Abstract
Objectives
To evaluate the effect of different pathways for developing a life story book (LSB) for people with dementia.
Method
Preliminary randomised control trial; 23 people with dementia in care homes (mean age 86) randomly assigned to receive either 12 individual life review sessions and co-creating a LSB or a personal LSB created by their relatives as a ‘gift’
Results
No difference in quality of life (quality of life–Alzheimer's disease (QOL–AD)) was observed between the two groups, six weeks after having received the LSB (F(1,20) = 0.08, p = 0.77). At this point, QOL–AD had improved for both groups, but there was a significant between-group difference at an intermediate assessment immediately after the life review sessions had been completed, before the LSBs were received (F(1, 20) = 5.11, p = 0.035), in favour of life review. A similar pattern was observed on autobiographical memory (extended autobiographical memory interview), with the life review group improving significantly more than the gift group during the life review sessions, but no difference was observed once all participants had had their LSB for six weeks. After the LSBs were produced – by either pathway – quality of relationship as rated by relatives improved significantly (F(2, 39) = 19.37, p < 0.001) and staff knowledge regarding the resident and attitudes to dementia improved.
Conclusion
The creation of LSBs – either through a life review process or by relatives without involving the person with dementia – has benefits for people with dementia, relatives and staff in care homes. However, undertaking a life review requires training and supervision.
Keywords: reminiscence, care home, older adult, staff and relatives
Introduction
A recent systematic review suggests that individual reminiscence work, using a life review or life story process, shows potential psychosocial benefits for people with dementia (Subramaniam & Woods, 2012). Benefits reported include enhanced well-being (Lai, Chi, & Kayser-Jones, 2004); improvements in mood and some components of cognitive function (Haight, Gibson, & Michel 2006; Morgan & Woods, 2010); and reductions in disorientation and anxiety and improvements in self-esteem, memory and social interaction (Tabourne, 1995). The use of a life review process to develop a life story book appeared to be associated with the most positive results with people with dementia (Haight et al., 2006; Morgan & Woods, 2010) and the review concluded that this approach merits further exploration.
Garland and Garland (2001) describe life review as a highly structured form of reminiscence, which allows the participant to ascribe meaning and value to his/her life, and to come to terms with uncomfortable issues. A definition is provided by Woods, Spector, Jones, Orrell, and Davies (2005): ‘Life review typically involves individual sessions, in which the person is guided chronologically through life experiences, encouraged to evaluate them, and may produce a life story book’ (p. 1). A life review process then helps a person with dementia to recount and evaluate his or her life history in chronological order. The process can be represented in tangible form as a life story book, photo album, scrap book, memory box or memory book.
Initially, life story books or scrapbooks were created for work with children in care before the concept was adapted for older adults (Gibson, 1994). Life story books are now very popular in the dementia care field, and in 2011 in England, the Department of Health provided the funding to train 500 people to carry out life story work with people with dementia (see www.lifestorynetwork.org.uk). Life story books have the potential to act as a tangible self- reminder and help to maintain a sense of continuity for people with memory difficulties.
A key area of uncertainty in this field relates to whether a life story book can be created for a person with dementia without the person's engagement in a life review process. Family members may often create a ‘This is your life’ book for their relative, combining photographs and words, and various templates are available to assist this. For example, Dementia UK provides a life story template with associated guidance (see www.Dementiauk.org). Such a book may be presented as a gift to the person, a tangible reminder of memories across the lifespan. Where the person has a severe cognitive impairment, involvement in life review may not be feasible, and this may be the only option. Given that the life review process can be time-consuming, and require input from trained, skilled and supervised practitioners, the question must be posed as to whether the combined life review/life story book approach has added value compared with the simpler process of producing a life story book with family members that may be given to the person as a gift.
Haight et al. (2003) have emphasised the important role of the person with dementia in having editorial control and decision-making power throughout the process of developing the book, with the life review and creation of the book proceeding hand in hand. However, Morgan and Woods (2010) noted that it appeared that improvements in mood were associated with the period after the completion of the book, with reports from participants emphasising the value they placed on the book per se. The principal aim of the current study is to seek to address this gap in our knowledge regarding life review and life story books, and, for the first time, examine whether a life story book produced without a life review process has equivalent benefits to the combined approach that has previously been shown to have therapeutic benefits.
The two previous studies on the combined life review/life story book intervention (Haight et al., 2006; Morgan & Woods, 2010) reported positive outcomes in comparison with treatment as usual controls, in relation to mood and aspects of cognition, but did not evaluate self-reported quality of life (QOL) directly. The current study additionally aims, in its first phase, to evaluate the effects of the combined approach on QOL in people with dementia, in comparison with people with dementia receiving usual care.
Woods et al. (2005) recommend that outcomes for family members and other caregivers also be evaluated in studies of reminiscence work. We hypothesise that the close involvement of relatives in the ‘gift’ group in the production of the life story book will lead to an improvement in the quality of relationship between the relative and the person with dementia after the book has been presented. A previous study (Baines, Saxby, & Ehlert, 1987) has shown improvements in care staff knowledge regarding residents’ personal details following group reminiscence work. We hypothesise that having access to residents’ life story books will improve care staff knowledge and also be associated with improved attitudes to people with dementia, reflecting person-centred care, irrespective of whether the book was produced by the person with dementia or their relative.
The research questions addressed by this study may accordingly be summarised as follows:
-
(1)
Does a life review intervention, resulting in a life storybook, have a positive effect on QOL (primary outcome), mood and autobiographical memory among older adults with dementia living in care homes compared with care as usual?
-
(2)
Does a life story book produced through a life review process improve QOL (primary outcome), mood and autobiographical memory among older adults with dementia living in care homes, when compared with a life story book produced for the participant without their involvement?
-
(3)
Does involving a relative in the production of a life story book for a resident with dementia lead to improvement in the quality of their relationship as perceived by relative and resident?
-
(4)
Does providing a life story book for a resident with dementia lead to changes in staff knowledge and attitudes?
Method
Design
This was a preliminary randomised, single blind controlled trial, with two parallel arms, assessed at 12 weeks (primary time-point for research question 1) and 18 weeks after baseline (primary time-point for research question 2).
Participants
The participants were all residents of care homes in North Wales (all but one privately owned). In total, 19 care homes were contacted and 14, with a total of 515 residents, agreed to an initial briefing meeting. Following this, the home manager or deputy manager together with the researcher scrutinised the list of residents at the care home to identify potential participants. The inclusion criteria for the study required the person to be a care home resident with a formal diagnosis of dementia, using the criteria from the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2000), in the mild to moderate range. Degree of dementia was operationalised with the clinical dementia rating (CDR) (Hughes, Berg, Danziger, Coben, & Martin, 1982). Participants were only included if judged to have mental capacity to give consent and had a relative willing and able to participate. Exclusion criteria included severe uncorrected impairment in vision or hearing, current or previous major psychiatric disorder and insufficient verbal ability in English to complete assessments. A total of 93 potential participants with a dementia diagnosis were shortlisted for further screening. Three care homes which had shortlisted 30 potential participants subsequently withdrew from the research. Ten potential participants’ relatives did not agree to participate, being too busy or living too distant from the care home. Seven potential participants refused to take part in the research (e.g. ‘not interested’, ‘tired’, ‘no time’), and three declined because they preferred to communicate through the medium of Welsh. Five potential participants were excluded as their dementia was rated as being severe, four in view of psychiatric disorders (schizophrenia, bipolar disorder) and four due to speech impairment. Five potential participants became ill or died before baseline assessment and one did not have an available relative. Thus 24 participants were eligible and entered the study (see Figure 1).
