Abstract
Background
Coronary artery disease (CAD) is a major cause of death in India. Data on outcome of CAD is scarce in the Indian population. This study determined the characteristics, treatment and one-year outcomes of acute coronary syndrome (ACS) in an Indian Cardiac Centre.
Methods
We carried out a cross sectional retrospective analysis of 1468 ACS patients hospitalized between January 2008 and December 2010 and followed up for 1 year in the Institute of Cardiovascular Diseases, Madras Medical Mission, Chennai. Mortality at 1 year, its determinants and 1 year major adverse cardiac events (MACE) were determined.
Results
The patients were aged 62.2 ± 11.2 years; males (75.2%) and had ST segment elevation myocardial infarction (STEMI) (33.9%), non ST segment elevation myocardial infarction (44.2%) and unstable angina (21.9%). Key pharmacotherapy included aspirin (98.2%), clopidogrel (95.1%), statins (95.6%), angiotensin converting enzyme inhibitor/angiotensin receptor blocker (50.6%) and beta blocker (83.1%). Angiography rate was 80.6%. In the STEMI group, 53.3% had primary angioplasty, 20.3% were thrombolysed and 16.1% received sole medical therapy. Overall coronary artery bypass graft rate was 12.4%. At one year, all-cause mortality and composite MACE were 2.5% and 9.7%, respectively. MACE included death (2.5%), reinfarction (4.0%), resuscitated cardiac arrest (1.8%), stroke (1.1%) and bleeding (0.4%). Main factors associated with mortality were combined left ventricular systolic and diastolic dysfunction (OR = 20.0, 95% CI = 6.63–69.4) and positive troponin I (OR = 12.56, 95% CI = 1.78–25.23). Troponin I independently predicted mortality.
Conclusions
ACS population was older than previously described in India. Evidence-based pharmacotherapy and interventions, and outcomes were comparable to the developed nations.
Keywords: Acute coronary syndrome, Treatment, Outcomes
1. Introduction
It is projected that coronary artery disease (CAD) would rise in the developing nations by 120% and 137% in women and men, respectively by 2020.1 Of all the developing nations, India is undergoing the most rapid epidemiologic transition from communicable to non-communicable diseases and at the third stage of the transition characterized by high burden of atherothrombotic dominated non-communicable diseases.2 Coronary artery disease constitutes the largest contributor to cardiovascular disease burden in India. A review of cross sectional surveys in 2008 showed that 3–4% and 8–10% of rural and urban Indian dwellers, respectively, have CAD.3 This represented a 2-fold increase in rural and 6-fold increase in urban prevalence over a period of 40 years. In India CAD is the leading cause of death accounting for 1.46 million deaths which represented 14% of all-cause mortality in 2004.4 It is projected that by 2020 ischemic heart disease will result in 2.5 million deaths while daily adjusted life years (DALYs) lost due to CAD will rise to about 7.67–14.4 million in men and 5.6–7.7 million in women in India.3 Compared to the western world, CAD epidemiology in India is characterized by premature occurrence in the young and low/middle income group, high mortality and high prevalence of diabetes.5,6
Acute coronary syndrome (ACS) is a spectrum of diseases comprising unstable angina (UA), ST segment elevation myocardial infarction (STEMI) and non ST segment elevation myocardial (NSTEMI). It is the major cause of mortality in CAD and represents a principal form of its clinical presentation. The results of a multicentre ACS Registry in India (CREATE) demonstrated a 30 day mortality of 5.6%.6 The outcome of ACS may however be influenced by the level of health care or hospital setting. Furthermore, there is limited data on the intermediate and long-term outcomes of ACS in India. We determined the characteristics, treatment and one-year outcome of patients with ACS in the Institute of Cardiovascular Disease, Madras Medical Mission, a tertiary cardiac care centre in Chennai, India.
2. Methods
2.1. Study population
The study population consisted of consecutive ACS patients aged ≥18 years who were hospitalized and followed up for a minimum of 12 calendar months between 1st January 2008 and 31st December 2010 at the Institute of Cardiovascular Disease, Madras Medical Mission Chennai, India. The institute is a specialized cardiac centre with 21 bed coronary care unit (CCU), cardiac surgery facility and 2 state-of-the art cardiac catheterization laboratories performing high volume percutaneous coronary interventions (PCI). It provides 24 h service including 24 h on-the-spot consultant coverage in the CCU and cardiac laboratory.
2.2. Study protocol
The inclusion criteria included ACS defined using documented triad of characteristic ischemic symptoms, ECG changes and cardiac biomarker (troponin I) status.7 STEMI was defined as characteristic angina symptoms and ST segment elevation of ≥1 mm in at least 2 adjacent limb leads or ≥2 mm in at least 2 contiguous precordial leads and/or presumed new onset left bundle branch block (LBBB) on initial 12-lead ECG and troponin level greater than hospital cut-off point of 0.012 ug/L. NSTEMI was diagnosed if there were angina symptoms with ST segment depression ≥1 mm or T wave abnormalities and elevated troponin level above 0.012 ug/L. Unstable angina was defined as documented angina symptoms at rest with ST segment depression or T wave abnormalities without ST segment elevation or elevated troponin level (below 0.012 ug/L). Patients with ST segment elevation following coronary artery bypass graft (CABG) or PCI were excluded.
