Abstract
Importance
Guidelines recommend women ≥75 years be informed of benefits and risks of mammography before being screened; however, few are adequately informed.
Objective
To develop and evaluate a mammography screening decision aid (DA) for women ≥75 years.
Design
We designed the DA using international standards. From July 2010 to April 2012, participants completed a pretest survey and read the DA prior to an appointment with their primary care physician (PCP); they completed a posttest survey after their appointment. Medical records were reviewed for follow-up information.
Setting
Boston academic primary care practice.
Participants
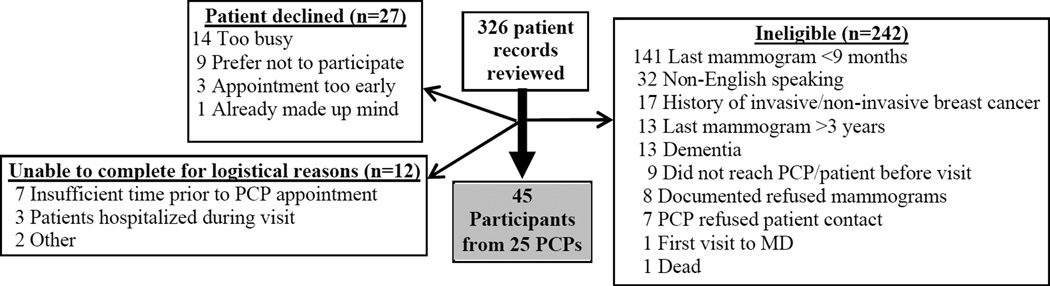
Eligible women were 75–89 years, English-speaking, had not had a mammogram in 9 months but were screened within the past 3 years, and did not have a history of dementia or invasive or non-invasive breast cancer. Of 84 women approached, 27 declined to participate, 12 were unable to complete the study for logistical reasons, and 45 participated.
Intervention
The DA includes information on breast cancer risk, life expectancy, competing mortality risks, possible outcomes of screening, and a values clarification exercise.
Outcomes
Knowledge of benefits and risks of screening, decisional conflict, and screening intentions; documentation in medical record of discussion of risks and benefits of mammography with PCP within 6 months; and receipt of screening within 15 months. We used the signed rank test and McNemar’s test to compare pretest/posttest information.
Results
Participant median age was 79 years; 69% were Non-Hispanic white; and 60% had attended some college. Comparison of “posttest” to “pretest” results found: 1) knowledge improved, p<0.001; and 2) fewer participants intended to be screened (56% after compared with 82% before, p=0.03). Decision conflict declined but not significantly (p=0.10). In the following 6 months, 53% of participants had a PCP note documenting discussion of risks and benefits of screening compared with 11% in the previous 5 years, p<0.001. While 84% had been screened within 2 years of participating; 60% were screened within 15 months after participating (at least 2 years since their last mammogram, p=0.01). Overall, 93% found the DA helpful.
Conclusions
Our findings suggest that a decision aid may improve older women’s decision-making around mammography screening.
INTRODUCTION
Currently, there are 11.4 million US women ≥75 years and this number is projected to nearly double by 2030.1 Meanwhile, breast cancer incidence increases with age.2 While mammography screening has been shown to reduce breast cancer mortality by 15% to 25% for women 50–74 years,3,4 none of the mammography screening trials included women ≥75 years.4 Screening may benefit some older women by detecting breast cancers early that otherwise would have resulted in major morbidity and/or mortality had treatment been delayed. However, screening may also cause immediate harm including pain, anxiety, complications from follow-up tests (e.g., breast biopsy), and overdiagnosis (detecting tumors that are of no threat).5Overdiagnosis is particularly concerning because complications from breast cancer treatment increase with age.6,7
Because there is an estimated 10-year lag-time to experiencing a mortality benefit but important risks to mammography that occur immediately,8 the American Geriatrics Society and the American Cancer Society recommend not screening older women in poor health and with short life expectancies.9,10 The United States Preventive Services Task Force states that there is insufficient evidence to recommend mammography to women ≥75 years.11 The guidelines all recommend older women be informed of mammography’s risks and benefits.9–11 However, in practice few older women are adequately informed.12 As a result, many overestimate the benefits and underestimate the harms of screening.13,14
Despite the need, there is no decision support available to help women ≥75 years decide whether or not to continue undergoing mammography screening. Decision aids (DAs) are designed to help patients learn more about a medical intervention, clarify their values, and be more involved in decision-making.15,16DAs may be designed in various formats (e.g., booklets, webpage) and differ from usual health educational materials because of their detailed focus on options and outcomes of a decision.16DAs have been shown to improve medical decision-making,15,16and are especially recommended when the ratio of benefits to risks of an intervention is uncertain,17 as is the case for mammography screening for women ≥75 years.
