Abstract
Background
The ability to identify potentially resistant participants early in the course of an intervention could inform development of strategies for behavior change and improve program effectiveness.
Objective
The objective of this analysis was to identify factors related to nonresponse (i.e., lack of behavior change) to an asthma management intervention for urban teenagers. The intervention targeted several behaviors, including medication adherence, having a rescue inhaler nearby, and smoking.
Methods
A discriminate analysis was conducted using data from a randomized trial of the intervention. Included in this analysis are participants who reported a physician diagnosis of asthma, completed a baseline questionnaire, were randomized to the treatment group, completed ≥2 of 4 educational sessions, and completed ≥2 of 3 follow-up questionnaires. Ninety students met criteria for inclusion in this subgroup analysis.
Results
In logistic regression models for medication adherence, nonresponse was related to low baseline asthma self-regulation, odds ratio = 3.6 (95% confidence interval = 1.3–9.5). In models for having an inhaler nearby, nonresponse was related to low baseline self-regulation and to rebelliousness, OR = 4.7 (1.6–13.2) and 5.6 (1.7–18.0), respectively. Nonresponse to smoking messages was related to rebelliousness, low emotional support, and low religiosity, ORs = 7.6 (1.8–32.3), 9.5 (1.4–63.5), and 6.6 (1.5–29.8) respectively.
Conclusions
Certain variables had the ability to discriminate the likelihood of response from that of nonresponse to an asthma program for urban, African American adolescents with asthma. These variables can be used to identify resistant subgroups early in the intervention, allowing the application of specialized strategies through tailoring. These types of analyses can inform behavioral interventions.
Keywords: Adolescent, African American, Asthma, behavior, nonresponse, tailoring
Background
Asthma control requires a combination of clinical management and patient self-regulation (1). Empowering patients to change negative behaviors that increase the likelihood of symptom flare-ups is challenging (2). Successful behavioral interventions have been designed to modify behavior through the application of theory-based methods based on the patient’s readiness to change and the patient’s cognitive processing in considering a change (3). These concepts correspond to the underlying principals of tailored interventions; that is, each patient is different.
Tailoring is defined as “any combination of information or change strategies intended to reach one specific person, based on characteristics that are unique to that person, related to the outcome of interest, and have been derived from an individual assessment” (4). Tailoring allows the personalization of health information to address relevant cultural, social, environmental, and psychological factors (5–10). Web-based disease management tools provide a means of delivering high-fidelity, tailored interventions that are easily disseminated to large groups of both clinic- and non–clinic-based populations. Because the collection of user-specific information is inherent to Web-based, tailored interventions, this approach allows the identification of participants with certain characteristics and the exclusive delivery of certain messages to that targeted subgroup.
According to the developers of the Transtheoretical Model, in any given population there is a subgroup of individuals who are more resistant to health interventions compared to the majority of participants (11). Early publications suggest that about 40% of persons with risk behaviors in a given population will be precontemplators with a low readiness to change, but researchers have used cluster analysis to identify distinct subgroups within low readiness stages that are particularly resistant or disengaged (12). More intensive interventions are needed to help these individuals overcome cognitive and situational barriers to behavior change (13).
Puff City is a computer-tailored program designed to help urban, African American adolescents gain better control of their asthma. The program uses tailored messages to motivate students to make positive changes in behaviors related to asthma management and control (14). Puff City was compared to existing Web-based, generic asthma education in a randomized trial conducted in six Detroit high schools. Results of the trial have been previously reported (14). Compared to the control group, students receiving the tailored program had lower asthma-related morbidity (symptom-days, symptom-nights, asthma hospitalizations, etc.) and more positive behavior changes.
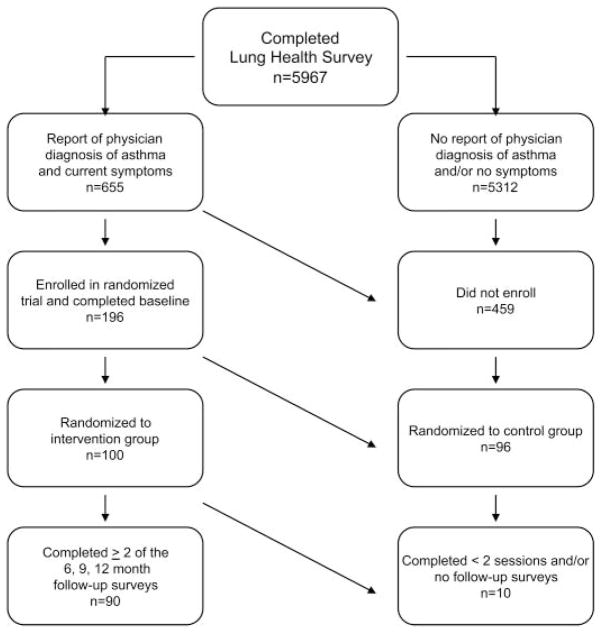
Despite the results of the randomized trial, many students who participated in the program did not change behavior. We hypothesized that program effectiveness could be improved by identifying student baseline characteristics that were significantly associated with lack of positive behavior change (Step 1 of link Figure 1), and using these characteristics as the basis for creation of submodules through which additional, theory-based strategies could be administered (Step 3 of Figure 1). As shown in Step 1 of Figure 1, the goal of this paper is to describe the analysis conducted using baseline data from the randomized trial of Puff City to identify baseline characteristics associated with student lack of behavior change (referred to as nonresponse) by 12-month follow-up. Questions included in our baseline questionnaire were based on (1) our own hypotheses about teen behavior, (2) a review of the literature, and (3) recommendations by our medical advisors. For this analysis, we included all demographic, contextual, behavioral, and attitudinal variables included on the baseline questionnaire.
