Abstract
Ulcerative colitis is associated with several malignancies. Here we report one such association, a rare one, with papillary thyroid carcinoma, and discuss the possible risk factors of such an association.
Keywords: Colonoscopy, Thyroid cancer, Ulcerative colitis, Ultrasonography
Introduction
The association between ulcerative colitis (UC) and papillary thyroid carcinoma (the most common cancer of this gland, occurring mainly in young adults below age 40) is rare, and has only been reported only in 2 cases (1, 2). We describe a further such case report.
Case Report
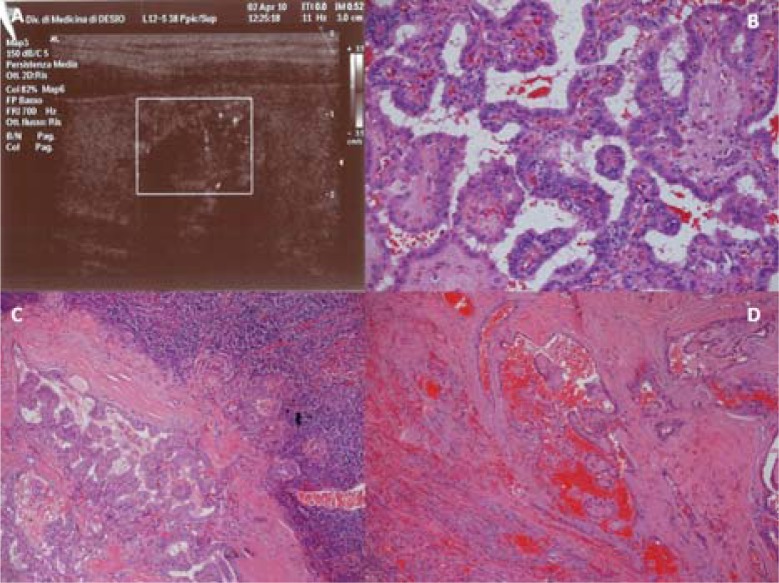
A 35 year old man was admitted in our department for a UC flare characterized by fever, abdominal pain and diarrhea associated to bloody stools; colonoscopy revealed severe pancolitis, confirmed by histology. The clinical picture gradually resolved after steroid treatment (prednisone 60 mg/day); mesalazine was started when tapering steroid therapy but it was stopped after some days due to abdominal pain associated to increased levels of pancreatic enzymes (amylase 160 U/L, normal upper value 100 U/L, lipase 160 U/L, normal upper value 60 U/L). Physical examination revealed a right thyroid nodule, confirmed by neck ultrasonography that showed a nodule 1.4 cm diameter with heterogeneous hypoechoic echogenic pattern associated with intra-parenchymal hyperechogenic microspots (Figure 1A). Cytological material obtained by ultrasound guided needle (25 gauge) aspiration revealed papillary thyroid carcinoma. Total thyroidectomy was performed; histological examination confirmed the diagnosis of papillary thyroid cancer (Figure 1B), also showing metastatic involvement in 5 out 13 latero-cervical lymph nodes removed and vascular invasion (Figures 1C and D). At present, the patient enjoys good health and is treated with salazopyrin, 1.5 g/day.
Figure 1.
A. Ultrasound appearance of right papillary thyroid carcinoma. B. Surgical specimen showing papillary thyroid carcinoma: complex and branching papillae, optical clear, with overlapping and grooved nuclei (hematoxylin and eosin, original magnification x20) C. Papillary carcinoma metastatic to a lymph node (hematoxylin and eosin, original magnification x4). D.Papillary thyroid carcinoma: vascular invasion (hematoxylin and eosin, original magnification x10)
Discussion
To date, only radiation exposure at young age has been shown as the most consistent risk factor identified and had been showed unequivocally to cause thyroid cancer. In the case reported by Evgenikos (2), the patient had been treated with immunosuppressive therapy (azathioprine) for 2 years; patients subjected to immunosuppressive therapy may have an increased risk of malignant tumors as skin carcinomas, non-Hodgkin lymphomas, Kaposi's Sarcoma, carcinoma of the cervix, perineum and vulva, and hepatobiliary carcinoma (3). Penn et al. (4) reported a thyroid tumor in a renal transplantation patient after immunosuppressive therapy; histology revealed a malignant lymphoma and multiple other organs were affected. Ginsberg et al. (1) described a young patient with papillary thyroid carcinoma, sclerosing cholangitis and UC, and Moss et al. (6) described five cases of papillary thyroid carcinoma associated with Crohn's disease with a mean age of 39 years (range 23-52 years) and a prevalence of female sex. None of these patients had history of thyroid dysfunction, radiation exposure, or a family history of thyroid cancer, although all underwent multiple computed tomographic and small bowel radiological studies during the course of their disease (6). The exposition to multiple radiological investigations, particularly in early adulthood, may thus predispose patients to papillary thyroid cancer (7).