Figure 1.
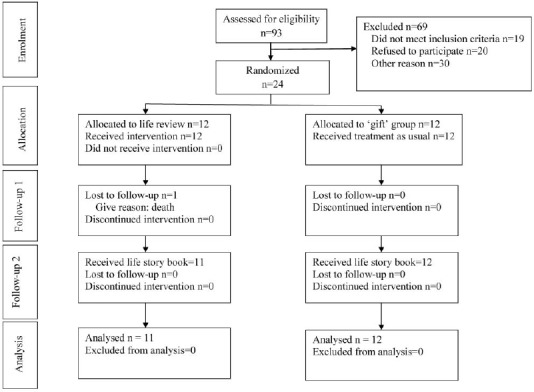
Consort flowchart of study.
Randomisation
Participants were allocated, following baseline assessment, to the two intervention conditions using a sequential individual-based randomisation, which randomises participants into parallel groups using a dynamic stratification algorithm (Schulz, Altman, & Moher, 2010). Each allocation aims to reduce any imbalance in the stratifying variables – in this case, gender. Even when the sample size is small, as in this case, the method ensures approximately equal balanced groups. The entire randomisation process was carried out by the North Wales Organisation for Randomised Trials in Health & Social Care, an accredited clinical trials unit.
Procedure
This project obtained ethical approval from the School of Psychology, Bangor University and the North Wales NHS Research Ethics Committee before commencing with other research procedures. Data were collected from April 2010 until November 2011.
Participants were identified through a number of care homes around North Wales. Potential eligible participants were approached by the care home managers with an information sheet describing the project in order to ascertain whether they would be interested to discuss the project further with the researcher. The home manager also approached relatives to ascertain their opinion. Where both parties were in agreement, the researcher would proceed to screen the eligibility of potential participants in order to establish inclusion criteria and securing written informed consent from participants and their relatives.
After baseline assessments were completed, participants were randomly allocated to either the ‘life review’ group or the ‘gift’ group. Participants in the life review group received 12 individual sessions undertaking the life review process leading to the development of their own life story book. Meanwhile, participants’ relatives in the gift group worked over the 12-week period, without involving the person with dementia, developing with the researcher a life story book for their relative. After the initial post-intervention assessment at the 12th week after baseline, each participant received their own completed life story book, with the gift group receiving this as a surprise gift. Each life story book recounted the life story of the participant in chronological order, illustrated with pictures from their childhood until the current time at the care home. Each page, story and picture was labelled clearly, e.g., where, when, what occasion and so on. The life story books, developed through life review sessions, also contained quotations from the person with dementia matched with appropriate pictures. Some information and pictures, e.g., school, church, car and place of work, were obtained from internet resources. On average, each book consisted of 50–70 pages and three copies of the life story book were printed; one copy with professional binding was given to the participant, and copies with comb binding were given to the participant's relative and to the care home's staff. A further assessment was carried out 6 weeks after the participant had received the life story book.
Intervention
The therapist (PS) was a qualified clinical psychologist from Malaysia undertaking doctoral studies in the UK. Clinical supervision was provided weekly with a consultant clinical psychologist (BW) with many years’ experience of reminiscence work. Prior to implementing the life review work, the therapist undertook supervised training in group reminiscence work for three months and became familiar with the assessment tools to be used working with older adults with dementia living in the community as part of the REMCARE project (Woods et al., 2009).
Life review/life story book intervention
The life review intervention was based on Haight's Life Review model and Life Review Experiencing Form (LREF; Haight, 1992). The purpose of the LREF is to achieve consistency of the life review process between participants (Haight, 1988). As explained by Haight (1988), therapists do not have to ask all the questions on the LREF, but can follow the lead of the reviewer. The initial focus is on childhood and adolescence, and then family, home and adulthood; the final phase addresses the summary portion of the life review. In this study, an average of 12 sessions (range 11–16 sessions) of life review over a 12-week period were needed to complete the process. Participants typically received an hour of life review work on a weekly basis. Some participants’ sessions were briefer (e.g., 30 minutes) due to the person having difficulty in continuously engaging in the life review process. However, this was compensated for by having two sessions in a week. The summarising aspect is considered important as it assists the person in evaluating and integrating life's events (Haight, 1988). The life story book was developed according to the progress of the life review process. Participants played an active and decisive role in creating their own life story book. After each life review session, the therapist would draft sections and edit the book to integrate previous information with new information, to be checked and endorsed by participant. The therapist reviewed the contents of the book with the participant during the following session to finalise the contents according to the previous life review session. The therapist liaised with the person's family to obtain suitable photographs and memorabilia. The pictures and the draft life story book from the previous session were important tools in helping participants engage in the life review sessions. Basically, the therapist's role in developing the life story book is primarily as ‘secretary’.
Life story book as gift intervention
Participants in the gift group were not involved in developing their own life story book. The researcher worked closely with the participant's relative, meeting with them five or six times over the period of 12 weeks to develop a life story book, illustrated with photographs and pictures to be given as a gift for their relative.
Measures
The administration of all tests at baseline was carried out by the researcher (PS) face to face with each participant. The 12- and 18-week assessments were carried out by two assessors who were blind to treatment allocation, and had no other involvement in the process of the research.
Clinical dementia rating (CDR) scale (Hughes et al., 1982)
The CDR was used to assess the severity of the person's dementia. The CDR scale is a clinician-rated dementia staging systems that tracks the progression of cognitive and functional deterioration, from 0 (healthy) through 0.5 (questionable dementia), 1 (mild dementia), 2 (moderate dementia) to 3 (severe dementia). The CDR scale stages are determined on the basis of the presumed order in which specific cognitive and functional abilities are lost during the usual natural course of Alzheimer's disease (Rush, First, & Blacker, 2008), combining information about changes in memory, orientation, judgement/problem solving and day to day function. The CDR has been reported to have good concurrent validity with other measures, good test–retest reliability and inter-rater reliability (r = 0.89) (Hughes et al., 1982). For this study, the CDR was rated after consulting the clinical records, feedback from staff, family members and from one-to-one interview with the participant.
Quality of life-Alzheimer's disease (QOL-AD; Logsdon, Gibbons, McCurry, & Teri, 2002)
The QOL-AD is a 13-item questionnaire designed to provide both a self-report and a caregiver (proxy) report of the QOL of the person with dementia. To facilitate its use with cognitively impaired individuals, the QOL-AD uses simple and straightforward language; responses are structured in a four-choice format that is consistent across all questions, and all items are rated according to the person's current QOL. The QOL-AD takes an average of 10 minutes to administer in an interview format. Overall scores were computed for the self-reports by summing the 13 items, for a total possible score ranging from 13 to 52, with higher scores indicating higher QOL (Logsdon et al., 2002). This tool has been reported to be valid and reliable when used with people with mild to moderate dementia in structured format (Hoe, Hancock, Livingston, & Orrell, 2006; Thorgrimsen et al., 2003). Only the participant version was used in this study, as all participants were able to provide an account of their own QOL.
