Abstract
BACKGROUND
We conducted a national survey of general surgeons to address the association between surgeon characteristics and the tendency to recommend surgery.
METHODS
We used a web-based survey with 25 hypothetical clinical scenarios with clinical equipoise regarding the decision to operate. The respondent-level tendency to operate (TTO) score was calculated as the average score over the 25 scenarios. Surgical volume was based on self-report. Linear regression models were used to evaluate the associations between TTO, other covariates of interest, and surgical volume.
RESULTS
There were 907 respondents. The mean surgical TTO was 3.05 ± .43. Surgeons had significantly lower TTO scores when responding to questions within their area of practice (P < .0001). There was no association between TTO and malpractice concerns, financial incentives, or compensation structure.
CONCLUSIONS
Surgeons recommend intervention far less frequently within their area of specialization. Malpractice concerns, volume, and financial compensation do not significantly affect surgical decision making.
Keywords: Surgical decision making, Survey, Surgical volume, Surgical specialization, Malpractice
In the last decade, research has shown a wide variation in the way medicine and surgery are practiced across the country. Practice variation is typically discussed using metrics such as the use of resources, spending, and cost (eg, average per capita Medicare spending varies almost 3-fold across the United States even after case-mix adjustment).1 As a result, the Office of Management and Budget has identified the reduction of practice variation as a key to reducing health care costs.2 Wennberg3 described the concept of “unwarranted variation” as differences in health care delivery that cannot be explained by illness, medical need, or the dictates of evidence-based medicine; much of his and others’ work at the Dartmouth Atlas of Healthcare, Lebanon, NH, investigated the possible reasons for this variation. They found that differential physician visits, specialist consultations, and hospitalizations are key contributors to practice variation.
Yet, aside from conclusions about physicians overall that have been extrapolated from these studies, few examine individual physician behavior at the center of the variation, especially in surgery.4,5 There is a great deal of interest in reducing unnecessary variation as it contributes to increasing health care costs, and the use of elective surgery has been implicated as a factor. Existing research looking at how general surgeons make decisions and the variety of ways in which surgeon behavior may be influenced is outdated and does not account for today’s medical and legal environment.6,7 As such, we undertook a national survey of general surgeons to determine the associations between a surgeon’s characteristics, including demographics, specialization, procedure volume, practice settings, financial compensation and malpractice fears, and their tendency to recommend surgery, which we refer to as the tendency to operate (TTO). In particular, we hypothesized a priori that financial compensation and incentives, specialization, surgical volume, and concerns about malpractice would influence a surgeon’s decision to recommend an operation.
Methods
All respondents provided consent to participate in the survey, and all data were deidentified before analysis. This study was approved by the Institutional Review Board at the University of Pennsylvania, Philadelphia, PA.
Study population
Respondents were initially recruited from the Philadelphia Academy of Surgery; there are 248 members. The American College of Surgeons (ACS) distributes a weekly e-mail of news bulletins entitled the ACS NewsScope to over 44,000 subscribers, many of whom are fellows of the ACS. The NewsScope e-mail included information about the survey 7 times over the course of the 1-year enrollment period. Lastly, the survey was advertised on the American Board of Surgery (ABS) website under the Maintenance of Certification (MOC) Part 2 link as a method of attaining MOC Part 2 credits. Because it was not possible to identify how many eligible surgeons received an invitation, we did not calculate a response rate. Our total study sample included 907 surgeons with representation from all 50 states. All surgeons were board certified or board eligible.
Survey development
In collaboration with the ABS, we designed a web-based survey instrument to assess surgeons’ decision making across a spectrum of general surgical conditions (Appendix 1). We enrolled participants over a 1-year period from April 2011 until April 2012. The survey consisted of 25 hypothetical clinical scenarios, which were designed to have a high degree of clinical uncertainty regarding the decision to operate (ie, surgical intervention was neither strictly indicated nor contraindicated and the decision relied on the discretion of the surgeon). We included 1 positive control question in which the patient was in definite need of surgical intervention and 1 negative control question in which surgical intervention was not indicated. All questions were tested for face and content validity with experts in each field from the Department of Surgery at the Hospital of the University of Pennsylvania, Philadelphia, PA, and revised based on feedback. All scenarios contained information about the age, sex, and race of the patient; these were constant for each question; however, the order of the 25 scenarios was randomized. Relevant signs and symptoms about a specific surgical condition were described, with laboratory data and imaging results as needed. Each scenario was thoroughly reviewed to ensure sufficient information to make a reasonably informed decision without being excessively detailed to reduce respondent burden. Respondents were instructed to respond to the patient scenario as they would treat an actual patient regardless of whether they typically performed the indicated procedure. Additional instructions included that no further medical or diagnostic testing would be done, and no interventional radiology procedures would be performed. We deliberately avoided excessively lengthy or confusing clinical scenarios.