We aimed to develop a comprehensive, easy-to-read DA for women ≥75 years contemplating mammography that informs users of mammography’s risks and benefits and includes tailored information about health and life expectancy. We evaluated the DA in a pilot pretest/posttest trial to examine its effect on older women’s knowledge about mammography, decisional conflict, and screening decisions. In addition, we examined whether providing patients with the DA before a clinic visit leads to more balanced discussion with primary care physicians (PCPs) about mammography.
METHODS
We developed a decision aid (DA) to help women ≥75 years with mammography screening decisions. We evaluated this DA in a pretest/posttest trial.
Description of Decision Aid
We developed our DA in concordance with International Standards.18,19 We used the Ottawa Decision Support Framework20 and considered older adults’ decision-making processes.21 To better understand older women’s decision-making and informational needs around mammography, we previously conducted a qualitative study.13 Since the current cohort of women ≥75 years tends to have low computer literacy,22we chose a pamphlet format.
Our DA includes information on the entire screening process - including follow-up tests and treatment.17It begins by explaining its purpose and who should read it (e.g., it is not for women with history of breast cancer). eTable1 provides justification and references for the DA’s content. Briefly, the information presented was collected through literature review and includes information on 1) breast cancer risk factors for women ≥75 years; 2) health/life expectancy; 3) likely outcomes if screened and not screened with mammography; 4) competing mortality risks; 5) breast cancer treatments; and 6) a values clarification exercise. The last page asks users their intentions of being screened on a 15-point validated scale and invites users to share this information with their clinician.23
To enhance clarity, we used at least 14 point font, brief sentences, and neutral tone.24We described outcomes using words and frequencies. We presented frequencies using pictographs (icon arrays)-a picture of 1,000 circles where each circle represents one woman and we shaded in the number likely to experience an outcome.25To maximize comprehension, we used the same denominator, 1,000 (allowing us to show events as whole numbers), and time frame (5 years) for every outcome.24 We used both positive (e.g., 975 are screened but not diagnosed with breast cancer) and negative framing (e.g., 25 are diagnosed with breast cancer).24
As recommended for DA development, we assembled a 10 member expert panel (internists, geriatricians, health services researchers, and a psychologist) to review iterative versions.19Once the expert panel approved a final version, we tested the DA’s comprehensibility among 5 older women who had recently decided whether or not to be screened. We revised the DA based on their feedback. We then tested the DA among 15 older women contemplating mammography and 5 of their PCPs recruited from a large academic primary care practice in Boston. We made additional edits based on their feedback. Throughout the pretest/posttest trial, we also made small, non-substantive changes to the DA to improve clarity. The final version is 11 pages, filled with pictures, and written at a 6th grade reading level (available in the appendix and by request).
Pretest/Posttest Trial
Study Sample
Women were eligible for the pretest/posttest trial if they 1) were 75–89 years; 2) did not have dementia (determined by problem list, PCP communication, or by score of >19 [indicative of severe impairment] on the Short-Blessed Test,26 which was administered before enrollment); 3) had no history of invasive or non-invasive breast cancer; 4) received care at a large general internal medicine or primary care geriatrics practice in Boston; and 5) were scheduled with their PCP between July 2010 and April 2012. To target women contemplating screening, we further excluded women who had not been screened in three years, women who had been screened in the past nine months, and women with documentation that they declined future mammograms. While increasingly data suggest that it is appropriate to screen women biennially,27 many women undergo mammography annually and we aimed to include women before their next mammogram.28
Recruitment
We identified women by reviewing PCP appointment logs. Once potentially eligible women were identified and PCPs gave approval for contact, we contacted women to inform them of the study and obtain verbal informed consent. Afterwards, a research assistant (RA) administered the pretest survey. We then asked women to come to a routine appointment with their PCP early to read the DA. After reading the DA, which takes approximately 5–10 minutes, participants attended their scheduled visit. PCPs were not required to discuss mammography. PCPs were informed that their patients received the DA and were sent the DA to review if preferred. After the visit, the RA administered the posttest survey. PCPs were sent a survey asking their perceptions of the DA. Beth Israel Deaconess Medical Center’s Committee on Clinical Investigations approved this study.
Data Collection
At baseline we assessed participant’s race/ethnicity, education, insurance, marital status, subjective numeracy,29 medical literacy (REALM-7 - range 0 to 7, higher scores indicate higher literacy),30 and estimated life expectancy (measured by the Schonberg index [scores ≥8 indicate ≤9 year mortality]).28,31 We assessed the following outcomes in both the pretest and posttest surveys (instruments available in eAppendix). All measures used are recommended to assess whether a DA improves decision-making.16,18,32
Outcomes
Knowledge about mammography
10 questions (2 multiple choice and 8 true/false); 7 questions were adapted from other studies.33–36 Three questions were developed based on material in our DA and were cognitively tested with 10 older women before using. We summed correct responses.