Standard structured questionnaire was utilized to collect data on demography including age, gender and nationality. Cardiovascular risk factors including alcohol consumption and smoking were recorded. Alcohol consumption greater than 40 drinks (males) or 30 drinks (females) per week was considered significant. Smoking of 10 or more cigarettes per day was considered significant. Type 2 diabetes was diagnosed as fasting blood glucose >126 mg/dL (7 mmol/L) or 2 h glucose level greater than (200 mg/dL) 11.1 mmol/L or history of diabetes and hypertension as history of hypertension/antihypertensive medication and/or blood pressure ≥140/90. Patients with high density lipoprotein cholesterol (HDL) level <40 mg/dl (men) or <50 mg/dl (women), and triglyceride level ≥150 mg/dl, serum total cholesterol >200 mg/dl or LDL cholesterol >130 mg/dl were considered to have dyslipidaemia. Information on family history of CAD was recorded.
The period from onset of symptoms to presentation in the hospital, baseline clinical characteristics and history of prior myocardial infarction (MI) or CABG or PCI were determined. Data on other laboratory investigations/procedures including renal biochemistry, left ventricular function, coronary angiography and ECG determined anatomical site of infarction in STEMI were collected. The treatment strategies including drug treatment, PCI and CABG as well as complications and outcomes were recorded.
All-cause mortality at 1 year as well as mortality at 7 days, 30 days, 6 months and 1 year major adverse cardiovascular events (MACE) including deaths, reinfarction, stroke, resuscitated cardiac arrest and major bleeding were determined. Myocardial reinfarction was defined as new troponin elevation with either new onset chest pain/discomfort or ECG changes consistent with infarction or both. Stroke was defined as focal neurological deficit of vascular origin lasting more than 24 h and confirmed by computed tomogram scan. Major bleeding was defined as a fall in hemoglobin of 5 g/dl or haemotocrit of 15% and cardiac arrest as resuscitated sustained ventricular tachycardia or ventricular fibrillation or asystole.
2.3. Statistical analysis
Data analysis was done using Statistical Package for Social Sciences software (SPSS Inc Chicago, Illinois version 17.0). Like most retrospective studies there was missing data. These were missing completely at random (MCAR) probably due to incomplete entry or loss of record. The analyses in which these data was involved were descriptive. We therefore handled the missing data using pairwise deletion.8 This was to ensure retention of the size of the study population, statistical power and representativeness of our results. Continuous variables were expressed as mean ± SD and compared using independent t-test (2-tailed). Discrete variables were presented as percentages (proportions) and compared using Chi square or Fisher's Exact test, as appropriate. We used univariate analysis to determine the effect of the following factors on one-year mortality: age, gender, ACS type (STEMI, NSTEMI and UA), risk factor, prior myocardial infarction, prior CABG, left ventricular function, number of diseased vessels, creatinine, ESR and leukocyte count. Factors that were significant predictors of outcome were used as independent variables in multiple logistic regression analysis aimed at determining the independent predictors of mortality (dependent variable). A p-value <0.05 was considered statistically significant.
3. Results
A total of 1504 patients with acute coronary syndrome (ACS) were admitted during the 3-year study period (2008–2010). Fifty six (3.7%) patients were lost to follow up and excluded from analysis. The remaining 1468 were made of STEMI (33.9%), NSTEMI (44.2%) and UA (21.9%) patients. Table 1 shows the general characteristics of the study population. The patients were aged 62.2 ± 11.2 years (range: 27–97 years, median 62 years). They were mostly (60.8%) in the 50–70 years age group and were predominantly males 1104 (75.2%) (Table 1). Compared to males, the females were older (64.1 ± 10.1 vs 61.5 ± 11.5 years; p < 0.0001). Dyslipidaemia (87.7%), hypertension (67.3%) and diabetes (58.6%) were the leading risk factors for CAD. Other risk factors included cigarette smoking (26.4%) and family history of CAD (12.0%). Low HDL cholesterol (80.7%) was the most frequent lipid abnormality. About 40.3% of patients had 3 or more risk factors for CAD. Males had a higher proportion of patients who were cigarette smokers than females (33.5% vs 1.4%, p < 0.0001). Compared to males, females had higher prevalence of hypertension (78.6 vs 65.2%; p < 0.0001) and diabetes (64.3 vs 56.6%; p = 0.01).
Table 1.
General characteristic of patients.