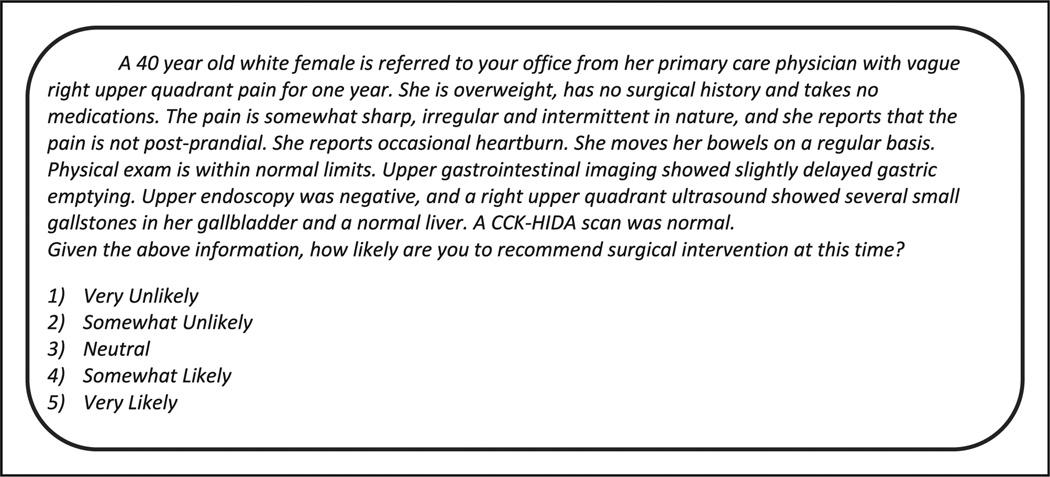
Following each of the scenarios, the following question was posed to the respondent: “Given the above information, how likely are you to recommend surgical intervention at this time?” Responses were graded on a 5-point Likert scale, ranging from “very likely” to “very unlikely,” including a “neutral” option (Fig. 1). Surgical cases varied across the following most common general surgery domains: hernias, abdominal surgery, breast surgery, colorectal surgery, trauma and surgical critical care, hepatobiliary surgery, vascular surgery, and endocrine surgery.
Figure 1.
An example of a clinical scenario regarding cholecystectomy. 1 = very unlikely, 2 = somewhat unlikely, 3 = neutral, 4 = somewhat likely, and 5 = very likely.
Study variables
Respondents answered 21 questions pertaining to their sociodemographics. Five questions were asked about malpractice concerns, including concerns about being involved in a lawsuit, ordering tests to avoid the appearance of malpractice, and reliance on consultants and technology to reduce the perceived risk of getting sued. These were drawn from a previously validated malpractice concerns scale.8 Surgeons were asked about their basic mode of financial compensation, the categories of which were derived from the ABS recertification application. Categories included the following: (1) fixed salary; (2) salary adjusted for performance (eg, surgeon’s own productivity, fee-for-service practice, practice’s financial performance, and practice profiling); (3) shift, hourly, or other time-based payment; (4) share of practice billings or workload; or (5) other methods. Respondents were asked if they were eligible for financial incentives such as periodic adjustments, bonuses, returns on withholds, or any type of supplemental payment either from the practice or from health plans. Geographical practice characteristics were based on rural-urban commuting area codes, a new Census tract-based classification scheme, as linked to reported practice zip codes. Lastly, respondents entered their most recent 1-year operative case log into 12 general categories. The standard surgical volume was defined as the sum of z scores of surgical volume in each of the 12 categories.
TTO was defined as the arithmetic mean of all scenario responses excluding the positive control question. The negative control question was included in the TTO score because of a larger than expected variability in responses. A mean of 1 would imply that the surgeon chose “very unlikely” for all scenarios; similarly, a mean of 5 would imply “very likely” was chosen for all scenarios.
Surgeon specialization was determined from self-reported surgical volume rather than fellowship status because we believed this would more accurately reflect their current areas of clinical focus. Specialist fields included were colorectal, vascular, trauma, breast, endocrine, hepatobiliary, hernia, and breast surgery. A surgeon was deemed a specialist in a field of surgery if his/her volume of cases in that field was greater than 2 standard deviations above the mean volume for all respondents in that field. To simplify the analysis, for surgeons who met criteria for specialization in multiple fields, the field with the highest standard deviation was assigned. A separate specialty-specific TTO score was calculated as the mean score of clinical scenarios relevant to the defined specialty.
Feedback and continuing medical education
After completion of the survey, respondents were then able to compare their individual responses to each scenario with cumulative responses for each answer choice depicted in a bar graph with previous respondents’ results. Surgeons could claim up to 5 American Medical Association (AMA) PRA Category 1 credit (TM) hours, which could be used toward MOC Part 2 as per our collaboration with the ABS. As part of the continuing medical education process, respondents answered an additional 18 questions regarding their assessment of the survey, including a free text box (Appendix 2).
Statistical methods
Continuous variables are expressed as means ± standard deviation or medians (interquartile range) depending on normality. Categorical variables are expressed as proportions. Internal validity of the survey instrument was assessed via the Cronbach alpha test and factor analysis, with eigenvalues greater than 1 being deemed sufficient for the identification of an independent factor. The Student t test and chi-square analyses were used to assess univariable associations with TTO and categorical exposures. The correlation between TTO and continuous variables was assessed via Pearson or Spearman coefficients depending on normality. Ordinary least squares regression was used in multivariable models examining TTO. Backward stepwise regression with a threshold of P <.05 was used to obtain parsimonious models. Standard surgical volume was log transformed given significant rightward skew. All statistics were analyzed using STATA 11.0 (College Station, TX).