Figure 1.
Steps to increasing effectiveness of a web-based asthma management program for urban teenagers. Step 1 is the focus of this paper.
With these results, a second iteration of Puff City will identify resistant students at baseline and direct them to a submodule for deeper tailoring before returning them to the original flow of the program.
Methods
Development of the Puff City program is described in a previous publication (13). Briefly, program content for Puff City was based on the recommendations for patient education published in the National Asthma Education and Prevention Program’s Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report II (EPRII), and includes concepts from other nationally accredited sources (15, 16).
Program Content
The Web-based program focuses on three core behaviors, namely controller medication adherence, rescue inhaler availability, and smoking cessation/reduction. To motivate behavior change in Puff City, tailoring is used to apply the concepts of the Transtheoretical Model and the Health Belief Model (17, 18). Health messages and information on asthma control are presented in reference to the core behaviors, allowing the delivery of information both central and peripheral to the behavior. Examples of the latter include information on basic asthma pathophysiology and trigger avoidance. The program consists of four consecutive educational computer sessions that make use of both normative (“compared to other students”) and ipsative feedback (“compared to your last session”). Messages are voiced-over to accommodate low literacy.
Randomized Trial
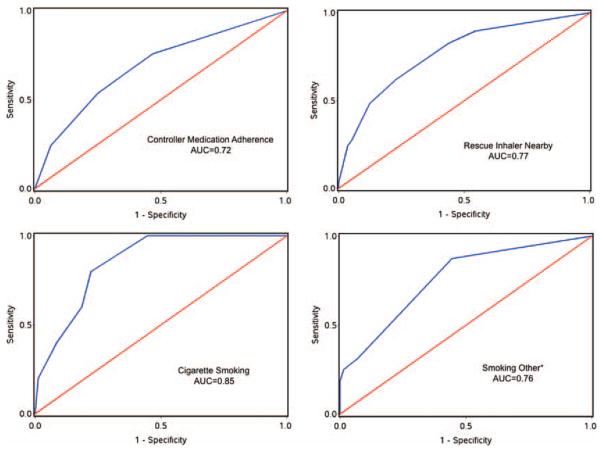
All aspects of the randomized trial were approved by the Institutional Review Boards of Henry Ford Health System (HFHS), the University of Michigan (UM), and the Detroit Public School Office of Research, Evaluation, and Assessment. To identify students with asthma symptoms, a Lung Health Survey was administered during an English class at participating schools. Students were eligible for the randomized trial if they met study criteria for current asthma, defined as report of ever having a physician diagnosis of asthma accompanied by one or more of the following: daytime and/or nighttime symptoms in the past 30 days, use of medication for asthma symptoms in the past 30 days, medical care use for asthma in the past year, and ≥1 refill(s) of β-agonists in the past year (15, 19, 20). Students were also eligible if they did not report a physician diagnosis, but answered positively to items selected from the International Study of Asthma and Allergies in Childhood (19) and reported symptom frequencies similar to those used in the EPRII (15) (EPRIII was not yet published) for classification of mild, intermittent asthma (Figure 2). Eligible students were invited to enroll in the randomized trial, which required written parental consent and student assent (14). Details of eligibility determination and enrollment appear in earlier publications (14, 21).
Figure 2.
Sample used for analysis of characteristics associated with non-response to a computer-tailored asthma intervention for urban teens.
Students accessed the program using computers at participating schools. Students identified current asthma medications using a computer module that contained names and illustrations of asthma medications. After completing a baseline questionnaire online, students were randomized to receive the tailored or generic program.
Core behavior status was determined at session 1 and reassessed during sessions 2 to 4. In each tailored session, students were asked to identify their personal barriers to behavior change from a list developed using the asthma literature and corroborated through focus groups with urban, African American teenagers. Students were asked to complete follow-up questionnaires at 6, 9, and 12 months post baseline, regardless of the number of sessions completed.