| Parameter | Male | Female | Total | p-value |
|---|---|---|---|---|
| No (%) | 1104 (75.2) | 364 (24.8) | 1468 (100) | |
| Age (years) | 61.5 ± 11.5 | 64.1 ± 10.1 | 62.2 ± 11.2 | <0.0001 |
| ≤50 years n (%) | 197 (17.8) | 33 (9.1) | 230 (15.7) | <0.0001 |
| 51–60 years n (%) | 328 (29.7) | 104 (28.6) | 432 (29.4) | 0.07 |
| 70–70 years n (%) | 332 (30.1) | 128 (35.1) | 460 (31.3) | 0.07 |
| >70 years n (%) | 247 (22.4) | 99 (27.2) | 346 (23.6) | 0.06 |
| STEMI n (%) | 412 (37.3) | 86 (24.5) | 498 (33.9) | <0.0001 |
| NSTEMI n (%) | 476 (43.1) | 172 (47.5) | 648 (44.2) | 0.01 |
| U Angina n (%) | 216 (19.6) | 106 (29.0) | 322 (21.9) | <0.0001 |
| Hypertension n (%) | 705/1081 (65.2) | 283/360 (78.6) | 988/1441 (68.6) | <0.0001 |
| Dyslipidaemia n (%) | 715/803 (89.0) | 217260 (83.4) | 932/1063 (87.7) | 0.01 |
| Diabetes n (%) | 605/1068 (56.6) | 228/356 (64.3) | 834/1424 (58.6) | 0.01 |
| Smoking n (%) | 350/1046 (33.5) | 4/295 (1.4) | 354/1341 (26.4) | <0.0001 |
| F History n (%) | 123/912 (13.4) | 23/295 (7.8) | 146/1207 (12.0) | 0.01 |
| Alcohol consumption n (%) | 162/933 (17.4) | 4/278 (1.1) | 166/1211 (13.7) | <0.0001 |
| RF ≥3 n (%) | 432/1082 (33.9) | 149/359 (41.5) | 581/1441 (40.3) | 0.6 |
| Prior MI n (%) | 329/980 (33.6) | 92/321 (28.7) | 421/1301 (32.4) | 0.10 |
| CAG n (%) | 853/1052 (81) | 254/339 (74.9) | 1107/1373 (80.6) | 0.01 |
| MVD n (%) | 465/770 (60.4) | 131/220 (59.6) | 596/990 (60.2) | 0.06 |
CAG: Coronary angiography. F: Family. MVD: Multiple vessel disease. RF: Risk factors.
In the STEMI group, 120 (75.9%) patients presented in Killip Class I. The anatomical sites of infarction (Fig. 1) were mainly the anterior (61.2%) and inferior (36.2%) walls. Males were more likely to have STEMI (82.7 vs 71.4%, p < 0.0001) while females were more likely to have NSTEMI/UA (28.6 vs 17.3%, p < 0.0001) (Table 2). Compared to NSTEMI/UA, patients with STEMI were significantly younger (60.4 ± 10.5 vs 63.0 ± 11.5 years, p < 0.0001), had higher heart rate (84.2 ± 18.9 vs 81.3 ± 18.2 beat per minute), lower systolic blood pressure (131.6 ± 25.1 vs 138.7 ± 26.5 mmHg p < 0.0001) and lower left ventricular systolic ejection fraction (41.0 ± 9.2 vs 45.0 ± 14.2, Table 2).
Fig. 1.
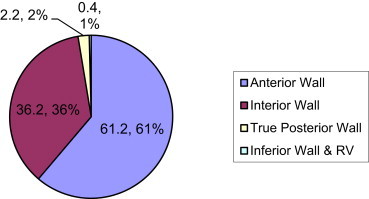
Anatomical sites of infarction.
Table 2.
Comparison of patients with STEMI and NSTEMI/UA.
| Parameter | STEMI | NSTEMI/UA | Total | p-value |
|---|---|---|---|---|
| No (%) | 498 (33.9) | 970 (66.1) | 1468 (100) | |
| Age (years) | 60.4 ± 10.5 | 63.0 ± 11.5 | 62.2 ± 11.2 | <0.0001 |
| Age >70 years n (%) | 84 (16.9) | 262 (27.0) | 346 (23.6) | <0.0001 |
| Male n (%) | 412 (82.7) | 692 (71.3) | 1104 (75.2) | <0.0001 |
| Female n (%) | 86 (17.3) | 278 (28.7) | 364 (24.8) | <0.0001 |
| RF ≥3 (%) | 232/489 (47.4) | 349/952 (36.7) | 581/1441 (40.3) | 0.01 |
| HTN duration (years) | 6.9 ± 5.9 | 8.3 ± 7.3 | 7.8 ± 6.9 | 0.01 |
| SBP (mmHg) | 131.6 ± 25.1 | 138.7 ± 26.5 | 136.3 ± 26.3 | <0.0001 |
| H Rate (bpm) | 84.2 ± 18.9 | 81.3 ± 18.2 | 82.3 ± 18.5 | 0.01 |
| LV EF (%) | 41.0 ± 9.2 | 45.0 ± 14.2 | 43.6 ± 12.7 | <0.0001 |
| SVD (%) | 169/368 (45.9) | 226/623 (36.3) | 395/991 (39.6) | 0.002 |
| CAG (%) | 404/479 (84.3) | 703/912 (77.1) | 1107/1391 (79.6) | 0.001 |
| PCI (%) | 225/422 (53.3) | 292/802 (36.4) | 517/1224 (42.2) | <0.0003 |
| Frq of hospitalization | 1.2 ± 0.5 | 1.3 ± 0.7 | 1.2 ± 0.6 | <0.0001 |
CAG: Coronary angiography. Freq: Frequency. H: Heart. HTN: Hypertension. LVEF: Left ventricular ejection fraction. Multiple vessel disease. PCI: Percutaneous coronary intervention. RF: Risk factors. SBP: Systolic blood pressure. SVD: Single vessel disease.
