Abstract
Background
Although interpersonal violence (“assault”) exists in every society, the World Health Organization (WHO) estimated that 90 % of the exposure burden occurs in low- and middle-income countries. The objectives of this study were to define the incidence of assault-related injuries among subjects presenting for emergency room care secondary to sustained trauma in Lilongwe, Malawi; to measure the impact of sex on incidence, injury type, and care received; and to measure the effect of both sex and geographic location of the injury on time to presentation for medical care.
Methods
This is a retrospective cohort analysis of data prospectively collected in the Kamuzu Central Hospital Trauma Surveillance Registry from July 2008 to December 2010 (n = 23,625). We used univariate, bivariate, and logistic regression analyses to measure association of sex with variables of interest, and geospatial mapping to evaluate the association of location of assault on time to presentation for care.
Results
The mean age of our trauma cohort was 27.7 years. Assaults accounted for 26.8 % of all injuries. Of those assaulted, 21.0 % (1299) were female, who were younger (26.2 vs. 28.1 years, p < 0.001), more likely to arrive to the hospital by minibus (p < 0.001), and less likely to arrive by police (p < 0.001). Altogether 62 % of the females were assaulted in their homes—much more often than their male counterparts (p < 0.001). Females were more likely to sustain contusions (p < 0.001) and males more likely to have lacerations and penetrating stab wounds (p < 0.001) or head injury (p < 0.001). Females had delayed hospital presentation following assault (p = 0.001) and were more likely to be treated as outpatients after adjusting for age, injury type, and injury location (adjusted odds ratio 1.74, 95 % CI 1.3–2.3, p < 0.001). Assaults clustered geographically in the Lilongwe district. Delayed presentation of females occurred irrespective of proximity to the hospital.
Conclusions
This study brings attention to sex differences in assault victims. A prevention strategy focusing on sex roles and domestic abuse of women is paramount. Efforts are needed to stop dischargin female assault victims back into a potentially unsafe, abusive environment.
Introduction
Interpersonal violence is a worldwide phenomenon. The World Health Assembly and the World Health Organization (WHO) have declared it a major public health issue, particularly in vulnerable populations such as women, children, and the poor [1, 2]. The WHO estimates that 1.6 million people die annually from acts of violence, and millions more suffer nonfatal injuries [3-5]. An estimated 4,400 people die every day because of intentional acts of violence, categorized as self-directed, interpersonal, or collective, with 90 % of these occurring in low- and middle-income countries (LMICs). The associated violence-related mortality and morbidity in LMICs is 2.5 times higher than in high-income countries [1, 3, 6].
In sub-Saharan Africa, violence-related injury rates range from 22.5 % in Cameroon to 48.0 % in Ethiopia, often constituting the most common mechanism of all injuries presenting to health care facilities [7-9]. In South Africa, the burden of injury attributable to interpersonal violence is estimated at 1.0 million disability adjusted life years, and this does not account for the psychosocial and long-term health sequelae [1, 5, 6, 10, 11].
The paucity of accurate data, compounded by the associated stigma of self-reporting, particularly in LMICs, creates challenges in the measurement of the true impact of violence in health and economic terms. Hence, available data are likely to underestimate the magnitude of the problem [9].
The objectives of this study were to (1) define the incidence of assault-related injuries among subjects presenting for emergency room care secondary to sustained trauma in Lilongwe, Malawi; (2) measure the impact of sex on incidence, injury type, and care received; and (3) measure the effect of both sex and geographic location of the injury on the time to presentation for medical care.
