Abstract
Aim
The aim of this study was to describe our results and investigate the survival of below-18-year-old patients undergoing LRDLT and the factors affecting this.
Background
Living Related Donor Liver Transplantation (LRDLT) has become a good option to provide suitable grafts for children with liver diseases. Using this method, children who have no chance for life can live a much longer life.
Patients and methods
The present study is a historical cohort study carried on 191 patients below-18-year-sold who had undergone LRDLT for the first time in the Namazi hospital liver transplantation center. Survival rate of the patients was assessed using Kaplan-Meier method. The effect of factors related to the recipients, donors, and the transplantation process on the patients’ survival was also investigated.
Results
1, 3, 5 and 11-year survival of patients was 71%, 66%, 65%, and 65%, respectively. In the univariate analysis, age, weight at transplantation, PELD/MELD score, existence of post-transplant complications were found to be effective factors on the patients’ survival. In the multivariate analysis, weight at transplantation, PELD/MELD score, and existence of post-transplant complications were the prognostic variables.
Conclusion
LRDLT is now well established with satisfactory results in our center. Although the survival rate of the patients is lower than the survival rate reported in other studies, but the survival of the patients who had survived 1 month after the transplantation was comparable to other studies.
Keywords: Survival, Pediatrics, Living Donor, Liver Transplantation
Introduction
Liver transplantation is the standard treatment for the patients with end-stage liver diseases and is accompanied by high success rate in the patients who cannot be treated by any other method. Nowadays, liver transplantation is routinely performed around the world. Moreover, its success rate which is assessed as 1-year survival has improved from 30% during the 1970s to 90% today (1–5).
Overall, children comprise 15-20% of the patients in liver transplantation waiting list. However, because children below 5 years of age have the highest mortality rate in comparison to the other age groups and liver transplantation is the only acceptable standard treatment which can save them from dying; this group of patients is more important (6).
Despite the present techniques to overcome the shortage of size matched cadaveric liver donors, there is still a lack of organs (7). Pediatric patients were the first recipients of living related donor liver transplantations (LRDLT) for two reasons. First, relatives can be most easily selected as potential donors with few ethical problems, and second, donor safety can be more easily preserved by leaving the larger right lobe of the donor intact after harvesting the left side of the liver (8).
In Iran, the first LRDLT in children was performed in Namazi hospital, Shiraz in 1999 (9). Before 1999 nearly all children with end-stage liver disease died because of several complications. However, we have 12 years of experience with LRDLT among this group of patients. Although more than a decade has passed from performance of LRDLT in children in Iran, no studies have been conducted on the children's survival rate and its effective factors after LRDLT. In addition, this surgery is one of the expensive interventions for both the patients and the health system. The aim of this retrospective study was to describe our results and investigate the survival of below-18-year-old patients undergoing LRDLT and factors affecting their survival of 191 LRDLT performed between 1999 and 2011.
Patients and Methods
The present study was a survival analysis which was performed in the form of a historical cohort study. The study population included all the 191 below-18-year-old patients who had undergone LRDLT for the first time in Namazi hospital, Shiraz, Iran between April 1999 and March 2011. The patients’ information was collected from their records included the recipients’ characteristics, such as age, sex, weight at transplantation, blood group, initial diagnosis of liver disease, CHILD score, and PELD/MELD score, donors’ characteristics, including age, sex, and blood group, and the transplant features, including the year of transplant, existence of post-transplant complications, and length of hospital stay after the transplantation. The Child-Pugh score, MELD (Model for End Stage Liver Disease is used for candidates age 12 and older) and the PELD (Pediatric End Stage Liver Disease Model is used for patients age 11 and younger). All the above mentioned categories compose the three systems for prioritizing candidates waiting for liver transplants based on statistical formulas that are very accurate for predicting who needs a liver transplant most urgently.
In addition, the information about the patients’ follow up was completed through phone contact with their family. It should be mentioned that the starting point of the patients’ survival analysis was the time of performing the first LRDLT, while the end point was considered as the patients’ death.
The present study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran. Besides, informed consents for obtaining the information as well as the follow-up data were taken from all the participating patients or their families.