Decisional Conflict Scale
A validated 16 item scale to measure whether one feels informed, clear about their values (e.g. “I am clear about whether the benefits or risks of mammography are more important to me”), and certain and supported in their decision-making.37,38 We calculated total and 5 subscale scores (uncertainty, informed, values clarity, support, effective). Scores on each scale range from 0–100 and lower scores indicate higher quality decision-making.
Screening intentions
A 15-point validated scale to assess one’s propensity to being screened. We categorized scores as 1–5 (yes), 6–10 (unsure), or 11–15 (no).23
Decision-making role
Older women’s preferred role in decision-making around mammography (active [patient makes final decision], shared, or passive to doctor).39
Acceptability
In the posttest survey only we asked about the DA’s length, clarity, and balance, whether it is anxiety provoking, and whether participants would recommend it to a friend.40 We also recorded additional comments participants made about the DA.
Screening discussions
We reviewed all participants’ primary care notes five years before participating and six months after to assess for documented discussions about mammography. We chose six months follow-up since we hypothesized that some women would ask their PCP about mammography at their next visit. We defined a balanced discussion as documentation beyond the typical notation endorsing mammography (e.g. “mammogram recommended ”). We categorized a woman as having received a balanced discussion about mammography if her PCP documented: a) discussion of a limitation of screening (e.g., “no data on benefit for this age”) or b) that mammography was discussed AND whether the patient chose to continue with screening. Three authors (ERM, MBH, MAS) coded whether a balanced discussion occurred (ERM and MBH were blinded to whether the relevant note was in the pre- or posttest period). The authors’ coding agreed on first review except in two cases and these cases were reconciled through consensus.
Screening
We performed chart abstraction to examine receipt of mammography screening 15 months after participation. Chart abstraction is considered the gold standard for assessing receipt of mammography.41We chose 15 months follow-up since it provided at least two years of data since participants’ last mammogram (9 months [eligibility criteria] +15 months [follow-up]=24 months since last mammogram). Two years is the upper bound of the recommended screening interval for women for whom mammography is appropriate.11We also captured any diagnostic mammograms performed. Screening done outside the health system is captured in preventive health sheets and/or physician notes. All medical records were reviewed twice by one author (MAS), the second time ≥20 months after patients participated to capture mammograms completed during the 15 month follow-up period but entered later.
Data Analysis
We used the signed rank and the exact McNemar’s test to compare pretest/posttest information. We further examined the effect of the DA on screening decisions among older women stratifying by life expectancy (≤9 vs. >9 year life expectancy).31We examined whether the acceptability of the DA differed by educational attainment using bivariable statistics. We aimed to recruit 42 patients to detect a moderate effect size (0.6 times the estimated standard deviation) of the DA on patient knowledge and decisional conflict assuming within-patient correlation of 0.1. We performed a complete case analysis. All analyses were completed using SAS statistical software, version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
We reviewed 326 patient records of which 84 met eligibility criteria (Figure 1). Of these 84 women, 27 declined participation and 12 were unable to complete the study due to scheduling conflicts or hospital admission. Women who did not participate did not differ in age from those who participated (p=0.20) and the 12 women who were unable to complete the study also did not differ from participants based on education (p=0.71). Table 1 provides the 45 participants’ sample characteristics.
Figure 1.
Sample Selection
Table 1.
Sample Characteristics
| Sample Characteristicsa | n=45 |
|---|---|
| Race | |
| Non-Hispanic White, No. (%) | 31 (69) |
| Non-Hispanic Black, No. (%) | 14 (31) |
| Education | |
| <High-school, No. (%) | 4 (9) |
| High-school, No. (%) | 14 (31) |
| Some college, No. (%) | 15 (33) |
| College degree or beyond, No. (%) | 12 (27) |
| Income | |
| $35K or less, No. (%) | 19 (42) |
| $36K to $65K, No. (%) | 8 (18) |
| $66K or higher, No. (%) | 7 (16) |
| Declined to answer, No. (%) | 11 (24) |
| Currently married, No. (%) | 12 (27) |
| Lives alone, No. (%) | 28 (62) |
| Orientation-Memory-Concentration Test | |
| 0–8 (no impairment), No. (%) | 40 (88) |
| 9–19 (mild to moderate impairment), No. (%) | 5 (12) |
| Life expectancy | |
| >9 years, No. (%) | 19 (42) |
| ≤ 9 years, No. (%) | 26 (58) |
| Medical literacy assessed using REALM-7b | |
| 7 medical terms correctly pronounced, No. (%) | 43 (96) |
| 5–6 medical terms correctly pronounced, No. (%) | 2 (4) |
| Subjective numeracy, median [IQR]c | 3.4 [2.6–3.9] |
Table 2 presents changes in outcomes post exposure to the DA relative to baseline. The posttest survey was done immediately after the visit in 82% (n=37) of cases and was administered a median of 9.5 days (interquartile range 4.5–14.5) after the pretest. We found that participants’ knowledge of mammography’s risks and benefits improved; women answered on average 1 more question correctly (interquartile range 0–2) on the 10 item index. Fewer participants intended to be screened after reading the DA. Among women with ≤9-year life expectancy, a significantly lower proportion intended to pursue screening after reading the DA compared to before. In contrast, we found no difference in screening intentions among women with >9-year life expectancy. Decisional conflict declined after reading the DA but not significantly. We also did not observe a significant change in the number of women preferring an active role in decision-making after reading the DA.