Coronary angiography (CAG) was performed in 80.6% of patients. The angiography rate was significantly higher in the STEMI than NSTEMI/UA group (84.3 vs 77.1%, p = 0.0001) (Table 2). Patients who had CAG were significantly younger (61.1 ± 10.5 vs 65.9 ± 12.9; p < 0.0001). Specific diseased vessels included the left anterior descending artery (77.4%), right coronary artery (58.6%), left circumflex (50.3%), left main coronary artery (12.6%) and others (5.2%) (Fig. 2). Single, double and triple vessel diseases were observed in 39.5%, 29.1% and 30.5% of patients, respectively. Nine (0.9%) patients had normal epicardial coronary arteries (Fig. 3). Single vessel disease was more frequent in the STEMI group (45.9 vs 36.3%; p < 0.01) while multiple vessel involvement, though higher in NSTEMI/UA, did not differ significantly between the two groups.
Fig. 2.
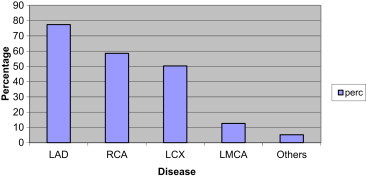
Pattern of coronary artery lesion. LAD: Left anterior descending artery. LCX: Left circumflex artery. LMCA: Left main coronary artery. RCA: Right coronary artery. Perc: Percentage.
Fig. 3.
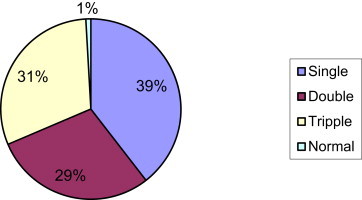
Grouping of coronary vessel lesion.
The rates of use of evidence-based pharmacotherapy and interventions are shown in Table 3. Aspirin, clopidogrel and lipid modifying drugs were used in 98.2%, 95.1% and 94.2% of patients, respectively. Other evidence-based drugs that were used included beta blockers (83.1%), angiotensin converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB) 50.6% and calcium channel blockers (CCB) (11.9%). Overall, 96.4% of patients had at least one or combinations of ACEI/ARB and BB (Table 3). Anticoagulant medication was used in 33.8% of patients, and this was predominantly (92.4%) low molecular weight heparin. Of the 384 referred patients with information on antiplatelet therapy, 193 (50.2%) had pre-referral antiplatelet treatment including aspirin (46.6%) and clopidogrel (45.8%).
Table 3.
Treatment and intervention.
| Drug treatment | Total no of patients | Patients treated n (%) |
|---|---|---|
| Acetyl salicylic acid (Aspirin) | 1468 | 1441 (98.2) |
| Clopidogrel | 1468 | 1396 (95.1) |
| Lipid lowering drugs | 1453 | 1383 (95.2) |
| ACEI or ARB | 1245 | 630 (50.6) |
| Beta blocker (BB) | 1245 | 1035 (83.1) |
| ACEI or ARB or BB | 1245 | 1199 (96.3) |
| Calcium channel blocker (CCB) | 1245 | 148 (11.9) |
| Anticoagulant use | 1468 | 624 (42.5) |
| LMWH | 1468 | 459 (31.3) |
| Unfractionated heparin | 1468 | 165 (11.2) |
| Thrombolysis | 498 | 101 (20.3) |
| PCI | 1223 | 515 (42.1) |
| CABG | 1223 | 152 (12.4) |
ACEI: Angiotensin converting enzyme inhibitor. ARB: Angiotensin receptor blocker. BB: Beta blocker. CABG: Coronary artery bypass graft. CCB: Calcium channel blocker. LMWH: Low molecular weight heparin. PCI: Percutaneous coronary intervention.
The time from onset of symptoms to presentation ranged from 5 min to 120 h (median 5 h, mode 24 h) in patients with STEMI 53.3%. In the STEMI group, 20.3% of patients were thrombolysed predominantly using streptokinase (94.0%), while 53.3% and 10.3% had primary PCI and CABG, respectively. Sole medical therapy was used in only 16.1% of STEMI patients. Overall, PCI was performed in 517 (42.2%) of 1224 patients, and 152 (12.4%) of 1223 patients had coronary artery bypass surgery (CABG). Patients who had CABG were significantly older than those who had PCI (62.5 ± 9.4 vs 59.6 ± 11.0, p = 0.003). Though males were more likely to have CAG than females (81.1% vs 74.7%; p = 0.01), there was statistically no significant gender difference in the rate of interventions: PCI (male 36.5%; female 30.5%, p = 0.06) and CABG (male 12.9%; female 10.0%, p = 0.17). Arrhythmias (3.7%), resuscitated cardiac arrest (1.8%) and intracardiac thrombus (1.5%) were the leading complications (Table 4).
Table 4.