Methods
This study encompasses a secondary analysis of prospectively collected hospital-based trauma registry data that had been described previously [12]. We included all subjects who presented to the Kamuzu Central Hospital (KCH) Emergency Department with assault-related trauma between July 2008 and December 2010. Malawian clerks collected demographic and injury-specific data at the time of admission (Table 1) including residence location (i.e. the area and district of residence of the injured patient). Injury setting includes the setting where the assault took place and is defined as the home, road/street, public building, work, school, other. We also recorded the area/district/village where the assault occurred. Date and time of day and the type of injury were recorded. Injury type was defined as laceration, contusion, abrasion, stab/penetrating, or fracture. Injury location was the variable used to designate the body location encompassing the primary site of the injury. Occupation, age, and sex of the patient are self-explanatory. Mode of transportation to the hospital included police, ambulance, personal vehicle, minibus, motorcycle, bicycle, or on foot. Disposition from the emergency room was defined as discharged from casualty, admitted to floor bed, admitted to high density unit, admitted to intensive care unit, died in casualty department, or brought in dead. Both the University of North Carolina (UNC) institutional review board and the National Health Sciences Research Committee of Malawi (NHSRC) approved this study.
Table 1.
Sex-based characteristics of the study cohort
| Characteristic | Total (n = 6184) | Male (n = 4869) | Female (n = 1299) | p |
|---|---|---|---|---|
| Age (years), mean | 27.7 | 28.1 | 26.2 | <0.001* |
| Occupation | ||||
| Small business owner | 19.2 % (1184) | 19.6 % (954) | 17.6 % (229) | 0.01 |
| Casual laborer | 18.0 % (1112) | 20.8 % (1012) | 7.5 % (98) | <0.001 |
| Unemployed | 11.1 % (689) | 9.5 % (462) | 17.4 % (226) | <0.001 |
| Student | 10.6 % (654) | 10.0 % (485) | 12.9 % (168) | 0.001 |
| Housewife | 5.7 % (355) | 0.3 % (15) | 26.1 % (339) | <0.001 |
| Twoa | 5.3 % (327) | 6.5 % (318) | 0.6 % (8) | <0.001 |
| Zerob | 3.9 % (241) | 4.1 % (197) | 3.2 % (42) | 0.006 |
| Others | 22.2 % (1372) | 25.2 % (1227) | 10.2 % (132) | |
| Missing | 4.0 % (250) | 4.0 % (194) | 4.5 % (59) | |
| Transport | ||||
| Private vehicle | 47.7 % (2950) | 48.3 % (2355) | 45.3 % (588) | 0.06 |
| Mini-bus | 21.6 % (1334) | 19.5 % (947) | 29.5 % (383) | <0.001 |
| Police | 10.6 % (655) | 11.5 % (561) | 7.2 % (94) | <0.001 |
| Walked | 7.6 % (470) | 7.4 % (362) | 8.2 % (107) | 0.3 |
| Ambulance | 7.6 % (468) | 7.7 % (375) | 7.0 % (91) | 0.4 |
| Others | 3.8 % (235) | 4.6 % (223) | 1.4 % (18) | |
| Missing | 1.1 % (67) | 1.0 % (47) | 1.4 % (18) | |
| Time to presentation (h) | 3.33 ± 97.6 | 3.18 ± 106.6 | 3.78 ± 53.0 | <0.001** |
| Alcohol use | 22.9 % (1413) | 25.6 % (1238) | 13.6 % (175) | <0.001 |
| Injury type | ||||
| Laceration | 50.9 % (3149) | 54.7 % (2662) | 36.8 % (478) | <0.001 |
| Contusion | 28.9 % (1785) | 24.5 % (1194) | 45.2 % (587) | <0.001 |
| Abrasion | 5.6 % (345) | 5.7 % (277) | 5.2 % (68) | 0.6 |
| Penentrating stab | 5.1 % (316) | 5.7 % (278) | 2.9 % (38) | <0.001 |
| Fracture | 4.2 % (258) | 4.3 % (208) | 3.9 % (50) | 0.5 |
| Others | 3.3 % (204) | 3.3 % (161) | 3.2 % (42) | |
