1. Introduction
Aspergillus was first catalogued by an Italian biologist – P. Micheli in 1729.1,2 The first case of infection was reported in a jackdaw in 1815 and in a human in 1842. In the 19th century it was an occupational hazard amongst wig combers when it caused allergic disease of the lungs. Aspergillus fumigatus is the most common species causing Aspergillosis. The spores of A. fumigatus are produced on specialized conidiophores ranging from 1.0 to 3.0 μm in diameter. The hyphae of A. fumigatus are 3–5 μm in diameter, septate, and often branch typically at a 45° angle.3 Aspergillus spores are widespread and are readily inhaled. Acute invasive Aspergillus infection mainly affects patients who are immunocompromised, and are extremely rare in immunocompetent individuals. It is rarely found in the heart. We are reporting a case of biopsy proven Aspergillosis extensively involving all the four chambers and the tricuspid and mitral valves of the heart and clinically mimicking neoplasm. No evident immunodeficiency could be identified in this case.
2. Case report
A 22-year-old male patient (who was HBsAg +ve with high viral load, DNA PCR 34 billion units) admitted for pain with numbness of both lower limbs and difficulty to walk since two months. He claimed to have taken vaccination for Hepatitis B 2 years back. He had weight loss of 15 kg over a period of 3 months. He had history of road transport accident and a head injury 5 months back and was treated in a local hospital. He took tetanus toxoid injection and pain killers from a local hospital. There were no signs or symptoms of severe head injury.
Clinically he was stable, except for weak pulse in the right dorsalis pedis and coldness of right leg. He was evaluated by the neurologist. Nerve conduction study of both lower limbs and computer tomography scan of the head were normal. Doppler examination of right lower limbs showed a big thrombus measuring 5.3 cm in the right common iliac artery and another thrombus measuring 1.2 cm in the right external iliac artery causing near total occlusion. The Electrocardiogram was normal. Chest skiagram showed miliary deposits throughout the lung fields.
The echocardiogram [Fig. 1] showed large tumor mass involving the inferior and inferolateral wall of the left ventricle extending across the atrioventricular groove into the lower one third of the left atrium. Mitral valve showed tumor vegetations attached to the posterior leaflet. Multiple tumor masses were seen involving the entire right atrial free wall with large vegetations attached to the tricuspid valve. Tumor masses involved the opening of the inferior venacava causing partial obstruction and extended to the superior venacava–right atrial junction.
Fig. 1.

Echocardiogram showing tumour masses with vegetations.
Computer tomography scan of chest [Fig. 2] showed large infiltrating hypo dense mass lesions which were seen involving the entire right atrial wall except the inter atrial septum. It extended in to the superior venacaval, inferior venacaval openings into the right atrium and compromising the right atrial cavity. Tricuspid valve showed large vegetations. Extensions into posterior, right lateral walls of right ventricle encased right coronary artery and its branches except right coronary origin. Another similar lesion was seen involving the free lateral and posterior walls of the left ventricle, including lateral aspect of mitral annulus and encroached into the adjacent left atrial wall encasing the mid and distal circumflex artery and its branches, partly the coronary sinus and veins. Mediastinal lymphadenopathy was also present. Clinically, malignancy or tuberculosis were considered.
Fig. 2.

CT scan showing the mass.
Mantoux test was negative. His CD4 count was normal, with a normal lymphocyte profile .The bone marrow biopsy and the bone marrow aspiration cytology were normal. Extensive investigations were done for HIV [ELISA/Western blot] and dyscollagenosis and they were negative. A trans catheter cardiac biopsy was done. Sections of biopsy specimen stained with haematoxylin and eosin showed multiple non-caseating granulomas and fungal hyphae. Periodic acid Schiff staining showed septate fungi with acute angles and a diagnosis of Aspergillus causing granulomatous lesion was made [Fig. 3].
Fig. 3.
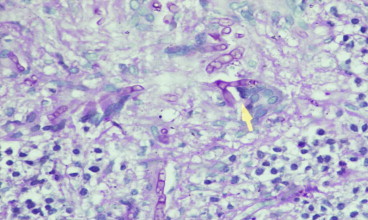
Histopathology slide showing septate hyphae with acute angles.
The patient was started on (antifungal) voriconazole 200 mg twice and entecavir 0.5 mg once in view of the high hepatitis B. Unfortunately after 3 days the patient developed aphasia and right-sided weakness. Magnetic resonance imaging scan of the head showed acute infarct in the left Middle cerebral artery territory. Patient was treated with low molecular weight heparin, antiplatelets and other supportive measures. Thrombolysis was not considered as the emboli were thought to be from the vegetations. Patient improved after one month of treatment. Echocardiogram repeated after three months showed reduction in the size of the mass [Fig. 4]. Patient was reassured and continued on voriconazole.
Fig. 4.

