Abstract
Background
The progressive decline in the CD4 count in HIV patients leads to a more general decline in immune functioning. The study has been carried out to determine the decline in CD4 count in HIV patients.
Methods
The study was conducted in a medical college hospital at Maharashtra. The information on baseline CD4 count was gathered from positive patient records registered in the central disease registry. The baseline CD4 count was the first count of CD4 obtained when the patient is diagnosed as HIV positive and further two subsequent readings. The time from baseline (t1) till the last CD4 count (t2) was divided into the different quartiles and the median decline in CD4 count in each quartile was determined. As the time between the two CD4 count measurements was not uniform the rate of change in CD4 was measured with respect to time as [X (t2) − X (t1)/(t2 − t1)]. Correlation was assessed using correlation coefficient.
Results
As the CD4 counts were following skewed distribution, the normality was achieved by cuberoot transformation. The overall rate of decline in CD4 count was estimated to be 35 cells/μL per year with 95% confidence interval (CI) as (17.01, 85.04). The correlation coefficient between decline in CD4 and the initial CD4 count in the four time quartiles was (r = −0.51; p = 0.001, r = −0.79; p = 0.000, r = −0.48; p = 0.015 and r = −0.80; p = 0.000) respectively. The median decline in the CD4 count in 0–6 months was 3 cells/μL, in (6–11) months was approximately 26 cells/μL, in (11–21.5) months was 30 cells/μL and in more than 21.5 months the median decline was 52 cells/μL.
Conclusions
There was a progressive decline in the CD4 count following HIV infection. An understanding of the influence of decline in CD4 count in HIV patients not on ART is important for clinical management of HIV disease.
Keywords: CD4 count, Human immunodeficiency virus (HIV), Antiretroviral therapy (ART)
Introduction
As recently as four decades ago, it was widely believed that infectious disease was no longer much of a threat in the developed world. The remaining challenges to public health, it was thought, stemmed from noninfectious conditions such as cancer, heart and degenerative disease. That confidence was shattered in the early 1980's by the advent of Acquired Immunodeficiency Syndrome or AIDS. Here was a devastating disease caused by a class of infectious agents – retroviruses that had first been found in human beings only a few years before. Today HIV infection in humans is considered pandemic by the World Health Organization (WHO). Nevertheless, complacency about HIV may play a key role in HIV risk.1,2 From its discovery in 1981–2012, AIDS killed more than 30 million people. HIV infects about 0.6% of the world's population.3 In spite of the startling nature of the epidemic, science responded quickly. In the two years from mid 1982 to mid 1984 the outlines of the epidemic were clarified, a new virus – the Human Immunodeficiency Virus or HIV was isolated and shown to cause the disease, a blood test was formulated and the virus's targets in the body were established.
HIV infects primarily vital cells in the human immune system such as helper T cells (to be specific, CD4+ T cells), macrophages, and dendritic cells.4 CD4 has a significant role in the immune function of T4 lymphocytes and also serves as a marker for that group of cells. Because of the central role of CD4 cells in immune regulation, their depletion can have widespread deleterious effects on the functioning of the immune system as a whole. The progressive decline leads to a more general decline in immune functioning and is the primary factor determining the clinical course of the HIV infected individual. Since the progressive decline in the CD4 count following HIV infection leads to a more general decline in the immune function and is the primary factor determining the clinical course of the HIV infected individual we attempted to determine the decline in CD4 count in HIV patients and assessed the effects of time, treatment, initial CD4 count and age on the rate of CD4 cell count decline.
Materials and Methods
The study was a register based study which was cleared by the Institutional Ethics Committee. The information on baseline CD4 count was gathered from HIV positive patient records registered in the central disease registry. The initial CD4 count or baseline CD4 count was the first count of CD4 obtained when the patient was diagnosed as HIV positive. Normality of CD4 count was assessed and cube root transformation was carried out to linearize the relationship with time and make the distribution of CD4 more symmetric. Two subsequent readings on individual patient was taken along with the time elapsed between the subsequent readings. The time from baseline (t1) till the last CD4 count (t2) was divided into the different quartiles and the median decline in CD4 count in each quartile was determined. The CD4 count at baseline at time t1 is X (t1) and at time t2 is X (t2). As the time between the two CD4 count measurements was not uniform the rate of change in CD4 was measured with respect to time as [X (t2) − X (t1)/(t2 − t1)]. We analyzed CD4 count decline in 209 individuals for whom two subsequent measurements on CD4 were available. We excluded CD4 counts measured greater than four years after first measurement because it would have introduced bias. We also excluded CD4 counts post ART initiation after initial CD4 as ART would alter the rate of decline in CD4 count.