Table 2.
Decision Aid Pretest and Posttest Information – Participant reported outcomes
| Outcome | Pretest (n=45) | Posttest (n=45) | p value |
|---|---|---|---|
| Knowledge, mean correct (SD) | 6.3 (1.3) | 7.3 (1.4) | <0.001 |
| Decisional Conflict Scale Total, mean (SD)a | 20.2 (13.7) | 16.5 (11.5) | 0.10 |
| Informed Subscaleb | 23.3 (15.0) | 18.0 (14.8) | 0.11 |
| Values Clarity Subscalec | 24.4 (16.5) | 19.6 (15.1) | 0.14 |
| Support Subscaled | 18.9 (20.4) | 12.8 (12.5) | 0.09 |
| Uncertainty Subscalee | 15.7 (16.6) | 15.4 (14.1) | 0.93 |
| Effective Decision Subscalef | 16.8 (16.2) | 16.3 (15.1) | 0.78 |
| Intentionsg | |||
| Intend to get a mammogram, No. (%) | 37 (82) | 25 (56) | 0.004 |
| Unsure/Intend not to get a mammogram, No. (%) | 8 (18) | 20 (44) | |
| Intentions (≤9 year life expectancy n=26) | |||
| Intend to get a mammogram, No. (%) | 22 (85) | 13 (50) | 0.004 |
| Unsure/Intend not to get a mammogram, No. (%) | 4 (15) | 13 (50) | |
| Intentions (>9 year life expectancy n=19) | |||
| Intend to get a mammogram, No. (%) | 15 (79) | 12 (63) | 0.45 |
| Unsure/Intend not to get a mammogram, No. (%) | 4 (21) | 7 (37) | |
| Preferred role in mammography screening decisionsh | |||
| Active (Patient makes the decision), No. (%) | 16 (39) | 18 (44) | 0.75 |
| Shared with doctor/Passive to doctor, No. (%) | 25 (61) | 23 (56) |
Decisional Conflict Scale- measures uncertainty in a decision, feeling informed in a decision, clear about personal values, supported, and whether one feels that decision-making is effective and likely to be implemented (scores range 0 [no decisional conflict] to 100 [extremely high decisional conflict]). There are 5 subscales detailed below.28,38
Informed Subcale – Scores range from 0 (feels extremely certain about best choice) to 100 (feels extremely uncertain about best choice).
Values Clarity Subscale- Scores range from 0 (feels extremely clear about personal values) to 100 (feels extremely unclear about personal values)
Support Subscale- Scores range from 0 (feels extremely supported in decision making to 100 (feels extremely unsupported in decision making).
Uncertainty Subscale- Scores range from 0 (feels extremely certain about best choice) to 100 (feels extremely uncertain about best choice).
Effective Decision Subscale- Scores range from 0 (good decision) to 100 (bad decision).
Intentions to be screened-15 point scale, 1–5 (yes), 6–10 (unsure), 11–15 (no)29
Controlled Preferences Scale-Assessed preferred role in decision-making around mammography screening.39
Overall, 96% (n=43) of women would recommend the DA, 93% (n=42) found it helpful, 71% (n=32) said the length was just right (29% [n=13] said it was too long), and 76% (n=34) found the amount of information just right (16% [n=10] thought there was too much information). Forty-two percent (n=18) found the information balanced, 42% found it slanted towards not getting a mammogram, and 16% (n=7) found it slanted towards getting a mammogram. All but one patient (98%) said they would prefer the DA to be on paper rather than computer. Perceptions of the DA did not differ by educational attainment; except that 44% (n=8) of women with a high school education or less compared to 19% (n=5) of women with at least some college education reported that the DA made them anxious (p=0.07).