Three months after antifungal treatment.
Patient was readmitted with h/o palpitation and ECG showed supra ventricular tachycardia with a heart rate of 202/min, which required DC version and he was started on verapamil. He remained in sinus rhythm. Patient was on antiviral and antifungal treatment and doing well for about one year. He was readmitted with history of fever, productive cough and dyspnoea. Patient was in respiratory distress. Chest X-ray showed consolidation of the entire left lung, which required ventilator support. A diagnosis of lung abscess with septicaemia was made. He succumbed to septicaemia.
3. Discussion
Aspergillosis usually affects patients who are immune-compromised, and are extremely rare in immune-competent individuals. Most healthy people have natural immunity to the Aspergillus mould. If someone with damaged lungs or a weakened immune system (like renal transplant patient)4,5 breathes in Aspergillus spores, the infection is more likely to stay. Aspergilloma is common in people who have cystic fibrosis or cavities in their lungs. Aspergillosis can range from about mild to a life threatening disease.
The diagnosis of infection caused by this filamentous fungus poses many difficulties, mainly due to the lack of a laboratory method which can discriminate colonization from infection. Invasive fungal infections are important causes of morbidity and mortality in patients who have received solid organ or bone marrow transplants.4–6 Infection with Aspergillus species can result in a variety of clinical syndromes, including sinusitis, tracheobronchitis, pneumonia, necrotizing cellulitis, brain abscess, and disseminated disease.7 Aspergilloma in the heart is rare. Aspergillus endocarditis8,9 tends to occur in patients who have undergone open heart surgery. It has also been described as a complication of parenteral nutrition and drug addiction. Most frequently, the aortic and mitral valves are the sites of infection. Aspergillosis presenting as mass lesions and involving all the chambers of heart is not reported in the literature. Our case is unique in this aspect. The patient was extensively investigated to determine the immune status.
We are reporting here a case of biopsy proven Aspergillosis in the heart which affected the chambers, mitral and tricuspid valves and responded initially with antifungal treatment with a significant regression of the mass. This patient was HBsAg +ve with high viral load. This high viral load might have suppressed his immune system. He took multiple injections 5 months back followed by a head injury. We assume that this might have been the cause of hepatitis infection. Chances of hepatitis B infection after a needle prick injury is 2%–40%.10 The infection is possible if the serum immunoglobulin levels are low in spite of Hepatitis B vaccination. Dyscollagenosis as well as HIV infections were ruled out after extensive investigations. Transcatheter cardiac biopsy helped us to make the diagnosis.
4. Conclusion
Most of the invasive cardiac fungal infections reported in the literature were diagnosed by autopsy or by excision.11 In our case we could make a diagnosis by the help of trans catheter biopsy. We conclude that Aspergillus not only affects the heart valves but also the cardiac chambers. Aspergillosis involving all the four chambers has not been reported. Invasive Aspergillosis in the heart is difficult to treat and mortality is very high. To the best of our knowledge, this is the first case report.
Conflicts of interest
All authors have none to declare.
Acknowledgement
The authors are deeply indebted to Prof. Leena Devi, Head of the department of pathology, for her assistance.
References
- 1.caltexmoldservices.com/…on/mold_library/aspergillus.
- 2.www.cdc.gov/fungal/aspergillosis/.
- 3.http://www.aspergillus.org.uk/.
- 4.Singh Nina, Paterson David L. Aspergillus infections in transplant recipients. Clin Microbiol Rev. 2005 January;18:44–69. doi: 10.1128/CMR.18.1.44-69.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiland D., Ferguson R.M., Peterson P.K., Snover D.C., Simmons R.L., Najarian J.S. Aspergillosis in 25 renal transplant patients. Epidemiology, clinical presentation, diagnosis, and management. Ann Surg. 1983 November;198:622–629. doi: 10.1097/00000658-198311000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baddley J.W., Stroud T.P., Salzman D., Pappas P.G. Invasive mold infections in allogenic bone marrow transplant. Clin Infect Dis. 2001;32:1319. doi: 10.1086/319985. [DOI] [PubMed] [Google Scholar]
- 7.Montoya J.G. Invasive aspergillosis in the setting of cardiac transplantation. Clin Infect Dis. 2003;37:S281–S292. doi: 10.1086/376527. 1999-Cited by 64-Related articles. [DOI] [PubMed] [Google Scholar]
- 8.Mullen P., Jude C., Borkon M. Aspergillus mural endocarditis. Echocardiographically silent Aspergillus mural endocarditis. West J Med. 1988 September;149:334–338. [PMC free article] [PubMed] [Google Scholar]
- 9.Challa S., Prayaga A.K., Vemu L. Fungal endocarditis: an autopsy study. Asian Cardiovasc Thorac Ann. 2004;12:95–98. doi: 10.1177/021849230401200202. [DOI] [PubMed] [Google Scholar]
- 10.Gerberding J.L. Management of occupational exposures to blood-borne viruses. N Engl J Med. 1995 Feb 16;332:444–451. doi: 10.1056/NEJM199502163320707. [DOI] [PubMed] [Google Scholar]
- 11.Gori F., Nesi G., Pedemonte E. Aspergillus fungus balls on the mitral valve. N Engl J Med. Jan 25, 2001;344:301–311. doi: 10.1056/NEJM200101253440418. [DOI] [PubMed] [Google Scholar]