As most of the statistical analysis is based on the normality of the data, we assessed the normality by the normal quintile plot and the goodness of fit was tested by Kolmogorove-Smirnov test using SPSS 14.0. The normality was achieved by transformation in order to linearize the relationship with time and make the distribution of CD4 count more symmetric. The average decline in CD4 count is expressed with 95% confidence interval (95% CIs). The average decline is also measured in different time quartiles. The correlation between rate of decline in CD4 count and baseline CD4 count was assessed using correlation coefficient.
Results
The data was obtained from registers maintaining information on HIV positive male patients. 310 HIV patients' data was studied. 24 patients who were already on antiretroviral therapy (ART) were excluded from the analysis. Out of 286 HIV positive patients who were not on ART, 77 patients did not have subsequent CD4 counts for two time periods and hence excluded. A total of 209 patients were subjected to further statistical analysis. The average age was 36 years (SD = 7) with average 10 years of schooling. 97% of the patients were married. 1 patient gave history of blood donation, 61% gave unknown as source of infection whereas 38% gave history of exposure to commercial sex worker. The distributional properties of CD4 count of all patients revealed that it follows a skewed distribution (Figs. 1 and 2). The Kolmogorov–Smirnov test to assess the normality of the variable was significant (p = 0.000). A low significance value (generally less than 0.05) indicates that the distribution of the data differs significantly from a normal distribution. To normalize the data cube root transformation was carried out to the data and the histogram re-plotted as shown in Fig. 3. The normal Q–Q plot for the transformed CD4 count is shown in Fig. 4. The Kolmogorov–Smirnov statistic tests for the transformed CD4 count yields the significance value of p = 0.20 implying that the transformed CD4 now follows a normal distribution and is suitable for further statistical analysis. Out of all patients, 209 patients who were not on ART and had more than two eligible subsequent CD4 count measurements were included for determining the rate of decline in CD4 count.
Fig. 1.
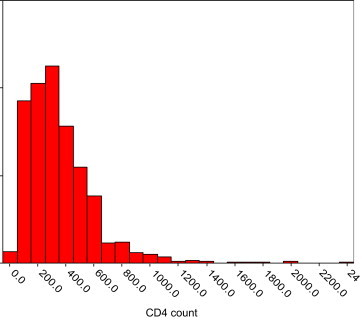
Distribution of baseline CD4.
Fig. 2.
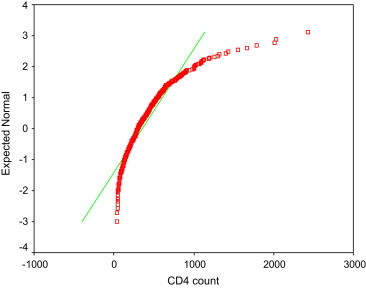
Normal Q–Q Plot of baseline CD4.
Fig. 3.
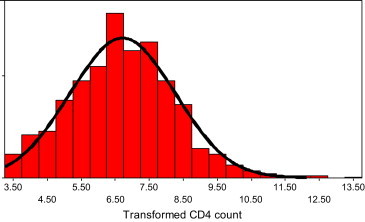
Distribution of transformed CD4 count.
Fig. 4.
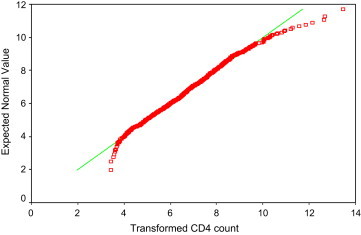
Normal Q–Q plot of transformed CD4.