The Autobiographical Memory Interview, Extended version (AMI, Kopelman, Wilson, & Baddeley, 1990; AMI-E, Woods et al., 2009)
The AMI was developed by Kopelman et al. (1990) as a semi-structured interview schedule with two sub-scales, the personal semantic schedule (PSS) and the autobiographical incident schedule (AIS). It was constructed to assess the recall of autobiographical incidents and of ‘personal semantic’ facts about the person's life across three broad phases of the lifespan: ‘childhood’, ‘early adult life’, and ‘recent’ events or facts. Personal semantic memory refers to factual knowledge about a person's own past (e.g., addresses where lived, names of teacher or friends or colleagues at work, etc.), and ‘autobiographical incidents’ to events recounted with descriptive richness and specificity in time and place (Kopelman, 1992). Kopelman et al. (1990) reported inter-rater reliability correlations of 0.83–0.86 between testers. The extended version, AMI-E (Woods et al., 2009), has additional sections relating to the middle years of the person's life to increase its relevance with older adults. Inter-rater reliability of the extended form was assessed alongside the current study with 25 people with dementia taking part in the REMCARE trial (Woods et al., 2009). Agreement (Pearson's correlation) between raters ranged from 0.70 to 0.98 for the different sections. For the middle to late adulthood PSS, the correlation between scores was 0.92 and for the middle to late adulthood AIS 0.90. Overall, the inter-rater reliability was 0.97 for the AMI (extended) PSS and 0.91 for the AMI (extended) AIS. These results indicate that the AMI-E has good inter-rater reliability values consistent with Kopelman's report (1990) for the original instrument.
The Geriatric Depression Scale (Residential) (GDS-12R, Sutcliffe et al., 2000)
The Geriatric Depression Scale (Residential) (GDS-12R) was developed from the 15-item version of the Geriatric Depression Scale (Sheikh & Yesavage, 1986) to measure depression levels in older adults in residential settings. The GDS-12R has greater internal reliability than the 15-item version. According to Sutcliffe et al. (2000), the GDS-12R provides researchers with a brief, easy-to-administer depression scale that is relevant to residential and nursing home populations.
Quality of the caregiving relationship questionnaire (QCPR) (Spruytte, Van-Audenhove, Lammertyn, & Storms, 2002)
This questionnaire seeks the view of the person with dementia of their relationship with their relative. The quality of caregiving relationship questionnaire (QCPR) consists of 14 items with two sub-scales, ‘warmth’ and ‘absence of conflict or criticism’ with internal consistency reported as 0.82 (Spruytte et al., 2002). The participant is required to respond on a 5-point Likert scale from ‘totally disagree’ to ‘totally agree’ with higher scores on both sub-scales indicating better relationship quality. The same questionnaire was also completed by the participant's relative evaluating their perspective of their relationship with the person with dementia.
Approaches to Dementia Questionnaire (ADQ) (Lintern, Woods, & Phair, 2000)
Staff attitudes were evaluated with the Approaches to Dementia Questionnaire (ADQ), which contains 19 Likert style statements; each scored from 1 (strongly disagree) to 5 (strongly agree). This measure has been widely used to assess staff attitudes to people with dementia (e.g., Zimmerman et al., 2005). It comprises two sub-scales, derived from factor analysis, ‘hope’ and ‘person-centred’, and can be summed to form a total score. The hopefulness sub-scale consists of eight items, reflecting a hopeful attitude to dementia, whereas the person-centred sub-scale consists of 11 items indicating recognition of personhood in dementia. Items are scored so that higher scores indicate more positive attitudes. Lintern (2001) reported Cronbach's internal consistency of .76 for hopefulness, .85 for person-centred care and .83 for total ADQ scores.
Staff knowledge of care-recipient questionnaire
This brief questionnaire was developed specifically for this study to measure care staff knowledge about residents. It comprises 14 questions asking the staff member to write down (without consulting the home's records) details regarding the participant such as his/her hobbies, favourite food, birthplace, school, etc. Each item was scored as ‘correct’ (where the answer given was consistent with the information provided by the participant and relatives), ‘incorrect’ (for an answer that was inconsistent with the information available from participant or relatives) or ‘don't know’ (where no answer was given). Higher numbers of ‘correct’ and lower numbers of ‘incorrect’ or ‘don't know’ answers indicated better knowledge, with a range from 0 to 14.
Statistical analysis
Baseline differences between the two groups on demographic variables were assessed with the Fisher's exact test for categorical variables and independent samples t-test for continuous variables. One-way between-group analyses of covariance (ANCOVA) were used for the main analyses, with the baseline score on the outcome measure entered as a covariate (Vickers & Altman, 2001). Three variables, GDS-12R, AMI-E AIS sub-scale and QCPR's conflict sub-scale, rated by the participant did not meet the assumptions of normality and were transformed before entry into the analysis (Pallant, 2010). Square root transformation was used for GDS-12R and AMI-E AIS. The QCPR's conflict sub-scale data were subject to a reflect and inverse transformation. Repeated measures analyses of variance (ANOVAs) were used to examine changes over time, with post hoc, paired t-tests comparisons using the Bonferroni correction. For staff data, between-group comparisons were not carried out, as staff may have had contact with residents in both groups, and the hypothesis was not specific to the method of production of the life story book.
Research question 1 was evaluated by comparing scores between the groups at the intermediate assessment (time 2), with baseline (time 1) as covariate, at the conclusion of the life review sessions. Research question 2, the effect of different approaches to the development of life story books, was evaluated by analysis of the final follow-up (time 3) scores, with baseline (time 1) as covariate, of the two groups. Research question 3 was evaluated by comparing scores at the intermediate assessment and at follow-up, with baseline as covariate, on the quality of relationship scale rated by participants and relatives. Research question 4 was evaluated by comparing scores of care staff before the life story book was developed with those after residents with dementia had received their life story book.
Results
Demographic and descriptive results
A total of 24 participants were randomly allocated to the life review group or to the ‘gift’ group. However, one participant from the life review group died in week 7, having participated in seven life review sessions. As no post-treatment data were available from this participant, data are presented for the remaining 23 who completed the study. Thus, there were 11 participants in the life review/life story book group and 12 participants in the life story as gift group.
Table 1 summarises the demographic information on these participants. There were no statistical differences between groups in age, gender, marital status, length of stay, diagnosis and CDR tested by Fisher's exact test (categorical variables) and independent samples t-test (continuous variables). The mean age was 86.48 (standard deviation (SD) 6.48; range 73–99), 16 (69%) were female, 18 (78%) widowed and the mean duration of living in a care home was 25.30 months (SD 9.52; range 25–51). On the CDR, 11 (47%) were assessed as having a mild degree of dementia, with the remainder being in the moderate range. Sub-type of dementia is typically not consistently recorded in care home records; four residents were specifically noted as having Alzheimer's disease and four as having vascular dementia; the remaining 15 had ‘dementia unspecified’. Six participants were receiving donepezil, an acetylcholinesterase inhibitor (AChEI). Psychotropic medication was being received by seven (30%) of the participants, most commonly anti-depressants, with three (13%) receiving anti-psychotic medication.
