Abstract
Background
Studies have documented inconsistent emergency anaphylaxis care and low compliance with published guidelines.
Objective
To evaluate anaphylaxis management before and after implementation of an emergency department (ED) anaphylaxis order set and introduction of epinephrine auto-injectors and to measure the effect on anaphylaxis guideline adherence.
Methods
A cohort study was conducted from April 29, 2008-August 9, 2012. Adult ED patients diagnosed with anaphylaxis were included. ED management, disposition, self-injectable epinephrine prescriptions, allergy follow-up and incidence of biphasic reactions were evaluated.
Results
The study included 202 patients. Median age of patients was 45.3 years (IQR 31.3 – 56.4); 139 (69%) were female. Patients who presented after order set implementation were more likely to be treated with epinephrine (51% vs. 33%, OR 2.05, 95%CI 1.04- 4.04) and admitted to ED observation unit (EDOU) (65% vs. 44%, OR 2.38, 95%CI 1.23-4.60) and less likely to be dismissed home directly from ED (16% vs. 29%, OR: 0.47, 95%CI 0.22- 1.00). Eleven patients (5%) had a biphasic reaction. Of these, five (46%) had the biphasic reaction in EDOU; one patient was admitted to intensive care unit (ICU). Six patients (55%) had reactions within 6 hours of initial symptom resolution of whom two were admitted to ICU.
Conclusion
Significantly greater proportions of anaphylaxis patients received epinephrine and were admitted to EDOU after introduction of epinephrine auto-injectors and order set implementation. Slightly over half of the biphasic reactions occurred within recommended observation time of 4-6 hours. These data suggest that the multifaceted approach to changing anaphylaxis management described here improved guideline adherence.
Keywords: anaphylaxis, emergency department, order set, self-injectable epinephrine, clinical decision support
INTRODUCTION
Several studies have demonstrated inconsistent anaphylaxis management in the Emergency Department (ED). A study published by Ross et al. using data from 34 EDs found that only 19% of patients with food-related allergic events received epinephrine as part of management.(1) Similarly, in a study including 15 EDs, only 13% of patients presenting with insect sting anaphylaxis received epinephrine while in the ED.(2) Low rates of self-injectable epinephrine prescriptions and allergist referrals in ED anaphylaxis patients have also been reported in several studies.(2-5) In addition, guidelines recommend that patients with anaphylaxis be observed for 4-6 hours due to the risk of a biphasic reaction, and prolonged observation periods are recommended for patients with severe or refractory symptoms.(6-8)
Epinephrine is the first line treatment for anaphylaxis, and delayed epinephrine administration has been associated with anaphylaxis fatality.(8-11) Epinephrine is available in different doses and concentrations and can be administered via several routes. Dosing errors in epinephrine administration can have potentially lethal consequences.(12) Thus, rapid administration of epinephrine in the setting of anaphylaxis can be challenging, and uncertainty about dosing and risk of error may deter providers from treating patients with epinephrine.
ED management of anaphylaxis is time and resource intensive. In order to ensure timely delivery of key interventions and to prevent omission of important aspects of care, experts have recommended an algorithmic approach.(13) An algorithmic approach was shown to be effective in improving the management of anaphylaxis in pediatric patients but has never been evaluated in adults.(14)
The objective of this study was to evaluate anaphylaxis management before and after the implementation of a multidisciplinary consensus-based emergency department anaphylaxis management order set and introduction of epinephrine auto-injectors, to determine the effect on anaphylaxis guideline adherence and to describe the biphasic reactions that occurred in our cohort.
METHODS
Study design and setting
A retrospective observational cohort study of ED patients presenting with anaphylaxis was conducted from April 29, 2008-August 9, 2012. The study was approved by the institutional review board. Patients were consecutively included at a tertiary care academic ED in southeast Minnesota with 73,000 annual patient visits. The ED includes 51 beds with an additional 10-bed observation unit and is staffed by approximately 35 attending physicians who supervise physician assistants, nurse practitioners, and residents.