Complications.
| Complications | No (%) |
|---|---|
| Arrhythmia | 42/1130 (3.7) |
| Resuscitated cardiac arrest | 26/1468 (1.8) |
| Intracardiac thrombus | 18/1182 (1.5) |
| Stroke | 16/1468 (1.1) |
| Ventricular aneurysm | 14/1468 (1.0) |
| Cardiogenic shock | 13/1468 (0.9) |
| Chordae rupture | 6/1468 (0.5) |
| Major bleeding | 5/1171 (0.4) |
| Ventricular septal rupture | 2/1468 (0.1) |
| Free wall rupture | 1/1140 (0.01) |
There were 37 (2.5%) deaths at 1 year of follow up Mortality rates at 7 days, 30 days, 6 months and 1 year were 0.4%, 0.7%, 2.0% and 2.5%, respectively. Mortality was fairly evenly spread during the first and second halves of the 1 year following ACS in the STEMI compared to NSTEMI/UA group (41.7% vs 58.3%) while deaths occurred predominantly during the second half of the year in the NSTEMI/UA patients (80% vs 20%). Mortality increased though at statistically insignificant levels with increasing age group: [11/662 (1.7%), 13/459 (2.8%) and 13/346 (3.8%); p = 0.10] in patients aged ≤60 years, 61–70 years and >70 years, respectively. Mortality increased at statistically significant level across increasing gradient of risk stratification: [low risk 3/761 (0.4%), intermediate risk 8/444 (1.8%) and high risk 19/174 (10.9%); p < 0.0001]. At 1 year of follow up 59/1463 (4.0%), 26/1468 (1.8%), 16/1468 (1.1%), and 5/1171 (0.4%) patients had reinfarction, resuscitated cardiac arrest and major bleeding, respectively. Composite major adverse cardiac event (deaths, myocardial infarction, stroke, cardiac arrest and bleeding) at 1 year was 9.7%.
The deceased and survivors at 1 year are compared in Table 5. Compared to the survivors the deceased were older (66.8 ± 10.7 vs 62.0 ± 11.2 years; p = 0.01) and had higher serum creatinine level (1.9 ± 1.7 vs 1.1 ± 1.6 mg/dl, p < 0.01) and higher frequency of hospital admissions (2.7 ± 2.0 vs 1.2 ± 0.5). The deceased also had higher proportion of patients with troponin positive I status (96.0 vs 65.7%, p < 0.0001), TIMI Risk Factors ≥3 (36.1 vs 20.8%, p = 0.02), and high risk class (60.6 vs 14.4%), severe LV dysfunction (18.9 vs 6.6%, p = 0.003), CABG (25.0 vs 2.1%) and ≥3 CAD risk factors (64.7 vs 39.7%, p = 0.003). The mean duration of first hospital admission was 5.5 ± 7.2 days (median 4 days). It did not differ among the deceased and survivors. Frequency of hospitalization ranged from 1 to 13 and was higher among NSTEMI/UA than STEMI patients (1.3 ± 0.7 vs 1.2 ± 0.5, p < 0.0001) and higher among the deceased compared to survivors at 1 year (2.6 ± 2.0 vs 1.2 ± 0.5, p < 0.0001).
Table 5.
Univariate comparison of deceased and survivors of ACS at 1-year post event.
| Parameter | Deceased | Survivors | Total | p-value |
|---|---|---|---|---|
| No (%) | 37 (2.5) | 1431 (97.5) | 1468 (100) | |
| Age (years) | 66.8 ± 10.7 | 62.0 ± 11.2 | 62.2 ± 11.2 | 0.01 |
| Age >70 years | 13 (35.1) | 333 (23.4) | 805 (54.8) | 0.09 |
| Male n (%) | 30 (81.1) | 1074 (75.1) | 1104 (75.1) | 0.40 |
| STEMI | 12 (32.4) | 486 (34.0) | 498 (33.9) | 0.85 |
| NSTEMI/UA | 25 (67.6) | 945 (66.0) | 970 (66.1) | 0.85 |
| Troponin I +ve (%) | 24/25 (96.0) | 258/393 (65.7) | 282/418 (67.5) | 0.002 |
| Previous MI (%) | 15/36 (41.7) | 406/1265 (32.1) | 421/1301 (32.4) | 0.23 |
| CABG n (%) | 9/36 (25.0) | 143/1179 (12.2) | 152/1215 (12.5) | 0.02 |
| Serum Cr (mg/dl) | 1.9 ± 1.7 | 1.1 ± 1.6 | 1.2 ± 4.0 | 0.01 |
| Severe LVSD n (%) | 7/37 (18.9) | 85/1286 (6.6) | 92/1323 (7.0) | 0.003 |
| Both LVSD & LVDD n (%) | 25/29 (86.2) | 246/1045 (23.5) | 271/1070 (25.3) | <0.0001 |
| Risk factor ≥3 (%) | 22/34 (64.7) | 558/1407 (39.7) | 580/1441 (40.2) | <0.003 |
| Frq hospitalized | 2.7 ± 2.0 | 1.2 ± 0.5 | 1.2 ± 0.6 | <0.0001 |
| TIMI RF ≥3 (%) | 12/33 (36.4) | 288/1105 (20.8) | 300/1138 (26.4) | <0.02 |
| High risk | 20/33 (60.6) | 174/1379 (14.4) | 194/1412 (13.7) | <0.0001 |
CABG: Coronary artery bypass graft. Frq: Frequency. LVSD: Left ventricular systolic dysfunction. LVDD: Left ventricular diastolic dysfunction. TIMI RF: Thrombolysis in myocardial infarction risk factors.