Table 1.
Summary of participants’ demographic information.
| Randomised participants n = 23 |
|||
|---|---|---|---|
| Life review group (n = 11) | Gift group (n = 12) | Fisher's exact test | |
| Characteristics | n (%) or mean (SD) | n (%) or mean (SD) | Statistics sig. |
| Age | 84.5 (6.7) | 88.3 (6.0) | p = 0.18a |
| Gender | |||
| •Male | n = 3 (27.3) | n = 4 (33.3) | p > 0.99 |
| •Female | n = 8 (72.7) | n = 8 (66.7) | |
| Marital status | |||
| •Married | n = 3 (27.3) | n = 2 (16.7)) | p = 0.64 |
| •Widowed | n = 8 (72.7) | n = 10 (83.3) | |
| Lengtd of stay (montds) | 26.5 (9.0) | 24.5 (10.2) | p = 0.56a |
| CDR | |||
| •Mild | n = 5 (45.5) | n = 6 (50.0) | p > 0.99 |
| •Moderate | n = 6 (54.5) | n = 6 (50.0) | |
| Medication | |||
| (i) Antidepressants | |||
| •Yes | n = 3 (27.3) | n = 3 (25.0) | p > 0.99 |
| •No | n = 8 (72.7) | n = 9 (75.0) | |
| (ii) Antipsychotics | |||
| •Yes | n = 2 (18.2) | n = 1 (8.3) | p = 0.59 |
| •No | n = 9 (81.8) | n = 11 (91.7) | |
| (iii) Anxiolytics | |||
| •Yes | n = 1 (9.1) | n = 2 (16.7) | p > 0.99 |
| •No | n = 10 (90.9) | n = 10 (83.3) | |
| (iv) AChEIs | |||
| •Yes | n = 3 (27.3) | n = 3 (25.0) | p > 0.99 |
| •No | n = 8 (72.7) | n = 9 (75.0) | |
Independent samples t-test.
The mean age of the 23 relatives who participated in the study was 64.65 (SD 10.74; range 44–83); 15 relatives (65%) were female. On the relationship with person with dementia, nine (39%) were daughters, four (17%) were sons and the rest 10 (43%) were made up of a variety of other relationships: nephew, brother, niece, son-in-law, wife, husband, daughter-in-law, sister and cousin.
The 68 care staff who participated in the study were predominantly female 62 (91%) with a mean age of 39.04 (SD 12.20; range 20–64). Their mean length of experience working in care homes was 8.31 years (SD 8.79; range 1–40). In terms of qualifications, 9 (13%) staff had no qualifications, 22 (32%) had achieved NVQ1 at level 1 or 2, 20 (29%) had NVQ at level 3 or 4, and 17 (25%) were educated to degree level. Only 3 (4%) were employed as registered nurses.
Research question 1: the effect of life review process compared with usual care (Table 2)
Table 2.
Intervention outcomes: the effect of life review and life story book.
| Baseline Mean (SD) | Post-intervention Mean (SD) | n | ANCOVA F(1, 20), p value | 6-week follow-up from post-intervention Mean (SD) | ANCOVA F(1, 20), p value | |
|---|---|---|---|---|---|---|
| QOL-AD | ||||||
| Life review | 30.1 (8.5) | 36.9 (6.9) | 11 | 5.11, p = 0.035* | 36.1 (7.8) | 0.08, p = 0.77 |
| Gift | 35.7 (2.5) | 35.5 (4.7) | 12 | 38.6 (3.8) | ||
| +GDS-12R | ||||||
| Life review | 4.7 (3.1) | 4.3 (3.7) | 11 | 0.93, p = 0.34 | 3.5 (2.7) | 0.14, p = 0.71 |
| Gift | 2.6 (1.4) | 2.5 (1.8) | 12 | 2.7 (1.7) | ||
| AMI-E | ||||||
| •PSS | ||||||
| Life review | 31.0 (19.7) | 36.3 (21.6) | 11 | 14.01, p = 0.001* | 35.4 (19.4) | 3.98, p = 0.060 |
| Gift | 36.7 (15.5) | 28.9 (18.3) | 12 | 33.3 (16.6) | ||
| •+AIS | ||||||
| Life review | 3.4 (2.8) | 8.2 (8.2) | 11 | 10.12, p = 0.005* | 6.6 (5.4) | 0.50, p = 0.49 |
| Gift | 6.5 (4.4) | 5.8 (4.1) | 12 | 8.6 (6.6) | ||
| •AMI total | ||||||
| Life review | 34.4 (22.0) | 44.5 (28.5) | 11 | 19.92, p < 0.001* | 42.0 (23.5) | 2.92, p = 0.10 |
| Gift | 43.2 (19.1) | 34.7 (21.3) | 12 | 42.0 (22.4) | ||
| QCPR (participant) | ||||||
| •Warmth | ||||||
| Life review | 32.4 (1.0) | 32.3 (2.3) | 11 | 2.56, p = 0.13 | 33.5 (2.3) | 4.51, p = 0.046* |
| Gift | 32.2 (1.0) | 31.2 (1.7) | 12 | 31.6 (2.1) | ||
| •+Conflict | ||||||
| Life review | 23.5 (0.8) | 21.5 (2.1) | 11 | 0.43, p = 0.52 | 22.0 (2.1) | 1.40, p = 0.25 |
| Gift | 22.8 (1.7) | 22.3 (1.2) | 12 | 22.5 (3.6) | ||
| QCPR (relative) | ||||||
| •Warmth | ||||||
| Life review | 34.3 (3.9) | 35.2 (3.7) | 11 | 0.21, p = 0.65 | 37.5 (3.0) | 0.08, p = 0.78 |
| Gift | 34.8 (4.6) | 34.5 (4.6) | 12 | 37.9 (2.6) | ||
| •Conflict | ||||||
| Life review | 21.1 (4.7) | 22.3 (4.1) | 11 | 0.120, p = 0.73 | 26.8 (4.1) | 0.03, p = 0.87 |
| Gift | 23.3 (3.3) | 24.3 (5.2) | 12 | 27.9 (2.2) | ||
Where assumption was violated, the variables were transformed to repeat ANCOVA analysis. However, untransformed mean/SD reported.
Significant results.
Table 2 shows the means and SDs for the QOL-AD, GDS-12R and AMI-E at each of the three time-points. The results of the ANCOVAs at the end of the life review intervention and six weeks later are presented, in each case with the baseline score as covariate.
At the 12-week assessment, the primary outcome variable, QOL-AD showed a significant improvement in scores for the life review group, in comparison with the ‘gift’ group who were receiving usual care during this period [F(1, 20) = 5.11, p = 0.035].
In relation to secondary outcomes, no significant difference was apparent on the measure of depression, the GDS-12R. However, there was a significant intervention effect on the memory test used, the AMI-E. This was evident on total scores [F(1, 20) = 19.92, p < 0.001] and on the two sub-scales, the PSS and AIS, reflecting memory for facts and for events, respectively. In each case, the scores of the life review group increased, while those of the usual care ‘gift’ group declined.
