freeze-dried bone: inadequate induced bone formation in athymic mice. A preliminary report. J Periodontol. 1995;66(9):822–828. doi: 10.1902/jop.1995.66.9.822. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz Z., Mellonig J.T., Carnes D.L., Jr. Ability of commercial demineralized freeze-dried bone allograft to induce new bone formation. J Periodontol. 1996;67:918–926. doi: 10.1902/jop.1996.67.9.918. [DOI] [PubMed] [Google Scholar]
- 14.Holmes R.E., Hagler H.K. Porous hydroxyapatite as a bone graft substitute in cranial reconstruction: a histometric study. Plast Reconstr Surg. 1988;81(5):662–671. doi: 10.1097/00006534-198805000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Hupp J.R., McKenna S.J. Use of porous hydroxylapatite blocks for augmentation of atrophic mandibles. J Oral Maxillofac Surg. 1988;46(7):538–545. doi: 10.1016/0278-2391(88)90143-7. [DOI] [PubMed] [Google Scholar]
- 16.Mombelli A., van Oosten M.A.C., Schurch E. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2(4):145–151. doi: 10.1111/j.1399-302x.1987.tb00298.x. [DOI] [PubMed] [Google Scholar]
- 17.Kan J.Y.K., Rungcharassaeng K., Lozada J. Immediate placement and provisionalization of maxillary anterior single implants. 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18:31–39. [PubMed] [Google Scholar]
- 18.Gomez-Roman G., Schulte W., d'Hoedt B., Axman-Krcmar D. The frialit-2 implant system: five year clinical experiences in single tooth and immediately postextraction applications. Int J Oral Maxillofac Implants. 1997;12(3):299–309. [PubMed] [Google Scholar]
- 19.Ludlow J.B., Nason R.H., Jr., Hutchens L.H., Jr., Moriarty J. Radiographic evaluation of alveolar crest obscured by dental implants. Implant Dent. 1995;4(1):13–18. doi: 10.1097/00008505-199504000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz-Arad D., Yaniv Y., Levin L., Kaffe I. A radiographic evaluation of cervical bone loss associated with immediate and delayed implants placed for fixed restorations in edentulous jaws. J Periodontol. 2004;75(5):652–657. doi: 10.1902/jop.2004.75.5.652. [DOI] [PubMed] [Google Scholar]
- 21.Truhlar R.S., Morris H.F., Ochi S., Winkler S. Assessment of implant mobility at second stage surgery with the periotest: DICRG interim report no 3. Implant Dent. 1994;3(3):153–156. doi: 10.1097/00008505-199409000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Zahran Amr, Samy Hisham, Mostafa Basma, Rafik Ramy. Evaluation of two different implant designs for immediate placement and loading in fresh extraction sockets. J Am Sci. 2010;6(12):1192–1199. [Google Scholar]
- 23.Cornelini R., Scarano A., Covani U., Petrone G., Piattelli A. Immediate one stage postextraction implant: a human clinical and histologic case report. Int J Oral Maxillofac Implants. 2000;15(3):432–437. [PubMed] [Google Scholar]
- 24.Schwartz-Arad D., Chaushu G. The ways and wherefores of immediate placement of implants into fresh extraction sites: a literature review. J Periodontol. 1997;68(10):915–923. doi: 10.1902/jop.1997.68.10.915. [DOI] [PubMed] [Google Scholar]
- 25.Iasella J.M., Greenwell H., Miller R.L. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990–999. doi: 10.1902/jop.2003.74.7.990. [DOI] [PubMed] [Google Scholar]
- 26.Becker W., Clokie C., Sennerby L., Urist M.R., Becker B.E. Histologic findings after implantation and evaluation of different grafting materials and titanium micro screws into extraction sockets: case reports. J Periodontol. 1998;69(4):414–421. doi: 10.1902/jop.1998.69.4.414. [DOI] [PubMed] [Google Scholar]
- 27.Boëck-Neto R.J., Gabrielli M., Lia R., Marcantonio E., Shibli J.A., Marcantonio E., Jr. Histomorphometrical analysis of bone formed after maxillary sinus floor augmentation by grafting with a combination of autogenous bone and demineralised freeze dried bone allograft or hydroxyl apatite. J Periodontol. 2002;73(3):266–270. doi: 10.1902/jop.2002.73.3.266. [DOI] [PubMed] [Google Scholar]