| Missing | 2.0 % (126) | 1.8 % (88) | 2.8 % (36) | |
| Injured body part | ||||
| Head or skull | 32.4 % (2001) | 34.6 % (1683) | 24.2 % (314) | <0.001 |
| Face | 21.8 % (1350) | 21.7 % (1055) | 22.4 % (291) | 0.4 |
| Other | 6.2 % (386) | 6.5 % (314) | 5.5 % (72) | 0.3 |
| Chest/T-spine | 6.2 % (381) | 5.8 % (281) | 7.6 % (99) | 0.01 |
| Hand | 4.6 % (284) | 4.6 % (222) | 4.7 % (61) | 0.8 |
| Abdomen/L-spine | 3.2 % (198) | 2.7 % (132) | 5.1 % (66) | <0.001 |
| Forearm | 3.1 % (194) | 2.9 % (142) | 4.0 % (52) | 0.04 |
| Shoulder/clavicle | 2.9 % (176) | 2.7 % (131) | 3.4 % (44) | 0.2 |
| Lower leg | 2.8 % (174) | 2.9 % (139) | 2.7 % (35) | 0.8 |
| Upper arm | 2.6 % (159) | 2.7 % (129) | 2.3 % (30) | 0.5 |
| Neck/C-spine | 2.4 % (149) | 2.0 % (95) | 4.2 % (54) | <0.001 |
| Others | 9.4 % (581) | 8.8 % (428) | 10.6 % (138) | |
| Missing | 2.4 % (146) | 2.1 % (101) | 3.3 % (43) | |
| Injury setting | ||||
| Home | 34.1 % (2109) | 26.7 % (1302) | 62.0 % (805) | <0.001 |
| Road/street | 29.6 % (1830) | 34.0 % (1655) | 12.8 % (166) | <0.001 |
| Public building | 10.9 % (671) | 11.9 % (578) | 7.2 % (93) | <0.001 |
| Work | 9.2 % (569) | 10.9 % (532) | 2.8 % (36) | <0.001 |
| Sport/recreation | 2.4 % (146) | 2.7 % (130) | 1.2 % (16) | 0.003 |
| School | 1.1 % (70) | 1.1 % (55) | 1.2 % (15) | 0.9 |
| Others | 4.3 % (266) | 4.7 % (229) | 3.0 % (39) | |
| Missing | 8.4 % (521) | 8.0 % (390) | 9.8 % (127) | |
| Disposition | ||||
| Outpatient | 86.6 % (5345) | 85.5 % (4161) | 91.1 % (1183) | <0.001 |
| Admitted | 10.5 % (647) | 11.3 % (550) | 7.2 % (93) | <0.001 |
| Died prior to admission | 0.8 % (49) | 0.9 % (46) | 0.2 % (3) | 0.01 |
| Missing | 2.2 % (134) | 2.3 % (112) | 1.5 % (20) |
Student’s t test
Wilcoxon rank-sum test
Describes the occupation of bus driver or bus conductor
Describes the occupation of peasant farmer
Statistical analysis
We performed univariate and bivariate analyses of the following variables of interest: subject’s sex, employment status, geographic residence, geographic setting of the injury, anatomic location of the injury, injury type, and clinical disposition (defined as admitted or discharged). Pearson’s χ2, Student’s t test, and the Wilcoxon rank-sum tests were used for statistical analyses where appropriate. Logistic regression was used to examine the relation between sex and discharge from the hospital, adjusting for the variables identified to be potential confounders in our bivariate analysis. The variables included in our model were age, injury type, injury location (anatomic), and injury setting (geographic). Result are reported as the odds ratio (OR) and 95 % confidence interval (CI), with p < 0.05 considered statistically significant (Stata 11; Stata, College Station, TX, USA).
Geographic basis and spatial analysis
Finally, to examine the association between geographic location of the injury and time to presentation for medical care, assault data were grouped according to geographic area and incorporated into an existing geographic information system of Lilongwe District. Lilongwe city is divided into administrative wards and rural Lilongwe is divided into Traditional Authorities (TAs), both referred to as areas. Geospatial maps were generated to examine qualitatively the distribution of assaults for both males and females across Lilongwe district.