Research question 2: the effect of life story books produced by a life review process compared with life story books presented as a gift (Table 2)
To address this question, ANCOVAs were carried out comparing the effect of intervention group at the assessment six weeks following the person having a life story book, with baseline scores entered as the covariate. There was now no difference between the groups on the primary outcome variable, QOL-AD. However, the longitudinal analysis indicated that there was a significant group × time interaction [F(1.54, 32.5) = 4.19, p = 0.033)]. During the six-week period following the usual care group participants receiving their life story book as a gift, their QOL mean scores increased by 3.1 points (p = 0.024) compared with a reduction of 0.8 points (p = 0.63) for those whose books had resulted from a life review process. The receipt of a life story book produced either through a life review process or by the participant's relative is associated with increased QOL among participants relative to the initial baseline assessment (p = 0.007).
Among the secondary outcome measures, there was no between-group difference evident on the GDS-12R depression scale six weeks after receipt of the life story books. On the AMI-E, the between-group difference at the six-week follow-up assessment was also not significant for total scores [F(1, 20) = 2.92, p = 0.10] or either sub-scale. However, the longitudinal analysis again showed a group × time interaction (for total score, [F(2, 42) = 8.36, p = 0.001]. In each case, the ‘gift’ group showed an improvement in score following the receipt of the book, whereas the life review group showed a small decrease. For total scores, the mean increase for the ‘gift’ group was 7.3 points (p = 0.047), compared with a reduction of 2.5 points for the life review group (p = 0.46).
Research question 3: the effect of life story books on quality of relationship as rated by participants and relatives (Table 2 and 3)
Table 3.
Quality of caregiving relationship (relative).
| Time period | ||||||||
|---|---|---|---|---|---|---|---|---|
| Measures | n | Time 1 (baseline)(Mean/SD) | Time 2 (post-life review)(Mean/SD) | Time 3 (6-weeks follow-up)(Mean/SD) | ANOVA |
Post hoc tests using the Bonferroni correction p value |
||
| (T1 vs. T2) | (T1 vs. T3) | (T2 vs. T3) | ||||||
| QCPR: total | 23 | 56.83 (5.49) | 58.17 (7.44) | 65.13 (5.40) | F(2, 39) = 19.37, p < 0.001 | p > 0.99 | p < 0.001 | p < 0.001 |
| QCPR: warmth | 23 | 34.57 (4.18) | 34.87 (4.07) | 37.74 (2.73) | F(2, 39) = 7.16, p = 0.003 | p > 0.99 | p = 0.013 | p = 0.003 |
| QCPR: conflict | 23 | 22.26 (4.11) | 23.30 (4.74) | 27.39 (3.23) | F(2, 35) = 16.21, p < 0.001 | p = 0.76 | p < 0.001 | p = 0.005 |
There was no between-group difference on the relationship scales, rated by the participant or the carer at the 12-week assessment. At the final assessment, contrary to the hypothesis, relationship warmth, rated by the person with dementia, was significantly improved for those who had completed a life review process [F(1, 20) = 4.51, p = 0.046]. No difference was apparent on the ratings of conflict in the relationship, or on the relative's ratings. Although there was no group × time interaction, the repeated measures analyses for the relatives’ ratings of the relationship (Table 3) indicated that there was a significant effect of time [F(2, 39) = 19.4, p < 0.001], with relationship scores improving significantly at the final follow-up assessment compared with the baseline and intermediate assessment.
Research question 4: the effect of life story books on care staff attitudes and knowledge (Table 4)
Table 4.
Care home staff attitudes and knowledge.
| Time period | ||||||||
|---|---|---|---|---|---|---|---|---|
| Measures | n | Time 1 (baseline)(Mean/SD) | Time 2 (post-intervention)(Mean/SD) | Time 3 (6-weeks follow-up)(Mean/SD) | ANOVA |
Post hoc tests using the Bonferroni correction p value |
||
| (T1 vs. T2) | (T1 vs. T3) | (T2 vs. T3) | ||||||
| ADQ: total | 46 | 73.54 (10.50) | 73.74 (9.23) | 80.07 (8.65) | F(2, 74) = 14.31, p < 0.001 | p > 0.99 | p < 0.001 | p < 0.001 |
| ADQ: hopefulness | 46 | 26.72 (5.16) | 27.00 (4.88) | 31.09 (5.55) | F(2, 84) = 19.38, p < 0.001 | p > 0.99 | p < 0.001 | p < 0.001 |
| ADQ: person-centred | 46 | 46.83 (6.82) | 46.74 (6.06) | 48.99 (4.65) | F(2, 74) = 3.92, p = 0.035 | p > 0.99 | p = 0.11 | p = 0.001 |
| Knowledge: correct | 68 | 5.93 (3.77) | 6.28 (4.14) | 8.79 (5.31) | F(2, 120) = 14.31, p < 0.001 | p > 0.99 | p < 0.001 | p < 0.001 |
| Knowledge: don't know* | 68 | 5.41 (3.68) | 4.12 (3.33) | 1.78 (2.25) | F(2, 115) = 31.65, p < 0.001 | p = 0.025 | p < 0.001 | p < 0.001 |
| Knowledge: incorrect* | 68 | 2.01 (2.37) | 1.54 (1.83) | 0.32 (0.68) | F(2, 119) = 24.88, p < 0.001 | p = 0.27 | p < 0.001 | p < 0.001 |
Lower scores indicate improvement.
A total of 68 staff directly involved as a carer for the resident with dementia took part. Of these, 65 (96%) at baseline, 58 (85%) at the intermediate assessment and 52 (76%) at the final assessment had completed the approaches to dementia questionnaire (ADQ). However, only 49 (72%) staff completed ADQ at all three point assessments. All 68 participants had completed the knowledge about resident with dementia questionnaires at each time-point.
A one-way repeated measures ANOVA with post hoc tests paired t-tests was conducted to compare scores on the ADQ scale and sub-scales and on the knowledge test across the three time-points (Table 4).
The ANOVA results indicated that the mean of each of the measures showed statistically significant differences between time-points (see Table 4). Post hoc paired t-tests (using the Bonferroni correction) showed that staff attitudes (ADQ total and sub-scales) towards the person with dementia did not change significantly before the life story book was completed (Time 1 vs. Time 2). However, after the life story book had been available for six weeks, staff attitudes had improved. Total scores and hopeful attitudes were significantly higher at the final follow-up compared with initial baseline scores (p < 0.001), and these scores as well as person-centred attitudes improved significantly between the intermediate assessment and the final follow-up (p ≤ 0.001). Staff knowledge (in terms of number of correct and incorrect answers) similarly did not show significant change until the final assessment, where scores were improved on both the baseline and intermediate assessments, although there were significantly less ‘don't know’ responses at the intermediate time-point (p = 0.025). It appears that both staff knowledge and staff attitudes show significant improvement in the period when the life story book is available.