Descriptive results are presented through tables. The Kaplan-Meier method was used for estimating probability of patient survival. In this method, survival was computed based on different variables in univariate manner and compared between different categories of the variables using Log-Rank test.Then, the significant variables and those with p < 0.2 were entered into the Cox regression model.Proportional hazard assumption was assessed by drawing Log [-log (t)] on Log (t) graphs. All the statistical analysis was performed using the SPSS statistical software (v.19).
Results
Among the 191 transplanted patients, 118 ones (61.8%) were boys, while 73 patients (38.2%) were girls. Other characteristics of recipient, donor and transplant are presented in Table 1. The mean±SD of the patients’ age and weight at transplant was 5.58& +macr;4.5 years and 19.1±12.6 kg, respectively. The mean±SD of PELD/MELD scores and length of hospitalization was 20.5±8.3 and 16.8±9.3 days.
Table 1.
Recipient, donor and transplant characteristics
| variable | subgroup | No. (%) | |
|---|---|---|---|
| Recipient characteristic | Age groups | <1 years | 16(8.4) |
| 1-12 years | 154(80.6) | ||
| 12-18 years | 21(11) | ||
| Blood groups | A | 68(36) | |
| B | 47(24.9) | ||
| AB | 11(5.8) | ||
| O | 63(33/3) | ||
| Weight at transplant | above mean | 49(34.3) | |
| below mean | 94(65.7) | ||
| Primary diagnosis | Metabolic disorder | 76(39.8) | |
| Cholestatic disease | 81(42.4) | ||
| Hepatitis | 12(6.3) | ||
| Malignancy | 3(1.6) | ||
| Other | 19(9.9) | ||
| CHILD class | A | 35(25) | |
| B | 72(51.4) | ||
| C | 33(23.6) | ||
| MELD/PELD score | <20 | 33(44.6) | |
| ≥20 | 41(55.4) | ||
| Donor characteristics | Age groups | 18-28 years | 44(31.2) |
| 28-38 years | 76(53.9) | ||
| 38-48 years | 21(14.9) | ||
| Sex | male | 61(34.7) | |
| female | 115(65.3) | ||
| Blood groups | A | 11(18.6) | |
| B | 13(22) | ||
| AB | 2(3.4) | ||
| O | 33(55.9) | ||
| Transplant characteristic | Year of transplant | 1999-2003 | 5(2.6) |
| 2004-2007 | 37(19.4) | ||
| 2008-2011 | 147(78) | ||
| existence complication | Yes | 101(58) | |
| No | 73(42) |
Among the 191 patients under study, 130 ones (68.1%) survived and 61 patients (31.9%) died after the transplant because of early or late complications and rejection. It should be noted that 27 (47.4%) of the deaths occurred in the first month after the transplantation, and no deaths occurred among the patients who survived 5 years after the transplant.
The survival rates of all the patients and those who survived at least 1 and 3 months after the transplantation are presented in Table 2. As the table depicts, after excluding the patients who had died in the first and the third months after the transplantation, 1-year survival was obtained as 83% and 88%, respectively.
Table 2.
11-year survival of the below-18-year-old patients transplanted in Namazi hospital liver transplant center, and who had survived at least 1 and 3 months after the transplantation using Kaplan-meier method
| Cumulative survival (%) | |||||||
|---|---|---|---|---|---|---|---|
| category | 1-month | 3-month | 6-month | 1-year | 3-year | 5-year | 11-year |
| All patient | 85 | 80 | 75 | 71 | 66 | 65 | 65 |
| Patients who survived at least 1 month after the transplantation | 93 | 93 | 88 | 83 | 76 | 76 | 76 |
| Patients who survived at least 3 months after the transplantation | 94 | 94 | 91 | 88 | 81 | 81 | 81 |
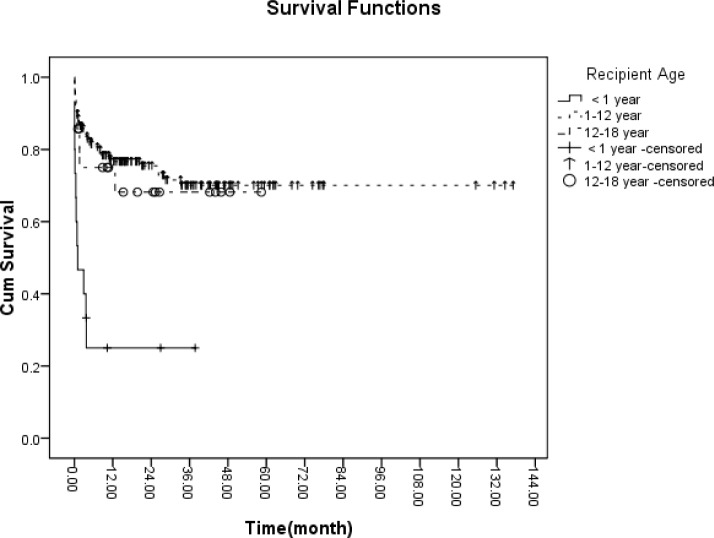
In the present study, the survival rate of below-one-year-old patients was lower than the other age groups (p < 0.001) (Figure 1).