Selection of participants
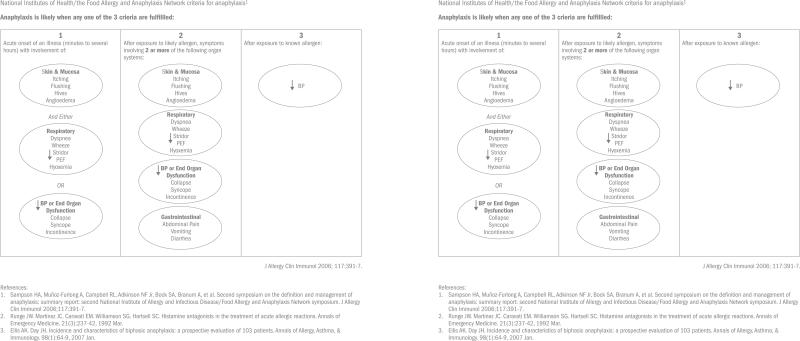
Patients 18 years of age and older who presented to the ED from April 29, 2008 to August 9, 2012 and who were diagnosed with anaphylaxis were eligible for inclusion. Electronic medical records were reviewed to ensure that the National Institute of Allergy and Infectious Disease and Food Allergy and Anaphylaxis Network (NIAID/FAAN) anaphylaxis diagnostic criteria were met.(7)
Intervention
With multidisciplinary input from specialists in emergency medicine, allergic diseases, pharmacy and nursing, we developed an Anaphylaxis Management Order Set designed to optimize the diagnosis, management, observation and safe dismissal of adult ED patients with anaphylaxis (Figure 1). It was then refined after incorporating feedback from key stakeholders in patient care. The ED anaphylaxis management order set included a schematic of the NIAID/FAAN anaphylaxis diagnostic criteria to promote accurate recognition. It also included medication dosing to be used in the ED and continued dosing if the patient was admitted to the ED observation unit (EDOU). Further, the order set included nursing orders to: 1) provide an anaphylaxis education packet to the patient with information about anaphylaxis, epinephrine auto-injector use, and patient advocacy organizations; 2) show a video demonstrating the use of an epinephrine auto-injector; 3) observe the patient demonstrating the proper use of an epinephrine auto-injector and; 4) provide anaphylaxis dismissal instructions with emphasis on allergen avoidance. A recommendation for a self-injectable epinephrine prescription was included along with an automated allergist referral on discharge to encourage optimal follow-up. The automated allergy referral involved an order for the nurse to request an allergy clinic follow up. The allergy clinic received information about the patient referral. The patient was then provided with contact information for the allergy clinic and was required to contact the allergy office to schedule the appointment. Epinephrine auto-injectors [0.3 mg (0.3 ml, 1:1000)] were also added to our automated medication dispensing machines in the ED to simplify dosing and administration of epinephrine.
Figure 1.
Emergency Department Anaphylaxis Management Order Set
The anaphylaxis management order set was made available to ED providers to use at their discretion on May 10, 2009. Providers were oriented to the order set at a 1-hour grand rounds presentation prior to implementation. Automated medication dispensing machines were stocked with epinephrine auto-injectors shortly before order set implementation. The ED Nursing Committee also conducted educational sessions for the nurses on proper use of epinephrine auto-injectors through demonstration with trainer pens. To ensure compliance with training sessions, a demonstration of the use of an epinephrine auto-injector was required as part of the emergency department's annual nurse competency assessment.
Data collection and outcome measures
Data were abstracted from electronic medical records using a standardized data abstraction form. Data were collected on order set use, patient demographics, inciting allergens, epinephrine use, characteristics and management of biphasic reactions, disposition, self-injectable epinephrine prescriptions and allergy follow-up. A biphasic reaction was defined as recurrence of symptoms within 72 hours meeting NIAID/FAAN criteria for anaphylaxis following symptomatic resolution of the initial event.
The outcome measures of interest were administration of epinephrine in the ED, ED disposition of patients, dismissal prescriptions for self-injectable epinephrine, frequency and timing of biphasic reactions, and allergist referral.
Statistical analysis
Continuous data are presented as medians with inter quartile ranges (IQR). Categorical data presented as percent frequency of occurrence were compared using the Chi square test. Logistic regression models were fit to measure the association between order set use and the outcome measures previously described.
Odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were calculated for each association. P-values represent 2-sided hypothesis testing, and p ≤ .05 was considered statistically significant. Statistical analyses were performed using JMP software version 9.0 (SAS Institute Inc, Cary, North Carolina). If no events were observed in a 2 by 2 table, this was corrected by adding a fixed value (+0.5) to all cells to avoid computational errors by dividing by a zero count.(15, 16)
RESULTS
There were 202 patients who presented to the ED with anaphylaxis during the study period. The median age was 45.3 (IQR 31.3-56.4) years; 139 (69%) were female. Approximately 90% of the cohort was Caucasian. A specific trigger was suspected in 75% of the patients (n=152) and was unknown in 25% (n=50). Overall, after ED management, 121 patients (60%) were observed in the EDOU, 39 (19%) were dismissed home from the ED, 11 (5%) were admitted to a general medical floor and 31 (15%) were admitted to an intensive care unit (ICU).