Results
Of the 23,625 subjects included in the trauma registry during the study period, 6,184 patients (26.8 %) met inclusion criteria for our analysis. There were 4,869 males (78.7 %) and 1,299 females (21.0 %) (Table 1).
Injury environment
Female subjects were significantly more likely to be housewives (26.2 %), followed by small business owners (17.6 %), unemployed (17.4 %), or students (12.9 %). Of the subset identified as students, females were significantly more likely to be assaulted (12.9 vs. 10.0 %, p = 0.001), and a significantly larger percent of unemployed females were assaulted than unemployed males (17.4 vs. 9.5 % p < 0.001).
Female subjects were significantly more likely to be assaulted in their homes than men [62.0 vs. 26.7 %; odds ratio (OR) 5.35, confidence interval (CI) 4.60–6.20, p < 0.001], and less likely to be assaulted on the road (12.8 vs. 34.0 %; OR 0.28, CI 0.24–0.34, p < 0.001), in a public building (7.2 vs. 11.9 %; OR 0.58, CI 0.46–0.73, p < 0.001), or at work (2.8 vs. 10.9 %; OR 0.24, CI 0.16–0.33, p < 0.001).
Overall, most subjects arrived at the hospital by private vehicle (47.7 %), evenly distributed between males and females. In contrast, female subjects were significantly more likely to be transported to the hospital by minibus (public transportation) (29.5 vs. 19.5 %; OR 1.75, CI 1.41–2.23, p < 0.001) and less likely by police (7.2 vs. 11.5 %; OR 0.60, CI 0.47–0.76, p < 0.001) than females. Males were more likely to present at the hospital earlier than females (3.2 vs. 3.8 h, p < 0.001), and there was a significantly longer time to presentation for women who were assaulted in the home compared with other assault victims (4.0 vs. 3.1 h, p < 0.001).
Injury types, location, and disposition
The most common injuries were lacerations (50.9 %), which were significantly less common in females than males (36.8 vs. 54.7 %; OR 0.48, CI 0.43–0.55, p < 0.001), followed by contusions (28.9 %), which were significantly more common in females than males (45.2 vs. 24.5 %; OR 2.6, CI 2.3–3.0, p < 0.001). The majority of injuries involved the head and face (54.2 %), and males had a higher percentage of injuries to the head (34.6 vs. 24.2 %; OR 2.21, CI 1.54–3.14, p < 0.001), whereas females had a higher percentage of injuries to the chest (7.6 vs. 5.8 %; OR 1.37, CI 1.07–1.74, p = 0.01), abdomen (5.1 vs. 2.7 %; OR 1.94, CI 1.42–2.66, p < 0.001), and neck (4.2 vs. 2.0 %; OR 2.21, CI 1.54–3.14, p < 0.001).
Only 10.5 % (n = 647) of subjects were admitted to the hospital. Females were significantly more likely to be discharged from the emergency department than males (91.1 vs. 85.5 %; OR 1.77, 95 % CI 1.41–2.23, p < 0.001).
Multivariate logistic regression model
After adjusting for age, injury setting, injury type, and body location, females remained significantly more likely to be discharged from the emergency department than male subjects [adjusted OR (AOR) 1.91, CI 1.43–2.54, p < 0.001].
Geographic distribution
The majority of reported cases occurred within Lilongwe district, with 10 female assaults and 59 male assaults reported from other districts. Geographic location of assault was unavailable for 30 % of the cohort, and residential area was unavailable for 28 %. All maps represent assaults as delineated by their location (area) of occurrence.
