Abstract
Isolated unilateral absence of a proximal pulmonary main artery is a rare congenital lesion which is often associated with other cardiovascular abnormalities and a diverse clinical presentation. It is usually diagnosed in childhood. Patients who survive into adulthood is uncommon. We report a case of 46 year old hypertensive and obese female who presented with progressive dyspnea. She had features of pulmonary hypertension. The diagnosis was confirmed by CT pulmonary angiography which showed absence of right pulmonary artery and conventional pulmonary angiography which showed ipsilateral lung receiving collaterals from Right coronary artery and its branches. The purpose of this report is to highlight the fact that UAPA, although a rare entity, should be kept in mind in patients with unexplained PAH and prolonged respiratory symptoms unresponsive to routine treatment modalities.
Keywords: Unilateral absence of pulmonary artery (UAPA), Pulmonary artery hypertension (PAH), Progressive Dyspnea
1. Introduction
Isolated unilateral absence of pulmonary artery (UAPA) is quite a rare entity which often presents with recurrent pulmonary infections and hemoptysis. Most of the patients develop pulmonary hypertension. The average age of UAPA patients is 14 years (0.1–58 years).1 However because of the atypical symptoms some patients are diagnosed much later in life as in our case.
2. Case report
A 46-year-old hypertensive female was admitted for evaluation of progressively worsening dyspnea for last 4 years. She was morbidly obese with BMI of 37 kg/m2. Her baseline vitals were stable and her O2 saturation was 93% at room air. Initial possibility of dyspnea secondary to pulmonary venous hypertension (PVH), Chronic Thromboembolic Pulmonary Hypertension (CTEPH) or chronic lung disease with hypoxia was kept. OSA was ruled by Berlin criteria.
Her baseline investigations including CBC, RFT, LFT and ECG were normal. CK-MB, D-dimer and thyroid profile were in normal range. Chest X-ray showed elevated right hemidiaphragm and less prominent right pulmonary hilum as compared to left side. Echocardiography revealed dilated RA/RV with systolic Pulmonary Artery Pressure (PAP) of 75 mm Hg. Type I diastolic dysfunction was present and there was minimal pericardial effusion. Short axis view at level of aortic valve showed non-visualization of right pulmonary artery. Pulmonary hypertension due to PVH and left heart causes was ruled out. CT pulmonary angiography was done which showed congenital interruption of right branch of pulmonary artery with small right hemithorax with dilated main pulmonary artery and left pulmonary artery (Fig. 1). Subsequently pulmonary angiography and cath was performed which showed total cut off of right pulmonary artery after its origin. PAP was 70/40 with mean PAP = 50 mm Hg. Coronary angio showed normal coronaries. Prominent collaterals were seen arising from conus branch of right coronary artery supplying the right pulmonary artery branches (Fig. 2). A few collaterals were seen to arise from left coronary artery and branches of descending aorta. So the diagnosis of absent right pulmonary artery with distal vasculature supplied by collaterals from coronaries and descending aorta was confirmed.
Fig. 1.
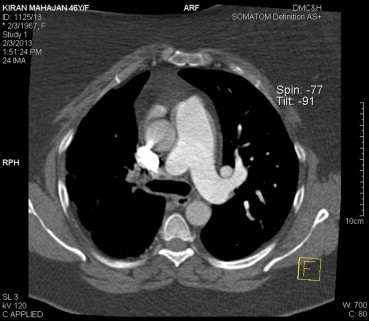
CT pulmonary angio showing absent right pulmonary artery.
Fig. 2.
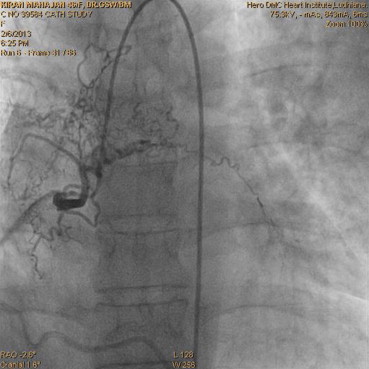
Angiogram showing prominent collaterals arising from RCA and supplying the right pulmonary artery branches.
Patient was discharged on phosphodiesterase inhibitors (Sildenafil) and oral anticoagulant therapy.
At one-month follow up there was significant improvement from NYHA class IV to class II.
3. Discussion
Congenital absence of one pulmonary artery is a rare congenital abnormality, with a prevalence of 1 in 200,000.2 It occurs equally in both sexes. Most of the patients have associated cardiovascular anomalies like Fallot's tetralogy, septal defects, right aortic arch and patent ductus arteriosus.3
This developmental anomaly is the result of a failure in the connection of the sixth aortic arch with the pulmonary trunk.4 The affected side is perfused by persisting embryonic arteries from the aorta or its branches, abnormal collaterals arising from the bronchial, subclavian, intercostal or diaphragmatic arteries, or hyperplastic normal bronchial arteries.
It has been reported that around 15% of the patients are asymptomatic.2 40% present with recurrent pulmonary infections, decreased exercise tolerance and exertional dyspnea.1 Extensive collateral circulation leads to hemoptysis in upto 20% of the affected individuals. Pulmonary arterial hypertension which develops due to increased blood flow to the unaffected lung is present in 25% cases and is an important affecting long-term survival.5
The entity of unilateral absence of pulmonary artery was reviewed in 3 publications covering different time era in last 60 years. Pool et al6 reviewed 32 cases before 1962. Shakibi et al5 studied 47 cases from 1962 to 1976. Harkel et al1 added a review of 108 cases from 1978 to 2000. Only 14 of them were asymptomatic. The median age of UAPA patients was 14 years (0.1–58 years). RPA was absent in 56–63% of the cases in these 3 case reviews.