Statistical Analysis
Included in this analysis are participants who (1) reported a physician diagnosis of asthma; (2) completed a baseline and were randomized to the treatment arm of the study (i.e., received the computer-tailored intervention); (3) completed at least two of the four educational sessions; and (4) completed at least two of three follow-up questionnaires. Controller medication adherence was defined as self-report of taking controller medication ≥5 days in the last 7 days. Availability of a rescue inhaler was defined as self-report of carrying a rescue inhaler ≥5 days of the last 7 days. Smoking was defined as self-report of smoking at least two cigarettes or cigars on the days smoked in the last 30 days (22). We also looked for potential associations between nonresponse and report of smoking cannabis in the past 30 days.
Definition of Response and Nonresponse
Positive change at any time during the follow-up period was considered response. Nonresponse was evaluated separately for each behavior and was defined as lack of change in negative behavior by last follow-up completed. Acquiring a previously unreported asthma medication during the intervention period was considered response, whereas lack of an asthma medication that was reported earlier was considered nonresponse.
Questions for religiosity, perceived emotional support (defined as a sense of feeling loved and valued) (23), and rebellion scales are presented in Table 1. The overall score for perceived emotional support was determined by calculating the average of three scales (special person, friends, and family). Also included was the Asthma Self-Regulation Interview (ASRI) developed by Zimmerman and Bonner in 1998, which theorizes that self-regulation of asthma follows a sequential path and is influenced by fundamental beliefs about the condition, perceptions of vulnerability, and the perceived ability to manage the condition (24). The ASRI categorizes patients into one of four phases with the lower phases representing less self-regulation. These and other variables collected at baseline are shown in Table 2. All variables are self-reported.
Table 1.
Measures for religiosity, rebellion, and perceived emotional support (teen).a
| Religiosity Rebellion26 | When under stress, I tend to pray, meditate, or work on my spiritual life.
|
| Perceived emotional support (teen)23 |
The following questions ask about friends, family, and significant others in your environment that may provide you with emotional support. Emotional support is your perception of feeling loved, valued, and special to others. Respond to the following questions by thinking about how caring you feel others are as you experience the challenges of living with asthma.
Now thinking about your family…
Now thinking about your friends…
|
Response categories: 1 = Strongly agree; 2 = agree; 3 = neutral; 4 = disagree; 5 = strongly disagree.
Table 2.
Summary statistics and source of variables used in analysis.
| Range
|
Data source
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | N | Mean | SD | Min | Max | Student baseline or session 1 | Caregiver baseline | ||
| Continuous and/or scaled | |||||||||
| SESa | 88 | 11904 | 2321 | 7333 | 15593 | x | |||
| Religiosityb (scale of 1–5) | 88 | 3.2 | 1.2 | 1 | 5 | x | |||
| Depression (teen)c (scale of 0–7) | 90 | 2.9 | 2.0 | 0 | 7 | x | |||
| Depression (caregiver)d (scale of 0–24) | 68 | 5.1 | 6.5 | 0 | 24 | x | |||
| Perceived emotional support (teen)e (scale of 1–5) | 89 | 3.9 | 0.7 | 2.25 | 5 | x | |||
| Perceived social support (caregiver)f (scale of 1–5) | 67 | 4.2 | 0.9 | 1.8 | 5 | x | |||
| Rebelliousnessg (scale of 1–5) | 88 | 2.2 | 0.7 | 1 | 4.7 | x | |||
| ASRIh (scale of 1–4 corresponding to 4 phases) | 87 | 2.4 | 1.1 | 1 | 4 | x | |||
| N | Yes
|
No
|
|||||||
| n | (%) | n | (%) | ||||||
|
| |||||||||
| Dichotomous, composite, and/or single-item | |||||||||
| Exposed to ETSi | 90 | 55 | (61.1) | 35 | (38.9) | x | |||
| Moderate persistent or severe persistent asthmaj | 89 | 29 | (32.6) | 60 | (67.4) | x | |||
| Caregiver has high school diploma | 67 | 27 | (40.3) | 40 | (59.7) | x | |||
| Teen’s BMI >85th percentilek | 90 | 14 | (15.6) | 76 | (84.4) | x | |||
| Teen reports smoking in last 30 days | 89 | 4 | (4.5) | 85 | (95.5) | x | |||
| Teen reports continuity of carel | 85 | 33 | (38.8) | 52 | (61.2) | x | |||
| Reports gap in health care coverage in last year | 90 | 13 | (14.4) | 77 | (85.6) | x | |||
Socioeconomic status (median household income per person).
“When under stress, I tend to pray, meditate or work on my spiritual life.”
Lucas et al., 2001 (45);
Kroenke et al., 2001 (46);
La Greca et al., 2002 (47);
Bartlett et al., 2004 (48);
Tyc et al., 2005 (26);
Zimmerman et al., 1999 (24).
Environmental tobacco smoke.
Based on symptom frequency and EPRII (15).
Body mass index calculated using student report of height and weight.
A positive response to either of the following: “Some people hardly ever see the same doc when they get medical care for their asthma symptoms. Is this true for you?” or “For some people the breathing problems they have had in the past are ignored when they see a new doctor. Is this true for you?” McCusker, 1984 (49).