The overall rate of decline in CD4 count was estimated to be 34.98 = 35 cells/μL per year (95% CI = 17.01, 85.04). The median time was 11 months and mean was 19.70 months (standard deviation SD = 24.03 months). The time variable was divided into the different quartiles namely Q1 = 6.0, Q2 = 11.0 and Q3 = 21.5. The decline in CD4 was determined in the four time quartiles viz. (0–6), (6–11), (11–21.5) and (≥21.5) is shown in Table 1 and the decline in CD4 count against the baseline or initial CD4 count is plotted as a scatter plot. When all the time quartiles are considered simultaneously and the scatter plots superimposed over each other it clearly brings out that as time increases the rate of decline in CD4 count from baseline or initial CD4 count increase (Fig. 5).
Table 1.
Decline in CD4 count in various time quartiles.
| Time quartiles in months (n) | Mean CD4 ± SD (95% CI) | Median decline in CD4 count (cells/μL) | Correlation coefficient between decline and initial CD4 count |
|---|---|---|---|
| 0–6 (129) | 354 ± 218.58 (316.28, 391.72) | 3 | −0.52 (p = 0.001) |
| 6–11 (24) | 319 ± 203.86 (237.44, 400.56) | 26 | −0.78 (p = 0.000) |
| 11–21.5 (28) | 307.29 ± 127.64 (260.01, 354.57) | 30 | −0.48 (p = 0.015) |
| ≥21.5 (28) | 379 ± 217.46 (298.45, 459.55) | 52 | −0.80 (p = 0.000) |
Fig. 5.
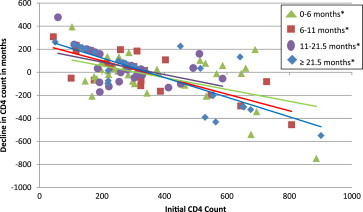
Decline in CD4 count in months.
Discussion
This study shows that the rate of decline in CD4 count is 3 cells/μL in 0–6 months, 26 cells/μL in 6–11 months, 30 cells/μL in 11–21.5 months and 52 cells/μL beyond 21.5 months. Studies pointed out the role of CD4 cell count as an important determinant of virological and immunological outcome. Studies suggest that the HIV-1 epidemic in the Netherlands may have become more virulent, leading to faster disease progression if untreated. Analysis of CD4 cell count decline before antiretroviral therapy (ART) initiation, a surrogate marker for disease progression, may be hampered by informative censoring as ART initiation is more likely with a steeper CD4 cell count decline.5 A Cox multivariate proportional hazards model allowed the authors to demonstrate that, based on an average of 22 months of follow-up, CD4 lymphocyte counts better at predicting disease progression. Population-based studies of the natural history of HIV infection in gay men show that the mean CD4 cell count prior to sero-conversion is about 1000/mm3; the count decreases to a mean of 780/mm3 at six months post-sero-conversion and to 670/mm3 at one year.6 However, some series show a more rapid and sustained decline after sero-conversion.7 After one year, the CD4 cell count declines at an average rate of approximately 50/mm3 per year, but there is substantial variation between patients.6,8,9 Study conducted by Margolick,8 on 859 self referred IVDUs aged 18 through 49 years with 18 month follow-up found that the median rate of decline in CD4 per 6 months was 7.6/μL for sero-positive IVDU's. Multivariate regression analysis showed no significant change in the cells over time and no change due to use of drugs. In another study, the average rate of decline was 14.3% per year but varied considerably between subjects. It further showed that the changes in CD4 had negligible correlation with the baseline CD4 count.
A study conducted in 1676 Asian patients in the TREAT Asia HIV observational database (TAHOD) showed that the decline in CD4 during 6–12 months was 21.5, in 18–24 months it was 25.8 and more than 24 months it was 59.1 cells.10 The CASCADE study conducted on 2820 HIV positive patients found the average CD4 cell decline to be 61 cells/μL per year.11 One of the explanations for varying decline rates in CD4 count could be wide variability in the data. It was observed that the time interval of getting two or more consecutive readings for CD4 counts in the same individual was variable. In terms of consistency, few patients' consecutive readings of CD4 were within 2 months as against few patients who had it after 72 months.
The Swiss HIV Cohort Study developed rules to guide frequency of CD4 cell count monitoring in HIV infection before starting ART.12 The study recommended that it is sufficient to measure CD4 cell count 1 year after a count >650 for a threshold of 200, >900 for 350, or >1150 for 500 × 106/L, respectively. When CD4 counts fall below these limits, increased monitoring frequency becomes advisable and these rules offer guidance for efficient CD4 count below particularly in resource limited settings.