A variety of imaging techniques are available to aid the diagnosis. A chest radiograph is usually the initial investigation that suggests the diagnosis. Echocardiography is helpful in excluding pulmonary hypertension and other intra-cardiac anomalies. CT is then performed for definitive diagnosis. Conventional angiography is reserved for patients requiring embolization or revascularization surgery.
Till date, there are only five case reports published describing a UAPA and coronary collaterals supplying the affected lung.7–11 Three of them reported absence of the right pulmonary artery8,10,11 while the other two reported absence of left pulmonary artery.7,9 In three of the five published cases there was no myocardial perfusion defect7–9 while in other two there was impairment of myocardial perfusion.10,11 Our patient is a middle aged female in which predominant collaterals were arising from right coronary artery and there was no evidence of myocardial ischemia.
When pulmonary hypertension is present in a patient with UAPA, their condition may be improved by revascularization of the side with the absent artery. In most cases, there is an identifiable artery at the hilum that may be used for revascularization.12
If revascularization is not possible, or when pulmonary hypertension does not improve, therapeutic measures such as those described for patients with primary pulmonary hypertension may be helpful. Our patient was put on phosphodiesterase inhibitors (Sildenafil) and oral anticoagulants.
Hemoptysis may be self-limiting over many years, but massive hemoptysis can be treated only by selective embolization of the systemic collaterals,13 or even pneumonectomy of the affected side.14
4. Conclusion
Isolated unilateral pulmonary artery agenesis usually presents in children but may remain undiagnosed till adulthood. Awareness of this condition will help in early diagnosis and treatment. The collaterals to the affected lung arising from the coronary vessels are also a rare entity.
Conflicts of interest
All authors have none to declare.
References
- 1.Ten Harkel A.D., Blom N.A., Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest. 2002;122:1471–1477. doi: 10.1378/chest.122.4.1471. [DOI] [PubMed] [Google Scholar]
- 2.Bouros D., Pare P., Panagou P. The varied manifestation of pulmonary artery agenesis in adulthood. Chest. 1995;108:670–676. doi: 10.1378/chest.108.3.670. [DOI] [PubMed] [Google Scholar]
- 3.Currarino G., Williams B. Causes of congenital unilateral pulmonary hypoplasia: a study of 33 cases. Pediatr Radiol. 1985;15:15–24. doi: 10.1007/BF02387847. [DOI] [PubMed] [Google Scholar]
- 4.Cucci C.E., Doyle E.F., Lewis E.W. Absence of a primary division of the pulmonary trunk. An ontogenetic theory. Circulation. 1964;29:124–131. doi: 10.1161/01.cir.29.1.124. [DOI] [PubMed] [Google Scholar]
- 5.Shakibi J.G., Rastan H., Nazarian I. Isolated unilateral absence of pulmonary artery: review of world literature and guidelines for surgical repair. Jpn Heart J. 1978;19:439–451. doi: 10.1536/ihj.19.439. [DOI] [PubMed] [Google Scholar]
- 6.Pool P.L., Vogel J.K., Blount S.G. Congenital unilateral absence of a pulmonary artery. The importance of flow in pulmonary hypertension. Am J Cardiol. 1962;10:706–732. doi: 10.1016/0002-9149(62)90248-5. [DOI] [PubMed] [Google Scholar]
- 7.Thompson J.A., Lewis S.A., Mauck H.P. Absence of the left pulmonary artery: anomalous collateral from the coronary artery to affected lung. Am Heart J. 1986;111:418–420. doi: 10.1016/0002-8703(86)90165-1. [DOI] [PubMed] [Google Scholar]
- 8.Gupta K., Livesay J.J., Lufschanowski R. Absent right pulmonary artery with coronary collaterals supplying the affected lung. Circulation. 2001;104:E12–E13. doi: 10.1161/hc2901.093602. [DOI] [PubMed] [Google Scholar]
- 9.Kochiadakis G.E., Chrysostomakis S.I., Igoumenidis N.E. Anomalous collateral from the coronary artery to the affected lung in a case of congenital absence of the left pulmonary artery effect on coronary circulation. Chest. 2002;121:2063–2066. doi: 10.1378/chest.121.6.2063. [DOI] [PubMed] [Google Scholar]
- 10.Kadi H., Kurtoglu N., Karadag B. Congenital absence of the right pulmonary artery with coronary collaterals supplying the affected lung: effect on coronary perfusion. Cardiology. 2007;108:314–316. doi: 10.1159/000099101. [DOI] [PubMed] [Google Scholar]
- 11.Soliman A., Jelani A., Eid A. Myocardial infarction due to coronary steal caused by a congenital unilateral absence of the right pulmonary artery: a rare case. BMJ. 2012 doi: 10.1136/bcr.04.2011.4108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sotomora R.F., Edwards J.E. Anatomic identification of so-called absent pulmonary artery. Circulation. 1978;57:624–633. doi: 10.1161/01.cir.57.3.624. [DOI] [PubMed] [Google Scholar]
- 13.Rene M., Sans J., Dominguez J. Unilateral pulmonary artery agenesis presenting with hemoptysis: treatment by embolization of systemic collaterals. Cardiovasc Intervent Radiol. 1995;18:251–254. doi: 10.1007/BF00239422. [DOI] [PubMed] [Google Scholar]
- 14.Mehta A.C., Livingston D.R., Kawalek W. Pulmonary artery agenesis presenting as massive hemoptysis: a case report. Angiology. 1987;38:67–71. doi: 10.1177/000331978703800110. [DOI] [PubMed] [Google Scholar]