Logistic regression was used to calculate odds ratios (ORs) and corresponding 95% confidence intervals to describe the relationship of selected variables to nonresponse. Discriminant analysis was used to determine the optimal ability (cut-point) of each variable to differentiate responders (positive behavior change) from nonresponders (lack of positive change), maximizing the sum of sensitivity and specificity. Variables included in the model as potential predictors of nonresponse were those with the highest univariate discriminant ability and p values <.10. Subsequently, variables were excluded from the final multivariable model if adjusted p value >.10 and/or >30% of values were missing. Receiver operating characteristic (ROC) curves were plotted based on the final logistic regression models for each targeted behavior. Area under the curve (AUC) was calculated using Proc Logistic in SAS.
Results
Six Detroit high schools participated in the randomized trial. Over 98% of students in the participating schools were African American, and an average of 52% of students across the six schools qualified for federal school lunch programs (Institute of Education Sciences, accessed July 2006). A total of 5967 students (80% of the 9th to 11th grade students) completed a case-identification form (Figure 2), of which 655 reported a physician diagnosis of asthma and current asthma symptoms, making them eligible for participation in the randomized trial. A total of 196 students (30% or 196/655) provided assent and consent and completed a baseline, of which 100 (51% or 100/196) were randomized to the treatment group (Figure 2). Details and discussion of enrollment appear in a previous publication (14). Of those randomized to the treatment group, n = 90 met criteria for inclusion in this analysis. Of these, 88 (97%) had 12 month follow-up. These 90 students did not statistically differ from those not included with respect to demographics (age, gender, socioeconomic status [SES]), caregiver education, physician diagnosis, or any of the characteristics in this analysis with the exception of Medicaid enrollment. There was a higher percentage of Medicaid enrollees in the group that was not included in the analysis (45.6% versus 80.0% for included and not included, respectively) with a p value of .05 (data not shown).
Controller Medication Adherence
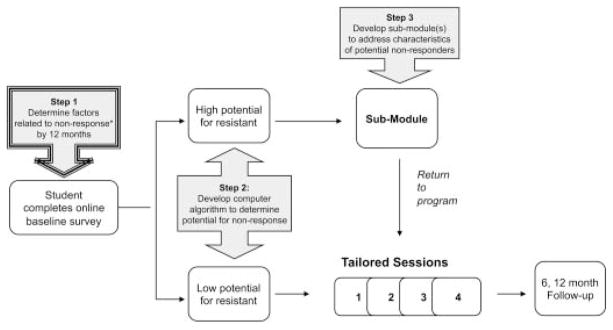
Factors related to nonresponse for each targeted behavior are presented in Table 3. A total of 55/90 students (61.1%) did not respond to intervention messages about adhering to the instructions of the prescribing physician. ASRI Phase 1 or 2 was significantly related to nonresponse with respect to controller medication adherence (Table 3). The OR describing the association between scoring >2.5 on the rebellion scale and nonresponse was also elevated (OR = 2.3), but the p value was .09. Among the nonrespondents, the top three most frequently selected barriers or difficult situations for adherence to controller medication included “when my asthma is not bothering me,” “when I feel I have control over my asthma,” and “when I do not feel sick.” The ROC Curve and AUC for medication adherence is shown in Figure 3. Area under the curve (AUC) for controller medication adherence was .77.
Table 3.
Results of stepwise logistic regression to identify variables associated with nonresponse.
| Variable | Adjusted ORa | 95% CIb | p |
|---|---|---|---|
| Controller Medication Adherence, n = 55 nonresponse/90 at risk | |||
| ASRI Phase 1 or 2c | 3.6 | 1.3–9.5 | .01 |
| Rebellion score >2.5d | 2.3 | 0.9–6.1 | .09 |
| Rescue Inhaler Nearby, n = 31 nonresponse/90 at risk | |||
| ASRI Phase 1 or 2 | 4.7 | 1.6–13.2 | <.01 |
| Rebellion score >2.5 | 5.6 | 1.7–18.0 | <.01 |
| Low perceived emotional supporte | 2.8 | 0.9–8.7 | .08 |
| Cigarette Smoking, n = 6 nonresponse/90 at risk | |||
| Rebellion score >2.5 | 7.8 | 0.7–87.9 | .09 |
| Low religiosityf | 7.5 | 0.9–60.5 | .06 |
| Low perceived emotional support | 5.7 | 0.7–45.7 | .10 |
| Smoking Other (includes cannabis, cigars), n = 17 nonresponse/90 at risk | |||
| Rebellion score >2.5 | 7.6 | 1.8–32.3 | <.01 |
| Low religiosity | 9.5 | 1.4–63.5 | .02 |
| Low perceived emotional support | 6.6 | 1.5–29.8 | .01 |
Adjusted odds ratio.
95% confidence interval.
Precompliant (Phase 1 or 2) on Asthma Self-Regulation Instrument (24).
>2.5 for responses to rebellion questions where 1 = strongly disagree (less rebellious) and 5 = strongly agree (more rebellious).