In conclusion, our study shows that there is significant decline in the CD4 count with time and correlation analysis shows that this decline in CD4 count is associated with baseline CD4 count. An understanding of the influence of decline in CD4 count in HIV patients not on ART is important for management of HIV positives.
Conflicts of interest
All authors have none to declare.
Acknowledgment
The authors are immensely grateful to Nagarjuna DS, former HOD Mathematics Dept, CME, Pune and Deepti Poojari for their invaluable help.
References
- 1.“CDC – HIV/AIDS – Resources – HIV Prevention in the United States at a Critical Crossroads”. Cdc.gov. http://www.cdc.gov/hiv/resources/reports/hiv_prev_us.htm.
- 2.“HIV and AIDS Among Gay and Bisexual Men” (PDF). http://www.cdc.gov/nchhstp/newsroom/docs/FastFacts-MSMFINAL508COMP.pdf.
- 3.Joint United Nations Programme on HIV/AIDS . 2006. Overview of the Global AIDS Epidemic.http://data.unaids.org/pub/GlobalReport/2006/2006_GR_CH02_en.pdf (PDF). 2006 Report on the global AIDS epidemic. ISBN: 9291734799. [Google Scholar]
- 4.Cunningham A., Donaghy H., Harman A., Kim M., Turville S. Manipulation of dendritic cell function by viruses. Curr Opin Microbiol. 2010;13(4):524–529. doi: 10.1016/j.mib.2010.06.002. PMID 20598938. [DOI] [PubMed] [Google Scholar]
- 5.Gras L., Geskus R.B., Jurriaans S. Has the rate of CD4 cell count decline before initiation of antiretroviral therapy changed over the course of the Dutch HIV epidemic among MSM? 2013;8(5) doi: 10.1371/journal.pone.0064437. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stein D.S., Korvick J.A., Vermund S.H. CD4+ lymphocyte cell enumeration for prediction of clinical course of human immunodeficiency virus disease: a review. J Infect Dis. 1992;165:352. doi: 10.1093/infdis/165.2.352. [DOI] [PubMed] [Google Scholar]
- 7.Schacker T., Collier A.C., Hughes J. Clinical and epidemiologic features of primary HIV infection. Ann Intern Med. 1996;125:257. doi: 10.7326/0003-4819-125-4-199608150-00001. [DOI] [PubMed] [Google Scholar]
- 8.Margolick J.B., Muoz A., Vlahov D. Changes in T-lymphocyte subsets in intravenous drug users with HIV-1 infection‖. JAMA. 1992;267(12):1631–1636. [PubMed] [Google Scholar]
- 9.Hughes M.D., Stein D.S., Gundacker H.M. Within-subject variation in CD4 lymphocyte count in asymptomatic human immunodeficiency virus infection: implications for patient monitoring. J Infect Dis. 1994;169:28. doi: 10.1093/infdis/169.1.28. [DOI] [PubMed] [Google Scholar]
- 10.Zhou Jialun, Sirisanthana Thira, Kiertiburanakul Sasisopin. Trends in CD4 counts in HIV-infected patients with HIV viral load monitoring while on combination antiretroviral treatment: results from the TREAT Asia HIV Observational Database. BMC Infect Dis. 2010;10:361. doi: 10.1186/1471-2334-10-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolbers Marcel, Babiker Abdel, Sabin Caroline. Pretreatment CD4 cell slope and progression to AIDS or death in HIV-infected patients initiating antiretroviral Therapy—The CASCADE Collaboration: a collaboration of 23 Cohort studies. PLoS Med. 2010 February;7(2):e1000239. doi: 10.1371/journal.pmed.1000239. Published online 2010 February 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buclin T., Telenti A., Perera R. Development and validation of decision rules to guide frequency of monitoring CD4 cell count in HIV-1 infection before starting antiretroviral therapy. PLoS ONE. 2011;6(4):e18578. doi: 10.1371/journal.pone.0018578. [DOI] [PMC free article] [PubMed] [Google Scholar]