Results
Our total study population was 907 surgeons. There was broad variation in how surgeons responded to the scenarios (Fig. 1). Less than 15% chose the “neutral” option per question. The post-test questionnaire was completed by 821 respondents. Of those, 703 (86%) felt that “all or most” or “many” of the survey questions contained sufficient information to make a reasonably informed decision. Only 5 (.61%) of surgeons felt that “few or none” of the scenarios contained enough information. Over 99% of respondents recommended surgery for the positive control question. However, less than 80% of respondents chose surgical intervention for the negative control question. Because of unexpected significant variability, this question was therefore included in the final TTO score.
Baseline characteristics of the study sample are listed in Table 1. Briefly, the average age was 51.9 ± .4 years. Male surgeons accounted for 78.1% of the study sample; 82.7% were white. Approximately one fourth of the study sample were surgeons at academic hospitals (26.1%), whereas private practice surgeons (large and small groups) accounted for 67.4% of surgeons and government/Veterans Affairs surgeons accounted for 6.5%. Roughly half (45.6%) worked with surgical residents on a weekly basis. Surgeons largely worked in urban areas (81.5%). Half of the respondents had completed surgical fellowships (50.4%). A majority of surgeons chose salary adjusted for performance (43.3%) as their basic financial compensation structure, with fixed salary as the next most common method of compensation (32.5%); 48.0% were eligible to receive financial incentives.
Table 1.
The baseline characteristics of survey respondents
| Surgeon characteristic | N = 907 |
|---|---|
| Age (y ± SD) | 51.9 (±.4) |
| Sex (%) | |
| Male | 78.1 |
| Female | 21.9 |
| Race (%) | |
| Black | 2.0 |
| White | 82.7 |
| Other | 15.4 |
| Ethnicity (%) | |
| Hispanic | 4.1 |
| Non-Hispanic | 95.9 |
| Fellowship (%Y) | 50.4 |
| Practice (%) | |
| Small (<4) | 54.9 |
| Large (≥4) | 12.5 |
| Government | 6.5 |
| Academic | 26.1 |
| Residents (%) | |
| Yes work with residents | 45.6 |
| Compensation (%) | |
| Fixed salary | 32.5 |
| Share of practice | 12.7 |
| Time based | 2.6 |
| Performance based | 43.3 |
| Other | 8.8 |
| Incentives (%Y) | 48.0 |
| Geography (%) | |
| Isolated | 1.2 |
| Small rural | 5.4 |
| Large rural | 9.5 |
| Urban | 81.5 |
Numbers are means ± standard deviations or percentages as indicated.
SD = standard deviation.
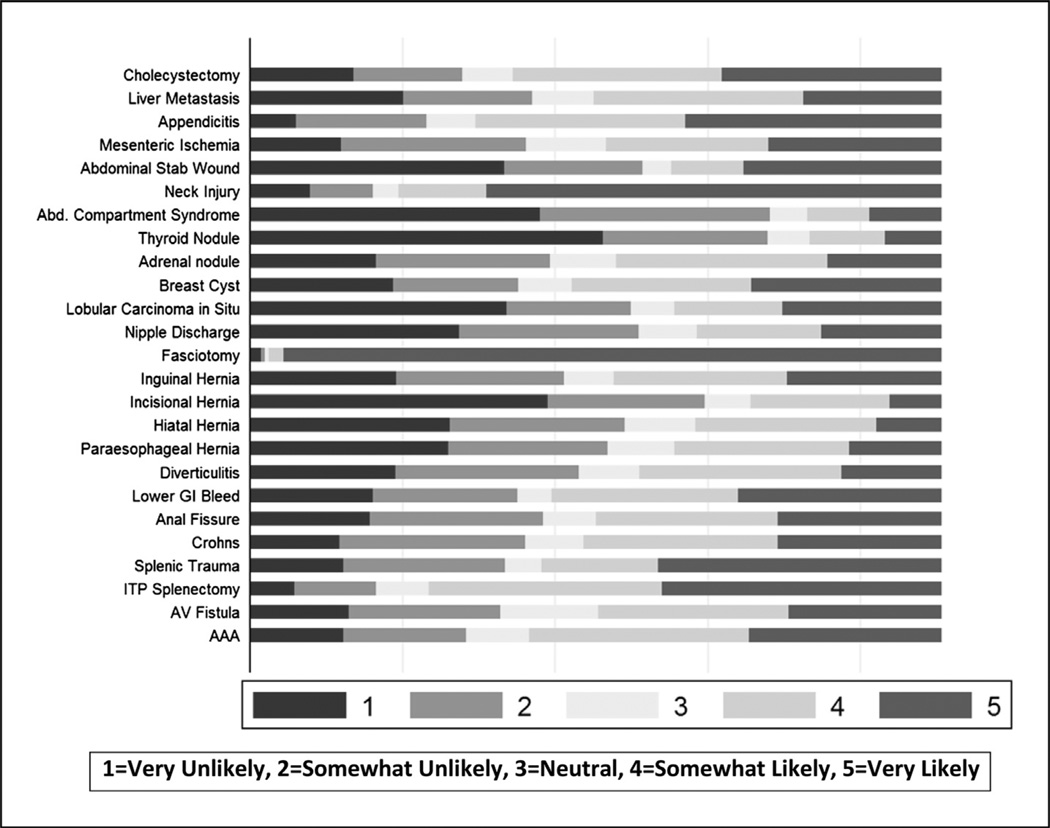
The mean TTO across all questions was 3.06 ± .43. Figure 2 shows the distribution of responses for each case scenario. Table 2 stratifies surgeon characteristics among tertiles of TTO in order to characterize surgeons across a spectrum of TTO, ranging from low (mean TTO <2.83) to high (mean TTO >3.25). In unadjusted analysis, older surgeons had significantly lower TTO scores than their younger colleagues (−.03 points per decade of life; 95% confidence interval (CI), −.06 to −.003; P = .03). White surgeons had lower TTO scores than nonwhite surgeons (mean TTO = 3.04 ± .42 vs 3.15 ± .46, P =.003). Fellowship training was also associated with a higher TTO (mean TTO = 3.09 ± .42 vs 3.03 ± .44, P = .03) in univariate analysis. Malpractice concern was variable in this population; the median for the 5 questions assessing malpractice concern was 2.4 (interquartile range = 1.6 to 3.2) skewed toward higher levels of concern. Higher or lower malpractice concern was not associated with TTO in unadjusted analysis nor was the subset of malpractice concern questions that pertained to “defensive medicine.”