<3.6 on average of three scales for emotional support, where 1 = strongly disagree (less support) and 5 = strongly agree (more support).
Responded disagree or strongly disagree to question regarding religion.
Figure 3.
Receiver Operating Characteristic Curves (ROC) and Area Under the Curve (AUC) for variables associated with non-response in a computer-tailored asthma management program for urban teenagers. *Includes cannibis and cigars.
Having a Rescue Inhaler Nearby
A total of 31/90 students (34.4%) did not respond to tailored messages about having a rescue inhaler nearby. Predictors of nonresponse included ASRI Phase 1 or 2 and rebellion score >2.5 (Table 3). We observed an OR = 2.8 for the association between a lower score on the perceived emotional support scale (<3.6 on a scale of 1–5 with 5 being highest), and nonresponse, however; the p value was .08. The top three reasons selected for not having a rescue inhaler nearby included “when I feel like my asthma is under control,” “when I know I am not going to have an asthma attack,” and “when I have no where to carry my inhaler.” AUC for nonresponse to having a rescue inhaler nearby was .72 (Figure 3).
Smoking
Of the 90 students in the analysis, 17 (18.9%) did not respond to the smoking messages in the intervention. In this population, a report of cigarette smoking was significantly associated with a report of cannabis/cigar smoking, OR = 8.5 (1.4–50.5), p = .02, at baseline and 12.7 (2.1–78.0), p < .01, at 12-month follow-up (data not shown). Factors associated with smoking nonresponse were rebellion score >2.5, religiosity <3, and low perceived emotional support (Table 3). These associations were near significance when considering cigarette smoking only, but all became significant when cigarette and cannabis/cigar smokers were considered together. The top three barriers or situations in which the student found smoking behavior difficult to change included “when stressed out,” “when angry or upset,” and “when hanging out with people who are smoking.” AUC for smoking nonresponse was .85 for smoking cigarettes, and .76 for smoking that included cannabis and cigars (Figure 3).
Because rebelliousness can be a common characteristic of teenagers, we examined the distribution of scores on the rebelliousness scale. Of the 21 students scoring >2.5 on the scale, 47.9% (10/21) scored >3.0, and 5% (1/21) scored >4.0. Also, because our analysis sample differed from those not included in the analysis by percentage enrolled in Medicaid, we examined the relationship between Medicaid enrollment and the variables included in this analysis. Medicaid enrollment was not significantly associated with the variables in Table 2 (all p values >.10; data not shown).
Discussion
We used data from the baseline questionnaire of a randomized trial to identify variables associated with nonresponse to an asthma management program that targets urban, African American teenagers with asthma. Very little has appeared in the published literature on factors related to asthma management in this population. We found several contextual and attitudinal variables related to nonresponse across the three core behaviors related to asthma management.
Lower ASRI and higher rebelliousness scores were related to nonresponse for controller medication adherence. According to the developers of the ASRI, families of asthma patients in Phase 1 are characterized as being in denial and lacking acceptance of asthma as a chronic disease (24). This concept supports our results. In terms of rebelliousness, avoiding or refusing to take medication as instructed is a means of resisting control or authority (25–27).
The scale used to assess rebelliousness in the baseline questionnaire identifies students with a tendency toward rebelliousness as well as those that may have more severe conduct disorders (27). About 5% of students scored >4.0 on the rebellion scale of 5. For these students, referrals for family counseling may be necessary in order for behavior change to occur (26, 27).
Adolescents are prone to ignoring signs of an oncoming asthma attack (28, 29). In one study, almost 50% of adolescents (aged 13 to 14 years) neither took medication nor called a physician when they experienced mild or moderate asthma symptoms (28). Compared to responders, students resistant to messages about having an inhaler nearby scored higher on rebellion, lower on asthma self-regulation, and perceived less emotional support. Students resistant to messages about always having a rescue inhaler nearby not only had relatively higher scores for rebelliousness and scores indicating low asthma-self-regulation, but also had scores indicating low perceived emotional support (30, 31). “Lack of a place to carry an inhaler” was listed as one of the top three barriers to changing this behavior, and may imply the absence of someone to assist the student in brainstorming about practical ways of making sure an inhaler is nearby (locker, gym bag, etc.). Helping these students find encouragement and support for management of asthma could result in better outcomes.
Several U.S. and non-U.S. studies have shown rebellion to be associated with smoking behavior (32–34). Our results suggest that smoking among students with asthma can be a form of rebellion, but is also used as a coping mechanism, and can be a behavior adopted by students who have a desire to fit in. Barriers to smoking cessation selected by nonresponders included factors that could be associated with low emotional support (stressed), with rebellion (angry or upset), and with an attempt to obtain acceptance or support from peers (when hanging out with friends who are smoking).