On univariate analysis factors associated with mortality (Table 6) included concomitant severe left ventricular systolic and diastolic dysfunction (OR = 20.0, 95% CI = 6.63–69.4); troponin I positive status (OR = 12.56, 95% CI = 1.78–25.23); high risk class (OR = 11.96, 95% CI = 5.31–27.34); severe left ventricular dysfunction (OR = 3.0, 95% CI = 1.28–8.15); CAD risk factors ≥3 (OR = 2.79, 95% CI = 1.31–6.03); CABG (OR = 2.41, 95% CI = 1.28–5.5); TIMI risk factors ≥3 (OR = 2.19, 95% CI = 1.0–4.73). Multiple logistic regression analysis involving age, gender, risk class, CAD and TIMI risk factors ≥3 each showed that only positive troponin status independently predicted mortality (p = 0.002).
Table 6.
Factors associated with mortality.
| Factors | Odd ratio | 95% CI | p-value |
|---|---|---|---|
| Both LVSD & LVDD | 20.0 | 6.63–69.40 | <0.0001 |
| Troponin +ve status | 12.56 | 1.78–25.13 | 0.002 |
| High risk class | 10.65 | 4.95–23.13 | 0.001 |
| Severe LVSD | 3.0 | 1.28–8.15 | 0.03 |
| Risk factor ≥3 | 2.79 | 1.31–6.03 | 0.003 |
| CABG | 2.41 | 1.28–5.50 | 0.02 |
| Diabetes | 2.24 | 1.0–5.15 | 0.03 |
| TIMI RF ≥3 | 2.19 | 1.0–4.73 | 0.02 |
CABG: Coronary artery bypass graft. Frq: Frequency. LVSD: Left ventricular systolic dysfunction. LVDD: Left ventricular diastolic dysfunction. TIMI RF: Thrombolysis in myocardial infarction risk factors.
During the study period (2008–2009), there were trends (Fig. 4) towards increasing annual rates of admission for ACS, coronary angiography, PCI, and use of ACEI inhibitors/ARB and beta blockers. Mortality and CABG rates fell over the same period (Fig. 4).
Fig. 4.
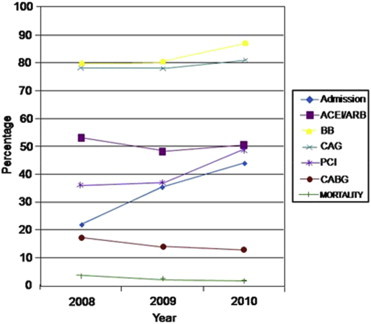
Trends in interventions and mortality. ACEI: Angiotensin converting enzyme inhibitor. ARB: Angiotensin receptor blocker. BB: Beta blocker. CAG: Coronary angiogram; CABG: Coronary arteries bypass graft. PCI: Percutaneous coronary intervention.
4. Discussion
This study provides information on descriptive epidemiology, practice patterns and outcomes of patients with ACS in a specialized cardiac centre in India. We observed similar demographic and CAD risk profiles to the previous reports from Indian and some other developing nations.5,6,9–11 However, our patients were relatively older and had higher prevalence of diabetes, dyslipidaemia and prior myocardial infarction (MI). The proportion of patients over 70 years of age in the current report, for example, almost doubles that in the CREATE Registry in India.6 Our patients were nonetheless younger than the Caucasian ACS population.12 Although the relatively higher age of the current study population may be incidental, it could be a reflection of an epidemiological evolution in the demography of Indian CAD patients. This trend has been described in the Caucasians. The average age of ACS patients, for example, increased over a 17-year period from 58.4 to 63.4 years in Montreal Heart Institute.13 As in previous reports,6,9,10 women were older and had higher rates of hypertension and diabetes mellitus, and lower rate of cigarette smoking than men.
The proportion of patients with STEMI in the current study is lower than the values previously reported in India6,9 but about 35% was observed in the Europeans.12 Recent data from other developing nations10,11 similarly showed STEMI rates lower than reported in the CREATE study. As acknowledged in the CREATE report,6 a sizable proportion of patients had no cardiac enzyme test and this might have influenced patients' categorization. Compared to NSTEMI/UA, our STEMI patients, like in previous reports from India and other developing nations,6,7,9–11 were younger and more likely to be males.
Key pharmacotherapy, particularly, antiplatelet treatment that included clopidogrel was used at a rate quite higher than many previous reports from India and comparable to the developed nations. About half of the referred patients had dual antiplatelet therapy prior to referral. This suggests an increasing awareness of current evidence-based guidelines in the management of ACS among Indian general physicians. Though only half of our patients received ACEI or ARB, the use of BB was very high, and almost all patients received either BB or ACEI/ARB or both. The rate of reperfusion therapy was higher in the current than previous reports from India.6,9 In the STEMI group, for example, almost 75% of patients had either primary PCI or thrombolysis, and only 16.1% had sole medical therapy. The remaining STEMI patients had surgical reperfusion. Though second generation fibrinolytic therapy including tenecteplase and reteplase has been shown to improve outcomes in STEMI patients, streptokinase remains the predominantly used thrombolytic agent in India probably because of financial constraint.