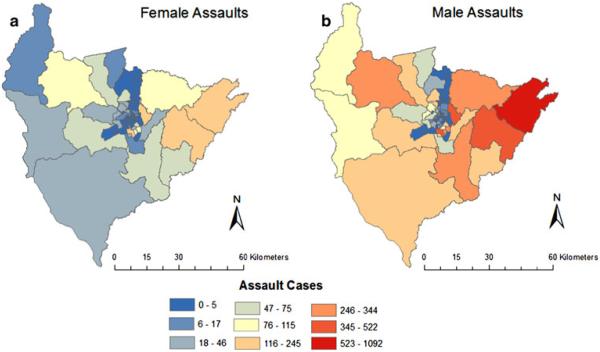
Both male and female assaults occurred in most areas. The concentration of assaults varied spatially, with the highest counts occurring in Lilongwe city (Fig. 1). There were spatial similarities between high male and female assault rates. Two areas had male and female assault rates of 50 or more assaults per 1,000 people. One area had a male assault rate of ≥50 per thousand males and ≥20 per thousand females.
Fig. 1.
Distribution of assaults on female and male patients in the areas in and around Lilongwe
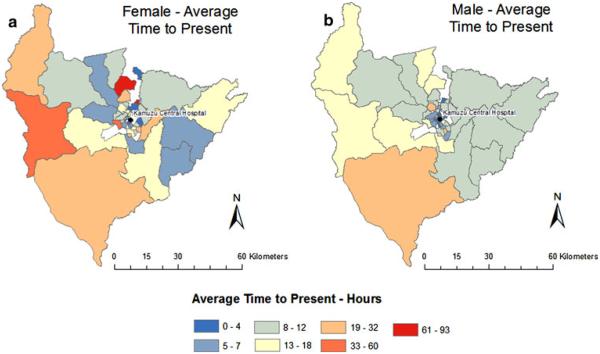
The area-level average time to presentation for female and male assaults was also compared (Fig. 2). There is a striking difference between female and male average times to presentation. Most notable were two areas with an average of >100 h for female assault victims to present at the hospital, whereas the average time for males never exceeded 100 h. The average time to presentation for male assaults was highest at approximately 50 h. Two areas with prolonged time to presentation, taking >50 and >20 h, respectively, were adjacent to the area where KCH is located.
Fig. 2.
Geospatial distribution of female and male patients with respect to time between injury and presentation to the hospital
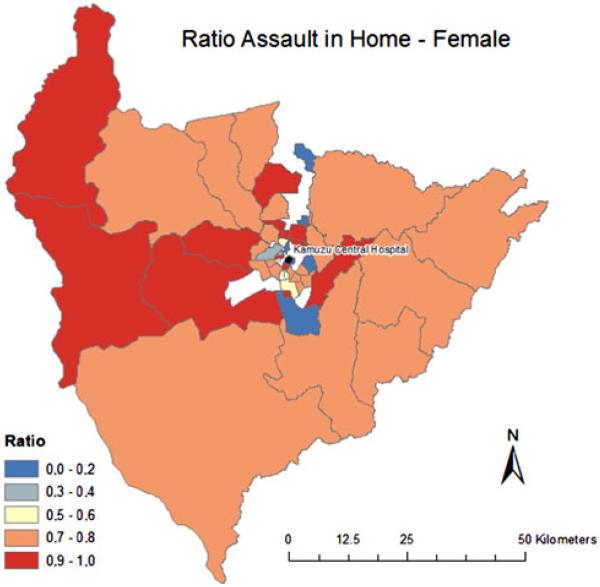
The ratio of female assaults occurring in the home/total female assaults was >0.5 for most areas with a reported case (Fig. 3). High ratios occurred in both rural and urban areas and appeared to cluster geographically. However, it should also be noted that half of the areas with a ratio of 1.0 reported a single assault. Despite this limitation, the spatial patterns of high ratios of assaults in the home suggest that further spatial analysis to characterize the significance of these clusters could shed light on neighborhood effects.
Fig. 3.