Smoking was also associated with low religiosity. Religiosity in adolescents has been shown to be protective against risk behaviors, including smoking, alcohol use, and truancy, even after controlling for socioeconomic status, family background, and self-esteem (35). A positive response to our question on religiosity could also indicate a higher level of social support (e.g., having a “church family”), which further supports the low perceived emotional support reported by students who were nonresponsive to the smoking messages (36, 37). Our assessment of “religiosity” does not constitute a complete assessment of spirituality, which would include several domains, such as church attendance, youth group attendance, importance of religion in daily life, and frequency of prayer (36, 37).
The AUCs corresponding to our ROC curves indicate a fair-to-good accuracy of these factors in the ability to distinguish nonrespondents from respondents (38). We acknowledge that other theory-based measures of motivation and self-efficacy not included in our analysis may have better discriminate ability. Although cigarette smoking and the smoking of other substances were significantly related at baseline, the AUC for cigarette smoking was better than that of smoking cigars/cannabis, perhaps because of the larger sample size or because of differing intentions associated with the use of various substances.
A small sample size and reliance on self-report data are limitations of this analysis. Another limitation is that we did not include relapse as an outcome in this analysis. According to Marlatt and other experts in this area, relapse is best treated as a separate outcome with its own determinants (e.g., failure to respond to relapse warning cues) (39). The sample used in this subgroup analysis also had fewer Medicaid enrollees than those who were excluded. As Medicaid enrollment was not associated with the variables used in this analysis, it is unclear how this may have impacted our results. Finally, our analysis focuses on a group of urban, African American adolescents with self-report of a physician diagnosis of asthma and may not be applicable to other age groups or populations. Because our analysis is restricted to students who completed at least two educational sessions on the computer and at least two follow-up questionnaires, results are not applicable to nonparticipants, and variables related to study retention may be different from those related to lack of behavior change. Moreover, variables related to behavioral change may be different among those retained in the study compared to those who did not complete the intervention and follow up.
Our results underscore the very real challenge to helping urban, African American adolescents with asthma. Some of the apparent underlying reasons for nonresponse could be addressed through Motivational Interviewing. For example, Motivational Interviewing (25) could be used to create dissonance between student self-proclaimed values or goals and current behavior. In Motivational Interviewing, counselors roll with resistance rather than confront or counterargue. In this way they help the client resolve their ambivalence without direct persuasion. Another example is to apply principles of Self Determination Theory, which distinguishes autonomous (“I want to control my asthma so that I can miss less school”) from controlled motivation (“My doctor says I need to take my medicine”) on a continuum of self-regulation (40). For individuals with high autonomy needs, interventions should focus on autonomy supportive messages and minimize messages that could be perceived as coercive or controlling. For controller medication adherence, behavior change strategies for students will also involve convincing participants of the chronic nature of asthma.
Results of analyses for having an inhaler nearby and smoking suggest the potential benefit of strategies that encourage coping, organization, and family support. For example, messages to smoking students already addressing personal risk could be supplemented by providing assistance in coping and exploring ways to reduce stressors (41, 43). Strategies for improving self-efficacy and enhancing coping skills are suggested by Marlatt and the Attribution Theory, and include breaking down the overall task of behavior change into smaller subtasks, or using positive self-talk (50). The Transactional Theory of Coping includes both problem management (directed at changing the situation causing stress) as well as emotional regulation (changing the way one feels about a stressor) (42, 43). Specifically for lack of change in having an inhaler nearby, some students also need assistance in finding encouragement and support for management of asthma.
Innovative means of reaching adolescents with chronic disease are necessary. We could not find other studies reporting on factors related to nonresponse, or lack of behavior change, in urban teenagers with asthma. This analysis will be used to develop additional strategies for encouraging behavior change in students meeting criteria for being particularly resistant.