Figure 1.
The 11-year survival curve of the below-18-year-old patients transplanted in Namazi hospital liver transplant center based on age group
Nevertheless, no significant difference was observed between the patients’ survival rates based on the recipient's sex, initial diagnosis of the liver disease, blood group, and CHILD category, donor's age, sex, blood group, year of transplant and length of hospital stay after the transplantation.
Moreover, the survival rate of the patients with weight below mean at transplant was lower than of the other group (p < 0.05).
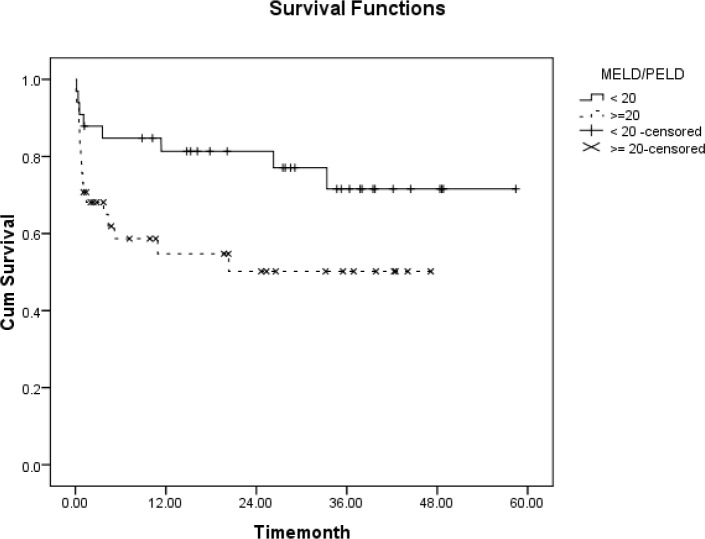
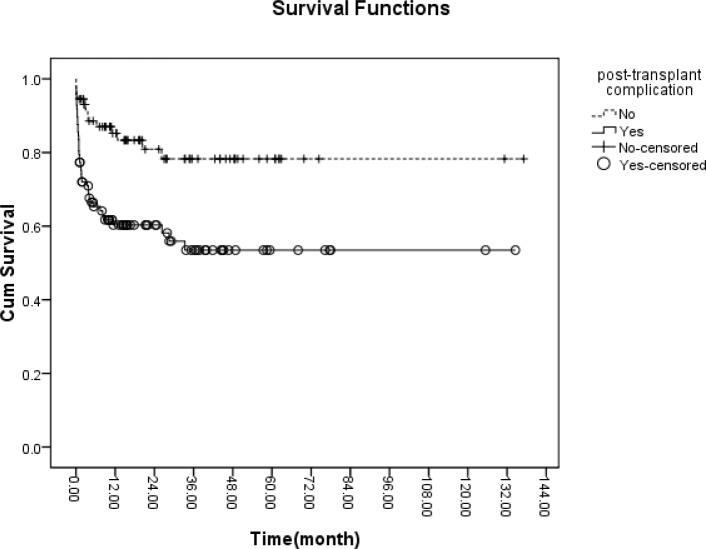
As shown in Figures 2 and 3, existence of post-transplant complications and PELD/MELD scores > 20 decreased the patients’ survival rate (p < 0.05).
Figure 2.
The 11-year survival curve of the below-18-year-old patients based on MELD/PELD
Figure 3.