Case-study vignettes
In this section, two participants’ experiences in taking part in the study are described, one of whom had developed a life story book through a life review process, with the other receiving it as a gift. All names used are pseudonyms.
Mary
Mary was an 80-year-old widow with moderate dementia living at the care home for the past 30 months. Initially, her sister, Jean, was reluctant to take part. However, she agreed after Mary had shown interest in the life story book idea and Jean provided pictures and other tangible documents to illustrate Mary's life history. Mary was very engaged in most of the life review sessions.
During the life review process, Mary expressed very rich information about her childhood. Once she recounted her childhood difficulties:
although I passed and qualified for the county school, I never got there because everything is too expensive … my father needed to look after my sister and brothers too … the County school needs special uniforms for different seasons … we couldn't afford that!
Mary started to work at a young age to support her family. When asked about her first job as reported by her sister Jean, Mary corrected the information:
I was a telephone operator with the post office for some years … many people don't know about that!
One sad part of Mary's life was her husband's death after a few years of their marriage. Sometimes during the life review session, she felt sadness about her husband's death. The life review process triggered many happy memories about her husband, greatly assisted by her wedding album, wedding invitation card and telegrams from relatives and friends which brought back many happy memories. Mary said:
We had a very happy life … he died too soon … I wish he lived longer … little longer!
Mary did not re-marry. She moved to live together with her parents and focused on her career.
I'm always happy with my job … very nice job! Sometimes I replaced other telephonists if they had other things to do.
At the final session, when the therapist asked about her overall life experiences and invited her to evaluate them, she replied:
When I look back at my life (long pause) … I have no regret … all looks fine … I'm happy … no need to change anything … only one thing … my husband … he died … what can I do? Can we do anything? Overall I'm happy with my life.
At the assessment following the completion of the life review, carried out by an independent assessor, Mary's scores on the QOL-AD and both sub-scales of the AMI had improved markedly. After Mary's completed life story book was left with her and another copy presented to her sister, Jean's reaction was:
She (Mary) told all this to you (referring to quotations from life review sessions). Hard for me to believe … I thought she can't remember all this. This is something great
Mary expressed great pleasure with her life story book and she said she would keep the book in a very safe place as the book is very important to her. Overall, in Mary's case, the book appeared to play a role as a maintenance tool after the completion of the life review process.
Nell
Nell was a 90-year-old widow living in the care home for two and a half years. Her CDR rating was indicative of mild dementia. She loved to read, and enjoyed solving puzzles and crosswords. Nell agreed to be part of the project saying that she had nothing to lose by taking part. Her son was supportive in providing Nell's life story and pictures. In addition, a number of pictures were gathered from online resources. Nell was randomised into the ‘gift’ group. Therefore, the researcher worked closely with her son and her daughter-in-law developing a life story book without any direct contact with Nell over a period of three months. However, her son did check the accuracy of some information, facts or/incidents with Nell without showing her the progressing drafted book. After the 12-week intervention period, one copy of the book was given to Nell as a gift, and one copy was provided for her son with another for the care home. The first reaction from Nell was:
I was very pleased with my book … all about me!
She was surprised with the gift and asked many questions, such as where the researcher had obtained her information and pictures. The researcher together with her son spent some time going through the book for the first time with her. Looking at each page, she read loudly, confirming the information in the book and also providing additional information that surprised her son. Her son and the home manager promised that they would spend time with Nell every time they had the chance.
In further feedback, Nell mentioned the book helped her to look back on her life.
Now, I can see my life again … lots of good memories … the book triggers and stimulates my memory … nice to have one (the book)
Nell's son also said that he really enjoyed all the process of developing the life story book for his mother as a gift. The process helped him to reminisce, especially regarding his memories of his mother.
I had a chance to revisit my life with my mother again … thank you so much!
He agreed that the book helped his mother in recalling many life events in her life. He further added:
The book helps me to spend quality time with my mother- … Now we engage in meaningful conversation. Every visit she would tell me new information from the book.
Discussion
This randomised controlled trial compared two different approaches to developing life story books with people with mild to moderate dementia living in care homes. The results are consistent with previous research (Morgan & Woods, 2010) in indicating that a life review process, resulting in a life story book, is associated with improved autobiographical memory, compared with usual care. Improvements were noted in both factual information and memory for events in the person's life. For the first time, improved QOL has also been shown in this context. On the other hand, in contrast to previous work (Haight et al., 2006; Morgan & Woods, 2010), improvements in mood were not identified. This may be related to a ‘floor’ effect, with mean scores of participants being below the clinical range.
However, when the ‘usual care’ group were themselves presented with a life story book, prepared by a relative as a ‘gift’, differences between the groups in autobiographical memory and QOL were no longer evident. The gift group's mean QOL and autobiographical memory improved significantly following receipt of the book, whereas the mean scores of participants who had undertaken a life review did not appear to change.
Our hypothesis that the close involvement of the relative in the ‘gift’ group in producing the life story book would lead to an improvement in relationship specifically for relatives and residents in this group was not supported. There was a clear improvement in the relationship, as rated by the relative, irrespective of group, in the period when the life story book was available. Although relatives were not directly involved in producing the book for those in the life review group, they actively sought out photographs and memorabilia, and so relatives in both groups may have experienced increased engagement. However, the improvement only appeared to begin when the book was available, perhaps related to its role in increasing communication and enhancing interaction (Woods, Keady, & Seddon, 2007).
Relationship ratings by the person with dementia showed less clear findings, being noted in the life review group in the period after the books were completed. This is paradoxical, in that this was the period when QOL was not showing improvement for this group.
This research also demonstrated improvements in staff attitudes and knowledge after the life story book was available. This is an important finding because our earlier systematic review on individual reminiscence work (Subramaniam & Woods, 2012) indicated that, despite their key role in caring for the person with dementia, the impact on staff was rarely evaluated. For example, some individual reminiscence work (e.g., Haight et al., 2006; Lai et al., 2004) involved staff directly in the intervention process but the effects on them were not reported. Therefore, for the first time, improved staff knowledge and attitudes has been shown in this context. The current finding parallels the improvements in staff knowledge after engagement with group reminiscence work with older adults with dementia reported by Baines et al. (1987).
The major limitation of the present study was the small sample size, which reduces the generalisability of the findings. There were also between-group differences at baseline on key variables, QOL-AD, AMI-E and GDS 12R. All possible measures were taken to avoid bias in randomisation, using a randomisation method determined, set up and controlled by an independent accredited clinical trials unit. All the participants were strictly selected according to the inclusion criteria and data were only entered for analysis after all the participants completed the trial. Despite these measures, the intervention group had lower scores on these measures at baseline assessment despite there being no demographic differences between the groups. Of course, these differences were controlled for statistically, using analysis of covariance, but interpretation of the results would clearly be more straightforward if the groups had been equivalent on key measures at baseline.
A further limit to generalisability was the use of a single therapist to provide all the interventions for both groups. The present study cannot indicate whether similar results would be obtained by different therapists. The current study also lacked an active control group. Improvements in the life review phase could be attributed to the social contact with and attention from the therapist.
Finally, the present study used multiple statistical tests in analysing the data, increasing the risk that some comparisons will reach statistical significance by chance. For example, the improvement in QCPR's warmth sub-scale at Time 3 for the life review group was at the threshold for significance, and could be a chance finding.