Of the 202 patients, 48 (24%) received care before implementation of order set and 154 (76%) after implementation of order set in our ED. After the introduction of the order set, it was used in 88 (57.2%) of the patients. Table I compares baseline characteristics of patients treated before and after the implementation of the order set. There were no significant differences between the two groups when comparing demographics, suspected triggers, pre-hospital use of epinephrine or history of asthma and cardiovascular disease.
Table I.
Patient characteristics based on order set use
| Characteristic | All Patients (N= 202) No. (%) | Order Set | p-value | |
|---|---|---|---|---|
| Before implementation (N= 48) No. (%) | After implementation (N=154) No. (%) | |||
| Female | 139 (69) | 31 (65) | 108 (70) | 0.47 |
| Age (years) | ||||
| Median (IQR) | 45.3 (31.3- 56.4) | 44.9 (32.8- 58.6) | 45.4 (31.1- 56.2) | 0.28 |
| Range | 18- 98.4 | 21- 98.4 | 18- 89.4 | |
| Race | ||||
| African American | 4 (2) | 0 | 4 (100) | 1.00 |
| White | 187 (93) | 47 (98) | 140 (91) | 0.13 |
| Asian | 2 (1) | 1 (2) | 1 (1) | 0.42 |
| Other/Unknown | 9 (5) | 0 | 9 (6) | 0.46 |
| Suspected trigger | ||||
| Food | 60 (30) | 13 (27) | 47 (31) | 0.65 |
| Medication | 41 (20) | 12 (25) | 29 (19) | 0.35 |
| Venom | 33 (16) | 8 (17) | 25 (16) | 0.94 |
| Other | 18 (9) | 4 (8) | 14 (9) | 1.00 |
| Unknown | 50 (25) | 11 (23) | 39 (25) | 0.74 |
| Prehospital Epinephrine | 31 (15) | 7 (15) | 24 (16) | 0.87 |
| History of Asthma | 46 (23) | 11 (23) | 35 (23) | 1.00 |
| History of cardiovascular disease | 27 (13) | 7 (15) | 20 (13) | 0.81 |
IQR: Interquartile Range.
ED management and disposition are shown in Table II. Patients who presented after order set implementation and epinephrine auto-injector introduction were more likely to be treated with epinephrine (51% vs. 33%, OR 2.05, 95%CI 1.04- 4.04) and admitted to the EDOU (65% vs. 44%, OR 2.38, 95%CI 1.23- 4.60) and less likely to be dismissed home directly from the ED (16% vs. 29%, OR: 0.47, 95%CI 0.22- 1.00). There were no statistically significant differences in the likelihood of receiving an epinephrine auto-injector prescription (62% vs. 54%, OR 1.36, 95% CI 0.71- 2.62), being admitted to the hospital (general medical floors or ICU) (19% vs. 27%, OR 0.62, 95% CI 0.29- 1.33) or allergy follow up (42% vs. 44%, OR 0.94, 95% CI 0.49- 1.81).
Table II.
Univariate analysis of ED management and patient disposition based on order set use
| Characteristic | All Patients (N= 202) No. (%) | Order Set | P value OR (95%CI) | |
|---|---|---|---|---|
| Before implementation (N= 48) No. (%) | After implementation (N=154) No. (%) | |||
| Use of epinephrine in ED | 94 (47) | 16 (33) | 78 (51) | 0.04, 2.05 (1.04- 4.04) |
| ED disposition | ||||
| Home | 39 (19) | 14 (29) | 25 (16) | 0.05, 0.47 (0.22-1.00) |
| Observation unit | 121 (60) | 21 (44) | 100 (65) | 0.009, 2.38 (1.23- 4.60) |
| General Hospital floor | 11 (6) | 4 (8) | 7 (5) | 0.30, 0.52 (0.15- 1.87) |
| Intensive Care Unit | 31 (15) | 9 (19) | 22 (14) | 0.45, 0.72 (0.31- 1.70) |
| General floor or ICU | 42 (21) | 13 (27) | 29 (19) | 0.22, 0.62 (0.29- 1.33) |
| Outcome | ||||
| SIE prescription | 121 (60) | 26 (54) | 95 (62) | 0.35, 1.36 (0.71- 2.62) |
| Allergist follow-up | 86 (43) | 21 (44) | 65 (42) | 0.85, 0.94 (0.49- 1.81) |
CI: Confidence Interval, ED: Emergency Department, ICU: Intensive Care Unit, OR: Odds ratio, SIE: self-injectable epinephrine.
