Abstract
Inflammatory fibroid polyp (known also as Vanek's tumor) is a type of localized, non-neoplastic inflammatory pseudotumor or inflammatory myofibroblastic tumor that occurs most commonly in the stomach but also in the small and large bowel. It is a documented cause of intussusception in adults. We report a case of a 40-year-old woman who presented with severe, postprandial abdominal pain followed by projectile vomiting over a period of three days. Ultrasonography demonstrated a solid and echogenic mass surrounded by the typical mural layers of an invaginated jejunum. She underwent urgent laparotomy and resection of an 18 cm tumor from the distal jejunum. The immuno-histopathological diagnosis after segmental jejunal resection was a jejunal inflammatory fibroid polyp. Although inflammatory fibroid polyps are seen very rarely in adults, they are among the probable diagnoses that should be considered in obstructive tumors of the small bowel causing intussusceptions.
Keywords: Inflammatory lymphoid polyp, Small bowel, Intussusception, Case report
Introduction
Inflammatory fibroid polyp (IFP) is a rare, idiopathic pseudo-tumorous lesion of the gastrointestinal tract, first described by Vanek in 1949 as an eosinophilic submucosal granuloma (1).They typically present in the 5th to 7thdecade of life (2). The underlying cause of inflammatory fibroid polyps (IFPs) is still unknown. Many have suggested etiologies possibly related to chemical, physical, or metabolic triggers (3). When present, they are mostly found in the gastric antrum (70%) or in the ileum (20%); however, they are considered to be very rare in the duodenum and jejunum(2).
Symptoms depend on the location of the lesion, including abdominal pain, vomiting, altered small bowel movements, GI bleeding and loss of weight. IFPs arising below the Treitz ligament can present with an acute abdomen (obstructive ileus) usually due to intussusceptions (4, 5).
Here, we report an unusual case of jejenojejunal intussusception caused by an IFP, the diagnosis of which was confirmed by immunohistochemistry.
Case Report
A forty years old woman was admitted to the emergency unit suffering from progressive abdominal pain, nausea and vomiting for 3 days. She had no significant medical history or surgical intervention. For the past three days she had complaints of a dull postprandial cramping abdominal pain. The physical examination of abdomen revealed muscular guarding and rebound tenderness in the peri-umbilical region. Laboratory evaluation demonstrated a leukocytosis, with lymphocytosis and iron deficiency anemia. Primarily the plain abdominal radiography detected air fluid level (Figure 1).
Figure 1.
Plain abdominal radiography. Air fluid level is observed.
Abdominal ultrasonography prior to her admission revealed a mass in right lower quadrant with a pseudo-kidney pattern and suggested intussusceptions (Figure 2). Surgical consult was requested and the patient was planned for urgent laparotomy with a diagnosis of small bowel obstruction.
Figure 2.
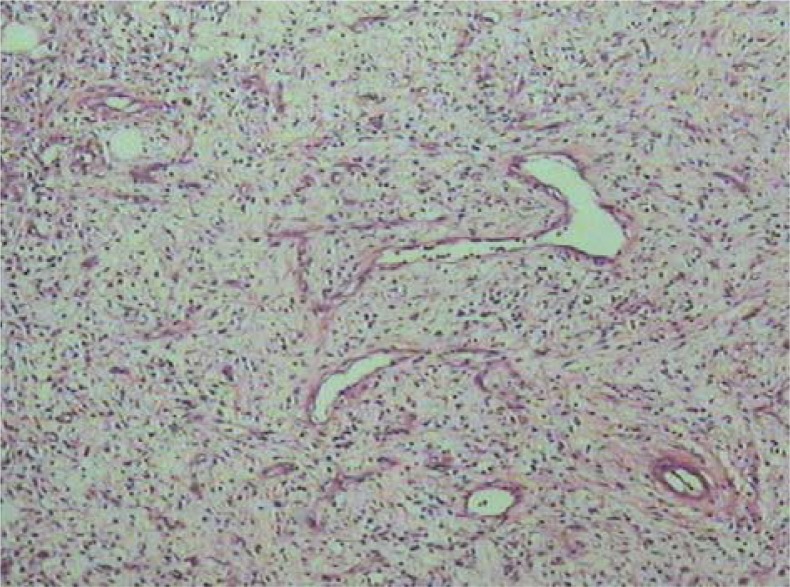
Histopathological finding showing ulcerative lesion with variable cellularity.
At the surgery a jejunal tumor causing jejuno-jejunal intussusceptions was found (Figure 3). The intussuscepted segment was resected and end-to-end anastomosis was carriedout. Post-surgical course was unremarkable and the patient was discharged after 7 days in a good condition.
Figure 3.