The 11-year survival curve of the below-18-year-old based on post-transplant complication
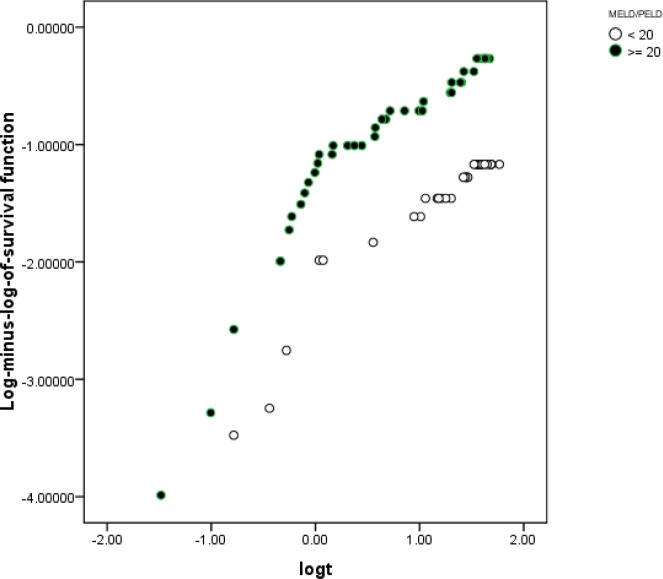
In order to assess the proportional hazard assumption, we plotted Log [-logS(t)] on Log (t) for all the significant variables. However, since all the graphs cannot be presented, the plot of log (-log(t)) on log(t) for the MELD/PELD are shown in Figure 4.
Figure 4.
Investigation of the of the proportional hazard assumption based on the MELD/PELD using the scatter plot of log(-log(S)) on log(t)
In order to model the effective factors in the survival rate, the variables with P < 0.2 and consistent hazard ratios in univariate analysis were entered into the Cox model. These variables included the recipient's age, the recipient's weight at transplantation, MELD/PELD score and existence of post-transplant complications. Then, Forward Likelihood ratio method was used in order to determine the final model and the results are presented in table 3. According to the results obtained from the Cox regression model, weight at transplantation, PELD/MELD score, and post-transplant complications were effective factors in the survival rate.
Table 3.
The results of multivariate analysis using the Cox regression model
| category | HR* | p | 95%CI for HR | |
|---|---|---|---|---|
| Lower | Upper | |||
| weight | ||||
| above mean | 1 | |||
| Below mean | 4.6 | 0.04 | 1.05 | 20 |
| PELD/MELD | ||||
| < 20 | 1 | |||
| ≥ 20 | 2.9 | 0.03 | 1.07 | 8.01 |
| Complication | ||||
| No | 1 | |||
| Yes | 3.9 | 0.01 | 1.3 | 11.5 |
Hazard Ratio
Discussion
LRDLT has become a good option to provide suitable grafts for children with liver diseases, mainly in developing countries, where cadaveric donation system are still limited (10). As surgical techniques and postoperative managements continue to advance, the outcomes of LRDLT have continued to improve (11). The LRDLT program at our center was initiated in 1999.Because of the scarcity of cadaveric donor, the number of LRDLTs increased in our transplant center. In the present study, 1-, 5-, and 11-year survival of the patients was 71%, 66%, and 65%, respectively, which is lower than the survival rate reported in other studies (8, 12–14). One reason for this difference is hospital mortality because the starting point of the patients’ survival analysis in our study was the time of performing the first LRDLT, while the starting point in other studies was varied and considered as the patients’ discharge from hospital so hospital mortality was not taken in consideration. Patient survival rates at 1 and 3 years after LRDLT in children in major studies are between 78% and 94% and 72% and 96%, respectively (8, 12–14).Considering the fact that 47.4% of all deaths had occurred in the first months after the transplantation, respectively, 1-, 5-, and 11-year survival of the patients who had survived 1 month after the transplantation was 83%, 76%, and 76%, respectively.