Eleven patients (5%) had a biphasic reaction. All these patients were admitted to the EDOU following the initial reaction. Six of these patients received care guided by order set on presentation of the initial reaction (Table III). Five of the reactions (46%) occurred in the EDOU. All of the reactions in the EDOU occurred within six hours after initial resolution of symptoms. Among these five patients, four of the biphasic reactions were treated with epinephrine, and one patient was admitted to the general medical floor and one to the ICU. Of the remaining six reactions that did not occur in the EDOU, one had a reaction at 3 hours after symptom resolution and all of the rest had reactions occurring at or after 10 hours. Among these patients, two were treated with epinephrine and one patient was admitted to the ICU.
Table III.
Characteristics of patients with biphasic reactions
| Patient | Age (years) | Sex | Before / after Order set implementation | Allergen | Time of onset after resolution (hrs) | History of Asthma | Location of biphasic reaction onset | Biphasic Signs/Symptoms | Treatment of Biphasic Reaction | Disposition after biphasic reaction |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 49 | F | Before | Unknown | 10 | No | Outside | MC/R | H1 | Home |
| 2 | 40 | M | Before | Medication(lidocaine) | 4 | No | EDOU | MC/GI | H1 | GM |
| 3 | 29 | M | Before | Food (fish) | 1 | Yes | EDOU | MC/ R | Epi, H1, B | Home |
| 4 | 31 | M | Before | Unknown | 3 | No | EDOU | MC/R | Epi, H1 | Home |
| 5 | 45 | F | Before | Unknown | 12-16 | No | Home | MC/CV/R | Epi, S, H1, B | Home |
| 6 | 30 | F | After | Food (fibreshake) | 36 | No | Home | MC/R/GI | H2, S, B | EDOU->Home |
| 7 | 64 | F | After | Medication (bactrim) | 24-48 | Yes | Home | MC/R | Epi, S, H1, H2, B | EDOU->Home |
| 8 | 69 | F | After | Medication (aspirin) | 2 | Yes | EDOU | R/GI | Epi, H1, H2, S | EDOU->Home |
| 9 | 60 | F | After | Medication (clindamycin) | 3 | No | Home | MC/GI/R | H1, H2, S, B | EDOU->GM->ICU |
| 10 | 47 | F | After | Food (soy) | 3 | No | EDOU | MC/R/CV | Epi, H1, H2, S, V, I | ICU |
| 11 | 35 | M | After | Unknown | 24 | No | Home | MC/R | H1, H2, S, B | EDOU->Home |
EDOU-Emergency Department Observation Unit, MC- Mucocutaneous Signs/Symptoms, R- Respiratory Signs/Symptoms, GI- Gastrointestinal Signs/Symptoms, CV- Cardiovascular Signs/Symptoms, Epi-Epinephrine, I-Intubation, H1- H1antihistamines, H2-H2 antihistamines, S-Steroids, B-Bronchodilator, V-Vasopressor), ICU- intensive care unit, GM- general medical floor
DISCUSSION
Anaphylaxis management guidelines developed with multidisciplinary representation and endorsed by national and international allergy organizations recommend treatment with epinephrine, a period of observation due to the risk of a biphasic reaction, SIE prescription, and allergy follow up.(6-8)
We found that a significantly greater proportion of anaphylaxis patients received epinephrine and were admitted to the EDOU after introduction of epinephrine auto-injectors and order set implementation. Thus, these data suggest that the multifaceted approach to changing anaphylaxis management described here improved anaphylaxis guideline adherence.
Patients with anaphylaxis present with diverse signs and symptoms involving various organ systems. Rapid diagnosis and appropriate early management is necessary to facilitate an optimal outcome. In a review on ED management of food allergies, Clark and Camargo suggested that an algorithm for the diagnosis and management of anaphylaxis would allow emergency medicine practitioners to more rapidly recognize and treat allergic reactions in the ED.(13) The ED Anaphylaxis Management Order Set described here incorporates diagnosis, management, observation; dismissal and outpatient follow up components of anaphylaxis care.