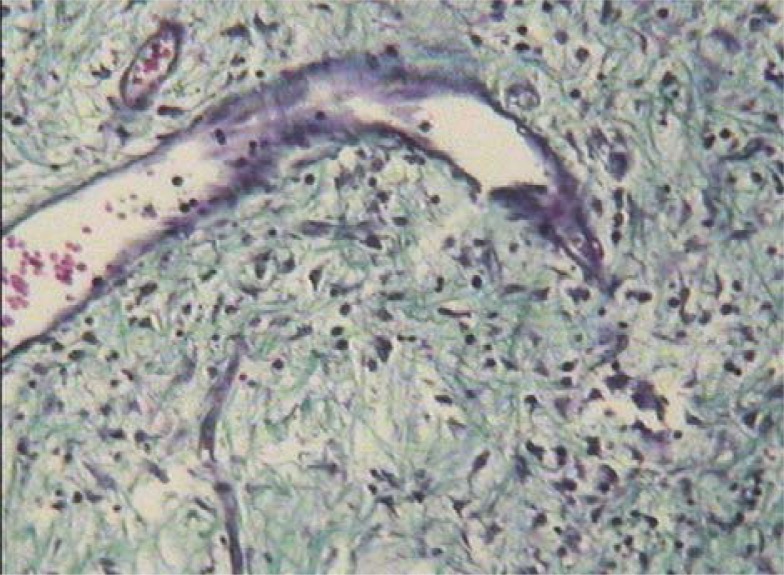
Blood vessels with thickened walls.
Postoperative macroscopic examination of the surgical specimen showed a firm 18×5×1cm mass, with foci of hemorrhage or grayish exudates and luminal surface that was composed of autolytic mucosa of thin nodularity and egg shaped mass. The lesion involved the entire thickness of the bowel wall with extensive ulceration of the overlying mucosa.
Histopathological analysis showed an ulcerative lesion with variable cellularity, formed by spindle cells with small number of mitosis and an abundant inflammatory infiltrate comprising mainly with eosinophils (Figure 2). Among the spindle cells blood vessels with thickened walls and vessel congestions at the sub mucosa and mucosa were observed (Figure 3).
The primary diagnoses were doubted between gastro-intestinal stromal tumor (GIST) and Vanek tumor. Immunohistochemical analysis was done on the specimen. The spindle cells were only positive for CD34. Histological hematoxylin-eosin (HE) stain sections revealed an inflammatory lymphoid polyp of the small bowel with active luminal surface ulcer which was covered with fibrino-purulent exudates.
The postoperative course was uneventful and the patient was discharged after 7 days. Six months after the surgery the patient was in no distress; she had some symptoms of bloating and mild change in her bowel movement. A thorough evaluation including complete laboratory examinations, upper endoscopy, colonoscopy with distal ileal evaluation and small bowel series were normal.
Discussion
IFPs are one of the least common benign small bowel tumors. They fall under the classification of sub mucosal connective tissue tumors and were first described by Vanek (1). They usually are discovered in the 5th to 7thdecade of life and can be found throughout the gastrointestinal (GI) tract but most commonly in the gastric antrum (70%) or ileum (20%), but rarely in the duodenum and jejunum (2). The underlying cause of inflammatory fibroid polyps (IFPs) is still unknown. Many have suggested etiologies possibly related to chemical, physical, or metabolic triggers (3).
Histologically they arise from the sub mucosa and are characterized by vascular and fibroblast proliferation and an inflammatory response, dominated by eosinophils (3). Further immuneohistochemical analysis can demonstrate variable reactivity for actin, CD34, desmin, CD117 and S100 (3). Most IFPs are polypoid masses smaller than 5 cm, but occasional reports of larger sizes up to 20 cm have been reported(6–8).In most patients, in whom IFPs are located in thes mall bowel, the clinical picture is characterized by symptoms and signs of obstructive ileus, usually due to the intussusception, and rapidly becomes a surgical emergency (5–9).
Patients with intussusceptions usually present with abdominal pain and nausea. Pre-operative diagnosis of intussusceptions is rare but can occur in finding a palpable mass on the abdomen or with the use of imaging techniques (10). The primary imaging modality of choice is ultrasound scanning, which enables the diagnosis or exclusion of intussusceptions with a sensitivity of 98 and 100%, respectively, a specificity of 88%, and a negative predictive value of 100% (11). In some cases abdominal CT scan has also been used as the primary diagnostic tool (8).
In the current case report, the patient presented with a dull, postprandial cramping abdominal pain. This case highlighted the importance of performing a thorough examination, even when patients present with unusual symptoms that are suspicious of functional pain. This case report demonstrates that intussusceptions, although rare in adults, should be considered in the differential diagnosis of abdominal pain. In this case, the preoperative clinical findings and ultrasonic images suggested invagination. The ultrasound images of the small bowel lumen showed a mass of 11 cm in diameter. Abdominal pain is the most common symptom, followed by vomiting and nausea (12). About 1000 IFPs have been described thus far in the literature, of which 70% were gastric in origin. Other GI sites affected (in decreasing order of frequency) were small bowel (mainly the ileum) (23%), colon and rectum (4%), gallbladder (1%), esophagus (1%), duodenum (1%), appendix (<1%) (13). An astonishing feature of the current case was the huge size of the tumor and its silent growth for eventually a couple of years without having any clinical presentation, until three days before the clinical presentation as an incomplete intestinal obstruction.