Map of Lilongwe areas shows the ratio of female assaults that occurred in the home compared to the total number of female assaults
Discussion
This study highlights the poignant differences in assault patterns between males and females in Malawi. Similar to other studies within this region, assault was the second-most common mechanism of trauma injuries, and there was a male predominance in patients presenting with assault-related injuries [7-9, 13-15].
In our study population, 62 % of women were assaulted at home versus only 27 % of males. This finding suggests intimate partner violence (IPV), a reality of the abuse and suffering endured by women in LMICs, specifically in sub-Saharan Africa. IPV is the most common type of violence against women, with data indicating that between 10 and 75 % of women report having been physically assaulted by an intimate partner during their lifetime [1, 5, 6, 11]. In South Africa and Egypt, nearly half of all murders of females are associated with IPV, representing the highest mortality rate from IPV in the world [2, 5, 10].
Factors associated with increased risk of IPV correlate with the presence of sociocultural norms that allow tolerance of subordination of women, early sexual intercourse and marriage for girls, increased parity, and polygamous relationships amidst extreme poverty [11, 15-17]. In Malawi, 34 % of mothers are teenagers, the average number of children per mother ranges from 7.7 (lowest wealth quartile) to 4.4 in the wealthiest quartile, and 20 % of women marry into a polygamous relationship [3, 15, 18]. In Malawi, one in five women experience physical IPV, one in ten experience sexual or emotional IPV, and 70 % of Malawian women consider violence against women to be a serious problem in their community [11]. However, only 17–27 % of Malawian women know the illegality of various types of abuse. When surveyed, 30 % of women and 20 % of men justify the abuse of women for reasons such as burning food and neglecting the children [11, 19].
As with all forms of violence, the consequences of IPV are more far reaching than the direct morbidity and mortality they cause, leading to psychological and behavioral problems and chronic medical conditions. They propagate a cycle of abusive behavior, thus increasing health care costs and economic losses due to decreased productivity [1, 20].
Role of the health care provider
Victims of IPV are more likely to report abuse to a health care provider than to the police [9, 11, 21-24]. In LMICs, only 4–25 % of female victims report the abuse to police, and only 7 % of those cases result in custodial sentences [11, 25]. Health care providers are uniquely positioned to intervene and attenuate the cycle of abuse. Hence, they should be trained to screen, identify, and treat IPV as part of a comprehensive violence prevention and management plan [1, 11]. We found that almost all of our female patients were immediately discharged home—back into the same environment where the initial assault occurred. The lack of services directed toward identifying and preventing IPV indicates a distinct unmet need at KCH.
Effects of community
Based on our geospatial mapping analysis, there were areas in Lilongwe with significantly high ratios of women assaulted in their homes. Geographic concentrations of poverty are associated with family disruption, community disorganization, and increased levels of unemployment as well as social acceptance of violence [2, 10, 19, 26, 27]. Therefore, evaluating the location of violent acts highlights an opportunity for targeted injury prevention programs that address the determinants of interpersonal violence. Specific health system changes that need to be implemented include strengthening the social support services for victims and focusing on community education in places where the risk of IPV is likely.
Limitations
Our data are hospital-based, making it difficult to calculate total burden of disease from intentional injuries. We also had to contend with missing data for our geospatial analysis. Therefore, this analysis presents merely a guide for future geospatial research that could lead toward more community-based interventions. However, the clear geographic patterns of the incidence of abuse, as well as the delay in presentation, warrant further investigation, which is currently ongoing at our institution.
Conclusions
The issue of IPV must resonate at the highest level of government in sub-Saharan African countries, This is particularly needed in a country such as Malawi, where President Joyce Banda—herself a survivor of a physically abusive marriage and long-time women’s rights activist and leader—has taken over the reigns of government [28-31].