Coronary angiography rate was higher than previously reported in India6,9 and comparable with the findings in the developed nations.12 The PCI rate was also higher than previously reported in India. Patients' choice of treatment strategy, disease severity, financial difficulties and old age might have influenced PCI rate in the current report. Patients who had PCI were, for example, significantly younger than those who had only medical treatment. Though coronary angiography rate was higher in males than females, there were no gender differences in the rates of PCI and CABG. This is similar to some previous reports14 but contrasts other reports that suggested women with ACS are less aggressively managed.15
The 1-year mortality rate observed in the current report is lower than the values in most multicentre Registries.6,10–12 It is however comparable to the findings in some single centre- based studies.13,16 The influence of hospital setting on the outcomes of ACS has been suggested. In the AMIS Registry,17 hospital categorized as grade A which is characterized by 24 h coronary care unit, cardiac catheterization and cardiac surgery services had lower mortality than category B hospitals where these services were not obtainable or obtainable to the same extent (2.8 vs 4.0%). Similarly, annual mortality rate was reported to have dropped over the years to as low as 1.5% in Montreal Heart Institute, a specialized cardiac centre.13 This was attributed to maximal utilization of available resources and best practices including adherence to evidenced based guidelines with proven benefits. These observations might have partly informed the emerging advocates of designated specialized cardiac centres for the care of ACS patients.
Though it has been consistently believed that Indians with ACS have higher mortality than the whites,2,6 a recent meta-analysis of 4 recently published studies showed that the prognosis of manifestation of CAD in South Asian people is not worse than Whites, and the increased coronary mortality rates in the former are due to the higher incidence of fatal and non-fatal CAD.18 Another recent comparison of a South Asian STEMI population with the Europeans showed that though the Asian STEMI patients were younger and more likely to be diabetic, the survival at discharge was similar compared to Europeans.19 It is nonetheless probable that the low mortality rate in the current report may be because our study population belonged predominantly to low/intermediate risk group with generally low rates of severe complications. Mortality rate was, for example, high in the high-risk group.
The clinical determinants of mortality in the current report are largely similar to the findings in previous studies.11,19–22 Only cardiac troponin I passed as an independent predictor of mortality. The prognostic role of this cardiac biomarker has been previously documented.21 We observed higher serum creatinine among the deceased compared to the survivors. This is similar to the findings in the GRACE study where creatinine clearance was an important predictor of mortality.22 In the current report, gender did not influence 1-year mortality. This is similar to some of the previous reports23 but at variance with some others.24 It was recently observed that mortality rates are higher among young women with ACS, but this difference tends to disappear with aging, and long term prognosis is similar or even better among older women.25 The prevalence of metabolic syndrome was not investigated in the current report. We however observed clustering of cardiovascular risk factors in about 40% of our patients. This is similar to the reported 45% prevalence rate of metabolic syndrome in ACS patients,26 and like metabolic syndrome, clustering of CAD risk factors adversely affected the outcome of ACS in the current report.
During the 3 years study period we observed a trend towards increasing rates of admission for ACS, interventions and use of key pharmacotherapy, and a fall in mortality. A minimal fall in surgical revascularization was also demonstrated. Some of these observations are similar to the findings in Montreal Heart Institute though the rate of surgical revascularization was stable during the period of study in this institute.13 Our findings need to be confirmed in a study over a longer period as 3 years is insufficient to determine temporal changes. They nonetheless probably indicate that the CAD epidemic is still on-going in India, and that there is increased awareness of the disease among the populace and improved compliance with evidence-based treatment guidelines among the physicians.
This study is not without limitations. Out-of-hospital events were not captured. However, the lost to follow up rate was low (3.7%) making its effect on overall outcome being probably minimal. As expected in all retrospective studies, there was missing data. Being a single center and hospital-based experience, our results cannot be generalized. It however illustrates the potential favorable outcome of ACS in a tertiary cardiac care setting.
In conclusion, our data demonstrated ACS patient population that is relatively older than previously described in India. Evidence-based pharmacotherapy and interventions as well as outcomes were favorably comparable to the data from developed nations. Trends towards increasing admission rate for ACS, utilization of therapeutic advances and fall in mortality were observed.
Conflicts of interest
All authors have none to declare.
Acknowledgment
We thank the departmental staff of Clinical Research, Medical Record and Electronic Processing Data of Institute of Cardiovascular Disease, Madras Medical Mission Chennai; and the senior medical students and junior registrars of the Department of Medicine, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria for their assistance in data collection and entry.