Figure 2.
The distribution of responses by clinical scenario. Fasciotomy was the positive control question.
Table 2.
Surgeon characteristics as stratified by tertiles of increasing TTO
| Tertile 1 | Tertile 2 | Tertile 3 | P value | |
|---|---|---|---|---|
| Age (y ± SD) | 53.6 ± .6 | 51.4 ± .6 | 50.9 ± .6 | .03 |
| Malpractice (score ± SD) | 2.5 ± .1 | 2.5 ± .06 | 2.5 ± .06 | .48 |
| Sex (%) | ||||
| Male | 77.5 | 77.1 | 79.5 | .46 |
| Female | 22.5 | 22.9 | 20.5 | .46 |
| Race (%) | ||||
| Black | 1.8 | .7 | 3.6 | .54 |
| White | 86.1 | 85.9 | 76.3 | .003 |
| Other | 12.1 | 13.4 | 20.5 | .004 |
| Ethnicity (%) | ||||
| Hispanic | 6.1 | 3.1 | 3.2 | .077 |
| Non-Hispanic | 93.9 | 96.0 | 96.8 | .077 |
| Fellowship (yes/no) (%) | 44.6 | 55.1 | 50.7 | .031 |
| Practice type (%) | ||||
| Small (<4) | 55.0 | 51.1 | 58.7 | .46 |
| Large (≥4) | 14.6 | 11.6 | 11.4 | .26 |
| Government | 6.8 | 9.1 | 3.6 | .23 |
| Academic | 23.6 | 28.2 | 26.3 | .49 |
| Residents (%) | ||||
| Yes | 43.2 | 48.9 | 44.5 | .34 |
| No | 56.8 | 51.1 | 55.5 | .34 |
| Compensation (%) | ||||
| Fixed salary | 30.0 | 34.8 | 32.5 | .63 |
| Share of practice | 15.7 | 13.2 | 9.4 | .03 |
| Time based | 2.9 | 1.9 | 3.2 | .89 |
| Performance based | 41.4 | 42.3 | 46.1 | .28 |
| Other | 10.0 | 7.8 | 8.8 | .93 |
| Incentives (%) | ||||
| Yes | 50.0 | 44.2 | 50.0 | .83 |
| No | 50.0 | 55.8 | 50.0 | .83 |
| Geography (%) | ||||
| Isolated | 0 | 1.6 | 2.0 | .25 |
| Small rural | 6.1 | 3.4 | 6.8 | .74 |
| Large rural | 11.4 | 9.8 | 7.5 | .16 |
| Urban | 79.5 | 82.2 | 82.5 | .16 |
P values reflect unadjusted associations between characteristics and continuous TTO.
SD = standard deviation; TTO = tendency to operate.
Tests for the internal validity of the clinical scenarios revealed a Cronbach alpha of .56. Factor analysis revealed 1 primary factor; this was determined to correspond to the specialty of an individual surgeon. Using restrictions set by the survey website, except for 22 incorrectly listed zip codes, there were no missing data.
Multivariable analysis
We included 11 variables in our multivariable analysis: age, sex, race, ethnicity, fellowship as a binary variable, practice type, resident interaction, compensation structure, financial incentives, geography, and volume. The results of a parsimonious regression model appear as Table 3. Significant findings included lower TTO scores for white surgeons (P = .003) and Hispanic surgeons (P = .04). One subtype of financial compensation, salary via share of billings/ workload, was significantly associated with a lower TTO (P = .02). Specifically, malpractice concern, overall volume, and financial incentives did not influence TTO. In addition, practice setting (ie, private practice, academic, or government) and working with residents did not influence the TTO.
Table 3.