Of 25 PCPs of the 45 participants, 15 PCPs (60%) completed a survey about using the DA, two of whom completed the survey for two different patients (we used the first survey completed). Overall, 73% (n=11) of PCPs agreed that using the DA would allow their patients to make more informed decisions; 80% (n=12) agreed that the DA would help their patients make more value laden decisions; and 93% (n=14) thought it would be helpful to patients. Sixty-seven percent (n=10) thought that using the DA was better than their usual approach to mammography. While 87% (n=13) thought the amount of information in the DA was just right, 67% (n=10) also reported it was too long. Additionally, 64% (n=10) found the DA balanced while 36% (n=5) found it slanted towards not getting a mammogram.
Table 3 presents the effect of exposure to the DA on PCP documentation of balanced discussions about mammography and on receipt of screening. We found that 53% of participants had a PCP note documenting a discussion of the risks and benefits of screening within six months of participating compared to 11% in the previous five years, p<0.001. Two women underwent diagnostic mammograms as their first follow-up test and were excluded from analyses examining receipt of screening. One of these woman experienced a negative diagnostic mammogram and the other was diagnosed with stage I ductal carcinoma. Among the 43 remaining women, 84% (n=36) were screened within two years before participating and 60% (n=26) by 15 months follow-up (p=0.01).
Table 3.
Decision Aid Pretest and Posttest Information –Data from Chart Abstraction (n=45)
| Documented discussion of benefits and risks of mammographya, No. (%) | 5 (11) [5 years before] | 24 (53) [6 months after] | <0.001 |
| Screened with mammographybc (n=43), No. (%) | 36 (84)[2 years before] | 27 (63) [15 months after] | 0.02 |
| Screened with mammographyb (≤9 year life expectancy n=25), No. (%) | 20 (80) [2 years before] | 13 (52) [15 months after] | 0.04 |
| Screened with mammographyb (>9 year life expectancy n=18), No. (%) | 16 (89) [2 years before] | 14 (78) [15 months after] | 0.63 |
We reviewed medical records the 5 years before participating and up to 6 months after participating to see if there was a primary care physician note documenting a discussion of the benefits/risks of mammography.
We examined screening 15 months after participating since this follow-up time allowed for information at least two years since participant’s last screening mammogram.
We excluded 2 women whose first follow-up test was a diagnostic mammogram.
DISCUSSION
Findings from this pilot study suggest that we have developed a promising decision aid (DA) that may improve older women’s mammography screening decisions. In a small sample of older women, our DA improved older women’s knowledge of mammography’s risks and benefits, led to fewer older women intending to be screened particularly those with short life expectancy, and possibly led to fewer women with short life expectancy being screened. Providing the DA before a visit with a PCP may also have led to improved patient-physician communication around screening.
Allowing older women to make an informed mammography screening decision is essential for high quality care. Our DA may improve this process. Only one other study, conducted in Australia, examined the effect of a mammography screening DA among older women. The DA used in that study was designed to help women aged 70 decide whether or not to continue screening. In Australia, although women ≥70 years may choose to be screened, only women aged 50–69 are invited for screening; therefore age 70 is a decision point. A large trial demonstrated that the DA increased older women’s knowledge about mammography but did not change participation in screening, even among women in poor health.33 The DA used was also limited by its length and high literacy requirement. Unlike our DA, the DA used in that study did not inform users about the uncertainty of a mortality benefit of mammography for older women, did not discuss the impact of life expectancy, and did not mention which breast cancer treatments may be offered to older women. Including these features may be why exposure to our DA resulted in fewer older women, particularly those with short life expectancy, choosing to be screened. Developing and testing a DA in the US is particularly important since there is high enthusiasm for cancer screening in the US.42,43
Although the majority of older women and their PCPs found our DA balanced, a substantial minority found it slanted towards not getting a mammogram. This may be due to years of public health messages and physicians emphasizing mammography’s benefits.42,44In this setting, an educational tool that presents mammography’s risk and benefits may be perceived by some as biased against mammography. Also, some have found that users of DAs perceive balance in the direction of the choice that they have made.45In our study 56% of women who were not screened found the DA slanted towards not getting a mammogram compared to 36% of women who were screened (p=0.20).Some women who chose not to be screened reported that the DA gave them this option. They had privately wondered if they could stop being screened but assumed they needed to continue. Furthermore, perfect balance may not be achievable in a DA if the body of evidence surrounding a test tends to favor not getting the test,45 which may be true in the case of mammography screening for women ≥75 years. However, based on our findings, we will make changes to the DA to improve balance. We will add that most older women treated with lumpectomy do well.46 Also, based on an updated literature review, we may have overestimated overdiagnosis and will reduce our estimate (see eTable 1 for justification).47 Despite perceptions by some that the DA was biased against screened, the majority (63%) of women chose to be screened after reading the DA, particularly those in good health.