Intramuscular injection of epinephrine is regarded as the first-line medication in the treatment of anaphylaxis.(17) Furthermore, delayed epinephrine administration has been associated with anaphylaxis fatality.(9-11) Despite the complexities of epinephrine dosing, many EDs do not stock epinephrine auto-injectors. An e-mail survey of local hospitals in southeast Michigan revealed that 6 of 7 hospitals did not stock prefilled intramuscular dose syringes for emergency use in anaphylaxis.(12)
The cost of the epinephrine auto-injector is significantly greater than the 1:1000 epinephrine vial and this difference must be considered in this time of overall increasing healthcare costs.(18) Although, hospital medication costs are difficult to ascertain and can vary widely based on multiple factors, the average wholesale price (AWP) of the autoinjector used in this study was approximately $75.00 US for both the 0.3 mg and 0.15 mg doses compared to the AWP for the 1 mg (1:1000) vial of epinephrine which is $3.00 US.(19) However, safe and accurate epinephrine administration is challenging due to the multiple possible routes of administration, associated dosages, patient acuity and the relatively infrequent need for administration. In addition, adverse cardiovascular complications and fatalities associated with epinephrine dosing are most commonly due to inappropriate dosing.(12) Thus, these risks must be carefully weighed against the increased cost.
We found a significant increase in epinephrine administration in our ED after introduction of the changes described here (33% to 51%). The rate of ED epinephrine administration in our study cohort is higher than in other ED studies of anaphylaxis. Prior studies have shown 13% to 24% of anaphylaxis patients received epinephrine in the ED in the absence of specific interventions to modify anaphylaxis management.(2, 4) However, our findings are similar to a study by Arroabarren and colleagues, who increased epinephrine use with an order set in their pediatric ED from 27% to 57.6%.(14)
Anaphylaxis management does not end with resolution of the acute episode. Patients must be prepared to treat symptom recurrence in case of a biphasic reaction or accidental re-exposure to the trigger. Although the differences in self-injectable epinephrine prescriptions (62% vs. 54%) did not reach statistical significance, the point estimate favored an increase after interventions (OR 1.36 95%CI 0.71- 2.62). Furthermore, our pre-implementation proportion was higher than those reported in previous studies, including an earlier study at our center where we found that 36.6% of patients were prescribed self-injectable epinephrine before ED discharge between 1990 and 2000.(3, 20) Arroabarren found an increase from approximately 7% prior to anaphylaxis order set implementation to 55% after order set implementation, a proportion similar to our pre-implementation proportion.(14) Thus, it is likely that implementation of similar changes in other adult EDs would result in significant increases in self-injectable epinephrine prescriptions.
Despite the inclusion of an automated referral in the order set, we did not find an increase in allergy follow up. The reasons for this are unclear but may be related to the already relatively high proportion of patients who followed up prior to order set implementation (44%).(2, 4) This is higher than the post-implementation referral rate in the Arroabarren study in pediatric patients (38%).(14) Furthermore, it may be that a significant amount of patients already had established allergy care prior to the ED visit. We did not collect data on how many patients had been evaluated by an allergist prior to the ED visit. However, we did collect data on the proportion of patients who had a prior prescription for self-injectable epinephrine and found that 40% of patients in our cohort did have a previous auto-injector prescription (data not shown) suggesting that they had previously been evaluated for anaphylaxis. Finally, because the referral was automated, providers may not have spent as much time discussing the importance of follow up with the patient. Further studies are needed to elucidate methods to ensure appropriate follow up after an ED visit for anaphylaxis.
Patients presenting with anaphylaxis should be observed due to the risk of a biphasic reaction. However, the time period of observation is controversial. Guidelines recommend that patients be observed for 4-6 hours and for longer periods if they present with severe or refractory symptoms.(7) The relatively low incidence of biphasic reactions and the time range of onset in our study are consistent with other retrospective studies.(21-23) Overall, 6 (55%) of patients had the onset of biphasic symptoms during the recommended time frame of observation in published guidelines. We found that after the implementation of the order set, patients were more likely to be admitted to the EDOU and less likely to be dismissed home. Although not statistically significant, admissions to the ICU or general medical floor decreased somewhat. We also found that all but one of the patients who experienced the onset of biphasic symptoms in the EDOU were treated with epinephrine and one (20%) was admitted to the ICU, demonstrating the need for additional interventions and underscoring the importance of observation. However, the benefits of observation must be weighed against the increased length of stay considering that the vast majority of patients did not experience a biphasic reaction. Additional studies are needed to evaluate the cost-effectiveness of observation and to identify patients who have the greatest risk of experiencing a biphasic reaction.