Parsimonious multivariable linear regression model of associations with TTO for all surgeons surveyed (N = 907)
| Overall score | ||
|---|---|---|
| Covariate | Mean TTO difference (95% CI) |
P value |
| Hispanic ethnicity | −.14 (−.29 to .00) | .04 |
| Compensation 2: share of billings | −.10 (−.19 to −.02) | .02 |
| White race | −.11 (−.19 to −.04) | .003 |
CI = confidence interval; TTO = tendency to operate.
Influence of specialization on tendency to operate
We then examined surgical specialists. Of the 907 surgeons, 354 (39.0%) were considered specialists by our previous definition rather than by fellowship. Specialty-relevant clinical scenarios included breast, trauma, colorectal, vascular, hepatobiliary, hernia, and endocrine cases; we excluded 104 specialists outside these categories (eg, plastic surgery, cardiothoracic surgery, and so on) because there were no relevant scenarios for those fields. Thus, there were 250 (27.6%) specialists for analysis.
Surgical specialists had a significantly lower TTO in scenarios relevant to their specialty as opposed to areas outside of their specialty (mean TTO = 2.77 ± 1.05 vs 3.03 ± .46, P < .001). In addition, surgical specialists chose to operate less often on patients within their field of expertise compared with all other surgeons (mean TTO = 2.77 ± 1.62 vs 3.14 ± 1.54, P < .001). This finding was strongest for breast surgeons for the breast scenarios (mean TTO = 1.96 ± .9 vs 2.92 ± .94, P <.001). In multivariable analysis, specialist surgeons paid by share of billings/ workload had lower TTO scores (P = .02), and those paid by time-based methods had higher TTO scores (P = .02) compared with other surgical specialists (Table 4). Male specialists recommended surgery more often than their female counterparts (P < .001).
Table 4.
Parsimonious multivariable linear regression model of associations with TTO for surgeons identified as specialists (n = 250)
| Specialty-specific scores | ||
|---|---|---|
| Covariate | Mean TTO difference (95% CI) |
P value |
| Male sex | .60 (.32–.87) | <.001 |
| Compensation 2: share of billings | −.49 (−.91 to −.08) | .02 |
| Compensation 3: time based | .82 (.12–1.53) | .02 |
| White race | −.44 (−.75 to −.12) | .007 |
CI = confidence interval; TTO = tendency to operate.
Lastly, surgeons recommended surgery significantly less often for male compared with female patients (mean TTO = 2.99 ± .53 vs 3.11 ± .51, P < .001). TTO was significantly lower for white patients in the scenarios compared with black patients (mean TTO = 2.89 ± .52 vs 3.25 ± .51, P < .001).
Comments
In this large national survey of general surgeons, we examined the individual and practice characteristics of the surgeon behind the decision-making process in an effort to better understand what drives surgical practice variation. We asked surgeons to report their likelihood of recommending surgery in 25 clinical scenarios in which the decision was based on the discretion of the surgeon rather than strict surgical indications. Some variation is likely a normal component of United States health care and may be caused by such factors as differential patient socioeconomic status and access to care.9,10 For example, Cooper et al11 found that poverty and the social determinants of health are the largest contributors to variation in health care use. We make the claim that some fraction of discretionary surgery contributes to unnecessary variation and aim to raise awareness in the surgical community to the possible influences they may unintentionally bring to the decision-making process.
Because physicians control most health care resources for their patients, the intensity and volume of health care use is directly related to their medical decision making and thus are responsible for a large share of health care costs. These costs include actual dollars as well as societal costs, especially if patients are undergoing procedures for which there may not be strong indications (including informed patient preference). Previous studies have examined spinal surgery as a prime example of unwarranted variation whereby rates of surgery are up to 6 times higher in some regions compared with others despite similar patients and indications.12 The fundamental issue is that outcomes are not better by morbidity and mortality measures, which provides an argument for a reduction in the volume of surgeries that contribute to unwarranted variation.12–17
Our results suggest that, when facing the same hypothetical patient, specialist surgeons tend to recommend surgery within their field less frequently than their colleagues. In addition, individual specialists are less likely to recommend surgery in their specialty area than in other areas. One explanation may be that surgeons are more comfortable managing a patient expectantly when the case is within their own field of expertise, whereas for surgical disease that they do not treat as often, an operation may be perceived as the safer approach. This has received only limited attention in the literature although there is some evidence that specialist breast surgeons perform fewer operations for benign breast disease compared with nonspecialist surgeons18 and have better breast cancer outcomes as well.19–21 Indeed, the finding that specialization corresponds to a lower TTO was strongest when we examined breast surgeons. There are several studies examining surgical specialization and improved outcomes.22,23 Hall et al24 described a significant relationship between increased specialization and reduced risk-adjusted mortality using a measure of surgical specialization based on the number of cases performed. Similar to our study, they defined a specialist by the number of actual cases performed rather than by fellowship status. There have been extensive studies regarding the relationship between case volumes and outcomes at both the hospital and surgeon level and across a variety of surgical specialties.25–30 Systematic reviews of these studies conclude that there is likely a beneficial effect of specialization regarding outcomes. Our study did not show an effect of volume on the tendency to recommend surgery, but it did show that specialization as measured by a relatively higher volume resulted in recommending less discretionary surgery.