Overall, we found a small non-significant decline in decisional conflict after reading our DA. While reducing decisional conflict has traditionally been an important goal of DAs, some argue that decisional conflict may promote appropriate deliberation.38,48 In the case of mammography, it is feasible that older women previously unaware of mammography’s limitations may feel more conflicted about screening after reviewing the DA than before. Our results tended to show that women felt more informed, clearer in their values and more supported in their decision-making; however, there was no change in certainty about one’s choice. In line with these findings, 30% of women found the DA anxiety-provoking, particularly women with lower educational attainment. These women reported feeling anxious that if they chose not to get screened they would be disappointing their PCP and/or deviating from societal norms. Our findings suggest that older women with lower educational attainment may need more support when using the DA or when engaging their PCP in shared decision-making around mammography.
While the majority of patients found the DA’s length just right, 64% of PCPs thought it was too long. An interactive web-based DA would allow users to focus on aspects of the DA helpful to them. Since we anticipate that future cohorts of older women will likely be more computer literate, we plan to develop and test a web-based version of the DA as a next step.
There are logistical challenges to using DAs in primary care including difficulty identifying appropriate patients for use, limited time during clinic visits, and inconsistent delivery by PCPs.49To overcome these challenges, we had a research assistant act as a panel manager and identify appropriate patients for use and provide patients with the DA before a PCP visit. Ideally, for implementation, health systems would have the infrastructure to identify eligible patients to read the DA before a visit. However, this is often not the case and more work is needed to identify best ways to implement decision support across a range of practices, especially for older adults. This is especially important since the Affordable Care Act explicitly promotes shared decision-making and use of decisions support interventions.50
This study has important limitations. First, generalizability is limited since it a small, single site study and many of the participants were highly educated. We used a quasi-experimental design and therefore changes in PCP discussions around mammography and declines in screening could be due to secular changes. Moreover, five participants were age 75 and a discussion about stopping mammography in the five years before participating may not have been appropriate. Knowledge may have improved since the posttest survey was the second exposure to the knowledge test. In addition, we cannot separate the effect of PCP knowledge of the DA from the effect of the DA itself; however, DAs are intended to supplement rather than replace physician-patient interaction.15,16 Finally, in this pilot study, our power to adjust our analyses for multiple comparisons was limited.
We designed a novel DA to help older women with decision-making around mammography screening. We next plan to test the DA’s efficacy in a large randomized controlled trial. The DA may lead to improved decision-making around mammography, especially among older women with short life expectancy who are least likely to benefit and are at greater risk of being harmed from screening.
Supplementary Material
ACKNOWLEDGMENT
We are grateful to Rossana Valencia, MPH and Christine Gordon, MPH for their work in developing and evaluating the decision aid. Written permission has been obtained from all persons named in this acknowledgment. Dr. Schonberg had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Mara Schonberg was supported by a Paul B. Beeson Career Development Award in Aging supported by the National Institute on Aging K23 [K23AG028584], The John A. Hartford Foundation, The Atlantic Philanthropies, The Starr Foundation, and The American Federation for Aging Research. Dr. Davis received support from Harvard Catalyst, The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers). Dr. Wee was supported by a NIH Midcareer Mentorship Award (K24DK087932). Dr. Marcantonio was supported by a Midcareer Investigator Award in Patient-Oriented Research from the National Institute on Aging (K24 AG035075). The sponsors had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Financial Disclosure Information: This research was supported by a Paul B. Beeson Career Development Award in Aging supported by the National Institute on Aging K23 [K23AG028584], The John A. Hartford Foundation, The Atlantic Philanthropies, The Starr Foundation, and The American Federation for Aging Research. Dr. Davis received support from Harvard Catalyst, The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers). Dr. Wee was supported by a NIH Midcareer Mentorship Award (K24DK087932). Dr. Marcantonio was supported by a Midcareer Investigator Award in Patient-Oriented Research from the National Institute on Aging (K24 AG035075).
Footnotes
Presentation: This research was presented in part at the 2012 annual meeting of the Gerontological Society of America in San Diego, CA, the 2013 meeting of the Society of General Internal Medicine in Denver, CO, the 2013 annual meeting of the American Geriatrics Society in Grapevine, TX, and the 2013 meeting of the Society of Medical Decision Making in Baltimore, MD.
We have no conflicts of interest to report.
REFERENCES
- 1.The next four decades. The older population in the United States: 2010 to 2050. Population estimates and projections. Appendix Table A-3. Projections of the Older Population by Selected Age Group and Sex, and Sex Ratios for the United States: 2010 to 2050. [Accessed October 23, 2013]; Available at: http://www.census.gov/prod/2010pubs/p25-1138.pdf.