LIMITATIONS
Our study is limited by its retrospective design and relatively small sample size. Although the uneven cohort sizes (before and after implementation) could introduce statistical bias, when comparing these two groups we found no significant differences. Also the “before implementation” cohort was the closest to the standard practice in our ED, and going back further in time (earlier than 2008) to increase the cohort before implementation would potentially introduce even more biases secondary to different treatments and standards of care. Furthermore, this is a single center study and the findings may not be generalizable to other academic centers or community practices. Multicenter prospective studies are needed for further evaluation.
CONCLUSION
In conclusion, patients treated following implementation of the order set and introduction of the epinephrine auto-injectors were more likely to receive epinephrine in the ED, be admitted to the EDOU and less likely to dismissed directly from the ED. The multifaceted approach described here addresses the complexities of anaphylaxis management and data suggest that implementation of such an approach in the ED may increase guideline compliance in anaphylaxis patients. Additional multidisciplinary collaborations including allergists and emergency physicians are needed to encourage the use of algorithms such as the one presented here to continue to improve ED anaphylaxis care and identify barriers to allergy follow up after the ED visit.
Highlights box.
1. What is already known about this topic?
Inconsistent emergency anaphylaxis care and low compliance with published guidelines have been documented in studies. An algorithmic approach was shown to be effective in improving the management of anaphylaxis in pediatric patients.
2. What does this article add to our knowledge?
The article provides an evaluation of anaphylaxis management before and after implementation of an emergency department (ED) anaphylaxis order set and introduction of epinephrine auto-injectors and measures the effect on anaphylaxis guideline adherence in adults.
3. How does this study impact current management guidelines?
The multifaceted approach described here addresses the complexities of anaphylaxis management and data suggest that implementation of such an approach in the ED may increase guideline compliance in anaphylaxis patients.
Acknowledgments
This publication was supported by NIH/NCRR/NCATS CTSA Grant Number UL1 RR024150. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Abbreviations
- CI
Confidence Interval
- ED
Emergency Department
- EDOU
Emergency Department Observation Unit
- ICU
Intensive Care Unit
- IQR
Interquartile Range
- NIAID/FAAN
National Institute of Allergy and Infectious Disease and Food Allergy and Anaphylaxis Network
- OR
Odds ratio
- SIE
self-injectable epinephrine
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ross MP, Ferguson M, Street D, Klontz K, Schroeder T, Luccioli S. Analysis of food-allergic and anaphylactic events in the National Electronic Injury Surveillance System. J Allergy Clin Immunol. 2008 Jan;121(1):166–71. doi: 10.1016/j.jaci.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Clark S, Long AA, Gaeta TJ, Camargo CA., Jr. Multicenter study of emergency department visits for insect sting allergies. J Allergy Clin Immunol. 2005 Sep;116(3):643–9. doi: 10.1016/j.jaci.2005.06.026. [DOI] [PubMed] [Google Scholar]
- 3.Campbell RL, Luke A, Weaver AL, St Sauver JL, Bergstralh EJ, Li JT, et al. Prescriptions for self-injectable epinephrine and follow-up referral in emergency department patients presenting with anaphylaxis. Ann Allergy Asthma Immunol. 2008 Dec;101(6):631–6. doi: 10.1016/S1081-1206(10)60227-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark S, Bock SA, Gaeta TJ, Brenner BE, Cydulka RK, Camargo CA. Multicenter study of emergency department visits for food allergies. J Allergy Clin Immunol. 2004 Feb;113(2):347–52. doi: 10.1016/j.jaci.2003.10.053. [DOI] [PubMed] [Google Scholar]