Our results also suggest that in unadjusted analysis, older surgeons tend to recommend surgery significantly less often than their younger colleagues in cases of discretionary surgery. We hypothesized a priori that in the face of uncertainty, surgeons may take a conservative approach, but conservatism may manifest itself differently as surgeons age. Younger surgeons may feel that operating is the conservative option, whereas older surgeons may be more comfortable with nonoperative management. There have been several studies examining physician age and clinical performance; in the case of primary care physicians, an inverse relationship has been noted between physician age and clinical performance.31,32 However, in surgery, except for very low-volume surgeons performing complex procedures such as pancreatectomy or carotid endarterectomy, surgeon age may not be an important predictor of operative risk.33 It is possible that older surgeons are able to maintain good outcomes by gradually compensating for minor atrophies in their technique as well as choosing less sick patients. However, age was not a significant predictor of TTO in the full model after taking into account other confounders, which was a surprising finding. White race was significant, and it is possible that the significant finding in univariate analysis for age is explained by the fact that most older surgeons are white. Indeed, we found that white surgeons recommend surgery less frequently than nonwhite surgeons. This may be caused by differences in surgeon race across geographic regions and the patient populations they serve and issues regarding patient compliance and access to care. This is an area of active study, and more research is needed to understand how age and race might affect an individual surgeon’s decisions and outcomes.
Significant findings within a compensation structure include that surgeons who are paid by a share of the billings or workload actually had lower TTO scores overall, which is contrary to our expectations. This was true for specialists as well. Surgeons receiving financial incentives and working for fee-for-service practices did not have significantly higher or lower TTO scores. There are many studies showing a significant relationship between physician-to-population ratio and the number of surgeries performed, so-called “physician-induced demand.”34,35 In these studies, the implication is that decisions are related to financial factors whereby surgeons create their own demand by performing more elective surgery. However, we do not find that fee-for-service practices or financial incentives result in higher use of discretionary surgery as a contributor of variation. Indeed, no form of compensation was associated with an increase in the recommendation for surgery.
Importantly, we did not find that surgeons’ malpractice concerns or volume influenced their use of discretionary surgery. Prior studies have shown that physicians often engage in defensive practices for fear of being involved in a malpractice lawsuit, with surgeons having some of the highest malpractice fears compared with other physicians.36,37 Higher malpractice costs (both premiums and payments) are associated with increased health care costs in the form of “defensive medicine”, such as diagnostic tests and minor procedures, although rates of major surgery may not be affected.37,38 Our results indicate that despite an overall high level of malpractice concern, surgeons who are more concerned about malpractice do not recommend more or less discretionary surgery. This is reassuring in that fear of liability should not enter the decision to recommend an operation.
Strengths of our study include its broad, national sampling of surgeons across a range of specialties and practice types and detailed case volume records. However, the study should be interpreted in light of several limitations. First, our Cronbach alpha score was .56, implying that the internal validity of the instrument was limited. Because this would limit the consistency of the measurement of TTO, it would tend to bias results toward the null hypothesis. Second, unmeasured confounders limit our ability to determine causal links between surgeon characteristics and TTO. Factors such as the local surgical culture in which the surgeon was trained and prior positive/negative experiences likely influence surgical decision making but are difficult to capture. Survey completion was optional, which could possibly introduce selection bias. Race and sex of the patient was significant in univariate analysis; however, patient race and sex in the scenarios were not randomized, so it is possible that this was a result of how the questions were written rather than a reflection of surgeon bias. Lastly, we used clinical scenarios to study physician behavior. The concept underlying the use of these clinical scenarios is that physicians will respond to the scenario in a manner consistent with their individual practice patterns. However, it is possible that surgeons tailored their responses over the 25 scenarios if they believed that their use of discretionary surgery was being measured because there was no “right” answer. When medical records are unavailable to provide detailed clinical information, measuring the behavior for specific clinical scenarios has been increasingly accepted as both a valid and cost-effective approach.39,40
Conclusions
In the absence of clear clinical guidelines, surgeons vary widely in their decision making regarding surgery, especially in cases of discretionary surgery. Previous studies have shown that despite higher rates of these types of surgery, outcomes may not be improved, and there may be a role for nonoperative management. We found that surgical specialization based on the number of cases performed is associated with less frequent recommendations to operate and could provide an argument to concentrate surgeries in the hands of surgeons who perform mainly those surgeries in an effort to reduce unnecessary variation. We do not find that financial incentives, fee-for-service practices, or malpractice fears influence the decision to operate.
Appendix
Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.amjsurg.2013.08.018.
Discussion
Paul Schenarts, M.D. (Omaha, NE): I would like to thank the Program Committee for the invitation to discuss this article. Dr Wilson should be congratulated on a well-designed and comprehensive evaluation as well as an excellently written manuscript. The data presented here are a meaningful contribution because the findings stand in stark contrast to several commonly held misconceptions. These include the assumption that subspecialists drive up the cost of health care and that the fear of malpractice, fee for service, and financial incentives influence the decision to operate. I do have 2 questions for Dr Wilson. First, when preparing residents to sit for the ABS examinations, it is frequently advised when given a difficult choice, the safest thing to do is operate. So my question is what influence did linking your survey directly to the American Board of Surgery and providing MOC credits have on your results? The addition of a second negative control scenario in which operation was contraindicated may have clarified the impact of this linkage. My second question is, given that over 80% of survey respondents practiced in an urban area where competition between surgeons for both patients and resources may be quite intense, what influence did this distribution of participants have on your results? In closing, again, congratulations on a job well done and continuation of the Penn tradition of excellent resident presentations.