- 2.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27(17):2758–2765. doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- 3.Independent UKPoBCS. The benefits and harms of breast cancer screening: an independent review. Lancet. 2012;380(9855):1778–1786. doi: 10.1016/S0140-6736(12)61611-0. [DOI] [PubMed] [Google Scholar]
- 4.Gotzsche PC, Jorgensen KJ. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2013;6:CD001877. doi: 10.1002/14651858.CD001877.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285(21):2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- 6.Buchholz TA. Radiation therapy for early-stage breast cancer after breast-conserving surgery. N Engl J Med. 2009;360(1):63–70. doi: 10.1056/NEJMct0803525. [DOI] [PubMed] [Google Scholar]
- 7.Crivellari D, Bonetti M, Castiglione-Gertsch M, et al. Burdens and benefits of adjuvant cyclophosphamide, methotrexate, and fluorouracil and tamoxifen for elderly patients with breast cancer: the International Breast Cancer Study Group Trial VII. J Clin Oncol. 2000;18(7):1412–1422. doi: 10.1200/JCO.2000.18.7.1412. [DOI] [PubMed] [Google Scholar]
- 8.Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O'Brien S, Walter LC. Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ. 2013;346:e8441. doi: 10.1136/bmj.e8441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Cancer Society Guidelines for the Early Detection of Cancer. [Accessed October 5, 2013]; Available at: http://www.cancer.org/Healthy/FindCancerEarly/CancerScreeningGuidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer. [Google Scholar]
- 10.Breast cancer screening in older women. American Geriatrics Society Clinical Practice Committee. J Am Geriatr Soc. 2000;48(7):842–844. [PubMed] [Google Scholar]
- 11.Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151(10):716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. W-236. [DOI] [PubMed] [Google Scholar]
- 12.Hoffman RM, Lewis CL, Pignone MP, et al. Decision-making processes for breast, colorectal, and prostate cancer screening: the DECISIONS survey. Med Decis Making. 2010;30(5 Suppl):53S–64S. doi: 10.1177/0272989X10378701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schonberg MA, Ramanan RA, McCarthy EP, Marcantonio ER. Decision making and counseling around mammography screening for women aged 80 or older. J Gen Intern Med. 2006;21(9):979–985. doi: 10.1111/j.1525-1497.2006.00487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Torke AM, Schwartz PH, Holtz LR, Montz K, Sachs GA. Older adults and forgoing cancer screening:"I think it would be strange". JAMA Intern Med. 2013;173(7):526–531. doi: 10.1001/jamainternmed.2013.2903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Connor AM, Rostom A, Fiset V, et al. Decision aids for patients facing health treatment or screening decisions: systematic review. BMJ. 1999;319(7212):731–734. doi: 10.1136/bmj.319.7212.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Connor AM, Stacey D, Entwistle V, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;(2):CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 17.Barratt A, Trevena L, Davey HM, McCaffery K. Use of decision aids to support informed choices about screening. BMJ. 2004;329(7464):507–510. doi: 10.1136/bmj.329.7464.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elwyn G, O'Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Connor AM, Jacobsen MJ. Workbook on developing and evaluating patient decision aids. [Accessed October 5, 2013];2003 Available from www.ohri.ca/decisionaid. [Google Scholar]
- 20.O'Connor AM, Tugwell P, Wells GA, et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns. 1998;33(3):267–279. doi: 10.1016/s0738-3991(98)00026-3. [DOI] [PubMed] [Google Scholar]
- 21.Peters E, Diefenbach MA, Hess TM, Vastfjall D. Age differences in dual information-processing modes: implications for cancer decision making. Cancer. 2008;113(12 Suppl):3556–3567. doi: 10.1002/cncr.23944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rideout V, Neuman T, Kichman M, Brodie M. Kaiser Family Foundation. 2005. e-Health and the Elderly: How Seniors Use the Internet for Health Information. [Accessed October 15, 2013]; http://kff.org/medicare/poll-finding/e-health-and-the-elderly-how-seniors-2/. [Google Scholar]
- 23.O'Connor AM. User Manual- Measures of Decision/Choice Predisposition [document on the Internet]. Ottawa: Ottawa Hospital Research Institute. [Accessed October 10, 2013];1996 :5. [modified 2003], Available from http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_ChoicePredisposition_Decision.pdf. [Google Scholar]
- 24.Bogardus ST, Jr, Holmboe E, Jekel JF. Perils, pitfalls, and possibilities in talking about medical risk. JAMA. 1999;281(11):1037–1041. doi: 10.1001/jama.281.11.1037. [DOI] [PubMed] [Google Scholar]