In the current study, among the variables which were assessed, only the recipient's age group, recipient's weight at transplantation, PELD/MELD score, and existence of post-transplant complications were related to the patients’ survival. In the same line, in the SPLIT study conducted in the U.S. and Canada, type of graft, and recipient's weight were considered as effective factors in the patients’ survival; such a way that the patients who had undergone transplantation with weight > 2 SD below mean had lower survival rates (15). Moreover, in comparison to other age groups, below-1-year-old children had the lowest survival rate, which is in agreement with other studies, including the one performed by Venick. However, this finding had no significant effect in the Cox model (16, 17)
The findings of the present study showed no significant relationship between the patients’ survival rate and CHILD categorization. Although this classification is widely used in predicting chronic liver failure (18), it has limitations for predicting the patients’ survival because only a 7-point difference is there between the minimum and maximum disease intensity based on its parameters (19). In this study also, since the patients’ CHILD categories were quite close, it showed no relationship with the patients’ survival. However, a significant relationship was found between the patients’ survival and PELD/MELD score as well as the existence of post-transplant complications.The pediatric end-stage liver disease model is a predictor of survival benefit and post transplant survival in pediatric liver transplant recipients for which a significant association was seen between survival and PELD at liver transplantation (15, 20). Biliary complications after LRDLT were the most common complications (8). Biliary complications are associated with increased hospitalization and decreased quality of life and also associated with survival (8, 15, 17).In this study, the patients’ survival rate did not show great changes 3 years after the transplantation and it remained constant after 5 years because in fact no deaths occurred since 5 years after the transplantation. This is consistent with the findings of other studies reporting the highest mortality rate of the patients in the first 90 days after the transplantation (21). Therefore, patient care in the first 3 months after transplantation is very important because most of the mortality occurs in this time. The higher mortality rate in the present study might be due to the limited healthcare facilities in our country as well as selection of more critically ill patients in our center. Although living donation has shown a real benefit due to the decreased waiting time, pediatric transplant groups are still faced with technical problems, including a higher incidence of biliary and vascular complications.
LRDLT is now well established with satisfactory results for both donors and recipients. The current organ shortage and the growth of waiting lists have inevitably had an impact on the provision of suitable grafts for children, leading to increased demand for living donation. In this study considering the fact that 47.4% of all deaths had occurred in the first months after the transplantation, 1-, 5-, and 11-year survival of the patients who had survived 1 month after the transplantation was 83%, 76%, and 76%, respectively, which is comparable to other studies.
Acknowledgements
The present article was extracted from the thesis written by Ms. Najmeh Haseli and was financially supported by Shiraz University of Medical Sciences (Grants No. 91-6132). Hereby, the authors would like to thank the personnel of Shiraz University of Medical Sciences and Namazi hospital Transplant Center for their cooperation in the study.
(Please cite as: Haseli N, Hassanzade J, Dehghani SM, Bahador A, Malek-Hosseini SA. living related donor liver transplantation in Iranian children: a 12- year experience. Gastroenterol Hepatol Bed Bench 2013;6(4):183-189).
References
- 1.Busuttil RW, Seu P, Millis JM, Olthoff KM, Hiatt JR, Milewicz A, et al. Liver transplantation in children. Ann Surg. 1991;213:48–57. doi: 10.1097/00000658-199101000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abramson O, Rosenthal P. Current status of pediatric liver transplantation. Clin Liver Dis. 2000;4:533–52. doi: 10.1016/s1089-3261(05)70125-2. [DOI] [PubMed] [Google Scholar]
- 3.Ghobrial RM, Farmer DG, Amersi F, Busuttil RW. Advances in pediatric liver and intestinal transplantation. Am J Surg. 2000;180:328–34. doi: 10.1016/s0002-9610(00)00550-x. [DOI] [PubMed] [Google Scholar]