Further research is needed to replicate these findings with people with mild to moderate dementia, with larger sample sizes to overcome the limitations of the current trial. Multiple sites and therapists following a common protocol would be needed. A longer follow-up period would also be of interest. The present study has suggested that the outcome measures used here are sensitive to change in this context, but economic evaluation would be required alongside a future trial.
The success of the life story books provides further encouragement for the development of alternative formats, including the use of digital media (Subramaniam & Woods, 2010). Further studies could consider comparing multi-media digital life story books with the conventional paper life story book.
The findings from this study add weight to the continued development and use of life story books. As well as any benefits for people with dementia, they have been shown, in this study, to improve staff attitudes and knowledge, underpinning person-centred care, and improve relatives’ perception of their relationship with the person with dementia.
The structured life review process does appear to provide a clinical evidence-based therapeutic tool to promote psychosocial well-being with people with dementia living in residential settings. This research supports the benefits of this approach over ‘treatment as usual’ adding new empirical evidence to our existing knowledge of the usefulness of life review reminiscence work (Haight et al., 2006; Morgan & Woods, 2010). The developing life story book was found to be an essential component of the life review process with people with dementia, acting as a ‘bridge’ between sessions. The drafted life story book helped the participant to recall the previous session and continue to engage in progressing through the life review. In addition, the drafted life story book also appeared to help in building trust and a meaningful relationship with the therapist.
This study does not, however, indicate that life story books can only be developed through a life review process. Books prepared by relatives without the person's involvement were also associated with improved QOL and autobiographical memory over the study period. Relatives can be encouraged to develop such books, especially where the person with dementia is less able to participate actively in the process. The findings support the hypothesis set out by Morgan and Woods (2010) that the life story book is an intervention in its own right.
Generally, dementia is seen as an irreversible progressive condition. Therefore, psychosocial treatment may be seen as having very little benefit. However, in this research, despite the progressive nature of dementia, persons with dementia showed they still had the ability to recall past memories and to experience improvements in their perceived QOL. This provides an opportunity for care staff, activity officers and other professionals to use life review and life story book as a part of care activity to improve and maintain the QOL, cognitive function and mood of individuals with dementia as long as possible. The clear difference that staff saw in people with dementia participating in the study could well have contributed to the improvements in hopeful attitudes regarding dementia, recognising that it was possible to make a difference. The emphasis on individual's life stories and experiences appeared to help staff to get to know residents better, and offers the potential for more individualised, person-centred care which recognises the importance of the person's biography (Kitwood, 1997).
The life story books appeared to have a significant impact on the participating care homes. Care home staff and relatives suggested that each resident should move into the care home together with their own life story book. Even some of the senior management were surprised with the amount of new information they had gained from the life story books of the participating residents. Some of the care homes that took part in the present trial started to develop life story books for all their residents, integrating the life story book as part of the care programme.
Participants’ relatives also experienced having accomplished something worthwhile and meaningful for the person with dementia. For example, some relatives reported that the book enabled them to spend quality time with the resident and reduced repetitive questions. Some relatives also made extra copies of the life story book for other significant family members. Some relatives started to develop a life story book for another older adult in their family. This approach provides a means for the relative to find constructive engagement with the person with dementia and the care home, which may be helpful in reducing some of the negative aspects experienced by many relatives in this position (Woods et al., 2007). Encouragement to produce a book before the person enters a home would perhaps also be beneficial. The improvement in relationship noted in this study may reflect the life story book assisting the relative to re-establish contact and meaningful communication with the person with dementia. Relatives often describe a loss of relationship, and this approach may help redress this.
The life review process has the potential to evoke unpleasant memories as well as memories of happy times. In the present study, two broad categories of unpleasant or disturbing memories were observed. First, almost half of the participants shared sadness and grief over the loss of a loved one in their life, mainly the loss of a spouse or children. Second, a few participants shared memories of traumatic experiences including war experiences, physical violence, domestic violence and sexual harassment. This led to negative emotions during some life review sessions, including emotional upset, feelings of guilt, stress, sadness and anger. However, in every case, participants were able to cope and move forward in the life review process progress with continued support from the therapist. Participants chose, without exception, not to include any details of traumatic memories in their life story book, although many did comment on bereavements and losses in their books.
On the basis of this experience, we would suggest that working on a life review process should only be undertaken by a trained helper equipped with knowledge regarding the nature of dementia, Kitwood's person-centred approach, cognitive processes, the life review model and, most importantly, person-centred counselling skills (Rogers, 1980). The trained staff need supervision from a professional with expertise in the field as observed in Haight et al. (2006) and Morgan and Woods (2010) studies. Where such training, supervision and expertise are not available, the current research suggests that the life story book can be developed satisfactorily by relatives for the person with dementia, although we would suggest that they present a draft version over which the person with dementia may exercise editorial control, rather than present the person with the ‘finished article’ as was the case in this study.
Overall, the present research provides some empirical evidence on the effects of the life review process and the creation of life story books with or without involving the person with dementia. Specifically, it has demonstrated that the creation of a life story book by a relative without involving the person with dementia may produce psychosocial benefit for people with dementia living in care homes. The life story books, however created, were viewed positively by participants, relatives and care staff. The creation of a life story book appears to be a valuable therapeutic approach to aid a person living with dementia.
Acknowledgements
Ponnusamy Subramaniam's doctoral studies at Bangor University are supported by the Government of Malaysia, and he is affiliated with the Health Psychology Unit, Universiti Kebangsaan Malaysia. We are grateful to Rhiannon Williams and Kat Algar for acting as independent assessors for follow-up assessments.