Interestingly, the risk of papillary thyroid cancer is decreased in women with a high saltwater fish intake and increased in women with a high multivitamin supplement intake (8); multivitamin treatment is often recommended in Crohn's disease patients to prevent malnutrition (6). In Moss's series (6), 2 out of 5 patients with papillary thyroid carcinoma were taking multivitamin products when thyroid cancer was diagnosed.
We were unable to identify possible risk factors in our UC patient. Thyroid cancer has increased in many countries in the last 20 years, without any significant change in mortality. This has been partially related to changes in diagnostic procedures with an increased detection of small cancers. Indeed, often incidentally discovered micro-carcinomas (less than 10mm diameter) are now the most frequent form of thyroid cancer, representing about 40 % of cases. The prognosis is excellent. Unexpectedly, the proportion of large thyroid cancer at diagnosis has remained stable representing around 20 % of cases. These forms are responsible of most of the thyroid cancer specific mortality and an intensification of their clinical screening is necessary.
Systematic ultrasonographic population screening of thyroid nodules could increase the proportion of small thyroid cancers diagnosed, although the cost-benefit of such a strategy should be properly evaluated. UC patients have a low prevalence of thyroid diseases (9).
(Please cite as: Casella G, Antonelli E, Di Bella C, Villanacci V, Rostami Nejad M, Baldini V, et al. Papillary thyroid cancer and ulcerative colitis. Gastroenterol Hepatol Bed Bench 2013;6(1):52-54).
References
- 1.Ginsberg GG, Goodman ZD, Lewis JH. A 22- year old man with thyroid cancer and cholestatic liver disease. Sem Liver Dis. 1991;11:64–71. doi: 10.1055/s-2008-1040424. [DOI] [PubMed] [Google Scholar]
- 2.Evgenikos N, Stephen JG. Papillary thyroid carcinoma associated with ulcerative colitis. Postgrad Med J. 1996;72:621–22. doi: 10.1136/pgmj.72.852.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babb RR. Association between diseases of the thyroid and the liver. Am J Gastroenterol. 1984;79:421–23. [PubMed] [Google Scholar]
- 4.Penn I, Hammond W, Brettaschneider L, Stard TE. Malignant lymphoma in transplantation patient. Transpl Proceed. 1969;1:106–12. [PMC free article] [PubMed] [Google Scholar]
- 5.Fraser AG, Orchard TR, Robinson EM, Jewell DP. Long term risk of malignancy after treatment of inflammatory bowel disease with azathioprine. Aliment Pharmacol Ther. 2002;16:1225–32. doi: 10.1046/j.1365-2036.2002.01297.x. [DOI] [PubMed] [Google Scholar]
- 6.Moss AC, Brennan AM, Cheifetz AS, Peppercorn MA. Thyroid cancer and Crohn's disease: association or coincidence? Inflamm Bowel Dis. 2006;12:79. doi: 10.1097/01.mib.0000192324.20545.bd. [DOI] [PubMed] [Google Scholar]
- 7.Ron E, Lubin JH, Shore RE, Mabuchi K, Modan B, Pottern LM, et al. Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res. 1995;141:259–77. [PubMed] [Google Scholar]
- 8.Mack WJ, Preston-Martin S, Bernstein L, Qian D. Lifestyle and other risk factors for thyroid cancer in Los Angeles County females. Ann Epidemiol. 2002;12:395–401. doi: 10.1016/s1047-2797(01)00281-2. [DOI] [PubMed] [Google Scholar]
- 9.Casella G, De Marco E, Antonelli E, Daperno M, Baldini V, Signorini S, et al. The prevalence of hyper- and hypothyroidism in patients with ulcerative colitis. J Crohn's Colitis. 2008;2:327–30. doi: 10.1016/j.crohns.2008.09.001. [DOI] [PubMed] [Google Scholar]