- 4.Muiesan P, Vergani D, Mieli-Vergani G. Liver transplantation in children. J Hepatol. 2007;46:340–48. doi: 10.1016/j.jhep.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Polido WT, Lee KH, Tay KH, Wong SY, Singh R, Leong SO, et al. Adult living donor liver transplantation in Singapore: the Asian centre for liver diseases and transplantation experience. Ann Acad Med Singapore. 2007;36:623–30. [PubMed] [Google Scholar]
- 6.McDiarmid SV. Current status of liver transplantation in children. Pediatr Clin North Am. 2003;50:1335–74. doi: 10.1016/s0031-3955(03)00150-0. [DOI] [PubMed] [Google Scholar]
- 7.Kóbori L, Máthé Z, Fazakas J, Gerlei Z, Doros A, Fehervari I, et al. Surgical aspects of pediatric liver transplantation. Living donor liver transplant program in Hungary. Orv Hetil. 2008;149:1271–75. doi: 10.1556/OH.2008.28336. [DOI] [PubMed] [Google Scholar]
- 8.Tannuri AC, Gibbelli NE, Ricardi LR, Santos MM, Maksoud-filho JG, Pinho-Apezzato ML, et al. Living related donor liver transplantation in children. Transplant proc. 2011;43:161–64. doi: 10.1016/j.transproceed.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Dehghani SM, Gholami S, Bahador A, Nikeghbalian S, Salahi H, Imanieh MH, et al. Morbidity and mortality of children with chronic liver diseases who were listed for liver transplantation in Iran. Pediatr Transplant. 2007;11:21–23. doi: 10.1111/j.1399-3046.2006.00619.x. [DOI] [PubMed] [Google Scholar]
- 10.Bahador A, Salahi H, Nikeghbalian S, Dehghani SM, Dehghani M, Kakaei F, et al. pediatric liver transplantation in Iran: a 9-year experience. Transplant Proc. 2009;41:2864–67. doi: 10.1016/j.transproceed.2009.07.046. [DOI] [PubMed] [Google Scholar]
- 11.Li C, Mi K, Wen TF, Yan LN, Li B, Yang JY, et al. Outcomes of patients with benign liver diseases undergoing living donor versus deceased donor liver transplantation. PLoS ONE. 2011;6:e27366. doi: 10.1371/journal.pone.0027366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heaton N, Faraj W, Melendez HV, Jassem W, Muiesan P, Mieli-Vergani G. Living related liver transplantation in children. Br J Surg. 2008;95:919–24. doi: 10.1002/bjs.6060. [DOI] [PubMed] [Google Scholar]
- 13.Sieders E, Peeters PM, TenVergert EM, De Jong KP, Porte RJ, Zwaveling JH. Prognostic factors for long-term actual patient survival after orthotopic liver transplantation in children. Transplantation. 2000;70:1448–53. doi: 10.1097/00007890-200011270-00009. [DOI] [PubMed] [Google Scholar]
- 14.Austin MT, Feurer ID, Chari RS, Gorden DL, Wright JK, Pinson CW. Survival after pediatric liver transplantation: why does living donation offer an advantage? Arch Surg. 2005;140:465–70. doi: 10.1001/archsurg.140.5.465. [DOI] [PubMed] [Google Scholar]
- 15.SPLIT Research Group. Martin SR, Atkison P, Anand R, Lindblad AS. Studies of Pediatric Liver Transplantation 2002: patient and graft survival and rejection in pediatric recipients of a first liver transplant in the United States and Canada. Pediatr Transplant. 2004;8:273–83. doi: 10.1111/j.1399-3046.2004.00152.x. [DOI] [PubMed] [Google Scholar]
- 16.Baliga P, Alvarez S, Lindblad A, Zeng L. Posttransplant survival in pediatric fulminant hepatic failure: the SPLIT experience. Liver Transpl. 2004;10:1364–71. doi: 10.1002/lt.20252. [DOI] [PubMed] [Google Scholar]
- 17.Venick RS, Farmer DG, McDiarmid SV, Duffy JP, Gordon SA, Yersiz H, et al. Predictors of survival following liver transplantation in infants: a single-center analysis of more than 200 cases. Transplantation. 2010;89:600–605. doi: 10.1097/TP.0b013e3181c5cdc1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Christensen E, Schlichting P, Fauerholdt L, Gluud C, Andersen PK, Juhl E, et al. Prognostic value of Child-Turcotte criteria in medically treated cirrhosis. Hepatology. 1984;4:430–5. doi: 10.1002/hep.1840040313. [DOI] [PubMed] [Google Scholar]
- 19.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–70. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 20.Barshes NR, Lee TC, Udell IW, O'mahoney CA, Karpen SJ, Carter BA, et al. The pediatric end-stage liver disease (PELD) model as a predictor of survival benefit and posttransplant survival in pediatric liver transplant recipients. Liver Transpl. 2006;12:475–80. doi: 10.1002/lt.20703. [DOI] [PubMed] [Google Scholar]
- 21.Van der Meulen JH, Lewsey JD, Dawwas MF, Copley LP. Adult orthotopic liver transplantation in the United Kingdom and Ireland between 1994 and 2005. Transplantation. 2007;8:572–79. doi: 10.1097/01.tp.0000280540.76370.37. [DOI] [PubMed] [Google Scholar]