- 5.Gaeta TJ, Clark S, Pelletier AJ, Camargo CA. National study of US emergency department visits for acute allergic reactions, 1993 to 2004. Ann Allergy Asthma Immunol. 2007 Apr;98(4):360–5. doi: 10.1016/S1081-1206(10)60883-6. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol. 2010 Sep;126(3):477–80. e1–42. doi: 10.1016/j.jaci.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 7.Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF, Jr., Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report--Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006 Feb;117(2):391–7. doi: 10.1016/j.jaci.2005.12.1303. [DOI] [PubMed] [Google Scholar]
- 8.Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World allergy organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J. 2011 Feb;4(2):13–37. doi: 10.1097/WOX.0b013e318211496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bock SA, Munoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001 Jan;107(1):191–3. doi: 10.1067/mai.2001.112031. [DOI] [PubMed] [Google Scholar]
- 10.Bock SA, Munoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001-2006. J Allergy Clin Immunol. 2007 Apr;119(4):1016–8. doi: 10.1016/j.jaci.2006.12.622. [DOI] [PubMed] [Google Scholar]
- 11.Greenberger PA, Rotskoff BD, Lifschultz B. Fatal anaphylaxis: postmortem findings and associated comorbid diseases. Ann Allergy Asthma Immunol. 2007 Mar;98(3):252–7. doi: 10.1016/S1081-1206(10)60714-4. [DOI] [PubMed] [Google Scholar]
- 12.Kanwar M, Irvin CB, Frank JJ, Weber K, Rosman H. Confusion about epinephrine dosing leading to iatrogenic overdose: a life-threatening problem with a potential solution. Ann Emerg Med. 2010 Apr;55(4):341–4. doi: 10.1016/j.annemergmed.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Clark S, Camargo CA., Jr Emergency management of food allergy: systems perspective. Curr Opin Allergy Clin Immunol. 2005 Jun;5(3):293–8. doi: 10.1097/01.all.0000168797.14487.73. [DOI] [PubMed] [Google Scholar]
- 14.Arroabarren E, Lasa EM, Olaciregui I, Sarasqueta C, Munoz JA, Perez-Yarza EG. Improving anaphylaxis management in a pediatric emergency department. Pediatr Allergy Immunol. 2011 Nov;22(7):708–14. doi: 10.1111/j.1399-3038.2011.01181.x. [DOI] [PubMed] [Google Scholar]
- 15.The Cochrane Collaboration Higgins JPT, S G, editors. Rare events (including zero frequencies) Cochrane Handbook for Systematic Reviews of Interventions Version 510. 2011 Chapter 16.9. [updated March 2011] [Google Scholar]
- 16.Simel DL, Bossuyt PM. Differences between univariate and bivariate models for summarizing diagnostic accuracy may not be large. J Clin Epidemiol. 2009 Dec;62(12):1292–300. doi: 10.1016/j.jclinepi.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World Allergy Organization anaphylaxis guidelines: summary. J Allergy Clin Immunol. 2011 Mar;127(3):587–93. e1–22. doi: 10.1016/j.jaci.2011.01.038. [DOI] [PubMed] [Google Scholar]
- 18.Westermann-Clark E, Fitzhugh DJ, Lockey RF. Increasing cost of epinephrine autoinjectors. J Allergy Clin Immunol. 2012 Sep;130(3):822–3. doi: 10.1016/j.jaci.2012.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Red Book. NJ Thomson PDR; Montvale: 2010. [Google Scholar]
- 20.Rudders SA, Banerji A, Corel B, Clark S, Camargo CA., Jr. Multicenter study of repeat epinephrine treatments for food-related anaphylaxis. Pediatrics. 2010 Apr;125(4):e711–8. doi: 10.1542/peds.2009-2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellis AK, Day JH. Incidence and characteristics of biphasic anaphylaxis: a prospective evaluation of 103 patients. Ann Allergy Asthma Immunol. 2007 Jan;98(1):64–9. doi: 10.1016/S1081-1206(10)60861-7. [DOI] [PubMed] [Google Scholar]
- 22.Kemp SF. The post-anaphylaxis dilemma: how long is long enough to observe a patient after resolution of symptoms? Curr Allergy Asthma Rep. 2008 Mar;8(1):45–8. doi: 10.1007/s11882-008-0009-7. [DOI] [PubMed] [Google Scholar]
- 23.Smit DV, Cameron PA, Rainer TH. Anaphylaxis presentations to an emergency department in Hong Kong: incidence and predictors of biphasic reactions. J Emerg Med. 2005 May;28(4):381–8. doi: 10.1016/j.jemermed.2004.11.028. [DOI] [PubMed] [Google Scholar]