- 25.Hawley ST, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ Couns. 2008;73(3):448–455. doi: 10.1016/j.pec.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 26.Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 27.Braithwaite D, Zhu W, Hubbard RA, et al. Screening outcomes in older US women undergoing multiple mammograms in community practice: does interval, age, or comorbidity score affect tumor characteristics or false positive rates? J Natl Cancer Inst. 2013;105(5):334–341. doi: 10.1093/jnci/djs645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schonberg MA, Breslau ES, McCarthy EP. Targeting of Mammography Screening According to Life Expectancy in Women Aged 75 and Older. J Am Geriatr Soc. 2013;61(3):388–395. doi: 10.1111/jgs.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 30.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 31.Schonberg MA, Davis RB, McCarthy EP, Marcantonio ER. External validation of an index to predict up to 9-year mortality of community-dwelling adults aged 65 and older. J Am Geriatr Soc. 2011 Aug;59(8):1444–1451. doi: 10.1111/j.1532-5415.2011.03523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kryworuchko J, Stacey D, Bennett C, Graham ID. Appraisal of primary outcome measures used in trials of patient decision support. Patient Educ Couns. 2008;73(3):497–503. doi: 10.1016/j.pec.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 33.Mathieu E, Barratt A, Davey HM, McGeechan K, Howard K, Houssami N. Informed choice in mammography screening: a randomized trial of a decision aid for 70-year-old women. Arch Intern Med. 2007;167(19):2039–2046. doi: 10.1001/archinte.167.19.2039. [DOI] [PubMed] [Google Scholar]
- 34.Stager JL. The comprehensive Breast Cancer Knowledge Test: validity and reliability. J Adv Nurs. 1993;18(7):1133–1140. doi: 10.1046/j.1365-2648.1993.18071133.x. [DOI] [PubMed] [Google Scholar]
- 35.van Agt H, Fracheboud J, van der Steen A, de Koning H. Do women make an informed choice about participating in breast cancer screening? A survey among women invited for a first mammography screening examination. Patient Educ Couns. 2012;89(2):353–359. doi: 10.1016/j.pec.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Wilcox S, Stefanick ML. Knowledge and perceived risk of major diseases in middle-aged and older women. Health Psychol. 1999;18(4):346–353. doi: 10.1037//0278-6133.18.4.346. [DOI] [PubMed] [Google Scholar]
- 37.O'Connor AM. User Manual- Decisional Conflict Scale (16 item statement format) [document on the Internet]. Ottawa: Ottawa Hospital Resarch Institute. [Accessed October 5, 2013];1993 :16. [updated 2010], Available from http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf. [Google Scholar]
- 38.O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 39.Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277(18):1485–1492. [PubMed] [Google Scholar]
- 40.O'Connor AM. User Manual-Acceptability [document on the Internet]. Ottawa: Ottawa Hospital Research Institute; copyright. [[modified 2002], Accessed October 13, 2013];1996 :5. Available from http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf. [Google Scholar]
- 41.Caplan LS, Mandelson MT, Anderson LA. Validity of self-reported mammography: examining recall and covariates among older women in a Health Maintenance Organization. Am J Epidemiol. 2003;157(3):267–272. doi: 10.1093/aje/kwf202. [DOI] [PubMed] [Google Scholar]
- 42.Schwartz LM, Woloshin S, Fowler FJ, Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291(1):71–78. doi: 10.1001/jama.291.1.71. [DOI] [PubMed] [Google Scholar]
- 43.Smith-Bindman R, Chu PW, Miglioretti DL, et al. Comparison of screening mammography in the United States and the United kingdom. JAMA. 2003;290(16):2129–2137. doi: 10.1001/jama.290.16.2129. [DOI] [PubMed] [Google Scholar]
- 44.Domenighetti G, D'Avanzo B, Egger M, et al. Women's perception of the benefits of mammography screening: population-based survey in four countries. Int J Epidemiol. 2003;32(5):816–821. doi: 10.1093/ije/dyg257. [DOI] [PubMed] [Google Scholar]
- 45.Barry MJ. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136(2):127–135. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 46.Audisio RA. The surgical risk of elderly patients with cancer. Surg Oncol. 2004;13(4):169–173. doi: 10.1016/j.suronc.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 47.Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005. doi: 10.1056/NEJMoa1206809. [DOI] [PubMed] [Google Scholar]
- 48.Nelson WL, Han PK, Fagerlin A, Stefanek M, Ubel PA. Rethinking the objectives of decision aids: a call for conceptual clarity. Med Decis Making. 2007;27(5):609–618. doi: 10.1177/0272989X07306780. [DOI] [PubMed] [Google Scholar]
- 49.Brackett C, Kearing S, Cochran N, Tosteson AN, Blair Brooks W. Strategies for distributing cancer screening decision aids in primary care. Patient Educ Couns. 2010;78(2):166–168. doi: 10.1016/j.pec.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 50.Washington: 111th Congress, 2nd Session; 2010. Senate and House of Representatives. The Patient Protection and Affordable Care Act. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.