Causes of intestinal obstruction in adult patients include adhesion bands, malignant tumors and hernia in descending order of appearance. Here we showed that in some cases benign tumors even at large sizes can be a cause for small intestinal obstruction and hence should be included in the pre-operative diagnostic list.
In conclusion, the recommended treatment of adult intestinal invagination is surgical resection of the intestinal segments involved; which was performed in our case and this was curative with no longstanding complication.
(Please cite as: Neishaboori H, Maleki I, Emadian O. Jejunal intussusception caused by a huge Vanek’s tumor: a case report. Gastroenterol Hepatol Bed Bench 2013;6(4):210-213).
References
- 1.Vanek J. Gastric submucosal granuloma with eosinophilic infiltration. Am J path. 1949;25:397–411. [PMC free article] [PubMed] [Google Scholar]
- 2.Wysocki AP, Taylor G, Windsor JA. Inflammatory fibroid polyps of the duodenum: a review of the literature. Dig Surg. 2007;24:162–68. doi: 10.1159/000102099. [DOI] [PubMed] [Google Scholar]
- 3.Kolodziejczyk P, Yao T, Tsuneyoshi M. Inflammatory fibroid polyp of the stomach. A special reference to an immunohistochemical profile of 42 cases. Am J Surg path. 1993;17:1159–68. doi: 10.1097/00000478-199311000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Parasi A, Triantafillidis JK, Barbatzas C, Karakosta A, Condilis N, Sotiriou H. Coexistence of Crohn's disease and inflammatory fibroid polyp of the small bowel. Report of a case and review of the literature. Ann Ital Chir. 2005;76:395–99. [PubMed] [Google Scholar]
- 5.Zager JS, Shaw JP, Kaufman JP, DeNoto G. Three cases of small bowel intussusception in relation to a rare lesion: inflammatory fibrous polyps. Dig Surg. 2001;18:142–46. doi: 10.1159/000050116. [DOI] [PubMed] [Google Scholar]
- 6.Calabuig-Farinas S, Lopez-Guerrero JA, Ribera MJ, Navarro S, Ramos D, Pellin A, et al. Inflammatory fibroid polyp of the small bowel with a mutation in exon 12 of PDGFR alpha. Virchows Archiv. 2009;454:327–31. doi: 10.1007/s00428-008-0715-5. [DOI] [PubMed] [Google Scholar]
- 7.Daum O, Hes O, Vanecek T, Benes Z, Sima R, Zamecnik M, et al. Vanek's tumor (inflammatory fibroid polyp). Report of 18 cases and comparison with three cases of original Vanek's series. Ann Diag Path. 2003;7:337–47. doi: 10.1016/j.anndiagpath.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Rehman S, Gamie Z, Wilson TR, Coup A, Kaur G. Inflammatory fibroid polyp (Vanek's tumour), an unusual large polyp of the jejunum: a case report. Cases J. 2009;2:7152. doi: 10.1186/1757-1626-2-7152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paikos D, Moschos J, Tzilves D, Koulaouzidis A, Kouklakis G, Patakiouta F, et al. Inflammatory fibroid polyp or Vanek's tumour. Dig Surg. 2007;24:231–33. doi: 10.1159/000103326. [DOI] [PubMed] [Google Scholar]
- 10.Jabar MF, Prasannan S, Gul YA. Adult intussusception secondary to inflammatory polyps. Asian J Surg. 2005;28:58–61. doi: 10.1016/S1015-9584(09)60262-1. [DOI] [PubMed] [Google Scholar]
- 11.Sundaram B, Miller CN, Cohan RH, Schipper MJ, Francis IR. Can CT features be used to diagnose surgical adult bowel intussusceptions? AJR Am J Roentgenol. 2009;193:471–78. doi: 10.2214/AJR.08.1801. [DOI] [PubMed] [Google Scholar]
- 12.Yakan S, Caliskan C, Makay O, Denecli AG, Korkut MA. Intussusception in adults: clinical characteristics, diagnosis and operative strategies. World J Gastroenterol. 2009;15:1985–89. doi: 10.3748/wjg.15.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wysocki P, Taylor G, Windsor J. Inflammatory Fibroid polyps of the duodenum: a review of the literature. Dig Surg. 2007;24:162–68. doi: 10.1159/000102099. [DOI] [PubMed] [Google Scholar]