Acknowledgments
This work was funded by NHLBI grant number HL068971.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.McGhan SL, Cicutto LC, Befus AD. Advances in development and evaluation of asthma education programs [review] Curr Opin Pulm Med. 2005;11:61–68. doi: 10.1097/01.mcp.0000146783.18716.31. [DOI] [PubMed] [Google Scholar]
- 2.Howland J, Bauchner H, Adair R. The impact of pediatric asthma education on morbidity. Assessing the evidence Chest. 1988;94:964–969. doi: 10.1378/chest.94.5.964. [DOI] [PubMed] [Google Scholar]
- 3.Cote J, Cartier A, Robichaud P, Boutin H, Malo JL, Rouleau M, et al. Influence of asthma education on asthma severity, quality of life and environmental control. Can Respir J. 2000;7:395–400. doi: 10.1155/2000/787980. [DOI] [PubMed] [Google Scholar]
- 4.Kreuter MW, Skinner CS. Tailoring: what’s in a name? Health Educ Res. 2000;15:1–4. doi: 10.1093/her/15.1.1. [DOI] [PubMed] [Google Scholar]
- 5.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 6.Resnicow K, Braithwaite RL. Cultural sensitivity in public health. In: Braithwaite RL, Taylor S, editors. Health Issues in the Black Community. 2. San Francisco, CA: Jossey-Bass; 2001. pp. 516–542. [Google Scholar]
- 7.Lancaster T, Stead L, Shepperd S. Helping parents to stop smoking: which interventions are effective? Paediatr Respir Rev. 2001;2:222–226. doi: 10.1053/prrv.2001.0144. [DOI] [PubMed] [Google Scholar]
- 8.Redding CA, Prochaska JO, Pallonen UE, Rossi JS, Velicer WF, Rossi SR, et al. Transtheorectical individualized multimedia expert systems targeting adolescents’ health behaviors. Cogn Behav Pract. 1999;6:144–153. [Google Scholar]
- 9.Orleans CT, Boyd NR, Bingler R, Sutton C, Fairclough D, Heller D, et al. A self-help intervention for African American smokers: tailoring cancer information service counseling for a special population. Prevent Med. 1998;27:S61–S70. doi: 10.1006/pmed.1998.0400. [DOI] [PubMed] [Google Scholar]
- 10.Skinner CS, Strecher VJ, Hospers H. Physicians’ recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–49. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Velicer W, Prochaska J, Fava J, Norman GJ, Redding C. Smoking cessation and stress management: applications of the Transtheoretical Model of behavior change. Homeostasis. 1998;38:216–233. [Google Scholar]
- 12.Dijkstra A, De VH. Clusters of precontemplating smokers defined by the perception of the pros, cons, and self-efficacy. Addict Behav. 2000;25:373–385. doi: 10.1016/s0306-4603(99)00073-8. [DOI] [PubMed] [Google Scholar]
- 13.Stotts AL, DiClemente CC, Dolan-Mullen P. One-to-one: a motivational intervention for resistant pregnant smokers. Addict Behav. 2002;27:275–292. doi: 10.1016/s0306-4603(01)00174-5. [DOI] [PubMed] [Google Scholar]
- 14.Joseph CL, Peterson E, Havstad S, Johnson CC, Hoerauf S, Stringer S, et al. A Web-based, tailored asthma management program for urban African-American high school students. Am J Respir Crit Care Med. 2007;175:888–895. doi: 10.1164/rccm.200608-1244OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Asthma Education and Prevention Program. Guidelines for the diagnosis and management of asthma. Expert Panel Report 2. Bethesda, MD: United States Department of Health and Human Services National Institutes of Health National Heart, Lung and Blood Institute; Apr, 1997. NIH publication no. 97-4051. [Google Scholar]
- 16.Croft DR, Peterson MW. An evaluation of the quality and contents of asthma education on the World Wide Web. Chest. 2002;121:1301–1307. doi: 10.1378/chest.121.4.1301. [DOI] [PubMed] [Google Scholar]
- 17.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 18.Rosenstock I. Historical Origins of the Health Belief Model. Health Educ Monogr. 1974;2:328–335. [Google Scholar]
- 19.Weiland SK, Bjorksten B, Brunekreef B, Cookson WO, von Mutius E, Strachan DP. Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): rationale and methods. Eur Respir J. 2004;24:406–412. doi: 10.1183/09031936.04.00090303. [DOI] [PubMed] [Google Scholar]
- 20.Council of State and Territorial Epidemiologists. Surveillance Asthma Prevalence Definition. 1998 http://www.cste.org/ps/1998/1998-eh-cd-01.htm.
- 21.Joseph CL, Baptist AP, Stringer S, Havstad S, Ownby DR, Johnson CC, Williams LK, Peterson EL. Identifying students with self-report of asthma and respiratory symptoms in an urban, high school setting. J Urban Health. 2007;84:60–69. doi: 10.1007/s11524-006-9121-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grunbaum JA, Kann L, Kinchen S, Ross J, Hawkins J, Lowry R, Harris WA, McManus T, Chyen D, Collins J. Youth risk behavior surveillance—United States, 2003 [erratum appears in MMWR Surveill Summ 2004; 53:536] MMWR Surv Summ. 2004;53:1–96. [PubMed] [Google Scholar]
- 23.Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a confirmation study. J Clin Psychol. 1991;47:756–761. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerman BJ, Bonner S, Evans D, Mellins RB. Self-regulating childhood asthma: a developmental model of family change. Health Educ Behav. 1999;26:55–71. doi: 10.1177/109019819902600106. [DOI] [PubMed] [Google Scholar]