Note
NVQ (National Vocational Qualification) reflects work-based learning and skills, in this context in providing direct care. Most direct care staff would be expected to have NVQ level 1 or 2, with staff in leadership roles having level 3 or 4. These staff would provide personal care and might administer medication, but nursing procedures such as dressings, changing catheters or injections would be undertaken by a registered nurse.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., test revision. Washington, DC: Author; 2000. [Google Scholar]
- Baines S., Saxby P., Ehlert K. Reality orientation and reminiscence therapy: A controlled cross-over study of elderly confused people. British Journal of Psychiatry. 1987;151:222–231. doi: 10.1192/bjp.151.2.222. [DOI] [PubMed] [Google Scholar]
- Dementia UK: Dementia UK life story template. Retrieved from www.dementia.uk.org.uk. [Google Scholar]
- Garland J., Garland C. Life review in health and social care. A practitioner's guide. Hove: Brunner-Routledge; 2001. [Google Scholar]
- Gibson F. What can reminiscence contribute to people with dementia? In: Bornat J., editor. Reminiscence reviewed: Evaluations, achievements, perspectives. Buckingham: Open University Press; 1994. pp. 46–60. [Google Scholar]
- Haight B.K. The therapeutic role of a structured life review process in homebound elderly subjects. Journals of Gerontology. 1988;43(2):40–44. doi: 10.1093/geronj/43.2.P40. [DOI] [PubMed] [Google Scholar]
- Haight B.K. The structured life review process: A community approach to the aging client. In: Jones G.M.M., Miesen B.M.L., editors. Caregiving in dementia: Research and applications. London: Routledge; 1992. pp. 272–292. [Google Scholar]
- Haight B.K., Bachman D.L., Hendrix S., Wagner M.T., Meeka A., Jolene J. Life review: Treating the dyadic family unit with dementia. Clinical Psychology and Psychotherapy. 2003;10:165–174. doi: 10.1002/cpp.367.. [DOI] [Google Scholar]
- Haight B.K., Gibson F., Michel Y. The Northern Ireland life review/life storybook project for people with dementia. Alzheimer's & Dementia. 2006;2(1):56–58. doi: 10.1016/j.jalz.2005.12.003.. [DOI] [PubMed] [Google Scholar]
- Hoe J., Hancock G., Livingston G., Orrell M. Quality of life of people with dementia in residential care homes. British Journal of Psychiatry. 2006;188:460–464. doi: 10.1192/bjp.bp.104.007658. [DOI] [PubMed] [Google Scholar]
- Hughes C.P., Berg L., Danziger W.L., Coben L.A., Martin R.L. A new clinical scale for the staging of dementia. British Journal of Psychiatry. 1982;140:566–572. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- Kitwood T. Dementia reconsidered: The person comes first. Buckingham: Open University Press; 1997. [Google Scholar]
- Kopelman D. Autobiographical memory in clinical research and practice. In: Conway M.A., Rubin D.C., Spinnler H., Wagenaar W.A., editors. Theoretical perspectives on autobiographical memory. Dordrecht: Kluwer; 1992. pp. 427–450. [Google Scholar]
- Kopelman M.D., Wilson B.A., Baddeley A. The Autobiographical memory interview. Suffolk: Thames Valley Test; 1990. [Google Scholar]
- Lai C.K.Y., Chi I., Kayser-Jones J. A randomized controlled trial of a specific reminiscence approach to promote the well-being of nursing home residents with dementia. International Psychogeriatrics. 2004;16(1):33–49. doi: 10.1017/S1041610204000055. [DOI] [PubMed] [Google Scholar]
- Life story network: Your story matters. Retrieved from www.lifestorynetwork.org.uk. [Google Scholar]
- Lintern T. Quality in dementia care: Evaluating staff attitudes and behaviour. Bangor, Wales: University of Bangor; 2001. (Unpublished doctoral dissertation) [Google Scholar]
- Lintern T., Woods B., Phair L. Before and after training: A case study of intervention. Journal of Dementia Care. 2000;8(1):15–17. [Google Scholar]
- Logsdon R.G., Gibbons L.E., McCurry S.M., Teri L. Assessing quality of life in older adults with cognitive impairment. Psychosomatic Medicine. 2002;64:510–519. doi: 10.1097/00006842-200205000-00016. Retrieved from http://www.psychosomaticmedicine.org/content/64/3/510. [DOI] [PubMed] [Google Scholar]
- Morgan S., Woods R.T. Life review with people with dementia in care homes: A preliminary randomized controlled trial. Non-Pharmacological Therapies in Dementia. 2010;1:43–60. [Google Scholar]
- Pallant T. SPSS survival manual: A step by step guide to data analysis using SPSS. 4th ed. Berkshire: McGraw-Hill; 2010. [Google Scholar]
- Rogers C.R. A Way of Being. Boston: Houghton Mifflin; 1980. [Google Scholar]
- Rush A.J., First M.B., Blacker D. Handbook of psychiatric measures. 2nd ed. Washington, DC: American Psychiatric Publishing; 2008. [Google Scholar]
- Schulz K.F., Altman D.G., Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Trial. 2010;11(32):1–8. doi: 10.1186/1745-6215-11-32.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh J.I., Yesavage J.A. Geriatric depression scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist. 1986;27:569–572. doi: 10.1300/J018v05n01_09. [DOI] [Google Scholar]
- Spruytte N., Van-Audenhove C., Lammertyn F., Storms G. The quality of the caregiving relationship in informal care for older adults with dementia and chronic psychiatric patients. Psychology & Psychotherapy: Theory, Research, and Practice. 2002;75:295–311. doi: 10.1348/147608302320365208. [DOI] [PubMed] [Google Scholar]
- Subramaniam P., Woods B. Towards the therapeutic use of information and communication technology in reminiscence work for people with dementia: A systematic review. International Journal of Computers in Healthcare. 2010;1(2):106–125. doi.org/10.1504/IJCIH.2010.037457. [Google Scholar]
- Subramaniam P., Woods B. The impact of individual reminiscence therapy for people with dementia: Systematic review. Expert Review of Neurotherapeutics. 2012;12(5):545–555. doi: 10.1586/ern.12.35. [DOI] [PubMed] [Google Scholar]
- Sutcliffe C., Cordingley L., Burns A., Mozley C.G., Bagley H., Huxley P., Challis D. A new version of the Geriatric Depression Scale for nursing and residential home populations: The Geriatric Depression Scale (Residential) (GDS-12R) International Psychogeriatrics. 2000;12(2):173–181. doi: 10.1017/S104161020000630X. [DOI] [PubMed] [Google Scholar]
- Tabourne C. The effects of life review program on disorientation, social interaction, and self-esteem of nursing home residents. The International Journal of Aging and Human Development. 1995;41(3):251–266. doi: 10.2190/EG53-878E-MGRK-BCPP. [DOI] [PubMed] [Google Scholar]
- Thorgrimsen L., Selwood A., Spector A.L., Royan L., Lopez M.M., Woods R.T., Orrell M. Whose quality of life is it anyway? The validity and reliability of the quality of life-Alzheimer's disease (QOL-AD) scale. Alzheimer Disease & Associated Disorders. 2003;17:201–208. doi: 10.1097/00002093-200310000-00002. [DOI] [PubMed] [Google Scholar]
- Vickers A.J., Altman D.G. Analysing controlled trials with baseline and follow up measurements. British Medical Journal. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. http://dx.doi.org/10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods R.T., Bruce E., Edwards R.T., Hounsome B., Keady J., Moniz-Cook E., Orrell M., Russell I.T. Reminiscence groups for people with dementia and their family carers: Pragmatic eight-centre randomised trial of joint reminiscence and maintenance versus usual treatment: A protocol. Trials. 2009;10:64. doi: 10.1186/1745-6215-10-64.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods B., Keady J., Seddon D. Involving families in care homes: A relationship-centred approach to dementia care. London: Jessica Kingsley; 2007. [Google Scholar]
- Woods B., Spector A.E., Jones C.A., Orrell M., Davies S.P. Reminiscence therapy for dementia. Cochrane Database of Systematic Reviews. 2005;2005(2):CD001120. doi: 10.1002/14651858.CD001120.pub2.. [DOI] [PubMed] [Google Scholar]
- Zimmerman S., Williams C.S., Reed P.S., Boustani M., Preisser J.S., Heck E., Sloane P.D. Attitudes, stress, and satisfaction of staff who care for residents with dementia. Gerontologist. 2005;45(1):96–105. doi: 10.1093/geront/45.suppl_1.96. [DOI] [PubMed] [Google Scholar]