References
- 1.Murray C.J.L., Lopez A.D. Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet. 1997;349:291–300. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Gupta R., Joshi P., Mohan V. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 3.Ghaffar A., Reddy K.S., Singhi M. Burden of non-communicable disease in South Asia. BMJ. 2004;328:807–810. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R. Burden of coronary artery disease in India. Heart. 2005;57:632–638. [PubMed] [Google Scholar]
- 5.Yusuf S., Hawken S., Ounpuu S., INTERHEART study of Investigators Effect of potentially modifiable risk factors associated with myocardial myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 6.Xavier D., Pais P.P., Devereaux P.J., on behalf of the CREATE registry investigators Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 7.Kim M., Kini A., Fuster V. Definitions of acute coronary syndromes. In: Fuster V., Alexander R.W., O’Rourke R.A., editors. Hurst's Heart. 12th ed. McGraw Hill; New York, NY: 2008. pp. 1319–2511. [Google Scholar]
- 8.Tsikriktsis Nikos. A review of techniques for treating missing data in OM survey research. J Oper Management. 2005;24:53–62. [Google Scholar]
- 9.Misiriya K.J.R., Sudhayakumar N., Abdul Khadar S., Raju G., Jayaprakash V.L., Pappachan J.M. The clinical spectrum of acute coronary syndromes: experience from a major center in Kerala. J Phys Assoc India. 2009;57 [PubMed] [Google Scholar]
- 10.Schamroth Colin. Management of acute coronary syndrome in South Africa: insights from the ACCESS (Acute Coronary Events – a multinational survey of current management strategies) registry. Cardiovasc J Afr. 2012;23 doi: 10.5830/CVJA-2012-017. Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Awad H.H., Zubaid M., Alsheikh-Ali A.A., Al Suwaidi J., Anderson F.A., Jr., Gore J.M. Comparison of characteristics, management practices, and outcomes of patients between the global registry and the Gulf Registry of Acute Coronary Events. Am J Cardiol. 2011;108:1252–1258. doi: 10.1016/j.amjcard.2011.06.040. [DOI] [PubMed] [Google Scholar]
- 12.Mandelzweig I., Battler A., Boyko V. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 13.Awaida Jean-Pierre S., Dupuis Jocelyn, Théroux Pierre. Demographics, treatment and outcome of acute coronary syndromes: 17 years of experience in a specialized cardiac centre. Can J Cardiol. 2006;22:121–124. doi: 10.1016/s0828-282x(06)70250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huffman Mark. Sex differences in the presentation and outcomes of acute coronary syndrome in India: results from the Detection and Management of Coronary Heart Disease (DEMAT) Registry. Circulation. 2010;122:A13324. [Google Scholar]
- 15.Bugiardini R., Estrada J.L., Nikus K., Hall A.S., Manfrini O. Gender bias in acute coronary syndromes. Curr Vasc Pharmacol. 2010;8:276–284. doi: 10.2174/157016110790887018. [DOI] [PubMed] [Google Scholar]
- 16.Minha S., Behar S., Krakover R., Boyko V., Vered Z., Blatt A. Characteristics and outcome of patients with acute coronary syndrome and normal or near-normal coronary angiography. Coron Artery Dis. 2010;21:212–216. doi: 10.1097/MCA.0b013e328338cd5c. [DOI] [PubMed] [Google Scholar]
- 17.Radovanovica Dragana, Urbanb Philip, Simonc René, Schmidlid Markus, Maggiorinie Marco, Ricklif Hans, (for the AMIS Plus Investigators) Outcome of patients with acute coronary syndrome in hospitals of different sizes. Swiss Med Wkly. 2010;140:314–322. doi: 10.4414/smw.2010.12986. [DOI] [PubMed] [Google Scholar]
- 18.Justin M., Zaman S. March 2009. Prognosis of Angina and Myocardial Infarction in South Asian and White Populations in the United Kingdom. A thesis submitted to University College London for the degree of Doctor of Philosophy Department of Epidemiology and Public Health University College London. [Google Scholar]
- 19.Arshad Sadia, Dhakam Sajid, Awan Safia. Outcomes in ST Elevation Myocardial Infarction; a comparison of a tertiary care center in Pakistan with European centers. J Pak Med Assoc. 2011;61:1215. [PubMed] [Google Scholar]
- 20.Constantinides S.S., Gieowarsingh S., Halim M., Been M., Shiu M.F. Predictors of mortality in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Heart. 2003;89:1245–1246. doi: 10.1136/heart.89.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ottani Filippo, Galvani Marcello, Antonia Nicolini Francesca. Elevated cardiac troponin levels predict the risk of adverse outcome in patients with acute coronary syndromes. Am Heart J. 2000;140:917–927. doi: 10.1067/mhj.2000.111107. [DOI] [PubMed] [Google Scholar]
- 22.Santopinto J.J., Fox K.A.A., Goldberg R.J., and on behalf of the GRACE Investigators Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE) Heart. 2003;89:1003–1008. doi: 10.1136/heart.89.9.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh M., Rihal C.S., Gersh B.J. Mortality differences between men and women after percutaneous coronary interventions. A 25-year, single-center experience. J Am Coll Cardiol. 2008;51:2313–2320. doi: 10.1016/j.jacc.2008.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Radovanovic D., Erne P., Urban P. Gender differences in management and outcomes in patients with acute coronary syndromes: results on 20,290 patients from the AMIS Plus Registry. Heart. 2007;93:1369–1375. doi: 10.1136/hrt.2006.106781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Claassen Mette, Sybrandy Kirsten C., Appelman Yolande E., Asselbergs Folkert W. Gender gap in acute coronary heart disease: myth or reality? World J Cardiol. 2012;4:36–47. doi: 10.4330/wjc.v4.i2.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al Suwaidi J., Zubaid M., El-Menyar A.A. Prevalence of the metabolic syndrome in patients with acute coronary syndrome in six middle eastern countries. J Clin Hypertens (Greenwich) 2010;12:890–8999. doi: 10.1111/j.1751-7176.2010.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