Violence, including domestic violence, deprives women of their ability to achieve their full potential by threatening their safety, freedom, and autonomy. It will be difficult to alleviate global poverty and ultimately improve human heath indices unless women are empowered. Reducing rates of IPV requires multilevel prevention strategies and approaches that emphasize the education of the populace, particularly women, while recognizing the differing interests, live realities, and contradictions among women of different social class, religious, and cultural backgrounds [1]. Furthermore, as health care providers we must identify victims by actively screening cases of suspected IPV and utilize surveillance data and geospatial analysis to inform health and legislative policy—setting priorities to ensure effective allocation of limited resources [5].
References
- 1.Krug E, Mercy J, Dahlberg L, et al. The world report on violence and health. Lancet. 2002;360:1083–1088. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 2.Mercy J, Butchart A, Rosenberg M, et al. Preventing violence in developing countries: a framework for action. Int J Inj Contr Saf Promot. 2008;15:197–208. doi: 10.1080/17457300802406955. [DOI] [PubMed] [Google Scholar]
- 3.WHO WHO Cooperation Strategy 2008–2013. 2012 Available at http://www.who.int/countryfocus/cooperation_strategy/ccs_mwi_en.pdf. Accessed June 2012.
- 4.Dahlberg L, Butchart A. State of the science: violence prevention efforts in developing and developed countries. Int J Inj Contr Saf Promot. 2005;12:93–104. doi: 10.1080/15660970500086239. [DOI] [PubMed] [Google Scholar]
- 5.Matzopoulos R, Bowman B, Butchart A, et al. Background on violence and its prevention in low- and middle-income countries. Intl J Inj Contr Saf Promot. 2008;15:177–187. doi: 10.1080/17457300802396487. [DOI] [PubMed] [Google Scholar]
- 6.Bowman R, Matzopoulos R, Butchart A, et al. The impact of violence on development in low- to middle-income countries. Int J Inj Contr Saf Promot. 2008;15:209–219. doi: 10.1080/17457300802417911. [DOI] [PubMed] [Google Scholar]
- 7.Julliard C, Mballa G, Ndongo C, et al. Patterns of injury and violence in Yaounde Camaroon: an analysis of hospital data. World J Surg. 2011;35:1–8. doi: 10.1007/s00268-011-1190-8. doi:10.1007/s00268-010-0825-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogendi J, Ayisi J. Causes of injuries resulting in a visit to the emergency department of a Provincial General Hospital, Nyanza, Western Kenya. Afr Health Sci. 2011;11:255–261. [PMC free article] [PubMed] [Google Scholar]
- 9.Ranney M, Odero W, Mello M, et al. Injuries from interpersonal violence presenting to a rural health center in Western Kenya: characteristics and correlates. Inj Prev. 2009;15:36–40. doi: 10.1136/ip.2008.019547. [DOI] [PubMed] [Google Scholar]
- 10.Norman R, Schneider M, Bradshaw D, et al. Interpersonal violence: an important risk factor for disease and injury in South Africa. Popul Health Metr. 2010;8:32. doi: 10.1186/1478-7954-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bazargan-Hejazi S, Medeiros S, Mohammadi R, et al. Patterns of intimate partner violence: a study of female victims in Malawi. J Inj Violence Res. 2013;5:38–50. doi: 10.5249/jivr.v5i1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samuel J, Akinkuotu A, Baloyi P, et al. Hospital-based injury data in Malawi: strategies for data collection and feasibility of trauma scoring tools. Trop Doct. 2010;40:98–99. doi: 10.1258/td.2009.090009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masiira N, Ombito B. Surgical admissions to the Rift Valley Provincial General Hospital, Kenya. E Afr Med J. 2002;79:373–378. doi: 10.4314/eamj.v79i7.8842. [DOI] [PubMed] [Google Scholar]