Niamey Wilson, M.D., M.S.H.P. (Philadelphia, PA): Thank you, Dr Schenarts. In response to your first question, I created the survey in collaboration with the ABS because Dr Richard Bell was 1 of my mentors, and he was the previous Executive Associate Director of the ABS. We decided that as a means of self-assessment, this would be a great opportunity for people looking to get Part 2 of MOC, which can be very difficult to obtain. At the completion of the survey you were able to see a bar graph of your answers compared with everyone else’s answers who had taken the survey previously. In this way, surgeons were able to compare their answer choices to other surgeons, and judge for themselves how well their answers corresponded to their peers. My response to the “operating is the safe choice” question is one of the key things we were trying to get at in this survey. These cases are discretionary surgeries, so operating on a patient for any of these questions would not be wrong. The questions were designed to have no right answer. By examining the surgeon level factors that contribute to the decision to operate, we can start to see the differences on an individual basis of why a particular surgeon would choose to operate and why another might not. It’s possible that linking the survey with the ABS may have had a slight influence on the results but we don’t feel this is significant. In response to the negative control question, we actually did have a question that was designed to be a negative control question but it turned out that about 25% of the people chose to operate on the patient. Therefore, it had too much variability to be considered a true control question, and this was likely simply the way the question was written. We did include it in our multivariable analysis. Lastly, the distribution of the surgeons who were taking the survey was indeed mostly urban, but we felt that this was actually a fair representation given that there are such great concentrations of surgeons in the heavily populated areas like the Northeast and the far West. We actually thought that the spread of the surgeons was fairly representative, and if you look at the breakdown between academic versus private practice versus government, that was also fairly representative of the surgeons in the community.
Shanu Kothari, M.D. (LaCrosse, WI): I have a question. Have you shared the results of this data with your own administrators at your institution?
Dr Wilson: Dr Murayama is the final author on the manuscript; he is the chief of surgery at one of the Penn hospitals, so he is aware of the results. We have not yet shared the results with the administrators.
Footnotes
The authors declare no conflict of interest.
References
- 1.Dartmouth atlas of health care [Internet] Hanover (NH): Dartmouth Institute; [Accessed February 11, 2012]. Dartmouth Institute for Health Policy and Clinical Practice. [cited 2012 Feb 22]. Available at: http://www.dartmouthatlas.org. [Google Scholar]
- 2.Congressional Budget Office, Congress of the United States. [Accessed February 11, 2012];Geographic Variation in Health Care Spending. 2008 Feb; [cited 2012 Feb 22]. Available at: www.cbo.gov.
- 3.Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ. 2002;325:961–964. doi: 10.1136/bmj.325.7370.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein AJ, Nicholson S. The formation and evolution of physician treatment styles: an application to cesarean sections. J Health Econ. 2009;28:1126–1140. doi: 10.1016/j.jhealeco.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Landon BE, Reschovsky J, Reed M, et al. Personal, organizational, and market level influences on physicians’ practice patterns: results of a national survey of primary care physicians. Med Care. 2001;39:889–905. doi: 10.1097/00005650-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Rutkow IM, Gittelsohn AM, Zuidema GD. Surgical decision making. The reliability of clinical judgment. Ann Surg. 1979;190:409–419. doi: 10.1097/00000658-197909000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rutkow IM. Surgical decision making. The reproducibility of clinical judgement. Arch Surg. 1982;117:337–340. doi: 10.1001/archsurg.1982.01380270055012. [DOI] [PubMed] [Google Scholar]
- 8.Fiscella K, Franks P, Zwanziger J, et al. Risk aversion and costs: a comparison of family physicians and general internists. J Fam Pract. 2000;49:12–17. [PubMed] [Google Scholar]
- 9.Billings J, Zeitel L, Lukomnik J, et al. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 10.Hofer TP, Wolfe RA, Tedeschi PJ, et al. Use of community versus individual socioeconomic data in predicting variation in hospital use. Health Serv Res. 1998;33:243–259. [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper RA, Cooper MA, McGinley EL, et al. Poverty, wealth, and health care utilization: a geographic assessment. J Urban Health. 2012;89:828–847. doi: 10.1007/s11524-012-9689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinstein JN, Bronner KK, Morgan TS, et al. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood) 2004;(Suppl Variation):VAR81–VAR89. doi: 10.1377/hlthaff.var.81. [DOI] [PubMed] [Google Scholar]
- 13.Fisher ES, Goodman D, Skinner J. Health care spending, quality, and outcomes; more isn’t always better. [Accessed February 1 2013];A Dartmouth Atlas Project Topic Brief. Available at: www.dartmouthatlas.org.