- 25.Resnicow K, Baskin M, Rahotep S, Periasamy S, Rollnick S. Motivational interviewing in health promotion and behavioral medicine. In: Cox W, Klinger E, editors. Handbook of Motivational Counseling. NewYork: John Wiley & Sons; 2004. pp. 457–476. [Google Scholar]
- 26.Tyc VL, Lensing S, Klosky J, Rai SN, Robinson L. A comparison of tobacco-related risk factors between adolescents with and without cancer. J Pediatr Psychol. 2005;30:359–370. doi: 10.1093/jpepsy/jsi030. [DOI] [PubMed] [Google Scholar]
- 27.Chapman KR, Walker L, Cluley S, Fabbri L. Improving patient compliance with asthma therapy. Respir Med. 2000;94:2–9. doi: 10.1053/rmed.1999.0667. [DOI] [PubMed] [Google Scholar]
- 28.Rich M, Lamola S, Gordon J, Chalfen R. Video intervention/prevention assessment: a patient-centered methodology for understanding the adolescent illness experience. J Adolesc Health. 2000;27:155–165. doi: 10.1016/s1054-139x(00)00114-2. [DOI] [PubMed] [Google Scholar]
- 29.Raherison C, Tunon-de-Lara JM, Vernejoux JM, Taytard A. Practical evaluation of asthma exacerbation self-management in children and adolescents. Respir Med. 2000;94:1047–1052. doi: 10.1053/rmed.2000.0888. [DOI] [PubMed] [Google Scholar]
- 30.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Person Assess. 1988;52:30–41. [Google Scholar]
- 31.Kyngas H. Support network of adolescents with chronic disease: adolescents’ perspective. Nurs Health Sci. 2004;6:287–293. doi: 10.1111/j.1442-2018.2004.00207.x. [DOI] [PubMed] [Google Scholar]
- 32.O’Connell K, Schwartz J, Gerkovich M, Bott M, Shiffman S. Playful and rebellious states vs. negative affect in explaining the occurrence of temptations and lapses during smoking cessation. Nicotine Tob Res. 2004;6:661–674. doi: 10.1080/14622200410001734049. [DOI] [PubMed] [Google Scholar]
- 33.Spijkerman R, Van Den Eijnden RJ, Engels RC. Self-comparison processes, prototypes, and smoking onset among early adolescents. Prevent Med. 2005;40:785–794. doi: 10.1016/j.ypmed.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 34.Albers AB, Biener L. The role of smoking and rebelliousness in the development of depressive symptoms among a cohort of Massachusetts adolescents. Prevent Med. 2002;34:625–631. doi: 10.1006/pmed.2002.1029. [DOI] [PubMed] [Google Scholar]
- 35.Sinha JW, Cnaan RA, Gelles RJ. Adolescent risk behaviors and religion: findings from a national study. J Adolesc. 2007;30:231–249. doi: 10.1016/j.adolescence.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 36.Nonnemaker J, McNeely CA, Blum RW. Public and private domains of religiosity and adolescent smoking transitions. Soc Sci Med. 2006;62:3084–3095. doi: 10.1016/j.socscimed.2005.11.052. [DOI] [PubMed] [Google Scholar]
- 37.Harris S, Sherritt L, Holder D, Kulig J, Shrier L, Knight J. Reliability and validity of the brief multidimensional measure of religiousness/spirituality among adolescents. J Relig Health. 2008;47:438–457. doi: 10.1007/s10943-007-9154-x. [DOI] [PubMed] [Google Scholar]
- 38.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 39.Larimer ME, Palmer RS, Marlatt GA. Relapse prevention. An overview of Marlatt’s cognitive-behavioral model. Alcohol Res Health. 1999;23:151–160. [PMC free article] [PubMed] [Google Scholar]
- 40.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 41.Romer D, Jamieson P. Do adolescents appreciate the risks of smoking? Evidence from a national survey. J Adolesc Health. 2001;29:12–21. doi: 10.1016/s1054-139x(01)00209-9. [DOI] [PubMed] [Google Scholar]
- 42.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education. Theory, Research and Practice. San Francisco: Wiley & Sons; 2002. [Google Scholar]
- 43.Lazarus RS. Psychological Stress and the Coping Process. New York: McGraw-Hill; 1966. [Google Scholar]
- 44.Canty-Mitchell J, Zimet GD. Psychometric properties of the multidimensional scale of perceived social support in urban adolescents. Am J Comm Psych. 2000;28:391–400. doi: 10.1023/A:1005109522457. [DOI] [PubMed] [Google Scholar]
- 45.Lucas CP, Zhang H, Fisher PW, Shaffer D, Regier DA, Narrow WE, et al. The DISC Predictive Scales (DPS): efficiently screening for diagnoses. J Am Acad Child Adolesc Psychiatry. 2001;40:443–449. doi: 10.1097/00004583-200104000-00013. [DOI] [PubMed] [Google Scholar]
- 46.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.La Greca AM, Bearman KJ. The Diabetes Social Support Questionnaire—Family Version: evaluating adolescents’ diabetes-specific support from family members. J Pediatr Psychol. 2002;27:665–676. doi: 10.1093/jpepsy/27.8.665. [DOI] [PubMed] [Google Scholar]
- 48.Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113:229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- 49.McCusker J. Development of scales to measure satisfaction and preferences regarding long-term and terminal care. Med Care. 1984;22:476–493. doi: 10.1097/00005650-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Ronan KR, Kendall PC. Self-talk in distressed youth: states-of-mind and content specificity. J Clin Child Psychol. 1997;26:330–337. doi: 10.1207/s15374424jccp2604_1. [DOI] [PubMed] [Google Scholar]