- 14.Hulme P. Mechanisms of trauma at a rural hospital in Uganda. Pan Afr Med Jl. 2010;7:5. doi: 10.4314/pamj.v7i1.69110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCloskey L, Williams C, Larson U. Gender inequality and intimate partner violence among women in Moshi, Tanzania. Int Fam Plann Perspect. 2005;31:124–130. doi: 10.1363/3112405. [DOI] [PubMed] [Google Scholar]
- 16.Ludermir A, Lewis G, Valongueiro S, et al. Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet. 2010;376:903–910. doi: 10.1016/S0140-6736(10)60887-2. [DOI] [PubMed] [Google Scholar]
- 17.Silva E, Ludermir A, Barreto de Arujo T, et al. Frequency and pattern of intimate partner violence before, during and after pregnancy. Rev Saude Publica. 2011;45:1–9. doi: 10.1590/s0034-89102011005000074. [DOI] [PubMed] [Google Scholar]
- 18.Anonymous . Organization for Economic Co-operation and Development. Social Institutions and Gender Index; Malawi: 2012. Available at http://genderindex.org/country/malawi. Accessed June 2012. [Google Scholar]
- 19.Uthman O, Lawoko S, Moradi T. Factors associated with attitudes towards intimate partner violence against women: a comparative analysis of 17 sub-Saharan countries. BMC Health Hum Rights. 2009;9:1–15. doi: 10.1186/1472-698X-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jewkes R. Emotional abuse: a neglected dimension of partner violence. Lancet. 2010;376:851–852. doi: 10.1016/S0140-6736(10)61079-3. [DOI] [PubMed] [Google Scholar]
- 21.Ortiz-Barreda G, Vives-Cases C. Violence against women: the role of the health sector in international legislation. Gac Sanit. 2012 doi: 10.1016/j.gaceta.2011.09.027. doi:10.1016/j.gaceta.2011.09.027. [DOI] [PubMed] [Google Scholar]
- 22.Howe A, Crilly M. Identification and characteristics of victims of violence identified by emergency physicians, triage, nurses, and the police. Inj Prev. 2002;8:321–323. doi: 10.1136/ip.8.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barancik J, Chatterjee B, Greene Y, et al. Northeastern Ohio trauma study. I. Magnitude of the problem. Am J Public Health. 1983;73:746–751. doi: 10.2105/ajph.73.7.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sutherland I, Sivarajasingam V, Shepherd J. Recording of community violence by medical and police services. Inj Prev. 2002;8:246–247. doi: 10.1136/ip.8.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jewkes R. Preventing sexual violence: a rights-based approach. Lancet. 2002;360:1092–1093. doi: 10.1016/S0140-6736(02)11135-4. [DOI] [PubMed] [Google Scholar]
- 26.Gottleib A. Intimate partner violence: a clinical review of screening and intervention. Womens Health. 2008;4:529–539. doi: 10.2217/17455057.4.5.529. [DOI] [PubMed] [Google Scholar]
- 27.Joyner K, Mash R. Recognizing intimate partner violence in primary care: Western Cape, South Africa. PLoS One. 2012;7:e29540. doi: 10.1371/journal.pone.0029540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uthman O. Geographical variations and contextual effects on age of initiation of sexual intercourse among women in Nigeria: a multilevel and spatial analysis. Int J Health Geogr. 2008;7:27. doi: 10.1186/1476-072X-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anonymous . UN Habitat. Lilongwe Urban Profile; Malawi: 2012. Available at http://www.unhabitat.org/pmss/listItemDetails.aspx?publicationID=3173. Accessed June 2012. [Google Scholar]
- 30.Karimi F, Basu M. Longtime women’s activist Banda sworn in as Malawi president. CNN news. 2012 Apr 7; 2012. Available at http://articles.cnn.com/2012-04-07/africa/world_africa_malawi-president_1_malawi-president-malawian-patricia-kaliati?_s=PM:AFRICA. Accessed June 2012.
- 31.Joyce Banda Foundation International 2012 Available at http://www.jbfoi.org/. Accessed June 2012.