- 14.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 15.Fisher ES, Wennberg DE, Stukel TA, et al. Variations in the longitudinal efficiency of academic medical centers. Health Aff (Millwood) 2004;(Suppl Variation):VAR19–3VAR12. doi: 10.1377/hlthaff.var.19. [DOI] [PubMed] [Google Scholar]
- 16.Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30:1441–1445. doi: 10.1097/01.brs.0000166503.37969.8a. discussion, 1446–7. [DOI] [PubMed] [Google Scholar]
- 17.Irwin ZN, Hilibrand A, Gustavel M, et al. Variation in surgical decision making for degenerative spinal disorders. Part I: lumbar spine. Spine (Phila Pa 1976) 2005;30:2208–2213. doi: 10.1097/01.brs.0000181057.60012.08. [DOI] [PubMed] [Google Scholar]
- 18.Hosie KB, Cope A, Wai LT, et al. Specialist breast surgeons perform less benign breast operations. Breast. 1994;3:215–217. [Google Scholar]
- 19.Kingsmore D, Ssemwogerere A, Hole D, et al. Specialisation and breast cancer survival in the screening era. Br J Cancer. 2003;88:1708–1712. doi: 10.1038/sj.bjc.6600949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gillis CR, Hole DJ. Survival outcome of care by specialist surgeons in breast cancer: a study of 3786 patients in the west of Scotland. BMJ. 1996;312:145–148. doi: 10.1136/bmj.312.7024.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skinner KA, Helsper JT, Deapen D, et al. Breast cancer: do specialists make a difference? Ann Surg Oncol. 2003;10:606–615. doi: 10.1245/aso.2003.06.017. [DOI] [PubMed] [Google Scholar]
- 22.Langer JC, To T. Does pediatric surgical specialty training affect outcome after Ramstedt pyloromyotomy? A population-based study. Pediatrics. 2004;113:1342–1347. doi: 10.1542/peds.113.5.1342. [DOI] [PubMed] [Google Scholar]
- 23.Schipper PH, Diggs BS, Ungerleider RM, et al. The influence of surgeon specialty on outcomes in general thoracic surgery: a national sample 1996 to 2005. Ann Thorac Surg. 2009;88:1566–1572. doi: 10.1016/j.athoracsur.2009.08.055. discussion, 1572–3. [DOI] [PubMed] [Google Scholar]
- 24.Hall BL, Hsiao EY, Majercik S, et al. The impact of surgeon specialization on patient mortality: examination of a continuous Herfindahl-Hirschman index. Ann Surg. 2009;249:708–716. doi: 10.1097/SLA.0b013e3181a335f8. [DOI] [PubMed] [Google Scholar]
- 25.Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 26.Bentrem DJ, Brennan MF. Outcomes in oncologic surgery: does volume make a difference? World J Surg. 2005;29:1210–1216. doi: 10.1007/s00268-005-7991-x. [DOI] [PubMed] [Google Scholar]
- 27.Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg. 2007;94:145–161. doi: 10.1002/bjs.5714. [DOI] [PubMed] [Google Scholar]
- 28.Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol. 2000;18:2327–2340. doi: 10.1200/JCO.2000.18.11.2327. [DOI] [PubMed] [Google Scholar]
- 29.Killeen SD, O’Sullivan MJ, Coffey JC, et al. Provider volume and outcomes for oncological procedures. Br J Surg. 2005;92:389–402. doi: 10.1002/bjs.4954. [DOI] [PubMed] [Google Scholar]
- 30.Killeen SD, Andrews EJ, Redmond HP, et al. Provider volume and outcomes for abdominal aortic aneurysm repair, carotid endarterectomy, and lower extremity revascularization procedures. J Vasc Surg. 2007;45:615–626. doi: 10.1016/j.jvs.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 31.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142:260–273. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 32.Stolley PD, Becker MH, Lasagna L, et al. The relationship between physician characteristics and prescribing appropriateness. Med Care. 1972;10:17–28. doi: 10.1097/00005650-197201000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Waljee JF, Greenfield LJ, Dimick JB, et al. Surgeon age and operative mortality in the United States. Ann Surg. 2006;244:353–362. doi: 10.1097/01.sla.0000234803.11991.6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuchs VR. The supply of surgeons and the demand for operations. J Hum Resour. 1978;13(Suppl):35–56. [PubMed] [Google Scholar]
- 35.Yip WC. Physician response to Medicare fee reductions: changes in the volume of coronary artery bypass graft (CABG) surgeries in the Medicare and private sectors. J Health Econ. 1998;17:675–699. doi: 10.1016/s0167-6296(98)00024-1. [DOI] [PubMed] [Google Scholar]
- 36.Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293:2609–2617. doi: 10.1001/jama.293.21.2609. [DOI] [PubMed] [Google Scholar]
- 37.Carrier ER, Reschovsky JD, Mello MM, et al. Physicians’ fears of malpractice lawsuits are not assuaged by tort reforms. Health Aff (Millwood) 2010;29:1585–1592. doi: 10.1377/hlthaff.2010.0135. [DOI] [PubMed] [Google Scholar]
- 38.Baicker K, Fisher ES, Chandra A. Malpractice liability costs and the practice of medicine in the Medicare program. Health Aff (Millwood) 2007;26:841–852. doi: 10.1377/hlthaff.26.3.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peabody JW, Luck J, Glassman P, et al. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283:1715–1722. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 40.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]